Abstract
Introduction:
People with mental health disorders are much more likely to smoke compared to those who do not. This study investigates recent trends in smoking behaviors among both these populations in England.
Methods:
We used survey responses from adults (aged 16 years and older) living in households in England who participated in the Health Survey for England from 1993 to 2011 (n = 11,300 per year on average). Linear regression was used to quantify annual changes over the time period in smoking prevalence, daily cigarette consumption, and desire to quit among respondents with and without 2 indicators of mental disorder (self-reported longstanding mental illness and recent use of psychoactive medication).
Results:
Among survey respondents who did not report a longstanding mental illness, there were long-term declines in smoking prevalence (−0.48% per year, 95% confidence interval [CI] = −0.56 to −0.40) and daily cigarette consumption (−0.14% per year, 95% CI = −0.17 to −0.11). Similar declines were also seen among respondents not taking psychoactive medications. However, there were no long-term changes in smoking prevalence and cigarette consumption among respondents who reported these indicators of mental disorder, although smoking prevalence among those taking psychoactive medications may have declined during the later part of the study period. Smokers both with and without the 2 indicators of mental disorder showed similar levels of desire to quit smoking.
Conclusions:
Smoking is largely unchanged since 1993 among those with indicators of longstanding mental disorders or recent psychoactive medication usage, although declines have been observed among those without such indicators of mental disorder.
Introduction
Smoking prevalence has declined in many countries in recent years, and overall mortality from smoking-related disease is now falling.1 However, survey data consistently highlight a higher smoking prevalence in people with mental health disorders,2,3 though temporal trends in prevalence in this group have not been extensively studied. In one study from the United States, declines in smoking prevalence seen in the general population from 2004 to 2011 did not extend to those with indicators of mental disorder4 and similar findings have been reported amongst adults living in New York State.5 Any widening of the prevalence gap between people with and without mental disorders, such as that suggested by these American data, will increase existing health impacts and inequalities.3,6–9 This article presents data from the Health Survey for England (HSE) to describe trends over time in smoking behavior in England in people who do and do not report having a longstanding mental disorder or that they are taking a psychoactive medication.
Methods
The HSE is a repeated annual cross-sectional household survey which has questioned on average 11,300 adults aged 16 and over in England each year since 1993 (range 4,610–16,551, with interviews taking place across the year). The survey uses a multi-stage stratified random sampling strategy to produce nationally representative information about a number of aspects of population health. We used data from 1993 to 2011 and extracted information on two indicators of mental disorder. Each year, respondents were asked “Do you have any long-standing illness, disability, or infirmity? By long-standing I mean anything that has troubled you over a period of time, or that is likely to affect you over a period of time?” This question has been used for many years across several UK surveys, with respondents’ answers categorized into major illness groups, including a category termed “longstanding mental illness, depression or anxiety.” Secondly, in the majority of years since 1995 HSE respondents have been asked for the names of prescribed medications they had taken within the 7 days prior to the interview, from which those taking psychoactive treatments (antipsychotics, mood stabilizers, antidepressants, and anxiolytics) were identified. Current smokers, defined as those who responded positively to the question “Do you smoke cigarettes at all nowadays?” were asked how many cigarettes they consume daily and, since 2000, whether they would like to give up smoking altogether.
For each year, smoking prevalence (with 95% confidence interval [CI]) was calculated separately in four subgroups of respondents: smokers reporting having a longstanding mental illness; smokers not reporting having a longstanding illness; smokers reporting taking a psychoactive medication at the time of the survey; and smokers not reporting taking a psychoactive medication at the time of the survey. In smokers, the average number of cigarettes consumed per day and (since 2000) the proportion wanting to quit smoking altogether was calculated for each group. Linear regression was used to quantify the temporal trend in each outcome measure in each subgroup over the study period. All analyses accounted for the survey sampling design and participant non-response.
HSE data were obtained from the Economic and Social Data Service and no additional ethical approval was required for their use. All analyses were carried out using STATA 12.0 (STATA Corp, College Station, TX).
Results
Prevalence of Mental Health Problems Over Time
The proportion of survey respondents reporting a longstanding mental health condition increased gradually from 1.7% in 1993 (95% CI = 1.5–1.9) to 3.8% in 2011 (95% CI = 3.3–4.2). Similarly, an increase was also observed in the proportion of respondents who reported taking a psychoactive medication at the time of the survey, from 3.8% in 1995 (95% CI = 3.5–4.1) to 5.5% in 2011 (95% CI = 5.0–6.1). There was some overlap between the two measures of mental disorder. In 2011, for example, 91.9% of respondents reported neither indicator, 2.0% reported both, 49.0% of respondents reporting a longstanding mental health condition also reported recent use of a psychoactive drug and 32.1% of respondents reporting taking a psychoactive drug also reported a longstanding mental health condition.
Smoking Prevalence and Cigarette Consumption Over Time
Figure 1 illustrates the temporal changes observed in smoking prevalence and cigarette consumption for respondents with and without a longstanding mental health condition and who were and were not taking a psychoactive medication. Table 1 presents the results of linear regression showing the average annual decline in each measure of smoking behavior over the time period for which data were available.
Figure 1.
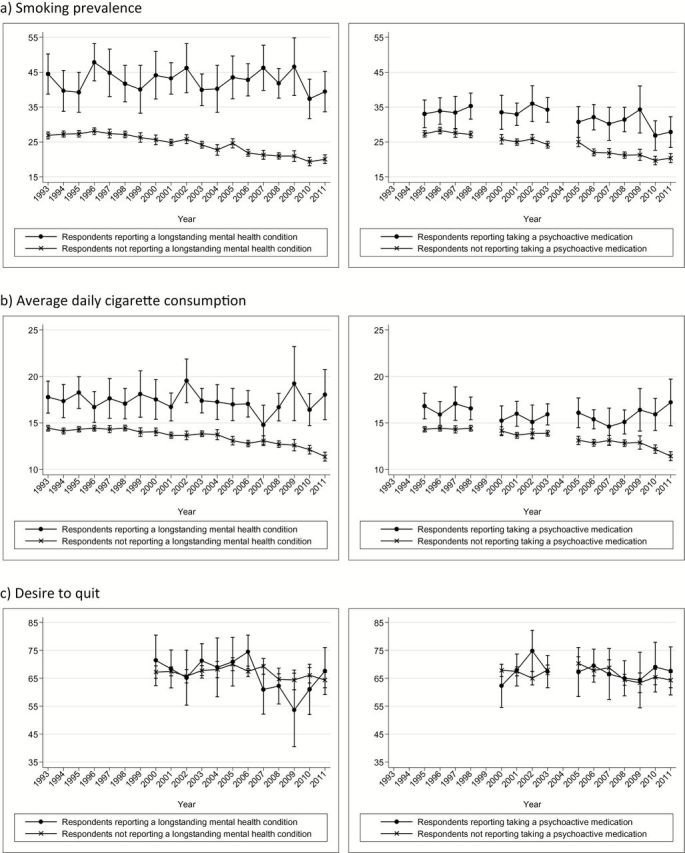
Temporal trends in smoking behvaiors according to self-reported mental health status and psychoactive drug use (bars indicate 95% CI). (A) smoking prevalence; (B) average daily cigarette consumption; (C) desire to quit. CI = confidence interval.
Table 1.
Annual Absolute % Changes in Smoking Behaviors Among Respondents Reporting and Not Reporting a Longstanding Mental Health Disorder or Currently Taking a Psychoactive Medication
| Respondents not reporting a mental health condition (% change, 95% CI) | Respondents reporting a mental health condition (% change, 95% CI) | Respondents not reporting taking a psychoactive medication (% change, 95% CI) | Respondents reporting taking a psychoactive medication (% change, 95% CI) | |
|---|---|---|---|---|
| Smoking prevalence | −0.48 (−0.56 to −0.40)** | −0.07 (−0.33 to 0.20) | −0.53 (−0.61 to −0.44)** | −0.32 (−0.54 to −0.10)* |
| Average daily cigarette consumption | −0.14 (−0.17 to −0.11)** | −0.03 (−0.12 to 0.07) | −0.16 (−0.19 to 0.12)** | −0.03 (−0.12 to 0.05) |
| Proportion of smokers reporting wanting to quit (from 2000) | −0.24 (−0.56 to 0.09) | −0.89 (−1.86 to 0.08) | −0.29 (−0.67 to 0.09) | −0.06 (−0.71 to 0.59) |
CI = confidence interval. *p < .05, **p < .001.
The comparatively small number of HSE respondents reporting a longstanding mental health condition (324 per year on average) or recent psychoactive drug use (502 per year) results in relatively large confidence intervals around the population estimates of smoking prevalence and cigarette consumption. However, inspection of Figure 1 and Table 1 suggests that smoking prevalence and average daily cigarette consumption have declined steadily over time in respondents without each indicator of mental disorder, but that there has been little change in those who report a longstanding mental health condition or who report taking a psychoactive medication.
Though a significant annual change in smoking prevalence in patients taking a psychoactive medication is reported in Table 1, inspection of Figure 1 suggests that the decline may only have occurred toward the end of the time series and indeed the regression coefficient for the trend over time excluding the last 2 years’ of data is non-significant. Smoking prevalence may perhaps have started to decline in 2010 in both indicators of mental disorder, with a small upturn in 2011, though further surveys are needed to confirm any trend.
Changes in Desire to Quit Over Time
The proportion of smokers with and without a longstanding mental illness who report wanting to quit shows no upwards or downwards trend over time. Similarly, there was no significant change over time in the proportion of smokers who are/are not taking a psychoactive medication who report wanting to quit.
As Supplementary data, we present results of analysis in respondents with both indicators and neither indicator of mental disorder. These results are in line with the data presented above, showing a statistically significant long-term decline in smoking prevalence and daily consumption in smokers with neither indicator of mental disorder, no significant trend in those with both indicators, and no change over time in desire to quit in both groups.
Discussion
The HSE data presented here show long-term declines in smoking prevalence and average daily cigarette consumption in people who do not report having a longstanding mental health condition or taking psychoactive medication, but no decline in those with these indicators of mental disorder, with the exception of a possible recent decline in prevalence in people taking a psychoactive medication. As a result, smoking-related health inequalities have arguably increased between these groups, despite all groups showing a similar desire to quit which has not changed since 2000 (apart from an apparent small decline in those with longstanding mental illness between 2006 and 2009, which appears to be increasing again since then).
There are some limitations with the HSE data analyzed in this study. From the questions asked of survey respondents and the resulting data available it is not possible to say in any detail what type of mental health disorder an individual has, or whether a respondent’s reported condition has been confirmed as a clinical disorder by professionals. The two indicators are likely capturing different types of mental disorder given the discrepancy between the proportions reporting positively to the two questions. A more comprehensive set of questions assessing specific serious mental health disorders would have been preferable to the questions asked in the HSE. However, national psychiatric morbidity surveys are carried out infrequently (in England, about every 7 years) and therefore the data are insufficient for assessing trends over time. Few annual national smoking surveys assess mental health adequately. We recommend that researchers advocate for the inclusion of improved questions in national smoking surveys in the future. In addition, as mentioned previously the small number of survey participants with the indicators of mental health used here limits the power to generate accurate estimates for each year. Indeed, the estimate of smoking prevalence in those taking a psychoactive medication in 2009 may be an outlier (Figure 1a), making it difficult to judge whether prevalence in this group has, in fact, been in decline since approximately 2003. The linear regression approach we have used to generate estimates of percentage changes in each outcome per year does not take into account the error around each annual estimate. However, our conclusions are unchanged when data are analyzed using a logistic model.
The 2007 Adult Psychiatric Morbidity Survey (APMS) reports a prevalence of 17.8% of any mental disorder, though for a number of specific conditions, including depression and anxiety, respondents are only asked whether they have been affected over the past week10; this makes comparison with the HSE estimates of longstanding mental disorder difficult. A study using national general practitioner data found a much higher prevalence (14%) of psychoactive medication usage at any point over the course of a year11 than the prevalence of current psychoactive medication use captured by the HSE survey (which asks about medication use within the 7 days prior to interview). A significantly higher smoking prevalence was observed in those using psychoactive medication in these general practitioner data11 and we have no reason to believe that there would be a difference in trends in smoking prevalence between this larger group of medication users and our smaller sample.
The proportion of survey respondents self-reporting a longstanding mental health condition has increased over time, which may reflect a greater willingness to report such problems rather than a true increase in their prevalence. Thus, the characteristics of the patients identified as having a longstanding mental health condition may have changed over time and, if these characteristics are also related to smoking behavior, this may confound assessment of longitudinal trends in smoking prevalence, cigarette consumption and desire to quit. Similarly, propensity to report smoking may have changed over time, particularly as the behavior has become less socially acceptable.
As a household survey the HSE excludes those with mental disorders who are not living in the community. People with the most severe mental illness may be living in inpatient healthcare institutions, or perhaps in other settings such as prisons and temporary housing, or be homeless. These groups are also known to have a higher smoking prevalence and the HSE may, therefore, underestimate the population prevalence of mental illness and smoking.
The disparity between the proportion of survey respondents reporting the use of psychoactive medication and those reporting a longstanding mental health condition indicates some complexities related to these measures of mental disorder. Certain psychoactive medications are commonly prescribed for the treatment of somatic rather than psychiatric conditions (e.g., antidepressants for chronic pain), and thus patients taking these drugs may not report themselves as having a longstanding mental condition. However, we included this measure for completion as some people with a mental health condition might not have classified their illness as “long-standing mental illness, depression or anxiety.”
Our findings are in line with those from America reported recently.4,5 Further work is needed to understand the reasons for the persisting high smoking prevalence and daily cigarette consumption in smokers with mental disorder. These figures may be driven by different patterns of smoking uptake and/or cessation in smokers with mental disorder compared to those without. Given that smokers both with and without a longstanding mental health condition report similar levels of desire to quit smoking altogether, similar to findings reported previously,12 it may be that there are barriers to cessation in smokers with mental disorders. One possible explanation is that these smokers receive cessation interventions less frequently during routine primary health care consultations than smokers without mental disorders, which may translate into lower quit rates.11
Figure 1 suggests that the fastest rate of decline in smoking prevalence and daily cigarette consumption in those who do not report a longstanding mental health condition has occurred since the start of the 21st century. A number of tobacco control measures have been introduced in England over this time period, including the addition of graphic health warnings to cigarette packaging, establishment of specialist cessation services, pricing policies, as well as the introduction of smokefree legislation. Such policies may have altered patterns of smoking, and smokers with indicators of mental disorder may not have responded in the same way to this changing policy environment as smokers without these indicators. Again, further work is warranted to investigate any differential impact of policies. Improved knowledge is vital to enable appropriate measures to be taken to reduce smoking in those with mental disorders and so reduce widening health inequalities caused by their persistent smoking patterns.
Funding
Both authors are members of the UK Centre for Tobacco and Alcohol Studies. Funding to UKCTAS from the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council, the Medical Research Council, and the National Institute of Health Research, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged.
Supplementary Material
Supplementary data can be found online at http://www.ntr.oxfordjournals.org.
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The authors thank Dr. Elena Ratschen, University of Nottingham, for her comments on the manuscript. Our analysis of trends in smoking behaviors was carried out as part of a wider report on smoking and mental health commissioned by the Royal College of Physicians.
References
- 1. Peto R, Lopez AD, Boreham J, Thun M. Mortality from Smoking in Developed Countries 1950–2005. 2012. http://www.ctsu.ox.ac.uk/~tobacco/ Accessed September 09, 2014. [Google Scholar]
- 2. Coulthard M, Farrell M, Singleton N, Meltzer H. Tobacco, Alcohol and Drug Use and Mental Health. London: The Stationary Office, 2002. http://www.ons.gov.uk/ons/rel/psychiatric-morbidity/tobacco--alcohol-and-drug-use-and-mental-health/2000/tobacco--alcohol-and-drug-use-and-mental-health---tobacco--alcohol-and-drug-use-and-mental-health.pdf Accessed September 09, 2014. [Google Scholar]
- 3. Ziedonis D, Hitsman B, Beckham JC, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Halth report. Nicotine Tob Res. 2008;10:1691–1715. [DOI] [PubMed] [Google Scholar]
- 4. Lê Cook B, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. J Am Med Assoc. 2014;311:172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. New York State Department of Health. Adults in New York who report poor mental health are twice as likely to smoke cigarettes. Tobacco Control Program StatShot. 5, 2012. http://www.health.ny.gov/prevention/tobacco_control/reports/statshots/volume5/n2_mental_health_and_smoking_prevalence.pdf Accessed September 09, 2014. [Google Scholar]
- 6. Brown S, Barraclough B, Inskip H. Causes of the excess mortality of schizophrenia. Br J Psychiatry. 2000;177:212–217. [DOI] [PubMed] [Google Scholar]
- 7. Department of Health. Healthy Lives, Healthy People: A Tobacco Control Plan for England. London: Department of Health, 2011. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213757/dh_124960.pdf Accessed September 09, 2014. [Google Scholar]
- 8. Osborn DPJ, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Research Database. Arch Gen Psychiatry. 2007;64:242–249. [DOI] [PubMed] [Google Scholar]
- 9. Parks J, Svendsen D, Singer P, Foti ME. Morbidity and Mortality in People with Serious Mental Illness. Alexandria, VA: National Association of State Mental Health Program Directors, 2006. http://www.nasmhpd.org/docs/publications/MDCdocs/Mortality%20and%20Morbidity%20Final%20Report%208.18.08.pdf Accessed September 09, 2014. [Google Scholar]
- 10. Royal College of Physicians and the Royal College of Psychiatrists. Smoking and Mental Health. London: Royal College of Physicians and the Royal College of Psychiatrists, 2013. [Google Scholar]
- 11. Szatkowski L, McNeill A. The delivery of smoking cessation interventions to primary care patients with mental health problems. Addiction. 2013;108:1487–1494. [DOI] [PubMed] [Google Scholar]
- 12. Siru R, Hulse GK, Tait RJ. Assessing motivation to quit smoking in people with mental illness: a review. Addiction. 2009;104:719–733. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


