Abstract
Red dot basal cell carcinoma, a distinctive morphologic variant of basal cell carcinoma that presents as a small red macule (dot) or papule, is described on a woman’s thigh. A high index of suspicion is necessary to consider the diagnosis since the tumor mimics a telangiectasia or an angioma.
BASAL CELL CARCINOMA IS THE most commonly occurring neoplasm in humans.1 Potential risk factors in the development of this cancer include genetic syndromes, environmental exposure, immunosuppression, and pigmentary phenotype.2–4 The clinical presentation of basal cell carcinoma is variable1–6; therefore, biopsy of a suspected tumor can confirm the diagnosis. A woman with a distinct, yet uncommonly described, variant of this cancer—red dot basal cell carcinoma—is described and the differential diagnosis is discussed.
CASE PRESENTATION
A 50-year-old woman with a prior history of two primary superficial melanomas on her back and two basal cell carcinomas on her left leg presented to the author’s practice. She presented for evaluation of an older, large, colored mass and a newer, small, red, flat area on her left leg above the knee. She mentioned that one of her prior basal cell carcinomas initially appeared similar to the smaller lesion.
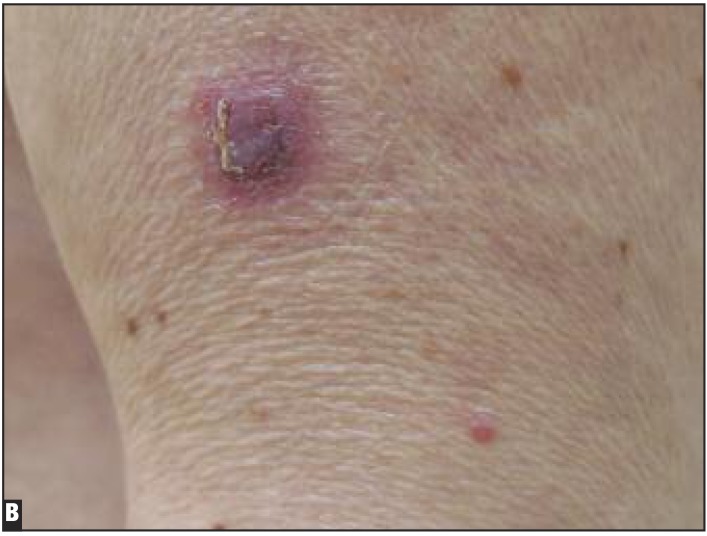
Cutaneous examination showed a 1.5x1.5cm purple-red nodule with erythema of the surrounding skin on the distal portion of the central left thigh. There was also a 3x3mm red macule (dot) on the distal lateral aspect of the left thigh, proximal to the knee (Figures 1A and 1B).
Figures 1A and 1B.
Distant (A) and closer (B) views of the left proximal leg of a woman. The purple-red tumor with adjacent erythema located on the central thigh is a large nodular basal cell carcinoma (asterisk). The smaller 3mm red macule (dot) on the distal lateral left thigh (proximal to the knee) is a red dot basal cell carcinoma (arrow).
Punch biopsy of both lesions was performed. Both specimens showed similar pathologic changes—nodular aggregates of basaloid tumor cells in the dermis; stromal changes and retraction artifact of the dermal collagen around the tumor aggregates were also noted. Correlation of the clinical presentation and the pathology established diagnoses of a nodular basal cell carcinoma for the larger tumor and a red dot basal cell carcinoma (with a nodular histology subtype) for the smaller neoplasm.
DISCUSSION
Basal cell carcinoma of the skin usually occurs on sun-exposed sites; however, less frequently, it can also appear on covered or unusual locations.7,8 The most common clinical presentation—a nodular basal cell carcinoma—is a pearly, pink or flesh-colored, papule with telangiectasia on its surface and a sharply demarcated border. As the tumor outgrows its blood supply, a central ulceration may occur.1–6
Other well-established morphologic subtypes of basal cell carcinoma include a superficial variant (which appears as a red plaque mimicking dermatitis or squamous cell carcinoma in situ), a pigmented variant (which appears as a brown plaque mimicking either a seborrheic keratosis or melanocytic lesion), and a morpheaform or infiltrating variant (which appears as a white area of indurated skin mimicking a scar).1–6 In addition, basal cell carcinoma can be multifocal or linear in distribution.9 Presentation of basal cell carcinoma as a small red dot is not only rare, but also seldom suspected.
The red dot basal cell carcinoma is a distinctive clinical subtype of this tumor. Although it may be regularly encountered in clinical practice, it has seldom been reported. Johnson et al,7 in 1994, mentioned the red dot basal cell carcinoma as an unusual variant of basal cell carcinoma. It was nearly 20 years later, in 2012, that Tromberg et al10 published a letter calling attention to this early presentation of basal cell carcinoma.
Clinically, the neoplasm presents as a small, red macule (or dot); it can be as tiny as 1mm in diameter.7,10 Johnson et al7 commented that the tumor was usually on sun-exposed sites. Morphologically, it mimics either a telangiectasia or a small angioma. Hence, the red dot basal cell carcinoma is a wolf in sheep’s clothing—a cutaneous malignancy that appears similar to a benign, often age-associated, dilatation or aggregation of blood vessels.
Differentiating a red dot basal cell carcinoma from a similar-appearing vascular lesion can be challenging. Since the diagnosis of red dot basal cell carcinoma is usually not suspected prior to skin biopsy, clinical assessment, such as diascopy, to evaluate the lesion has not been described. In contrast to a telangiectasia that characteristically blanches when a glass microscope slide is pressed firmly upon the lesion, an angioma does not blanch with diascopy; however, a red dot basal cell carcinoma has not been evaluated with this technique. In the future, when the diagnosis of red dot basal cell carcinoma is considered, either dermoscopy or confocal microscopy may potentially be useful to aid in the differentiation of red dot basal cell carcinomas from benign vascular lesions.6
Tromberg et al10 noticed that “… a subtle shiny induration or pearling of the epidermis around the red dot can be seen…” when the surrounding skin is stretched. However, they were not able to correlate the clinical presentation of a red dot basal cell carcinoma with a specific histologic pattern of the tumor. In addition, they noted that the size of the red dot was not predictive of the subsequent wound defect following complete tumor removal using Mohs surgery—for some of the tumors, the visible small red dot represented “the tip of an iceberg” with a much larger area of tumor size being present in the dermis.10
CONCLUSION
Red dot basal cell carcinoma is a unique and distinctive morphologic variant of basal cell carcinoma. The tumor presents as a red macule or papule, as small as 1mm in diameter. The pathology of red dot basal cell carcinoma does not correspond to a specific subtype of basal cell carcinoma and the size of the dot does not always correspond to the diameter of the tumor excised. Clinically, the neoplasm mimics a benign vascular lesion, such as a telangiectasia or an angioma. A high index of suspicion by the clinician is necessary to consider the diagnosis. When the possibility of a red dot basal cell carcinoma is entertained, either dermoscopy or confocal microscopy or both might be helpful in differentiating the neoplasm from a telangiectasia or an angioma. Therapeutic intervention for red dot basal cell carcinoma is similar to other subtypes of basal cell carcinoma, with successful management following complete surgical excision of the tumor.
Footnotes
Disclosure:The author reports no relevant conflicts of interest.
REFERENCES
- 1.Crowson AN. Basal cell carcinoma: biology, morphology and clinical implications. Mod Pathol. 2006;19:S127–S147. doi: 10.1038/modpathol.3800512. [DOI] [PubMed] [Google Scholar]
- 2.Rubin AI, Chen EH, Ratner D. Basal cell carcinoma. N Engl J Med. 2005;353:2262–2269. doi: 10.1056/NEJMra044151. [DOI] [PubMed] [Google Scholar]
- 3.Brooke RCC. Basal cell carcinoma. Clin Med. 2005;5:551–554. doi: 10.7861/clinmedicine.5-6-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong CSM, Strange RC, Lear JT. Basal cell carcinoma. Br Med J. 2003;327:794–798. doi: 10.1136/bmj.327.7418.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen PR. Basal cell carcinoma. J Gt Houst Dent Soc. 1995;67(1):20–21. [PubMed] [Google Scholar]
- 6.Mackiewicz-Wysocka M, Bowsczyc-Dmochowska M, Strzelecka-Weklar D, et al. Basal cell carcinoma-diagnosis. Contemp Oncol (Pozn) 2013;17:337–342. doi: 10.5114/wo.2013.35684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson TM, Tschen J, Ho C, et al. Unusual basal cell carcinomas. Cutis. 1994;54:85–92. [PubMed] [Google Scholar]
- 8.Cohen PR. Basal cell carcinoma of the axilla: review of the world literature. Am J Clin Dermatol. 2014;15:95–100. doi: 10.1007/s40257-014-0066-8. [DOI] [PubMed] [Google Scholar]
- 9.Chopra KF, Cohen PR. Linear basal cell carcinomas: report of multiple sequential tumors localized to a radiotherapy port and review of the literature. Tex Med. 1997;93(7):57–59. [PubMed] [Google Scholar]
- 10.Tromberg J, Dinehart S, Amonette R. “Red dot” basal cell carcinoma: an early and distinct clinical presentation [letter] Dermatol Surg. 2012;38:1761–1763. doi: 10.1111/j.1524-4725.2012.02539.x. [DOI] [PubMed] [Google Scholar]