Abstract
Objective
A recent HIV outbreak in a rural network of persons who inject drugs (PWID) underscored the intersection of the expanding epidemics of opioid abuse, injection drug use (IDU), and associated increases in hepatitis C virus (HCV) infections. We sought to identify U.S. communities especially vulnerable to rapid spread of IDU-associated HIV, if introduced, and new or continuing high rates of HCV infections.
Design
We conducted a multi-step analysis to identify which indicator variables were highly associated with IDU. We then used these indicator values to calculate vulnerability scores for each county to identify which were most vulnerable.
Methods
We used confirmed cases of acute HCV infection reported to the National Notifiable Disease Surveillance System, 2012–2013, as a proxy outcome for IDU, and 15 county-level indicators available nationally in Poisson regression models to identify indicators associated with higher county acute HCV infection rates. Using these indicators, we calculated composite index scores to rank each county’s vulnerability.
Results
A parsimonious set of six indicators were associated with acute HCV infection rates (proxy for IDU): drug overdose deaths, prescription opioid sales, per capita income, white, non-Hispanic race/ethnicity, unemployment, and buprenorphine prescribing potential by waiver. Based on these indicators, we identified 220 counties in 26 states within the 95th percentile of most vulnerable.
Conclusions
Our analysis highlights U.S. counties potentially vulnerable to HIV and HCV infections among PWID in the context of the national opioid epidemic. State and local health departments will need to further explore vulnerability and target interventions to prevent transmission.
Keywords: human immunodeficiency syndrome (HIV), hepatitis C virus (HCV), persons who inject drugs, opioid epidemic, vulnerability analysis
Introduction
During the past decade, the U.S. opioid epidemic has fueled an increase in illicit injection drug use (IDU) and new hepatitis C virus (HCV) infections, especially within non-urban communities.1–6 For the first time, late in 2014, injection of prescription opioids was linked to an outbreak of HIV infections in a rural U.S. community (Austin in Scott County, Indiana). This event raised concerns about the vulnerability of similar communities to the rapid spread of HIV infection if introduced into a network of persons who inject drugs (PWID). The socioeconomic context within which this outbreak occurred was not unique: unemployment and poverty in the county exceeded national levels,7 educational attainment was low,7 and life expectancy was poor.8 During November 2014 – October 2015, 181 persons were diagnosed with HIV infection, of whom 92% were coinfected with HCV.9 This county of approximately 24,000 persons reported fewer than five new HIV infections in the preceding ten years.9,10
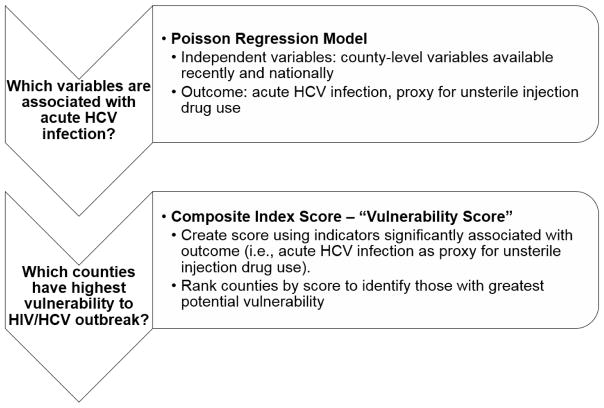
Rapid recognition of the outbreak and implementation of intensive control efforts likely reduced new HIV and HCV infections and limited their geographic spread.9 Identifying jurisdictions particularly vulnerable to a similar outbreak can increase awareness of current vulnerability and guide public health efforts to detect and prevent this type of event. To this end, we conducted a multi-step analysis (Figure 1) to identify which set of indicators (independent variables) is highly associated with IDU, then used each U.S. county’s values for these indicators to calculate a vulnerability score for each county, and finally identified which states and specific counties are most vulnerable.
Figure 1.
Multi-step approach to identify counties with greatest vulnerability to rapid dissemination of injection drug use-associated HIV infection, if introduced, and new or continued Hepatitis C virus infections.
Methods
Outcome variable
Nationally, there is no reliable county-level measure of IDU, the outcome of interest for this analysis. We therefore relied on a proxy measure for this behavior. We chose the county-level rate of persons reported with confirmed acute HCV infection as the best proxy measure for the county-level rate of PWID for three reasons. First, the acute phase of HCV infection occurs very close in time to the injection event and is transitory.5,6 Although not all acute HCV cases are acquired through IDU and not all PWID get HCV, the county-level rates of acute HCV and IDU are assumed to have a fixed relationship that does not vary by time, place, or infection. Second, HCV is highly transmissible, especially through IDU, which is the primary risk factor for HCV infection.5,6 Third, acute HCV infections are reported nationally through the National Notifiable Disease Surveillance System (NNDSS).11 Although the sensitivity of the NNDSS is limited,12 it has been demonstrated sufficient for other national-level analyses and the large majority of states and the District of Columbia voluntarily report cases.2,4,13
We included NNDSS data from 2012 and 2013. Counties in states that reported no acute HCV cases to CDC in 2012 or 2013 were excluded from the analysis (i.e., missing values). We applied the following rules to identify counties with zero cases of acute HCV infection from those with missing values in a given year. For states that reported >1 case, we assumed counties with no reported acute HCV cases had zero cases. For states that reported one case of acute HCV infection for one year and no cases in the other year, we assumed that all other counties had zero acute HCV cases during the one-case year and all counties had missing values for the other year. Thus, that state was included for the analysis in the one-case year and excluded in the other year because there was limited evidence the state was able to consistently identify and report acute HCV cases.
Potential indicator variables
We investigated county-level independent variables that were known or plausibly associated with IDU and that could thus potentially serve as indicators of vulnerability to rapid dissemination of HIV/HCV infection among PWID. We required that data for potential indicators be available nationally at the county level or transformable to the county level, reported at least annually, recent (ideally reported within the past three years), and complete (<10% of U.S. counties missing values). Data were transformed, if needed, by converting data aggregated by 3- or 5-digit ZIP codes to 5-digit county Federal Information Processing Standard (FIPS) codes using area proportion method. Forty-eight potential indicators were identified and considered from six domains: 1) drug-overdose mortality, 2) access to prescription opioids (e.g., production, sales, prescriptions), 3) access to care (e.g., evidence of use of care or treatment services related to IDU), 4) drug-related criminal activity (e.g., arrests for drug possession or sales), 5) prevalence of IDU (e.g., survey-based data), and 6) sociodemographic characteristics associated with geographic areas with higher IDU prevalence. Table 1 describes 15 of 48 potential indicators that met our inclusion criteria (see Supplemental Digital Content, Figure S1, which shows maps of the county-level indicators). Data from 2012 and 2013 were used when available since the indicators are intended to reflect current areas of vulnerability; when not available, we used data from the most recent year available. All indicators were treated as continuous numerical variables except presence of urgent care facilities and access to interstate within five miles of county border, which were dichotomous (yes/no). Descriptive statistics, including median, mean, first quartile and third quartile were calculated for the 13 continuous indicators; frequency and percentage were calculated for the two dichotomous indicators.
Table 1.
Indicators assessed for association with acute Hepatitis C virus infection as proxy for unsafe injection drug use
| Indicator | Source | Definition |
|---|---|---|
| 1. Drug overdose mortality (drug overdose deaths per 100,000 population) | National Center for Health Statistics (NCHS)/National Vital Statistics, 2012 and 2013 | Drug overdose deaths were extracted using the ICD-10 based on the following underlying cause of death codes: X40-X44 (unintentional); X60-X64 (suicide); X85 (homicide); Y10-Y14 (undetermined intent). County-level rates were calculated per 100,000 population using US Census population estimates for 2012 and 2013. |
| 2. Prescription opioid sales (Prescription opioid sales per 10,000 population) | Drug Enforcement Administration (DEA) - Automation of Reports and Consolidated Orders System (ARCOS), 2013 | The rate of morphine milligram equivalent kilograms sold of opioid pain relievers per 10,000 population in 2013 were transformed from 3-digit ZIP to 5-digit county FIPS using an area proportion method. The rate for the 3-digit ZIP within which the county centroid is located was applied to the entire county. |
| 3. Mental health services (Mental health providers per 100,000 population) | Centers for Medicare and Medicaid Services, National Provider Identification, 2014 | Mental health providers include psychiatrists, psychologists, and licensed clinical social workers specializing in mental health care. The rate was calculated as the number of mental health providers per 100,000 population (2010 Census). |
| 4. Insurance coverage (Percent of population without insurance coverage) | American Community Survey, 2012 and 2013 5-year estimates | The number of person without health insurance coverage was divided by total civilian noninstitutionalized population. |
| 5. Urgent care facilities (Presence, Yes/No, of an urgent care facility) | HSIP 2012 Gold Database | Urgent care is defined as the delivery of ambulatory medical care outside of a hospital emergency department on a walk-in basis without a scheduled appointment. This indicator was dichotomized to yes – at least 1 urgent care facility or no – no urgent care facility. Publication date: 07/17/2009. |
| 6. Vehicle availability (Percent of households with access to a vehicle) | American Community Survey, 2012 and 2013 5-year estimates | The number of households with a vehicle available divided by the total estimated number of households per county. |
| 7. Access to interstate (Highway/interstate access within 5 miles) | ESRI maps and data, 2014 | At least 1 interstate or major US highway exit in or within 5 miles of the county border. Edition date: 06/30/2010. |
| 8. Education (Percent of population without high school diploma) | American Community Survey, 2012 and 2013 5-year estimates | The number of persons aged 25 years and older with less than a 12th grade education (including individuals with 12 grades but no diploma) divided by the estimated county population age 25 years and older. |
| 9. Income (Per capita income, log base 10) | American Community Survey, 2012 and 2013 5-year estimates | The mean income per person in the county; derived by dividing the total income of all people 15 years and older by the total population; modeled as log base 10. |
| 10. Population density (Population per square mile) | US Census | The average population per square mile per county; modeled as log base 10. |
| 11. Poverty (Percent of persons in poverty) | American Community Survey, 2012 and 2013 5-year estimates | Poverty levels were defined by the Census Bureau, which uses a set of income thresholds that vary by family size and composition to determine who is in poverty. If a family’s total income is less than the family’s threshold, then that family and every individual in it is considered in poverty. The number of persons in poverty was divided by the estimated total county population. |
| 12. Race/ethnicity (Percent of population of white, non-Hispanic race/ethnicity) | American Community Survey, 2012 and 2013 5-year estimates | The number of persons who reported they were not Hispanic or Latino and were of white race alone divided by the estimated total county population. |
| 13. Unemployment (Percent of population unemployed) | American Community Survey, 2012 and 2013 5-year estimates | The number of civilian persons unemployed and actively seeking work divided by the estimated total civilian population aged 16 years and older. |
| 14. Urban/Rural status (NCHS Urban/Rural continuum classification) | NCHS, 2013 | Counties were categorized into 1 of 6 categories based on Office of Management and Budget’s February 2013 delineation of metropolitan statistical areas and micropolitan statistical areas. Categories include: 1) Large central metro, 2) Large fringe metro, 3) Medium metro, 4) Small metro, 5) Micropolitan, and 6) Non-Core. |
| 15. Buprenorphine prescription capacity (Buprenorphine prescription capacity by DATA 2000* waiver per 10,000 population) | SAMHSA DATA 2000 Program Information, 2014 (restricted data set) | The total number of patients each DATA-waived physician could prescribe to, either 30 or 100, as of June 2014 were transformed from 5-digit ZIP to 5-digit FIPS using an area proportion method. County-level rates were calculated per 10,000 population using US Census population estimates for 2012 and 2013. |
The Drug Addiction Treatment Act of 2000 (DATA 2000) permits physicians who meet certain qualifications to treat opioid addition with Schedule III, IV, and V narcotic medications in treatment centers outside of the traditional Opioid Treatment Program setting.
Note: ICD-10 International Classification of Diseases, Tenth Revision; SAMHSA DATA 2000 Substance Abuse and Mental Health Services Administration Drug Addiction Treatment Act of 2000, FIPS Federal Information Processing Standards.
Regression modeling
We used modeling to identify a parsimonious set of IDU-associated indicators with the strongest association with our proxy measure of IDU: acute HCV infection. We modeled the rate of acute infections by county using a multilevel Poisson model with year (2012, 2013) nested in county and county nested in state with the county population set as the offset. We treated the states and counties as random effects to account for heterogeneity. Each of the 15 indicators was modeled using a univariable Poisson random-effects model. Per-capita income and population per-square-mile were modeled on a log10 scale. We entered all 15 indicators in a multivariable model and removed the indicator with the highest p-value, then removed and added indicators in a backwards stepwise procedure until all remaining variables had a p-value<0.05. We used this approach because we were aiming to identify indicators with the strongest association with county-level acute HCV infection rates rather than indicators causally associated with acute HCV infection, in which case step-wise modeling procedures are not recommended (see Supplemental Digital Content, Regression Modeling Analyses which describes the Modeling Procedure). We assessed the linearity assumption and collinearity of our continuous indicators (see Supplemental Digital Content, Regression Modeling Analyses which describes the Continuous Indicators Linearity Assessment and Collinearity Assessment of Indicators). Standardized regression coefficients were calculated from the final multivariable model to determine the relative contribution of each indicator (see Supplemental Digital Content, Regression Modeling Analyses which describes the Standardized Regression Coefficients).
Application of indicators to generate vulnerability scores
To calculate a vulnerability score for each county, we created a scoring dataset that contained the value for each of the final indicators by county. For drug overdose mortality rate, we imputed the median value for the indicator from the values among the bordering counties for 133 (4.2%) counties, assuming that the surrounding counties were most similar to the county with the missing value.14 We averaged indicator values if two years of data were available. For each county, we then multiplied the county’s value for each indicator variable by that indicator’s regression coefficient from the final model and summed to produce a vulnerability score. We ranked counties by their vulnerability scores from 1 to 3,143 with a higher score indicating higher vulnerability.
To account for uncertainty in each county’s vulnerability score, we used simulation to estimate the 90% confidence interval (CI) for each county’s vulnerability score by drawing 10,000 samples from a normal distribution for each regression coefficient. We identified a county as vulnerable when the upper 90% CI for that county’s vulnerability score exceeded or matched the vulnerability score for the 2,985th ranked county (i.e., lower threshold for the top 5% of counties with the highest vulnerability scores) (see Supplemental Digital Content, Composite Index (Vulnerability) Score and Rank, which describes the methodology for the vulnerability scores).
HIV proximity
For each vulnerable county, we sought to assess the likelihood that HIV might be introduced into a network of PWID in that county based on the prevalence of HIV infection in that county and nearby. We defined “HIV proximity” as the weighted average rate of people living with diagnosed HIV infection (PLWH) in and around that vulnerable county at year-end 2012. We demarcated a 20-mile buffer zone around the border of each vulnerable county based on data from the U.S. Department of Transportation National Household Travel Survey that the average daily distance traveled per person per day was 36 miles (approximately 20 miles when rounded for a radius).15 Using a method of spatial smoothing,16 we calculated the area proportion of each county adjacent to the vulnerable county that intersected the vulnerable county’s 20-mile buffer zone and the corresponding weighted numbers of PLWH and total population represented by the buffer zone. We summed these buffer zone values with the values for the vulnerable county to calculate an estimated HIV proximity rate of PLWH per 10,000 population. We used Jenks natural breaks to group counties by estimated HIV proximity.17
Results
The number of acute HCV infection cases reported to CDC in 2012 and 2013 were 1,778 and 2,138 respectively. Of the reported cases, 1,710 (96%) in 2012 and 2,074 (97%) in 2013 were reported from 2,970 counties with valid county FIPS codes and were included in modeling. There were 173 counties in 8 states, as well as the District of Columbia, with no data during 2012–2013; these jurisdictions were excluded from modeling analyses (Alaska, Arizona, Delaware, District of Columbia, Hawaii, Mississippi, New Hampshire, Rhode Island, and Wyoming). Descriptive statistics are presented in Table 2.
Table 2.
Descriptive statistics of potential indicator variables for acute HCV infection and results of regression modeling
| Indicators | Descriptive Statistics1 | Univariable | Multivariable2 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Median | Mean | First quartile | Third quartile | RR | P-value | Regression coefficient | Standardized regression coefficient | sRR | P-value | |
|
|
|
|||||||||
| Drug overdose deaths per 100,000 pop. | 11.7 | 13.6 | 5.8 | 18.4 | 1.024 | <0.0001 | 0.016 | 0.116 | 1.210 | <0.0001 |
| Prescription opioid sales per 10,000 pop. | 7.0 | 7.6 | 5.2 | 9.2 | 1.075 | <0.0001 | 0.024 | 0.052 | 1.090 | 0.0115 |
| Mental health providers per 100,000 pop. | 75.6 | 110.7 | 27.5 | 151.6 | 0.999 | 0.1800 | ||||
| Percent of pop. without insurance coverage | 14.6 | 15.1 | 11.1 | 18.4 | 1.021 | 0.0271 | ||||
| Percent of households with access to vehicle | 94.2 | 93.7 | 92.4 | 95.6 | 1.023 | 0.0029 | ||||
| Percent of pop. without high school diploma | 18.8 | 19.9 | 13.8 | 24.8 | 1.008 | 0.1103 | ||||
| Per capita income, $ | 22,715 | 23,439 | 19,847 | 25,942 | 0.057 | <0.0001 | −2.181 | −0.125 | 0.810 | <0.0001 |
| Pop. per square mile, log base 10 | 46.8 | 46.7 | 18.2 | 123.0 | 0.639 | <0.0001 | ||||
| Percent of pop. living in poverty | 15.8 | 16.4 | 12.0 | 19.9 | 1.027 | <0.0001 | ||||
| Percent of pop. of non-Hispanic white race/ethnicity | 85.7 | 78.7 | 67.9 | 94.0 | 1.028 | <0.0001 | 0.027 | 0.314 | 1.680 | <0.0001 |
| Percent of pop. unemployed | 8.6 | 8.8 | 6.4 | 10.9 | 1.053 | <0.0001 | 0.038 | 0.082 | 1.140 | 0.0095 |
| NCHS Urban/Rural continuum classification | 5.0 | 4.6 | 3.0 | 6.0 | 1.179 | <0.0001 | ||||
| Buprenorphine prescription capacity by DATA 2000 waiver per 10,000 pop. | 7.9 | 24.9 | 0.0 | 35.5 | 1.001 | 0.0664 | 0.002 | 0.046 | 1.080 | 0.0095 |
|
|
|
|||||||||
| N | % | |||||||||
|
|
|
|||||||||
| Access to highway/interstate within 5 miles (Y/N) | 3722 | 65.28% | 0.679 | 0.0111 | ||||||
| Presence of urgent care facility (Y/N) | 2186 | 38.30% | 0.755 | <0.0001 | ||||||
Note. Pop. Population; RR risk ratio; sRR standardized risk ratio
The sample size for the descriptive statistics and univariable regression models is n=2,970 counties (number of counties with acute HCV data) except for drug overdose deaths (n=2,704).
The final multivariable model includes drug overdose deaths per 100,000 population, therefore the sample size is n=2,704.
In the univariable regression models, all indicators were significant at p<0.1, except mental health providers and percentage of the population without high school diploma (Table 2). We found neither substantial departures from linearity nor collinearity between the continuous indicators. Based on the final multivariable model, the following indicators were most significantly associated with the county-level acute HCV infection rate: drug overdose deaths per 100,000 population (regression coefficient [β] 0.016; p<0.0001), prescription opioid sales per 10,000 population (β 0.024; p=0.012), median per capita income, log base 10 (β −2.181; p<0.0001), percent of population of white, non-Hispanic race/ethnicity (β 0.027; p<0.0001), percent of population aged ≥16 years unemployed (β 0.038; p=0.0095), and buprenorphine prescribing potential by DATA 2000 waiver per 10,000 population (β 0.002; p=0.0095) (see Supplemental Digital Content, Supplemental Results and Figures 2 and 3, which describe the Model Fit Results, show the reported rate of acute HCV infection and model-estimated rate of acute HCV infection by county, and illustrate the model fit and 90% confidence intervals for the counties identified as vulnerable).
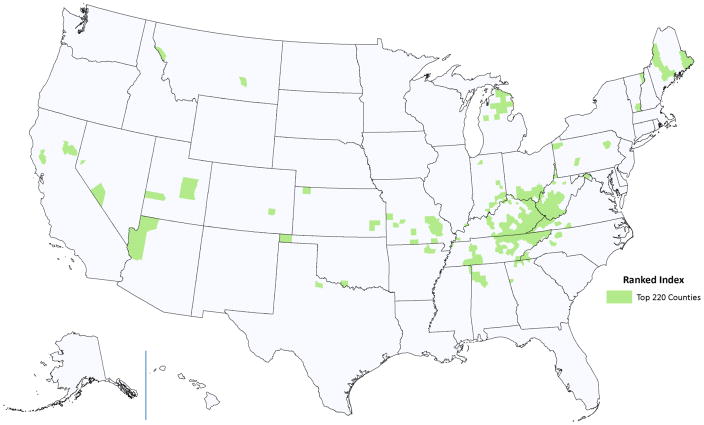
Figure 2.
Counties for which estimated vulnerability scores or their upper 90% confidence interval exceeded the 95th percentile. Map produced by the Geospatial Research, Analysis, and Services Program (GRASP).
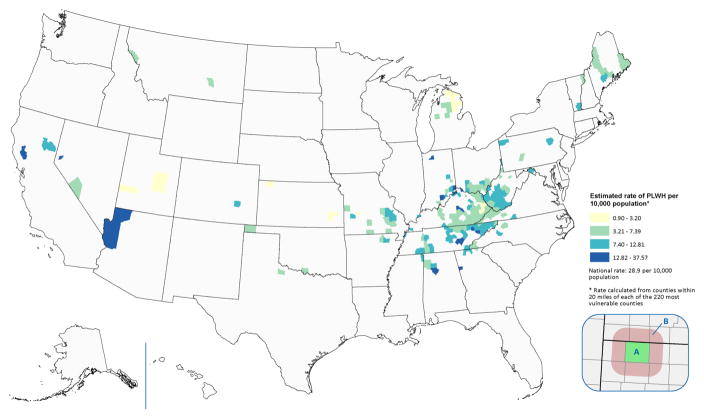
Figure 3.
Estimated rate of people living with diagnosed HIV infection (PLWH) per 10,000 population in and around each vulnerable county at year-end 2012. The weighted average rate of people living with diagnosed HIV infection in the vulnerable county (inset A) and 20 miles beyond the vulnerable county border (inset B) was calculated using the area proportion of each adjacent county within the 20 mile buffer zone and the number of PLWH and county population estimates at year-end 2012. Map produced by the Geospatial Research, Analysis, and Services Program (GRASP).
Vulnerability scores were calculated for all counties using the final model regression coefficients. We identified 220 counties in 26 states as vulnerable communities (Figure 2) (see Supplemental Digital Content, Supplemental Results and Tables 1 and 2, which describe the Composite Index (Vulnerability) Score and Rank and counties identified as vulnerable).
The estimated HIV proximity at year-end 2012 ranged from 0.9 to 37.6 per 10,000 population (Figure 3). With one exception, the estimated HIV proximity for all vulnerable counties was lower than the national rate of 29.3 per 10,000 population.
Discussion
We have developed a method to identify U.S. counties vulnerable to rapid spread of IDU-associated HIV, if introduced, and new or continuing high numbers of HCV infections among PWID. The method employed a proxy measure for county-level IDU (i.e., acute HCV infection). Ecological-level measures have been used previously to create CDC’s Social Vulnerability Index. That index was designed to identify socially vulnerable populations that are more likely to be adversely affected during disaster events (e.g., elderly, people living in poverty).18 It assesses overall census tract vulnerability on the basis of 14 census variables and calculates an overall percentile rank of social vulnerability for each area.18 Our method builds on this approach by first identifying the specific indicators associated with HCV (proxy for IDU). We then calculated an index score to rank counties as well as account for the relative contribution of each indicator to identify the most vulnerable communities. The evolution of IDU in the United States is dynamic and this method can be applied periodically to account for those changes. Improved reporting of acute HCV infections to NNDSS and the identified indicators will increase the accuracy of the method for identifying vulnerable counties over time.
Deaths from drug overdose have grown exponentially in the past decade, surpassing motor vehicle traffic accidents as the leading cause of unintentional injury-related death in the United States.19 Overdose death rates due to prescription opioids increased nearly four-fold from 2000 to 2013.20 Prescription opioids are the most commonly abused prescription drug, and an estimated 10–20% of people who abuse prescription opioids escalate to injection of prescription opioids or heroin,21–23 creating opportunity for IDU-associated outbreaks of HIV or HCV infection.24,25 Rates of acute HCV infection have increased steadily nationwide from 2006–2012, most notably east of the Mississippi River and particularly among states in central Appalachia.4 The potential for an HIV outbreak within an opioid-injecting population was realized in Scott County, Indiana,26 which ranked 32nd among the top 220 counties in our vulnerability analysis.
The demography of PWID and persons diagnosed with acute HCV infection in the United States has changed substantially. From 1999 to 2002, HCV diagnoses in the U.S. were greater among men, non-Hispanic blacks, and persons aged 40–49 years.27 Persons diagnosed with acute HCV infection now are equally likely to be male as female, are predominantly of white, non-Hispanic race/ethnicity, and younger age.2,4,13,28,29 Our finding that white, non-Hispanic race/ethnicity significantly associated with county-level acute HCV infection reflects these changes.
The counties identified in our analysis were overwhelmingly rural. Since 2006, rates of acute HCV infection have increased faster in rural than in urban areas4 consistent with introduction and spread of this infection into populations made newly vulnerable by the expansion of IDU in rural America. The outbreak in Scott County, IN was notable for the absence or minimal availability of harm-reduction strategies to prevent IDU-associated HIV and HCV infections, such as addiction treatment and rehabilitation, medication-assisted therapy (MAT), and syringe service programs (SSPs).9 This outbreak illustrated the need for harm-reduction strategies suited to the rural context. Our analysis can help identify those rural areas at highest risk of infectious complications from IDU where interventions can be prioritized. Unemployment and income were also significantly associated with risk for acute HCV infection. It has been hypothesized that financial stressors increase vulnerability to drug use so that young adults in economically deprived areas may accumulate more risk factors for drug use and be more likely to establish drug dependencies at a younger age than persons in more economically privileged areas.30 Since the Great U.S. Recession of 2007–2009, rural areas have experienced persistent and greater unemployment and poverty than urban areas.31
Buprenorphine is approved for MAT of opioid use disorder. The indicator “buprenorphine prescribing potential by waiver per 10,000 population” represents the potential availability of this form of MAT to the population of a county, reflecting the capacity to treat in response to demand for services and not the actual rate of people receiving treatment.32 In 2011, 43% of U.S. counties had no buprenorphine-waivered physicians,32 indicating that capacity to prescribe MAT likely lags behind the need. It is important that these indicators are not interpreted as causally associated, rather are understood as indicators of potential vulnerability for this type of outbreak.
The risk for introduction and spread of HIV infection into a vulnerable community of persons will vary according to the estimated HIV proximity of the community and the community’s IDU practices. Although estimated HIV proximity was lower than the national average for nearly all of the 220 counties identified as most vulnerable, it is important to consider the estimated HIV proximity in the context of local IDU practices and their identification as a vulnerable county. Scott County, IN was not in the highest estimated HIV proximity group, but the injection practice in Scott County, IN was notable for the high frequency of injections and combined with the relatively large and dense network of PWID9 in the absence of effective strategies to reduce IDU-associated infection leaving the community vulnerable to this type of outbreak.
All health officials can review these results along with the most recent sources of data on HIV and acute HCV diagnoses available to them. Additional local insight may be gained by examining data sources about other factors associated with IDU that were not available for inclusion in our analysis. There are a number of indicators we would like to consider that are not available nationwide but may provide substantial local insight. These data include emergency department and hospital admissions for drug overdose or intoxication; arrests for drug possession or sales; and opioid prescribing patterns from state prescription drug monitoring programs.33 CDC is preparing additional advice to assist health departments so they can assess whether their jurisdiction is experiencing or at risk of new HIV and HCV infections potentially related to IDU (personal communication).
This analysis is subject to limitations. First, we excluded potential indicators, as noted above, because we established strict inclusion criteria to assess vulnerability for each county. Second, this analysis was intended to identify areas currently vulnerable; however, some of the data were ≥3 years old. Third, all ecologic analyses based on reported cases of notifiable disease and deaths are subject to potential underreporting (e.g., HCV data) or misclassification (e.g., cause of death) biases. Reporting of acute HCV infections to NNDSS is susceptible to underreporting12 not only because reporting is passive and voluntary but also because the surveillance case definition captures only persons with symptoms of an illness that is often asymptomatic. These limitations are likely similar throughout the United States and we are unaware of any systematic differences that would meaningfully bias indicator selection. The implementation of complete and timely acute HCV surveillance by all states will increase the accuracy of this method. Fourth, the HIV proximity measure might not accurately measure risk of IDU-associated HIV transmission. Our estimate is limited by the distance of the buffer zone selected and may not reflect the population distribution within each county or underlying characteristics of PLWH in these areas (e.g., percent with suppressed viral load). Lastly, the indicators used may result in bias against identifying urban areas as vulnerable since the percentages of certain characteristics (e.g., percentage white, non-Hispanic) are lower in urban counties. However, the historic concentration of IDU in urban areas has likely resulted in these areas having already taken preventive actions (e.g., SSPs, access to MAT) to reduce risk for infections from IDU.
Prompted by a recent outbreak of HIV infection among PWID in a rural community, we developed a method to identify other communities vulnerable to rapid dissemination of IDU-associated HIV, if introduced, and new or continuing high numbers of HCV infections. Identification of a county as vulnerable to this type of outbreak does not mean an outbreak is eminent; rather jurisdictions identified as at-risk might use potentially informative local data that were not available nationally and take action as recommended in the April 2015 CDC Health Alert Network advisory.34 Expanding epidemics of prescription opioid abuse and IDU and shifting demography and geography, heralded by national changes in patterns of acute HCV infection, are critical driving forces of vulnerability. To reduce vulnerability, targeted interventions in accordance with efforts to prevent and treat substance use disorder and to reduce risk of infectious complications of IDU are warranted.
Supplementary Material
Acknowledgments
The authors would like to thank Drs. Paul Sutton, PhD, at the National Center for Health Statistics, and Jinhee Lee, PharmD, at the Substance Abuse and Mental Health Services Administration, for providing data and expertise on indicator data. We thank Drs. Debra Houry and Grant Baldwin at the CDC National Center for Injury Prevention and Control for their leadership, guidance, and support of this analysis.
Footnotes
Conflicts of Interest and Sources of Funding: No conflicting financial interests exist for any co-author. No funding was received for this analysis.
Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Meeting presentations: National HIV Prevention Conference, Atlanta, December 2015
Contributor Information
Michelle M Van Handel, Division of HIV/AIDS Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Charles E Rose, Division of HIV/AIDS Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Elaine J Hallisey, Geospatial Research, Analysis & Services Program, Division of Toxicology and Human Health Sciences, Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Jessica L Kolling, DRT Strategies with the Geospatial Research, Analysis & Services Program, Division of Toxicology and Human Health Sciences, Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Jon E Zibbell, Division of Viral Hepatitis, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Brian Lewis, HP Enterprise Services with the Geospatial Research, Analysis & Services Program, Division of Toxicology and Human Health Sciences, Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Michele K Bohm, Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Christopher M Jones, Division of Science Polity, Office of the Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services, Washington, DC, United States.
Barry E Flanagan, HP Enterprise Services with the Geospatial Research, Analysis & Services Program, Division of Toxicology and Human Health Sciences, Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Azfar-E-Alam Siddiqi, Division of HIV/AIDS Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Kashif Iqbal, Division of HIV/AIDS Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Andrew L Dent, Geospatial Research, Analysis & Services Program, Division of Toxicology and Human Health Sciences, Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Jonathan H Mermin, Office of the Director, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
Eugene McCray, Division of HIV/AIDS Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
John W Ward, Division of Viral Hepatitis, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
John T Brooks, Division of HIV/AIDS Prevention, National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, United States.
References
- 1.Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–74. doi: 10.1146/annurev-publhealth-031914-122957. [DOI] [PubMed] [Google Scholar]
- 2.Zibbell JE, Iqbal K, Patel RC, et al. Increases in hepatitis C virus infection related to injection drug use among persons aged </=30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. MMWR Morb Mortal Wkly Rep. 2015;64(17):453–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Lipari RN, Hughes A. The NSDUH: Trends in Heroin Use in the United States, 2002 to 2013. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Adminstration; Rockville, MD: 2015. [PubMed] [Google Scholar]
- 4.Suryaprasad AG, White JZ, Xu F, et al. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006–2012. Clin Infect Dis. 2014;59(10):1411–9. doi: 10.1093/cid/ciu643. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. [Accessed 8 October 2015];Viral hepatitis surveillance -- United States. 2013 Available at: http://www.cdc.gov/hepatitis/statistics/2013surveillance/index.htm.
- 6.Centers for Disease Control and Prevention. [Accessed 8 October 2015];Viral hepatitis surveillance -- United States. 2012 Available at: http://www.cdc.gov/hepatitis/statistics/2012surveillance/index.htm.
- 7.U.S. Census Bureau. State and County Quick Facts. [Accessed 10 December 2015];Scott County, Indiana. 2015 Available at: http://www.census.gov/quickfacts/table/PST045214/18143,00.
- 8.Conrad C, Bradley HM, Broz D, et al. Community Outbreak of HIV Infection Linked to Injection Drug Use of Oxymorphone--Indiana, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(16):443–4. [PMC free article] [PubMed] [Google Scholar]
- 9.Peters PJ, Pontones P, Hoover KW, et al. An Outbreak of HIV infection Linked to Injection Drug Use of Oxymorephone -- Indiana, 2014–2015. NEJM. [provisionally accepted] [Google Scholar]
- 10.United States Census Bureau. [Accessed 18 February 2016]; Available at: http://www.census.gov/
- 11.Centers for Disease Control and Prevention. [Accessed 7 October 2015];National Notifiable Disease Surveillance System (NNDSS) Available at: http://www.cdc.gov/nndss/
- 12.Onofrey S, Aneja J, Haney GA, et al. Underascertainment of Acute Hepatitis C Virus Infections in the U.S. Surveillance System: A Case Series and Chart Review. Ann Intern Med. 2015;163(4):254–61. doi: 10.7326/M14-2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Use of enhanced surveillance for hepatitis C virus infection to detect a cluster among young injection-drug users -- New York, November 2004–April 2007. MMWR Morb Mortal Wkly Rep. 2008;57:517–21. [PubMed] [Google Scholar]
- 14.Gelman A, Hill J. Chapter 25 - Missing-data imputation in Data Analysis Using Regression and Multilevel/Hierarchical Models. Cambridge University Press; 2006. pp. 529–544. [Google Scholar]
- 15.US Department of Transportation. [Accessed 18 February 2016];Summary of Travel Trends - 2009 National Household Travel Survey. Available at: http://nhts.ornl.gov/2009/pub/stt.pdf.
- 16.Tiwari C, Rushtin G. Using Spatially Adaptive Filters to Map Late State Colorectal Cancer Indicidence in Iowa, in Developments in Spatial Data Handling. Springler; Berlin Heidelberg: 2005. pp. 665–676. [Google Scholar]
- 17.Jenks GF. The data model concept in statistical mapping. International Yearbook of Cartography. 1967;7:186–190. [Google Scholar]
- 18.Flanagan BE, Gregory EW, Hallisey EJ, et al. A Social Vulnerability Index for Disaster Management. J of Homeland Security and Emergency Management. 2011;8(1) Article 3. [Google Scholar]
- 19.Warner M, Chen LH, Makuc DM, et al. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011;81:1–8. [PubMed] [Google Scholar]
- 20.Hedegaard H, Chen LH, Warner M. Drug-poisoning deaths involving heroin: United States, 2000–2013. NCHS Data Brief. 2015;190:1–8. [PubMed] [Google Scholar]
- 21.Neaigus A, Miller M, Friedman SR, et al. Potential risk factors for the transition to injecting among non-injecting heroin users: a comparison of former injectors and never injectors. Addiction. 2001;96(6):847–60. doi: 10.1046/j.1360-0443.2001.9668476.x. [DOI] [PubMed] [Google Scholar]
- 22.Lankenau SE, Teti M, Silva K, et al. Patterns of prescription drug misuse among young injection drug users. J Urban Health. 2012;89(6):1004–16. doi: 10.1007/s11524-012-9691-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Substance Abuse and Mental Health Services Adminstration. BHSIS Series. Substance Abuse and Mental Health Services Adminstration; Rockville, MD: 2014. Center for Behavioral Health Statistics and Quality, Treatment Episode Data Set (TEDS): 2002–2012. National Admissions to Substance Abuse Treatment Services. [Google Scholar]
- 24.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132(1–2):95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 25.Jones CM, Logan J, Gladden RM, et al. Vital Signs: Demographic and Substance Use Trends Among Heroin Users - United States, 2002–2013. MMWR Morb Mortal Wkly Rep. 2015;64(26):719–25. [PMC free article] [PubMed] [Google Scholar]
- 26.Indiana State Department of Health. [Accessed 16 September 2015];HIV Outbreak in Southeastern Indiana. Available at: https://secure.in.gov/isdh/26649.htm.
- 27.Armstrong GL, Wasley A, Simard EP, et al. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144(10):705–14. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Notes from the field: Hepatitis C virus infections among young adults - rural Wisconsin, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:358. [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Hepatitis C virus infection among adolescents and young adults: Massachusetts, 2002–2009. MMWR Morb Mortal Wkly Rep. 2011;60:537–41. [PubMed] [Google Scholar]
- 30.Keyes KM, Cerda M, Brady JE, et al. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104(2):e52–9. doi: 10.2105/AJPH.2013.301709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.United States Department of Agriculture. Rural America at a Glance. United States Department of Agriculture; 2014. [Accessed 18 February 2016]. Available at: http://www.ers.usda.gov/media/1697681/eb26.pdf. [Google Scholar]
- 32.Stein BD, Gordon AJ, Dick AW, et al. Supply of buprenorphine waivered physicians: the influence of state policies. J Subst Abuse Treat. 2015;48(1):104–11. doi: 10.1016/j.jsat.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brandeis University, PDMP Center of Excellence. [Accessed 16 September 2015];Prescription Drug Monitoring Program Center of Excellence. Available at: http://pdmpexcellence.org/content/coe-prescription-behavior-surveillance-system-0.
- 34.Centers for Disease Control and Prevention. Outbreak of recent HIV and HCV infections among persons who inject drugs. [Accessed 6 November 2015];Health Alert Network. 2015 Available at http://emergency.cdc.gov/han/han00377.asp.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.