Abstract
For the treatment of HIV, compliance in regard to appointment attendance and medication usage is critical. Various methods have been attempted to increased HIV care compliance, and a method that has inspired many published studies is text message reminders. We conducted a meta-analysis of the literature from inception through May 2016 using the following databases: Pubmed, Embase, CINAHL, Web of Science, and Cochrane. Examples of terms used in the search included exploded versions of “HIV, “AIDS”, “cell phone”, “SMS”, “text message”, “reminder”. After abstract and manuscript review, articles were discussed with co-author and included based on consensus. We excluded qualitative analyses, observational studies without an intervention, and studies without a control or pre-intervention group. We used random-effects models to calculate odds ratios (OR) and standardized mean differences (SMD) for the text message intervention. Thirty-four unique studies were found and included in the meta-analysis. For the 7 articles relating to non-attendance, text message reminders significantly reduced the rates of non-attendance (OR, 0.66; 95% CI, 0.48–0.92; P= .01; I2=52%). For the 20 articles on drug adherence, text message reminders significantly increased adherence (SMD, 0.87; 95% CI, 0.06–1.68; P=.04; I2=99%). For the 11 articles with physiologic measures (CD4 count or viral load), text message reminders led to significant improvement (SMD, 1.53; 95% CI, 0.52–2.55; P=.003; I2=99%). This meta-analysis reveals that text message reminders are a promising intervention that can be used to increase HIV care compliance when logistically feasible. Further study should focus on which populations benefit the most from this intervention, and successful implementers could create an established technological infrastructure for other clinics to adopt when seeking to boost compliance.
Keywords: HIV, AIDS, compliance, text message, cell phones
INTRODUCTION
In the treatment of HIV infections, appointment attendance and medication adherence is critical to good control of this disease. Various methods have been attempted to increase compliance, including the use of text message reminders, which has had a number of published studies to evaluate its usefulness. Studies in urban HIV clinics in the U.S. have found that the vast majority of patients own mobile phones and would use them to enhance medication adherence (Miller & Himelhoch, 2013). Patients and providers both have noted some of the benefits of text message reminders, such as their ease of use and the ability to personalize messages and their timing (Baranoski et al., 2014).
In impoverished areas of the world, achieving HIV-related compliance can be even more difficult. At an established HIV program in Kibera, Nairobi, one of Africa’s largest informal urban settlements, more than one third of patients were non-adherent to their treatment regimen (Unge et al., 2010). Therefore, looking to improve adherence rates, researchers have done research on text message reminders in resource-constrained settings. In studies in Peru (Curioso & Kurth, 2007; Menacho, Blas, Alva, & Roberto Orellana, 2013) and Botswana (Reid et al., 2014), patients viewed HIV-related health promotion via communication technology positively. Furthermore, in a 2010 study of an antiretroviral therapy clinic in Durban, South Africa, 81% of patients owned a cell phone, and 96% of respondents were willing to be contacted by the clinic via text messaging (Crankshaw et al., 2010). A survey of secondary school students in Mbarara, Uganda found that 61% of those who owned a cell phone said they would access a text messaging-based HIV prevention program if it were available (Mitchell, Bull, Kiwanuka, & Ybarra, 2011). In Asia, studies have found similar results. Across multiple HIV clinics in Vietnam, 85% of patients used mobile phones, 79% found cell phone reminders an effective adherence aid, and 64 % expressed willingness-to-use the service with an average willingness-to-pay of $2.50 per month (Tran & Houston, 2012). In a cross-sectional survey of 801 Chinese people living with HIV, 88% of the participants owned mobile phones and 80% felt daily text reminders to take medication would be helpful (Xiao et al., 2014).
Text message reminders have been effective in a number of fields unrelated to HIV care: antenatal and postnatal care (Watterson, Walsh, & Madeka, 2015), contraception (Halpern, Lopez, Grimes, Stockton, & Gallo, 2013), immunizations (Odone et al., 2015), breast cancer screening (Kerrison, Shukla, Cunningham, Oyebode, & Friedman, 2015), smoking cessation (Vodopivec-Jamsek, de Jongh, Gurol-Urganci, Atun, & Car, 2012), sunscreen use (Armstrong et al., 2009), and some asthma and diabetes outcomes (de Jongh, Gurol-Urganci, Vodopivec-Jamsek, Car, & Atun, 2012). For HIV care, a number of studies have accumulated that seek to quantify the benefit of text message reminders. Our current paper seeks to identify and amalgamate all HIV compliance-related text messaging studies – spanning a range of study types – into an up-to-date and comprehensive set of meta-analyses. Our hypothesis was that text message reminders would improve compliance in all aspects of HIV care.
METHODS
No human participants were involved in this study and only previously published literature was included, thus the project was exempt from requirements for human subjects research review.
Search Strategy
We conducted a meta-analysis of the literature using the following databases from inception thru May 2016: PubMed (MEDLINE), EMBASE, CINAHL, Web of Science, and Cochrane. Studies in any language that investigated text message reminders for HIV care were available for inclusion. Terms used in the search included exploded versions of “HIV, “AIDS”, “cell phone”, “SMS”, “text message”, “reminder”. For example for PubMed, the search algorithm was “(HIV Infections[MeSH] OR HIV[MeSH] OR hiv[tiab] OR hiv-1[tiab] OR hiv-2*[tiab] OR hiv1[tiab] OR hiv2[tiab] OR hiv infect*[tiab] OR human immunodeficiency virus[tiab] OR human immune deficiency virus[tiab] OR human immunodeficiency virus[tiab] OR human immune-deficiency virus[tiab] OR (human immun*) OR (deficiency virus[tiab])) OR acquired immunodeficiency syndromes[tiab] OR acquired immune deficiency syndrome[tiab] OR acquired immunodeficiency syndrome[tiab] OR acquired immune-deficiency syndrome[tiab] OR (acquired immun*) OR (deficiency syndrome[tiab]) OR HIV[tiab] OR HIV/AIDS[tiab] OR HIV-infected[tiab] OR HIV[title] OR HIV/AIDS[title] OR HIV-infected[title]) AND (”Cellular Phone“[Mesh] OR telephone[tiab] OR phone[tiab] OR mobile[tiab] OR cellphone[tiab] OR ”cell phone"[tiab] OR sms[tiab] OR text*[ti] OR messag*[ti] OR remind*[ti]).” In order to capture any missed studies, we hand-searched the references from the discovered studies and reviews.
Study Selection
In our search for studies on text message reminders for HIV-related compliance, we excluded studies centered on qualitative measures; observations without an intervention; support groups or use of SMS messaging to connect with other patients or a physician; analyses without a control group or pre-intervention group; educational text messages; programmable medication reminder devices; texting for test result delivery; phone call interventions not in conjunction with text messaging. Prior to data analysis, we chose to include articles on text messaging via a pager because the intervention still consisted of a text reminder via a portable device. After abstract and manuscript review, all articles for potential inclusion were discussed amongst the co-authors and included based on consensus. Figure 1 summarizes the selection of articles used in this study.
Figure 1.
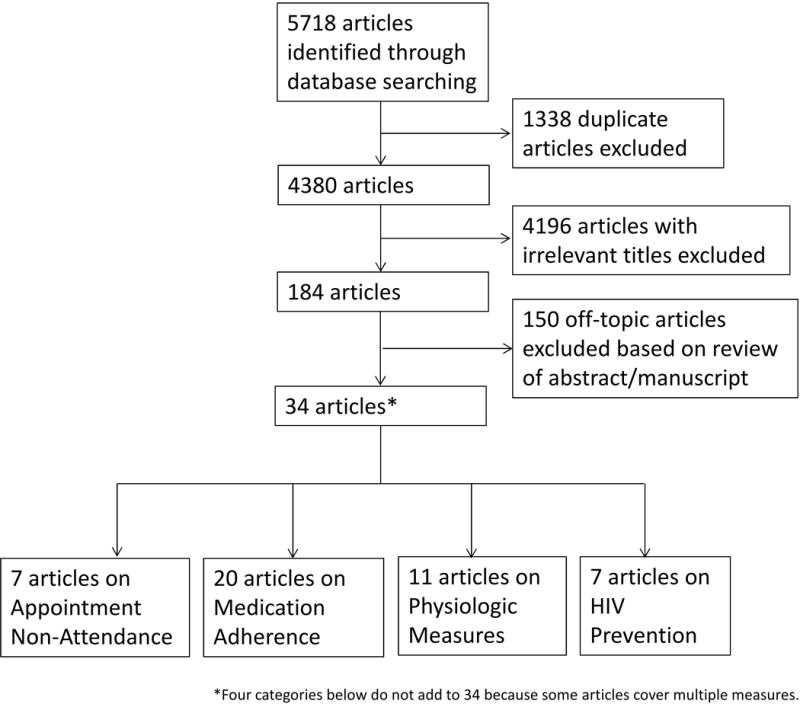
Search protocol flow chart
*Four categories below do not add to 34 because some articles cover multiple measures.
Data Extraction
For each study, we extracted outcome data to calculate a standardized mean difference or odds ratio. When possible, we used intention-to-treat data. We classified the study focus into four categories: Appointment Non-Attendance, Medication Adherence, Physiologic Measures, and HIV Prevention (which was then divided into Appointment Non-Attendance and Avoiding High-Risk Sexual Behavior). Points specific to the extraction of data from each study is included as a Supplemental Table.
Statistical Analyses
We generated meta-analytic estimates of intervention effect using random-effects models. Effect sizes were calculated as standardized mean difference (SMD) or odds ratios (OR). Analyses were performed using Review Manager (RevMan) version 5.2 software (Cochrane Collaboration). We measured heterogeneity for each outcome across studies using the I2 test. When the data required to calculate a standard deviation (SD) were not included in an article, we requested it from the study’s authors, and when information was not forthcoming, imputation of the mean SD of the group for that particular variable was utilized. Imputation of more than 2 SDs was not required for any analysis. When a study produced binary data (e.g. number who attended vs did not attend), the data was converted to a continuous percentage and the SD was estimated assuming a binomial distribution. An aggregate effect size was calculated for each group of articles. No subgroup analyses were planned a priori.
RESULTS
The results of the search strategy are shown in Figure 1 and all studies are characterized in Table 1. The search identified a total of 5,718 articles from all databases. Articles were systematically excluded: 1,338 duplicates, 4,196 articles with irrelevant titles, 150 off-topic articles based on review of the abstract or manuscript. This left 34 unique studies to be included in the meta-analysis. Seven articles contained data on “Appointment Non-Attendance,” 20 articles on “Medication Adherence,” 11 articles on “Physiologic Measures”, 7 articles on “HIV Prevention” (5 with “Did Not Attend Rates” and 2 on “Avoidance of High-Risk Sexual Behavior”). Some studies contained data on multiple outcome measures and thus fit into two of the above categories for meta-analysis.
Table 1.
| Author | Year | Study Type |
Location | Study Population (HIV-positive) | Study Duration |
Intervention | Experimental # | Control # |
|---|---|---|---|---|---|---|---|---|
| Non-Attendance | ||||||||
| Bigna et al | 2014 | RCT | Cameroon | Carers of children with or exposed to HIV | 1 appt | Text message | 60 | 61 |
| Farmer et al | 2014 | Pre-Post | London | Clinic patients | 1 year | Text message | 951 | 822 |
| Ingersoll et al | 2015 | RCT | USA: VA | People with drug use & recent ART nonadherence | 12 weeks | Text message | 33 | 30 |
| Kliner et al | 2013 | Pre-Post | Swaziland | Newly-diagnosed and obtaining CD4 results | 1 appt | Text message | 162 | 297 |
| Norton et al | 2014 | RCT | USA: NC | Clinic patients | 1 appt | Text message | 25 | 27 |
| Odeny et al | 2014 | RCT | Kenya | Pregnant women | 1 appt | Text message | 194 | 187 |
| Perron et al | 2010 | RCT | Switzerland | Clinic patients | 1 appt | Call ± text | 150 | 153 |
| Medication Adherence | ||||||||
| Ammassari et al | 2011 | Pre-Post | Italy | Adults with suboptimal adherence | 9 months | Text message | 106 | 145 |
| da Costa et al | 2012 | RCT | Brazil | Brazilian women | 4 months | Text message | 8 | 13 |
| Dowshen et al | 2012 | Pre-Post | USA: PA | Youths on ART with poor adherence | 24 weeks | Text message | 21 | 21 |
| Garofalo et al | 2015 | RCT | USA: IL | Youths and young adults with poor adherence | 6 months | Text message | 43 | 49 |
| Haberer et al | 2016 | RCT | Uganda | Individuals initiating ART | 9 months | Text message | 21 | 21 |
| Hardy et al | 2011 | Pre-Post | USA: MA | Adults receiving HIV primary care | 6 weeks | Text message | 10 | 10 |
| Ingersoll et al | 2015 | RCT | USA: VA | People with drug use & recent ART nonadherence | 12 weeks | Text message | 33 | 30 |
| Kalichman | 2016 | RCT | USA: GA | Adults with poor adherence | 12 months | Text message | 150 | 151 |
| Lester et al | 2010 | RCT | Kenya | Patients initiating ART | 12 months | Text message | 273 | 265 |
| Lewis et al | 2012 | Pre-Post | USA | MSM aged ≥ 25 | 3 months | Text message | 18 | 18 |
| Maduka et al | 2012 | RCT | Nigeria | Patients with a history of non-adherence | 4 months | Text + counseling | 52 | 52 |
| Mbuabaw et al | 2012 | RCT | Cameroon | Adults aged ≥ 21 on ART | 6 months | Text message | 101 | 99 |
| Moore et al | 2014 | RCT | USA: CA | Patients with co-occurring bipolar disorder | 30 days | Text message | 25 | 25 |
| Orrell et al | 2015 | RCT | South Africa | ART-naïve patients | 48 weeks | Text message | 115 | 115 |
| Pop-Eleches et al | 2011 | RCT | Kenya | Adults who had initiated ART within 3 months | 48 weeks | Text message | 289 | 139 |
| Rodrigues et al | 2012 | Pre-Post | India | Patients on ART | 6 months | Pictorial text + call | 141 | 141 |
| Sabin et al | 2015 | RCT | China | Adults on ART | 6 months | Text message | 63 | 56 |
| Safren et al | 2010 | RCT | USA: MA | Patients with poor adherence | 2 weeks | Pager text message | 19 | 25 |
| Shet et al | 2014 | RCT | India | Adult, ART naïve patients | 2 years | Pictorial text + call | 300 | 299 |
| Simoni et al | 2009 | RCT | USA: WA | Patients at a public HIV clinic | 3 months | Pager text message | 56 | 57 |
| Physiologic Measures | ||||||||
| Ammassari et al | 2011 | Pre-Post | Italy | Adults with suboptimal adherence | 9 months | Text message | 123 | 123 |
| Dowshen et al | 2012 | Pre-Post | USA: PA | Youths on ART with documented poor adherence | 24 weeks | Text message | 21 | 21 |
| Garofalo et al | 2015 | RCT | USA: IL | Youths and young adults with poor adherence | 6 months | Text message | 20 | 23 |
| Kalichman et al | 2016 | RCT | USA: GA | Adults with poor adherence | 12 months | Text message | 110 | 98 |
| Lester et al | 2010 | RCT | Kenya | Adults initiating ART | 12 months | Text message | 273 | 265 |
| Lewis et al | 2012 | Pre-Post | USA | MSM aged ≥ 25 | 3 months | Text message | 37 | 37 |
| Maduka et al | 2012 | RCT | Nigeria | Patients with a history of non-adherence | 4 months | Text message | 52 | 52 |
| Orrell et al | 2015 | RCT | South Africa | ART-naïve patients | 48 weeks | Text message | 115 | 115 |
| Rana et al | 2016 | Pre-Post | USA: RI | Adults with higher risk of loss-to-follow-up | 6 months | Text message | 32 | 32 |
| Shet et al | 2014 | RCT | India | Adult, ART naïve patients | 2 years | Pictorial text + call | 315 | 316 |
| Simoni et al | 2009 | RCT | USA: WA | Patients at a public HIV clinic | 3 months | Pager text message | 56 | 57 |
| Prevention - Non-attendance | ||||||||
| Bourne et al | 2011 | Pre-Post | Australia | HIV-negative MSM categorized as high-risk | 1 testing appt | Text message | 1798 | 1753 |
| Burton et al | 2013 | Pre-Post | UK | HIV-negative patients categorized as high-risk | 1 testing appt | Text message | 274 | 266 |
| Mugo et al | 2016 | RCT | Kenya | HIV-negative patients | 1 testing appt | Text + call | 199 | 207 |
| Nyatsanza et al | 2015 | Pre-Post | UK | HIV-negative patients categorized as high-risk | 1 testing appt | Personalized text | 266 | 273 |
| Odeny et al | 2012 | RCT | Kenya | HIV-positive males with recent circumcisions | 1 testing appt | Text message | 592 | 596 |
| Prevention - Avoiding High-Risk Behaviors | ||||||||
| Odeny et al | 2014 | RCT | Kenya | HIV-positive males with recent circumcisions | 6 weeks | Text message | 491 | 493 |
| Reback et al | 2012 | Pre-Post | USA: CA | HIV-negative methamphetamine-using MSM | 2 weeks | Text message | 48 | 52 |
For the 7 articles relating to “Appointment Non-Attendance,” 5 were RCTs and 2 were pre-post studies. Altogether, there were 1,608 experimental subjects and 1,607 control subjects (Figure 2). Overall, text message reminders significantly reduced the rates of non-attendance (OR, 0.66; 95% CI, 0.48–0.92; P= .01; I2=52%; Figure 2). For the 20 articles on “Medication Adherence,” 14 were RCTs and 6 were pre-post studies. Altogether, there were 1,844 experimental subjects and 1,731 control subjects (Figure 3). Overall, text message reminders significantly increased medication adherence (SMD, 0.87; 95% CI, 0.06–1.68; P=.04; I2=99%; Figure 3). For the 11 articles with “Physiologic Measures,” 7 were RCTs and 4 were pre-post studies. Altogether, there were 1,154 experimental subjects and 1,139 control subjects (Figure 4). Overall, text message reminders led to improvement in the physiologic measures (SMD, 1.53; 95% CI, 0.52–2.55; P=.003; I2=99%; Figure 4). For the 5 articles relating to “HIV Prevention – Appointment Non-Attendance,” 2 were RCTs and 3 were pre-post studies. Altogether, there were 3,129 experimental subjects and 3,095 control subjects. Overall, text message reminders significantly reduced the rates of non-attendance (OR, 0.63; 95% CI, 0.47–0.84; P= .002; I2=83%; Figure 5). For the 2 articles relating to “HIV Prevention – Avoidance of Certain High-Risk Sexual Behavior,” 1 was an RCT and 1 was a pre-post study. Altogether, there were 539 experimental subjects and 545 control subjects. Overall, text message reminders did not significantly reduce the rates of high-risk sexual acts (OR, 0.66; 95% CI, 0.19–2.35; P= .52; I2=86%; Figure 6).
Figure 2.
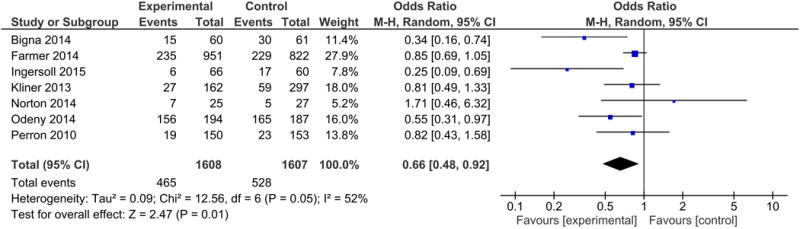
Forest plot for the Appointment Non-Attendance Meta-Analysis
Figure 3.
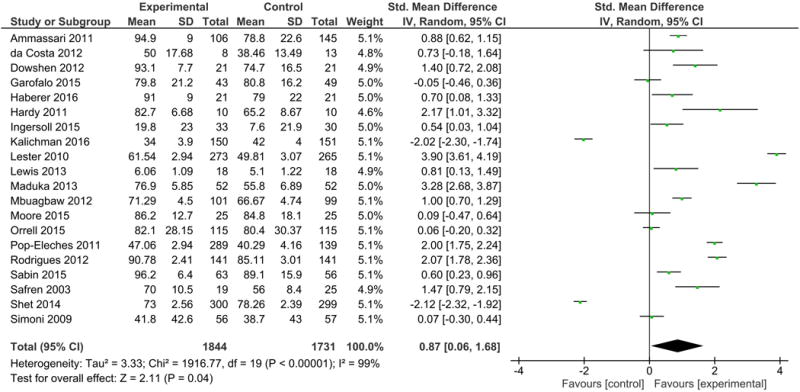
Forest plot for the Medication Adherence Meta-Analysis
Figure 4.
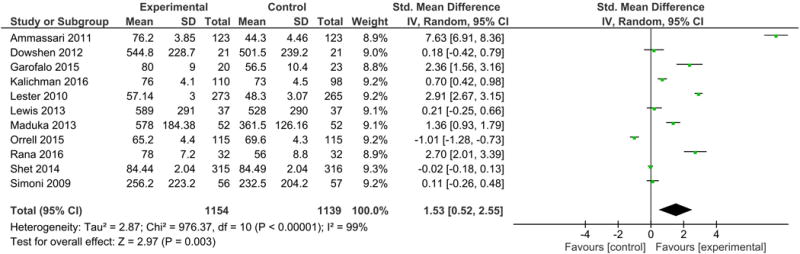
Forest plot for the Physiologic Measures Meta-Analysis
Figure 5.
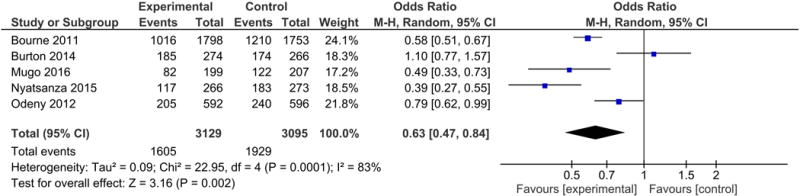
Forest plot for the HIV Prevention – Appointment Non-Attendance
Figure 6.
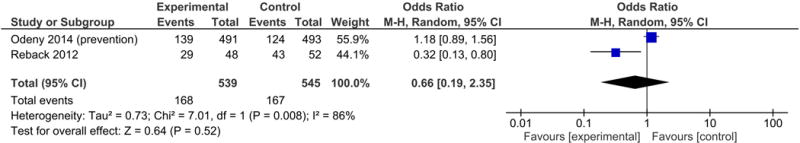
Forest plot for the HIV Prevention – Avoidance of Certain High-Risk Sexual Behavior
DISCUSSION
This meta-analysis reveals that text message reminders are a valuable tool to increase HIV-related compliance. We found significant benefits in regard to non-attendance, medication adherence, and physiologic measures. For both of the HIV primary prevention meta-analyses, decreases in non-attendance and high-risk sexual behaviors were present (however, only the former was statistically significant).
Our findings regarding the effectiveness of text message reminders are consistent with the meta-analyses discussed in the Introduction showing increased compliance with text message reminders used in other healthcare settings. Our meta-analysis focused on all aspects of HIV care that have been studied in relation to text messaging, which includes studies beyond RCTs. Moreover, it has been updated with studies through mid-2016. One advantage we see in this study is that previous systematic reviews, while comprehensive in scope, did not involve statistical synthesis of the data and instead drew more subjective conclusions. For example, a 2013 systematic review on the use of mobile phone messaging for HIV infection prevention, treatment, and care and concluded that there was “limited evidence on the effectiveness of mobile phone messaging for HIV care” (van Velthoven, Brusamento, Majeed, & Car, 2013). With the inclusion of more recent published reports in this meta-analysis, it appears that there is sufficient evidence on the effectiveness of text messaging for HIV care.
One of the limitations of this meta-analysis is the high rates of heterogeneity within each analysis. This is likely secondary to the multiple types of studies included, the various different study populations, and the slightly different interventions (e.g. timing of text messages). To reduce the chance of type 1 error from multiple comparisons, we did not do further meta-analyses within subgroups. With the addition of more studies going forward, future analyses may limit their a priori hypotheses to specific populations or types of studies, and this would likely lower the high heterogeneity levels we found. Another limitation of this analysis is that it gave the same weight to an RCT as a non-RCT. We considered this as acceptable since we believed that it was outweighed by greater inclusivity and increasing the number of data points for analysis. In addition, the RCT studies tended to be more robust with larger sample sizes, so they naturally received more weight than a smaller non-RCT.
Given the improvements in compliance seen in this meta-analysis, the use of text messaging reminders should be pursued when feasible in HIV clinics. The populations in the analyzed studies varied significantly, and the future studies should delve deeper into who benefits the most and least from text message interventions within one population. Until further characterization is possible, it seems likely that any clinic with high rates of noncompliance with HIV care would benefit from text message reminders. With the near-ubiquity of mobile phones worldwide and now smartphones in the developed world, implementation of text message interventions is a natural next step in using technology for health maintenance, especially with younger patients, who typically feel the most comfortable with new technology. In the near future, with the increasing prevalence of wearable devices, reminders via these devices may become alternatives to cell phone reminders.
Text message intervention studies have reported varying costs, on the scale of hundreds to thousands of dollars for initial set-up of a reminder system (van Velthoven et al., 2013). A 2014 study in South India determined the cost of implementing a text reminder system to be $1.27-$1.57 per patient per year (Rodrigues, Bogg, Shet, Kumar, & De Costa, 2014). However, once the texting system was instituted, maintenance costs could be as low as $0.005 per text message (Kunutsor et al., 2010). If systems are established on a large scale in a country, perhaps by a central health agency, costs for a new clinic to implement text message reminders would be minimal. Moreover, multiple websites advertise free services for setting up individual or group text reminders. However, concerns regarding HIPAA, confidentiality and other privacy concerns would need to be strongly considered before such services could be used, especially with sensitive information such as HIV status.
Conclusion
It appears that text message reminders are a promising intervention that should be used to increase HIV care compliance when feasible. Further study should focus on which populations benefit the most from this intervention, and adoption of this intervention would benefit from a central infrastructure created by an organization such as the government or other public health organization, thus enabling easier adoption of text message reminders in clinics with poor compliance.
Supplementary Material
Acknowledgments
This research was supported by the Intramural Research Program of the National Institutes of Health (NIH), National Library of Medicine (NLM) and Lister Hill National Center for Biomedical Communications (LHNCBC).
Sources of Financial Support: None.
Footnotes
Institution Where Research Was Conducted: National Institutes of Health
Disclaimer
The views and opinions of the authors expressed herein do not necessarily state or reflect those of the National Library of Medicine, National Institutes of Health or the US Department of Health and Human Services.
Declarations of Interest: The authors report no conflicts of interest
Contributor Information
Jonathan E. Mayer, Department of Medicine, Johns Hopkins Bayview Medical Center, Johns Hopkins University School of Medicine, 4940 Eastern Ave, Baltimore, MD, USA 21224-2780, 407-267-8642.
Paul Fontelo, Lister Hill National Center for Biomedical Communications, National Library of Medicine, National Institutes of Health, Bethesda, MD, USA 20892, 301-435-3265.
References
- Armstrong AW, Watson AJ, Makredes M, Frangos JE, Kimball AB, Kvedar JC. Text-message reminders to improve sunscreen use: a randomized, controlled trial using electronic monitoring. Arch Dermatol. 2009;145(11):1230–1236. doi: 10.1001/archdermatol.2009.269. [DOI] [PubMed] [Google Scholar]
- Baranoski AS, Meuser E, Hardy H, Closson EF, Mimiaga MJ, Safren SA, Kumar VS. Patient and provider perspectives on cellular phone-based technology to improve HIV treatment adherence. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv. 2014;26(1):26–32. doi: 10.1080/09540121.2013.802282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crankshaw T, Corless IB, Giddy J, Nicholas PK, Eichbaum Q, Butler LM. Exploring the Patterns of Use and the Feasibility of Using Cellular Phones for Clinic Appointment Reminders and Adherence Messages in an Antiretroviral Treatment Clinic, Durban, South Africa. AIDS Patient Care & STDs. 2010;24(11):729–734. doi: 10.1089/apc.2010.0146. [DOI] [PubMed] [Google Scholar]
- Curioso WH, Kurth AE. Access, use and perceptions regarding Internet, cell phones and PDAs as a means for health promotion for people living with HIV in Peru. BMC Med Inform Decis Mak. 2007;7 doi: 10.1186/1472-6947-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev. 2012;12:CD007459. doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern V, Lopez LM, Grimes DA, Stockton LL, Gallo MF. Strategies to improve adherence and acceptability of hormonal methods of contraception. Cochrane Database Syst Rev. 2013;(10):CD004317. doi: 10.1002/14651858.CD004317.pub4. [DOI] [PubMed] [Google Scholar]
- Kerrison RS, Shukla H, Cunningham D, Oyebode O, Friedman E. Text-message reminders increase uptake of routine breast screening appointments: a randomised controlled trial in a hard-to-reach population. Br J Cancer. 2015;112(6):1005–1010. doi: 10.1038/bjc.2015.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunutsor S, Walley J, Katabira E, Muchuro S, Balidawa H, Namagala E, Ikoona E. Using mobile phones to improve clinic attendance amongst an antiretroviral treatment cohort in rural Uganda: a cross-sectional and prospective study. AIDS Behav. 2010;14(6):1347–1352. doi: 10.1007/s10461-010-9780-2. [DOI] [PubMed] [Google Scholar]
- Menacho LA, Blas MM, Alva IE, Roberto Orellana E. Short Text Messages to Motivate HIV Testing Among Men Who have Sex with Men: A Qualitative Study in Lima, Peru. Open AIDS J. 2013;7:1–6. doi: 10.2174/1874613601307010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller CW, Himelhoch S. Acceptability of Mobile Phone Technology for Medication Adherence Interventions among HIV-Positive Patients at an Urban Clinic. AIDS Res Treat. 2013;2013:670525. doi: 10.1155/2013/670525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell KJ, Bull S, Kiwanuka J, Ybarra ML. Cell phone usage among adolescents in Uganda: acceptability for relaying health information. Health Educ Res. 2011;26(5):770–781. doi: 10.1093/her/cyr022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odone A, Ferrari A, Spagnoli F, Visciarelli S, Shefer A, Pasquarella C, Signorelli C. Effectiveness of interventions that apply new media to improve vaccine uptake and vaccine coverage. Hum Vaccin Immunother. 2015;11(1):72–82. doi: 10.4161/hv.34313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid MJ, Dhar SI, Cary M, Liang P, Thompson J, Gabaitiri L, Steenhoff AP. Opinions and attitudes of participants in a randomized controlled trial examining the efficacy of SMS reminders to enhance antiretroviral adherence: a cross-sectional survey. J Acquir Immune Defic Syndr. 2014;65(2):e86–88. doi: 10.1097/QAI.0b013e3182a9c72b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues R, Bogg L, Shet A, Kumar DS, De Costa A. Mobile phones to support adherence to antiretroviral therapy: what would it cost the Indian National AIDS Control Programme? J Int AIDS Soc. 2014;17 doi: 10.7448/ias.17.1.19036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran BX, Houston S. Mobile phone-based antiretroviral adherence support in Vietnam: feasibility, patient’s preference, and willingness-to-pay. AIDS Behav. 2012;16(7):1988–1992. doi: 10.1007/s10461-012-0271-5. [DOI] [PubMed] [Google Scholar]
- Unge C, Sodergard B, Marrone G, Thorson A, Lukhwaro A, Carter J, Ekstrom AM. Long-term adherence to antiretroviral treatment and program drop-out in a high-risk urban setting in sub-Saharan Africa: a prospective cohort study. PLoS One. 2010;5(10):e13613. doi: 10.1371/journal.pone.0013613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Velthoven M, Brusamento S, Majeed A, Car J. Scope and effectiveness of mobile phone messaging for HIV/AIDS care: A systematic review. Psychology Health & Medicine. 2013;18(2):182–202. doi: 10.1080/13548506.2012.701310. [DOI] [PubMed] [Google Scholar]
- Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev. 2012;12:CD007457. doi: 10.1002/14651858.CD007457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watterson JL, Walsh J, Madeka I. Using mHealth to Improve Usage of Antenatal Care, Postnatal Care, and Immunization: A Systematic Review of the Literature. Biomed Res Int. 2015;2015:153402. doi: 10.1155/2015/153402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y, Ji G, Tian C, Li H, Biao W, Hu Z. Acceptability and factors associated with willingness to receive short messages for improving antiretroviral therapy adherence in China. AIDS Care. 2014;26(8):952–958. doi: 10.1080/09540121.2013.869540. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


