Abstract
Rationale
Reductions in cue-induced craving and subjective response to drugs of abuse are commonly used as initial outcome measures when testing novel medications for the treatment of addiction. Yet neither the relationship between these two measures at the individual level nor the moderating effects of pharmacotherapies on this relationship has been examined.
Objective
This secondary data analysis sought to examine 1) the predictive relationship between cue-induced craving and subsequent acute subjective response to methamphetamine (MA) and 2) whether the opioid-receptor antagonist naltrexone moderated this association in a sample of non-treatment-seeking individuals who met DSM-IV criteria for MA use disorder (abuse or dependence).
Methods
Participants (N = 30) completed two four-day medication regimens (oral naltrexone 50-mg or placebo, in a randomized, counterbalanced, and double-blind fashion). On day four of each medication regimen, participants completed a cue-reactivity paradigm followed by intravenous MA administration. Methamphetamine craving was assessed after the cue-reactivity paradigm, and subjective response to MA was assessed during MA infusion.
Results
Cue-induced craving for MA was positively associated with post-infusion subjective MA effects, including positive (i.e., stimulation, good effects, feel drug, high), negative (i.e., anxious and depressed), and craving-related (i.e., want more, would like access to drug, crave) responses. Naltrexone, vs. placebo, significantly reduced the association between cue-induced craving and positive subjective response to MA.
Conclusions
The findings indicate that naltrexone moderates the predictive relationship between cue-induced craving and positive subjective effects of MA, thereby suggesting a behavioral mechanism by which naltrexone may be efficacious in treating MA use disorder.
Keywords: Methamphetamine, Naltrexone, Craving, Subjective Response
Introduction
Recent studies have indicated that naltrexone, an opioid receptor antagonist that is approved for heroin and alcohol use disorders, may be a promising pharmacotherapy for stimulant use disorders, including methamphetamine (MA) use disorder. In a clinical trial, naltrexone treatment reduced amphetamine use and produced greater abstinence rates compared with placebo in a sample of amphetamine-dependent individuals (Jayaram-Lindström et al. 2008a), although a smaller combined pharmacotherapy study did not replicate these results in MA users (Grant et al. 2010). Laboratory studies have identified potential behavioral mechanisms for the observed treatment efficacy of naltrexone. For example, naltrexone reduces tonic amphetamine craving and subjective response in amphetamine-dependent patients (Jayaram-Lindström et al. 2004; Jayaram-Lindström et al. 2008b) and decreases cocaine craving, but not positive subjective effects, during acute cocaine administration to stimulant users (Comer et al. 2013). We have observed that naltrexone reduces both MA cue-induced craving and the acute subjective effects of MA, such as stimulation and craving, during controlled MA administration (Ray et al. 2015). Taken together, these results suggest that naltrexone may be an effective treatment for MA use disorder through its reduction in tonic and cue-induced craving as well as by altering subjective drug effects. However, given the limited number of studies that have investigated naltrexone specifically for MA use disorder and the pressing need for pharmacological treatments, additional studies are warranted to further elucidate the biobehavioral mechanisms underlying the potential efficacy of naltrexone for MA use disorder.
Situational increases in drug craving are often proximal to drug use in the laboratory and the real world settings and have been identified has one of the strongest predictors of lapse and relapse during quit attempts (Shiffman et al. 1996; Shiffman and Waters 2004; Leeman et al. 2009; Epstein DH et al. 2009; Preston and Epstein 2011; for review, Sinha 2013). For example, in cocaine- and MA-dependent individuals, the magnitude of craving and craving-related beliefs are predictive of relapse during treatment (Hartz et al. 2001; Rohsenow et al. 2007; Paliwal et al. 2008; Galloway and Singleton 2009; Lee et al. 2010). Further, tonic craving for MA has been observed at least five weeks into abstinence and appears to render users particularly vulnerable to relapse within this period (Hartz et al. 2001; Galloway and Singleton 2009; Zorick et al. 2010). Accordingly, craving has been advanced as a surrogate marker of MA dependence (Galloway and Singleton 2009), and a reduction in drug craving represents a common goal in addiction treatment (Pavlick et al. 2009). Although tonic MA decreases as a function of abstinence duration (Hartz et al. 2001; Galloway and Singleton 2009; Wang et al. 2013), cue-induced MA craving has been observed to gradually increase at least three months into abstinence (Wang et al. 2013). A prolonged and sensitized responsivity to drug-related stimuli is critical in the etiology and maintenance of addiction, as highlighted by the incentive sensitization theory (Robinson and Berridge 1993; Robinson and Berridge 2001) and recent studies of individual differences in conditioned cue responsivity in rats (Flagel et al. 2009; Robinson and Flagel 2009). Thus, as discussed elsewhere (Sinha 2013; Courtney and Ray 2014), a reduction in cue-induced craving may be a primary indicator of the potential efficacy of a medication for MA use disorder.
Similar to drug craving, subjective drug effects are related to subsequent patterns of use in the laboratory and real world settings, as well as the development and maintenance of substance use disorders (e.g., Shiffman et al. 2006; King AC et al. 2011; for review, de Wit and Phillips 2012). Across most drugs of abuse, including stimulants, increases in positive mood and stimulation are positively associated with drug choice and self-administration in the laboratory (Chait 1993; de Wit and Doty 1994; Tancer and Johanson 2003; Corbin et al. 2007); conversely, greater subjective experiences of aversive drug effects (e.g., anxiety, sedation, depression, etc.) or reduced stimulation are associated with a decrease in these outcome measures (De Wit et al. 1989; Chutuape and De Wit 1994). Although the relationship between subjective response to MA and subsequent drug use or abuse has not been investigated, retrospective reports in cocaine users have indicated that initial positive subjective effects (e.g., liking, wanting, alertness) are associated with higher frequency of future use and development of abuse and dependence more so than negative subjective effects (Davidson et al. 1993; Grant et al. 2005; Lambert et al. 2006). On the basis of such findings, reductions of the pleasurable or stimulatory effects of drugs of abuse have been advanced as markers of efficacy in medication development for addiction (Roche and Ray 2015; Ray et al. 2016).
Nonetheless, the utility of subjective response to acute drug administration as an outcome measure in medication development studies for stimulant use disorders has been debated (Comer et al. 2008; Haney 2009). As discussed in multiple reviews (Haney and Spealman 2008; Comer et al. 2008), the dose at which a medication effectively reduces positive subjective responses to cocaine is not necessarily sufficient to reduce self-administration in the laboratory or drug use in a clinical-trial setting. One possible explanation for this incongruity is that the subjective effects of a drug of abuse show high interindividual variability and may be affected by numerous variables (Ray et al. 2016), including stage and severity of substance use disorder (Bujarski and Ray 2014; Bujarski et al. 2015), expectancy of drug effects (Kirk et al. 1998; Volkow et al. 2003; Mitchell et al.), motives for use (Wardell et al. 2016), psychological and physiological state (Chait 1993; Söderpalm and de Wit 2002; Söderpalm et al. 2003; Childs et al. 2011; Brkic et al. 2016), or a combination of these factors (Treloar et al. 2015). Thus, it may be more ecologically valid and clinically informative to test the effects of medications on subjective drug response during affective states, such as during levels of high stress or craving, that approximate naturalistic situations in which an individual may be at high risk for relapse.
While several studies have examined the relationship between stress responses and subjective drug effects (Söderpalm and de Wit 2002; Söderpalm et al. 2003; Childs et al. 2011; Brkic et al. 2016), to our knowledge no studies in humans have examined how magnitude of cue-induced craving may predict proximal and subsequent subjective response to a drug of abuse. In addition to the variability in subjective response described above, cue-reactivity is also thought to be highly variable between individuals and may differentially influence drug seeking behavior, acute response to drugs of abuse, and the development of addiction (Flagel et al. 2009; Robinson and Flagel 2009; Witteman et al. 2015). Therefore, in order to help clarify how naltrexone may affect cue-induced craving and subjective response, it may be necessary to characterize how naltrexone affects the relationship between these two variables at the subject level rather than examining each variable in isolation. The objective of this secondary data analysis of (Ray et al. 2015) was to examine 1) the predictive relationship between cue-induced craving and subsequent acute subjective response to MA at the individual level and 2) whether naltrexone moderated this association in a sample of 30 non-treatment-seeking individuals who meet criteria for MA use disorder.
Methods
The study protocol and all procedures were approved by the Institutional Review Board of the University of California, Los Angeles and were conducted in accordance with the Declaration of Helsinki. Detailed methodology of the general experimental and screening procedures has been published elsewhere (Ray et al. 2015) and is summarized here. Non-treatment-seeking MA users were recruited from the Los Angeles community via online and print advertisements. Inclusion criteria were: (1) meeting current DSM-IV criteria for MA abuse or dependence, (2) being fluent in English, (3) age between 18 and 50 years, (4) a MA-positive urine toxicology screen, and (5) agreeing to abstain from MA during the study as evidenced by a MA-negative urine upon each inpatient admission and every morning during their inpatient stay. Exclusion criteria were: (1) current treatment for MA use, a history of treatment in the 30 days before enrollment, and/or current desire for treatment for MA use, (2) a DSM-IV diagnosis of current (last 12 months) drug dependence (other than MA or nicotine), lifetime schizophrenia, bipolar disorder, any psychotic disorder, or current major depressive disorder with suicidal ideation, as indicated on the Structured Clinical Interview for DSM-IV (SCID; (First 2005), (3) current use of psychoactive drugs, other than marijuana, MA, and nicotine, verified by a toxicology screen, (4) significant medical problems as indicated by physical examination or laboratory tests (i.e. a blood chemistry panel and liver profile), (5) current use of medications that are contraindicated with the use of naltrexone (e.g., prescription opioids), (6) a positive test for pregnancy, are currently nursing, or refusing to use a reliable method of birth control, (7) cardiovascular abnormalities in EKG or vital signs as determined during the physical exam or inpatient stay, and (8) reporting intranasal as the only route of MA administration.
A total of 126 individuals (74% men) completed an initial in-person screening session, and 46 individuals completed a secondary medical screening with the study physician. Of the 126 who completed the in-person screen, 80 individuals did not proceed to or complete the medical screening for the following reasons: failure to produce a positive MA urine screen (n = 19), did not show up to physical exam (n = 18), unable to contact/no longer interested (n = 16), failure to meet eligibility criteria from the SCID (n = 14), currently using other psychoactive and/or contraindicated drugs (n = 9), only using MA intranasally (n = 2), outside of age range (n = 1), unable to successfully complete questionnaires and diagnostic interviews (n = 1). Of the 46 individuals who completed the medical screening, 14 did not complete an experimental session: eight were ruled ineligible for medical reasons, three were no longer interested/unable to be contacted, two demonstrated abnormal EKG/cardiovascular measures during the MA infusion, and one tested positive for MA during the inpatient stay prior to the MA infusion. Thirty-two individuals (75% male, mean age = 36.47 [SD = 8.68]) completed at least one experimental session; thirty of whom (73.3% male, mean age = 36.93 [SD = 8.77]) completed both experimental sessions: one while at naltrexone target dose and the other on matched placebo.
Screening Procedures
Interested individuals first called the laboratory and completed a telephone-screening interview. Eligible callers were then invited to the laboratory, where they received a full explanation of the study procedures and provided written, informed consent. At that time, participants were required to test positive for MA on a urine toxicology screen and have negative test results for all other drugs (excluding marijuana). Participants then completed questionnaires on demographics, drug use history, and psychological functioning. The following interviews were administered by trained masters-level clinicians: (a) the 30-day Timeline Follow-Back (TLFB) to capture daily MA use over the 30 days prior to the visit (Sobell et al. 1988) and (b) the SCID (First 2005) to assess criteria for MA dependence and abuse and to screen for exclusionary psychiatric diagnoses.
Participants deemed eligible following the in-person screening were invited to return to the laboratory to complete a physical exam with the study physician. Participants were required to provide a negative urine toxicology screen for all drugs (including MA, excluding marijuana) at this time. The physical exam consisted of clinical laboratory testing (i.e. a blood chemistry panel and liver profile) and an electrocardiogram (EKG).
Medication Administration and Inpatient Procedures
Participants who maintained eligibility after the physical exam were admitted to the UCLA Clinical and Translational Research Center (CTRC) inpatient unit on that same day and were randomized to take the first study medication (naltrexone or matched placebo). Participants ingested the study medication under staff supervision for four days and completed the first experimental session on medication day four, which consisted of a cue-reactivity paradigm followed by an intravenous (IV) MA administration two hours later. Participants were discharged from the unit on day five, and following a 7–14 day washout period, were re-admitted to the unit for their second inpatient stay, when they received the remaining study medication (naltrexone or placebo) in counterbalanced, randomized, and double-blind fashion. Following completion of the second inpatient stay, but prior to discharge on day five, participants received a motivational interview session that was delivered by a Master’s level clinician under the supervision of a licensed psychologist targeting reduction of MA use and promoting treatment-seeking. Naltrexone was titrated to minimize adverse events from 25-mg on day one to 50-mg doses on days two through four. Oral naltrexone was selected over the injectable formulation given the non-treatment-seeking nature of the sample and the need for a timely washout period that would support the feasibility of the crossover design. Participants received $40 for completing the in-person screening visit, $40 per inpatient day ($400 total), and $50 for each of the two experimental sessions. Participants who completed all parts of the study received a $100 bonus.
Cue Reactivity Paradigm & Measures
On day four of each admission, participants completed a guided cue-exposure protocol (Monti et al. 1987) modified for relevance to MA. The protocol included the presentation of two audio-recorded scripts (MA and water control), each approximately 5 minutes in length and delivered in a non-counterbalanced fashion (control first) to avoid potential carryover effects. The scripts instructed the participant to recall sensory and emotional memories related to their use of MA (or water). At various times during the cue exposure, the participant was instructed to handle physical cues (glass MA pipe or glass of water). All participants reported past experience with smoking MA, lending validity to the physical drug cue. After each standardized exposure, participants completed the MA Urge Questionnaire (MAUQ), which is an 8-item Likert-scale questionnaire assessing MA craving. Examples of the rated statements include: “All I want to do now is use methamphetamine,” and “I want to use methamphetamine so bad I can almost feel it.” An average of the items was computed. Internal reliability for this measure was high at each assessment (Cronbach’s α’s ≥ 0.92).
MA Administration Paradigm & Measures
Two hours after completion of the cue-exposure paradigm, participants completed a MA challenge. Participants received an infusion of 30-mg MA, administered in two 15-mg doses, each infused over two-minutes and separated by 30 minutes for safety monitoring. The 30-mg MA dose was selected because it is a commonly abused quantity, and infusion of this dosage reliably produces typical subjective MA effects (Newton et al., 2005; Johnson et al., 2007; Fowler et al., 2008). The IV administration method was selected over other routes (e.g., oral, smoked, etc.) to provide greater precision over MA dosing and eliminate aspects of inter-subject variability that may affect subjective response to MA. Further, previous research demonstrated a similar pattern of pharmacokinetic and subjective response to MA when comparing IV and smoking routes of administration (Cook et al, 1993), supporting the experimental validity of using IV MA administration in individuals who commonly smoke MA.
Assessment of subjective responses began immediately following administration of the second 15-mg MA dose. The primary outcome measure for this study was the Drug Effects Questionnaire (DEQ; (Morean et al. 2013), which was administered prior to MA administration (i.e., baseline) and then again at 5, 10, 15, 20, 30, 60, 90, and 120 minutes following the second 15-mg MA dose. The DEQ that was administered in this study was an 11-item questionnaire capturing subjective responses to drugs of abuse. The eleven items that were analyzed from this questionnaire were: “How much do you feel any drug effects?,” “How good are the drug effects you are feeling right now?,” “How high are you?,” “How stimulated do you feel right now?,” “How bad are the drug effects you are feeling right now?,” “How much would you like to access the drug right now?,” “How much would you like more of the drug, right now?,” “How depressed do you feel right now?,” “How anxious do you feel right now?,” “How much do you like the effects you are feeling now?, and “How much do you crave more of the drug right now?”. Participants were asked to rate their current feelings on a Likert scale ranging from 0 (none at all) to 10 (a lot).
Medication and Methamphetamine
Naltrexone was purchased from and compounded by Bayview Pharmacy (Saunderstown, RI) into blister packs with one oral capsule administered each day. The matched placebo was administered in one capsule each day. Participants swallowed the study medication under the observation of CTRC research nursing staff. Medication order was randomized and counterbalanced. Methamphetamine Hydrochloride (HCl): MA HCl was provided by a NIDA contractor. The UCLA Investigational Drug Pharmacy prepared two 15-mg (5-ml) infusions in 0.9% sodium chloride solution for each MA administration session. The dose selected and administration procedures were consistent with previous behavioral pharmacology studies (Newton et al., 2005 Newton et al., 2008).
Statistical Analysis
The data analysis had two primary aims: 1) to test the association between cue-induced craving and subjective response to the MA challenge, and 2) to determine if naltrexone, vs. placebo, moderated the association between cue-induced craving and subjective response to MA. For these analyses, we utilized hierarchical linear models (HLMs). Of note, HLM provides several advantages over alternative models (e.g., repeated-measures ANOVA) including a more flexible covariate structure and enhanced power, and HLM is preferred over ANOVA when analyzing repeated measures collected at unequal time intervals (Gueorguieva and Krystal 2004). In the HLM framework the repeated observations of DEQ scores are nested (at Level 1) within persons (at Level 2), with all post-infusion DEQ scores included in the model for each subjective effect. All models included random person-level intercepts and random slopes for post-infusion time to allow individual heterogeneity in the intercept and rate of change in DEQ scores. Analyses were conducted in Stata 13.0 (StataCorp., 2013) using restricted maximum likelihood estimation, a robust method of estimation in HLM with small sample sizes (Hoyle and Gottfredson 2015)). Missing data modifications were not required, as full data were obtained in this sample of study completers.
All models controlled for study design factors including medication condition, time, and any significant medication × time interactions. The baseline (pre-infusion) DEQ rating was a covariate in all models, which is preferred over other methods of baseline control (e.g., change scores) when estimating experimental effects (Vickers and Altman 2001). Medication sequence was also tested as a covariate but did not predict variance in subjective effects and was dropped from further analyses. Before examining primary hypotheses, preliminary analyses examined potential demographic predictors of post-infusion DEQ scores, including sex, age, and ethnicity, and any statistically-significant predictors (p < .05) were retained in further analyses. Models then tested: 1) the main effect of cue-induced craving MAUQ score on DEQ subjective effects and 2) cue-induced craving MAUQ score interaction with medication condition. The interaction effects were followed by tests of the MAUQ simple slopes to estimate the effect of cue-induced craving on DEQ scores within each medication condition.
Results
Replication and covariates of subjective effects
Sample characteristics are presented in Table 1. Preliminary analyses using the HLM approach examining study design predictors replicated the primary results reported previously in this sample using an ANOVA approach, which are reviewed briefly here. Statistically significant (ps < 0.05) medication × time interactions were observed for “Feel”, “High”, “Bad”, and “Anxious”, with naltrexone producing more rapid decline in these subjective effects following MA challenge. Significant main effects of medication were found for “Stimulated”, “Access”, “Like”, “Depressed”, “More”, and “Crave”, with naltrexone producing lower overall ratings of these subjective effects. Baseline DEQ score was significantly and positively associated with post-infusion DEQ scores for nearly all subjective effects, with the exception of “High” and “Good”. Finally, the only significant demographic predictor was ethnicity for “More” and “Access”, with lower scores for Caucasians, which was controlled for in subsequent analyses.
Table 1.
Sample characteristics
| Variable | Percentage or mean (SD) | Range |
|---|---|---|
| Education (years) | 12.19 (3.41) | 4 – 21 |
| Age | 36.93 (8.78) | 23 – 50 |
| Sex (% men) | 73% | |
| Ethnicity (% Caucasian) | 37% | |
| Age of first MA use | 24 (9.83) | 13 – 47 |
| Years of MA use | 12.48 (8.46) | <1 – 32 |
| DSM-IV MA abuse/dependence symptom count | 6.00 (2.26) | 2 – 11 |
| Number of MA use days (past 30 days) | 21.26 (8.15) | 9 – 30 |
| Primary route of MA use (n = 28) | ||
| Smoke | 93% | |
| Snort | 3.5% | |
| Inject | 3.5% | |
| Cigarette smokers (%) | 63% | |
| Alcohol drinkers (%) | 70% | |
| Number of alcohol-drinking days (past 30 days) | 5.56 (8.63) | 0 – 30 |
| Alcohol drinks per drinking day (past 30 days) | 4.07 (3.67) | <1 – 14 |
Abbreviations: DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; MA, methamphetamine.
Main effects of cue-induced craving on subjective response to MA
Cue-induced craving for MA, as assessed by the MAUQ, was significantly and positively associated with post-infusion DEQ scores for nearly all of the subjective effects (Table 2). Strong associations were observed for “Feel”, “High”, “Good”, “Stimulated”, “More”, “Access”, and “Crave”, with somewhat weaker but statistically significant associations for “Anxious” and “Depressed”. These significant associations were present when controlling for the effects of medication, time, medication × time interaction, and baseline DEQ scores on post-infusion DEQ scores. Cue-induced craving was not significantly associated with “Like” or “Bad”. Overall, greater levels of cue-induced craving prior to the MA challenge were associated with a larger subjective response to the MA challenge, in terms of positive (i.e., stimulation, good drug effects, feel drug, drug high), aversive (i.e., anxious and depressed), and craving-related (i.e., want more drug, would like access to drug, crave more of the drug) subjective effects.
Table 2.
Effects of medication, time, baseline score, and cue-induced craving on subjective effects following methamphetamine challenge (N = 30).
| Medication | Time | Medication × Time | Baseline DEQ Score | Cue-Induced Craving | |
|---|---|---|---|---|---|
| b | b | b | b | b | |
| Feel | 0.30 | −0.02*** | −0.01** | 0.41 | 0.45*** |
| Bad | 0.75*** | 0.00 | −0.01** | 1.18*** | 0.02 |
| High | 0.21 | −0.02*** | −0.01* | −0.24 | 0.34*** |
| Anxious | −0.08 | 0.00 | −0.01*** | 0.41*** | 0.22* |
| Like | −0.33* | −0.02*** | NA | 0.32*** | 0.12 |
| Good | −0.12 | −0.02*** | NA | −0.42 | 0.37*** |
| Depressed | −0.19* | 0.01* | NA | −0.36* | 0.23*** |
| Stimulated | −0.98*** | −0.02*** | NA | 0.59*** | 0.80*** |
| More | −0.78** | −0.01** | NA | 0.56*** | 0.78*** |
| Access | −0.83*** | −0.01** | NA | 0.28*** | 0.89*** |
| Crave | −0.43** | −0.01*** | NA | 0.16*** | 0.71*** |
p < .05,
p < .01.
p < .001.
Note: Cells marked “NA” were effects that were not included in the models that tested the MAUQ main effect, as preliminary analyses indicated a non-significant medication × time interaction for these terms. Abbreviations: DEQ: Drug Effects Questionnaire.
Interaction of cue-induced craving and naltrexone subjective response to MA
Given the significant association between cue-induced craving and subjective effects of MA, final analyses examined moderation of this association by medication condition (Table 3). Statistically significant cue-induced craving × medication interactions were observed for “Feel” (b = −0.73, p < 0.001), “High” (b = −0.37, p < 0.001), “Good” (b = −0.51, p < 0.001), and “Stimulated” (b = −0.35, p < 0.01). These interactions revealed that the positive association between cue-induced craving and subjective MA response was significantly reduced when receiving active naltrexone compared to placebo (Figure 1). Simple-slopes analyses revealed that in the placebo condition, greater cue-induced craving significantly predicted greater ratings of “Feel”, “High”, and Good”, but in the naltrexone condition these effects were not statistically-significant (Table 3). Greater cue-induced craving significantly predicted greater ratings of “Stimulated” in both medication conditions, but this effect was significantly lower in the active naltrexone condition compared to placebo. The cue-induced craving × medication interaction was not significant for the remaining subjective effects.
Table 3.
Interaction of medication condition and cue-induced craving on subjective effects following methamphetamine challenge (N = 30).
| Interaction Effect: Medication × Cue-Induced Craving | Simple slope: Cue-induced craving | |||
|---|---|---|---|---|
| b | z | Placebo | Naltrexone | |
|
|
|
|||
| Feel | −0.73*** | −6.71 | 0.79*** | 0.05 |
| High | −0.37*** | −3.27 | 0.51*** | 0.14 |
| Good | −0.51*** | −4.48 | 0.61*** | 0.10 |
| Stimulated | −0.35** | −3.00 | 0.96*** | 0.62*** |
| Like | −0.06 | −0.50 | 0.15 | 0.09 |
| Bad | −0.11 | −1.16 | 0.07 | −0.04 |
| More | 0.14 | 0.78 | 0.81*** | 0.99*** |
| Depressed | 0.08 | 1.10 | 0.19** | 0.28*** |
| Anxious | −0.04 | −0.33 | 0.24* | 0.20 |
| Access | 0.32 | 1.74 | 0.82*** | 1.06*** |
| Crave | 0.01 | 0.10 | 0.70*** | 0.71*** |
p < .05,
p < .01.
p < .001.
Figure 1.
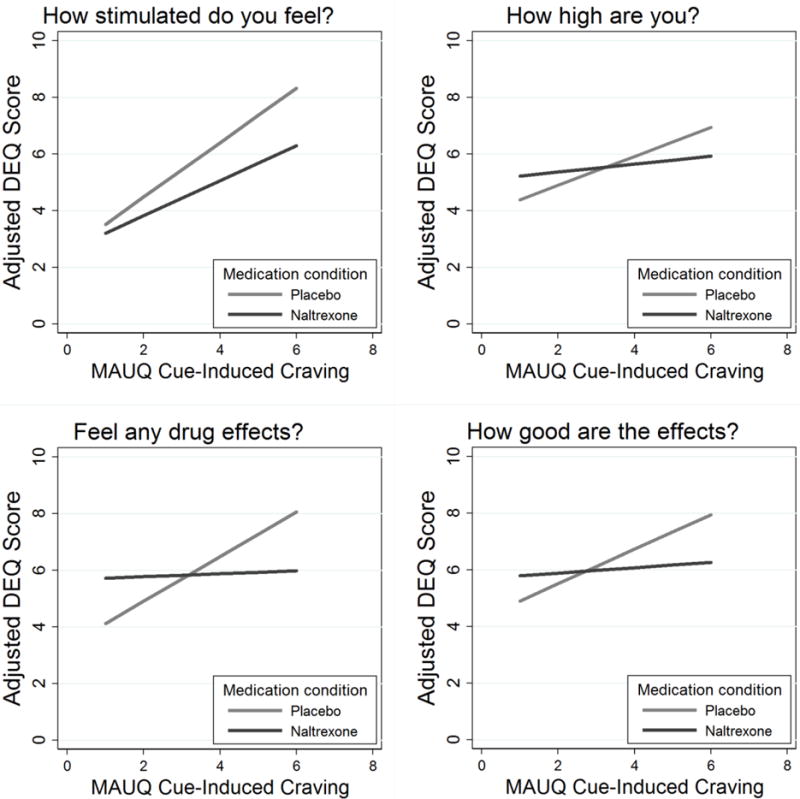
Active naltrexone moderates the association between cue-induced craving and subjective response following MA challenge. Figures display model-adjusted Drug Effect Questionnaire scores (estimated at 10 minutes post-infusion for display purposes) as a function of MAUQ cue-induced craving scores, with separate plots for the naltrexone and placebo conditions.
Altogether these results suggest that naltrexone moderated the association between cue-induced craving and positive subjective effects without impacting the associations between cue-induced craving and aversive or craving-related subjective effects. To ensure that these moderation results were not due to a “ceiling effect,” that is, that naltrexone uniformly blunted all positive subjective effects independent of its effects on MA craving, we visually inspected scatterplots of subjective response to MA during naltrexone and placebo (data not shown). We did not observe evidence that naltrexone produced a restricted subjective-response range. These findings along with the overall pattern of the results (i.e., naltrexone produced statistically different effects on each positive subjective response to MA) support the interpretation that naltrexone moderates the relationship between cue-induced craving and the positive subjective effects of MA. Finally, several covariates were also tested in the previously described models, including past 30-day MA and alcohol use, MA dependence severity, duration since first use of MA, and lifetime alcohol symptom count. None of these covariates significantly predicted subjective response to MA nor did their inclusion impact the previously reported main effects or interactions involving naltrexone.
Discussion
This study was the first to examine the predictive relationship between cue-induced MA craving and subsequent subjective response in individuals with MA use disorder (as measured by DSM-IV MA abuse or dependence). The findings suggested that greater levels of cue-induced craving were associated with larger positive (i.e., stimulation, good drug effects, feel drug, drug high), negative (i.e., anxious and depressed), and craving-related (i.e., want more drug, would like access to drug, crave more drug) subjective responses to acute MA administration. Additional analyses indicated that naltrexone moderated the association between cue-induced craving and positive subjective MA effects but not those related to craving or negative effects. These results provide initial evidence for individual variability in craving level predicting proximal subjective drug effects and may have also elucidated behavioral mechanisms by which naltrexone can be efficacious in treating MA use disorder.
Behavioral responses to drug-related cues and the subjective effects of drugs of abuse have both demonstrated high interindividual variability, which in turn is related to differences in drug-seeking behavior and the development of addiction (Flagel et al. 2009; de Wit and Phillips 2012; Ray et al. 2016). Additionally, prior studies have reported that psychophysiological states that are reliably associated with craving in drug users, such as high levels of stress and/or negative affect, may influence the subjective effects of drugs of abuse (Söderpalm and de Wit 2002; Söderpalm et al. 2003; Childs et al. 2011; Brkic et al. 2016). For example, a psychosocial stressor was reported to dampen the positive and negative subjective effects of MA while potentiating MA craving in healthy controls (Söderpalm et al. 2003). The present findings show that cue-induced craving at the level of the individual MA user is predictive of subjective response to MA, potentially suggesting shared underlying circuitry for each process. Interestingly, animal literature has demonstrated that rodents who are preferentially responsive to drug-conditioned stimuli (i.e., “sign-trackers”), comparable to the drug cues in the current study, also demonstrate greater psychomotor sensitization to stimulants and will work harder to obtain stimulant drugs than those who are less responsive to conditioned stimuli (i.e., “goal-trackers”; Flagel et al. 2008; Saunders and Robinson 2010; Saunders et al. 2013). This sensitized responsivity to drug-conditioned cues in rodents has been linked to heightened dopaminergic activity in several brain areas, including mesocorticolimbic and corticostriatalthalamic circuitry (Flagel et al. 2007; Flagel et al. 2009; Yager et al. 2015; Fraser et al. 2016). Further, cue-induced craving in humans is associated with striatal dopamine release (Wong et al. 2006; Volkow et al. 2006) and with activity in frontal, limbic, and midbrain areas (Grant et al. 1996; Childress et al. 1999; Kilts et al. 2001; Courtney et al. 2016) that are also acutely activated by drugs of abuse and involved in the hedonic effects of drugs and natural rewards (Richard et al. 2013; Berridge and Kringelbach 2015). Thus, we speculate that individuals who experience intensified cue-induced craving may possess an underlying neurobiological state that primes them to be hypersensitive to the subjective effects of the drug.
Across drugs of abuse, increases in craving have been identified as the single greatest predictor of whether an individual will participate in drug-seeking behavior and use a drug (Sinha 2013). While there have been no studies that have assessed the relationship between subjective response to MA during a lapse (i.e., a “slip”) or full relapse during treatment and future drug use, studies employing ecological momentary assessment (EMA) in tobacco smokers trying to quit have found that the magnitude of positive subjective effects during the first lapse after abstinence is predictive of the severity of that lapse, which in turn is highly predictive of progression to the next lapse and, ultimately, full relapse (Shiffman et al. 2006). When interpreted in the context of our current findings, this could suggest the subset of MA users that experience co-occurring heightened sensitivity to both drug cues and subjective drug effects are at high risk for continued problematic use and unsuccessful quit attempts. The sensitized responsivity to drug-related cues could promote chronic MA use and inability to sustain abstinence, whereas the augmented positive subjective MA effects after craving-induced use could increase the severity of that MA use episode and the likelihood of a single lapse turning into full relapse.
Despite the potentially problematic predictive relationship between cue-induced craving and subjective effects of MA, we also found that naltrexone was predominantly effective in reducing the positive subjective effects of MA in individuals who experienced high levels of cue-induced craving. In support of this finding, brain areas involved in both cue-induced craving and the hedonic effects of drugs are mediated in part by endogenous opioid activity (Richard et al. 2013; Berridge and Kringelbach 2015), providing a pharmacological mechanism by which naltrexone may dampen the relationship between craving and positive subjective MA effects. Furthermore, this finding suggests that naltrexone may be particularly effective in treating MA-dependent individuals who are susceptible to drug-cue-induced craving by disrupting the link between craving level and the positive acute effects of MA. For example, in individuals who still experience high degrees of cue-induced craving while taking naltrexone and are at high risk for a lapse, naltrexone would block the positive subjective effects of MA during that slip and potentially limit the severity of that MA use episode. As MA is often used in a binge pattern, which is in turn thought to relate to its neurotoxicity, cognitive impairment, and addiction maintenance (Cho and Melega 2001; Semple et al. 2003; Bujarski et al. 2014), the reduction in the severity of a lapse or use episode may be critical in improving treatment outcomes.
This study is not without limitations that should be considered when interpreting the present results. Although most relevant studies have found that drug preference and use are associated with heightened positive subjective drug effects, some have suggested that an attenuated positive subjective response may lead to increased use because individuals require more drug to experience the desired mood changes (for review, see de Wit and Phillips 2012). The latter interpretation, if proven valid, suggests patients who experience high levels of cue-induced craving could increase their MA use while on naltrexone, which would not support its use as a treatment for MA use disorder. An additional caveat is that naltrexone only attenuated the relationship between cue-induced MA craving and positive subjective MA effects. Although most findings indicate that positive effects are most closely related to future drug use and abuse, there is some evidence in cocaine users that initial aversive effects may also be related to future development of stimulant use disorders (Grant et al., 2005). Our results do not suggest that naltrexone is effective in reducing the positive relationship between cue-induced craving level and craving-related (i.e., want more drug, would like access to drug) or negative (i.e., anxious and depressed) MA subjective effects. Additional limitations include the single dose of naltrexone and the MA administration schedule. The MA infusion schedule (two 15-mg MA doses infused over two minutes and separated by 30 minutes) was selected to produce a gradual increase in cardiovascular parameters but may not be generalizable to real-world patterns of self-administration. Finally, although it is of interest to speculate on how the present results may be related to treatment outcomes with naltrexone, the participants in this study could have met criteria for either MA abuse or dependence and were not seeking treatment. Therefore, our interpretation of the findings should be viewed with some caution.
In summary, the present study found that level of cue-induced MA craving was predictive of subsequent subjective MA response in individuals with MA use disorder. Additional analyses revealed that naltrexone attenuated the relationship between craving and positive subjective effects, potentially suggesting a behavioral mechanism by which naltrexone may be an effective treatment for MA use disorder. Several lines of future research may productively extend the current results. First, as discussed in detail elsewhere (Ray et al. 2015), it is essential to determine whether the ability of a medication to affect subjective response to drugs of abuse in the laboratory is predictive of clinical outcomes. Second, these results point to the need of more EMA studies in individuals with stimulant use disorders. At present, only a handful of EMA studies in cocaine users have been conducted, and, to our knowledge, no EMA studies have been performed in MA users. An EMA study could replicate the present results in a naturalistic setting, ideally in treatment seekers, as well as examine how the relationship between craving level and subjective response relates to future MA use and abuse. Finally, future studies should consider examining the association between cue-induced craving and subjective drug response in other populations of substance users in order to determine whether the relationship generalizes to other substances of abuse.
Acknowledgments
This research was supported by a grant from the National Institute on Drug Abuse (DA029831) to LAR. Support for this study was also provided by a grant from the UCLA Clinical and Translational Science Institute, grants UL1RR033176 and UL1TR000124. DR was supported by postdoctoral awards from the California Tobacco Related Disease Research Program (18KT-0020) and T32 DA024635. SB was supported by a training grant from the National Institutes of Alcohol Abuse and Alcoholism (F31 AA022569), and KEC was supported by a training grant from the National Institute on Drug Abuse (F31 DA035604). LAR has received study medication from Pfizer and MediciNova and served as a consultant for GSK. EDL received support from the Thomas P. and Katherine K. Pike Chair in Addiction Studies and the Marjorie Greene Family Trust.
References
- Berridge KC, Kringelbach ML. Pleasure systems in the brain. Neuron. 2015;86:646–664. doi: 10.1016/j.neuron.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brensilver M, Heinzerling KG, Shoptaw S. Pharmacotherapy of amphetamine-type stimulant dependence: An update: Pharmacotherapy of ATS dependence. Drug Alcohol Rev. 2013:n/a–n/a. doi: 10.1111/dar.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brkic S, Söderpalm B, Gordh AS. High cortisol responders to stress show increased sedation to alcohol compared to low cortisol responders: An alcohol dose–response study. Pharmacol Biochem Behav. 2016;143:65–72. doi: 10.1016/j.pbb.2016.02.004. [DOI] [PubMed] [Google Scholar]
- Bujarski S, Hutchison KE, Prause N, Ray LA. Functional significance of subjective response to alcohol across levels of alcohol exposure. 2015 doi: 10.1111/adb.12293. [DOI] [PubMed] [Google Scholar]
- Bujarski S, Ray LA. Subjective response to alcohol and associated craving in heavy drinkers vs. alcohol dependents: An examination of Koob’s allostatic model in humans. Drug Alcohol Depend. 2014;140:161–167. doi: 10.1016/j.drugalcdep.2014.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujarski S, Roche DJO, Lunny K, et al. The relationship between methamphetamine and alcohol use in a community sample of methamphetamine users. Drug Alcohol Depend. 2014;142:127–132. doi: 10.1016/j.drugalcdep.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health 2015 [Google Scholar]
- Chait LD. Factors influencing the reinforcing and subjective effects of d-amphetamine in humans. Behav Pharmacol. 1993;4:191–200. [PubMed] [Google Scholar]
- Childress AR, Mozley PD, McElgin W, et al. Limbic activation during cue-induced cocaine craving. 1999 doi: 10.1176/ajp.156.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs E, O’Connor S, de Wit H. Bidirectional Interactions Between Acute Psychosocial Stress and Acute Intravenous Alcohol in Healthy Men. Alcohol Clin Exp Res. 2011;35:1794–1803. doi: 10.1111/j.1530-0277.2011.01522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho AK, Melega WP. Patterns of methamphetamine abuse and their consequences. J Addict Dis. 2001;21:21–34. doi: 10.1300/j069v21n01_03. [DOI] [PubMed] [Google Scholar]
- Chutuape MAD, De Wit H. Relationship between subjective effects and drug preferences: ethanol and diazepam. Drug Alcohol Depend. 1994;34:243–251. doi: 10.1016/0376-8716(94)90163-5. [DOI] [PubMed] [Google Scholar]
- Comer SD, Ashworth JB, Foltin RW, et al. The role of human drug self-administration procedures in the development of medications. Drug Alcohol Depend. 2008;96:1–15. doi: 10.1016/j.drugalcdep.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer SD, Mogali S, Saccone PA, et al. Effects of acute oral naltrexone on the subjective and physiological effects of oral D-amphetamine and smoked cocaine in cocaine abusers. Neuropsychopharmacology. 2013;38:2427–2438. doi: 10.1038/npp.2013.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook CE, Jeffcoat AR, Hill JM, et al. Pharmacokinetics of methamphetamine self-administered to human subjects by smoking S-(+)-methamphetamine hydrochloride. DRUG Metab Dispos-BETHESDA- 1993;21:717–717. [PubMed] [Google Scholar]
- Corbin WR, Gearhardt A, Fromme K. Stimulant alcohol effects prime within session drinking behavior. Psychopharmacology (Berl) 2007;197:327–337. doi: 10.1007/s00213-007-1039-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney KE, Ghahremani DG, Ray LA. The Effects of Pharmacological Opioid Blockade on Neural Measures of Drug Cue-Reactivity in Humans. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2016;41:2872–2881. doi: 10.1038/npp.2016.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney KE, Ray LA. Methamphetamine: An update on epidemiology, pharmacology, clinical phenomenology, and treatment literature. Drug Alcohol Depend. 2014;143:11–21. doi: 10.1016/j.drugalcdep.2014.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson ES, Finch JF, Schenk S. Variability in subjective responses to cocaine: initial experiences of college students. Addict Behav. 1993;18:445–453. doi: 10.1016/0306-4603(93)90062-e. [DOI] [PubMed] [Google Scholar]
- de Wit H, Doty P. Preference for ethanol and diazepam in light and moderate social drinkers: a within-subjects study. Psychopharmacology (Berl) 1994;115:529–538. doi: 10.1007/BF02245577. [DOI] [PubMed] [Google Scholar]
- de Wit H, Phillips TJ. Do initial responses to drugs predict future use or abuse? Neurosci Biobehav Rev. 2012;36:1565–1576. doi: 10.1016/j.neubiorev.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wit H, Pierri J, Johanson CE. Reinforcing and subjective effects of diazepam in nondrug-abusing volunteers. Pharmacol Biochem Behav. 1989;33:205–213. doi: 10.1016/0091-3057(89)90451-6. [DOI] [PubMed] [Google Scholar]
- Epstein DH, Willner-Reid J, Vahabzadeh M, et al. REal-time electronic diary reports of cue exposure and mood in the hours before cocaine and heroin craving and use. Arch Gen Psychiatry. 2009;66:88–94. doi: 10.1001/archgenpsychiatry.2008.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB. Structured clinical interview for DSM-IV-TR Axis I disorders: Patient edition. Biometrics Research Department; Columbia University: 2005. [Google Scholar]
- Flagel SB, Akil H, Robinson TE. Individual differences in the attribution of incentive salience to reward-related cues: Implications for addiction. Neuropharmacology. 2009;56(Suppl 1):139–148. doi: 10.1016/j.neuropharm.2008.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flagel SB, Watson SJ, Akil H, Robinson TE. Individual differences in the attribution of incentive salience to a reward-related cue: influence on cocaine sensitization. Behav Brain Res. 2008;186:48–56. doi: 10.1016/j.bbr.2007.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flagel SB, Watson SJ, Robinson TE, Akil H. Individual differences in the propensity to approach signals vs goals promote different adaptations in the dopamine system of rats. Psychopharmacology (Berl) 2007;191:599–607. doi: 10.1007/s00213-006-0535-8. [DOI] [PubMed] [Google Scholar]
- Fowler JS, Volkow ND, Logan J, et al. Fast uptake and long-lasting binding of methamphetamine in the human brain: Comparison with cocaine. NeuroImage. 2008;43:756–763. doi: 10.1016/j.neuroimage.2008.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraser KM, Haight JL, Gardner EL, Flagel SB. Examining the role of dopamine D2 and D3 receptors in Pavlovian conditioned approach behaviors. Behav Brain Res. 2016;305:87–99. doi: 10.1016/j.bbr.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway GP, Singleton EG. How long does craving predict use of methamphetamine? Assessment of use one to seven weeks after the assessment of craving: Craving and ongoing methamphetamine use. Subst Abuse Res Treat. 2009;1:63. [PMC free article] [PubMed] [Google Scholar]
- Grant JD, Scherrer JF, Lyons MJ, et al. Subjective reactions to cocaine and marijuana are associated with abuse and dependence. Addict Behav. 2005;30:1574–1586. doi: 10.1016/j.addbeh.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Grant JE, Odlaug BL, Kim SW. A double-blind, placebo-controlled study of N-acetyl cysteine plus naltrexone for methamphetamine dependence. Eur Neuropsychopharmacol. 2010;20:823–828. doi: 10.1016/j.euroneuro.2010.06.018. [DOI] [PubMed] [Google Scholar]
- Grant S, London ED, Newlin DB, et al. Activation of memory circuits during cue-elicited cocaine craving. Proc Natl Acad Sci. 1996;93:12040–12045. doi: 10.1073/pnas.93.21.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gueorguieva R, Krystal JH. Move over anova: Progress in analyzing repeated-measures data andits reflection in papers published in the archives of general psychiatry. Arch Gen Psychiatry. 2004;61:310–317. doi: 10.1001/archpsyc.61.3.310. [DOI] [PubMed] [Google Scholar]
- Haney M. Self-administration of cocaine, cannabis and heroin in the human laboratory: benefits and pitfalls. Addict Biol. 2009;14:9–21. doi: 10.1111/j.1369-1600.2008.00121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haney M, Spealman R. Controversies in translational research: drug self-administration. Psychopharmacology (Berl) 2008;199:403–419. doi: 10.1007/s00213-008-1079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartz DT, Frederick-Osborne SL, Galloway GP. Craving predicts use during treatment for methamphetamine dependence: a prospective, repeated-measures, within-subject analysis. Drug Alcohol Depend. 2001;63:269–276. doi: 10.1016/s0376-8716(00)00217-9. [DOI] [PubMed] [Google Scholar]
- Hoyle RH, Gottfredson NC. Sample size considerations in prevention research applications of multilevel modeling and structural equation modeling. Prev Sci. 2015;16:987–996. doi: 10.1007/s11121-014-0489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayaram-Lindström N, Hammarberg A, Beck O, Franck J. Naltrexone for the treatment of amphetamine dependence: a randomized, placebo-controlled trial. Am J Psychiatry. 2008a;165:1442–1448. doi: 10.1176/appi.ajp.2008.08020304. [DOI] [PubMed] [Google Scholar]
- Jayaram-Lindström N, Konstenius M, Eksborg S, et al. Naltrexone attenuates the subjective effects of amphetamine in patients with amphetamine dependence. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2008b;33:1856–1863. doi: 10.1038/sj.npp.1301572. [DOI] [PubMed] [Google Scholar]
- Jayaram-Lindström N, Wennberg P, Hurd YL, Franck J. Effects of naltrexone on the subjective response to amphetamine in healthy volunteers. J Clin Psychopharmacol. 2004;24:665–669. doi: 10.1097/01.jcp.0000144893.29987.e5. [DOI] [PubMed] [Google Scholar]
- Johnson BA, Roache JD, Ait-Daoud N, et al. Effects of acute topiramate dosing on methamphetamine-induced subjective mood. Int J Neuropsychopharmacol. 2007;10:85–98. doi: 10.1017/S1461145705006401. [DOI] [PubMed] [Google Scholar]
- Karila L, Weinstein A, Aubin H-J, et al. Pharmacological approaches to methamphetamine dependence: a focused review. Br J Clin Pharmacol. 2010;69:578–592. doi: 10.1111/j.1365-2125.2010.03639.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilts CD, Schweitzer JB, Quinn CK, et al. Neural activity related to drug craving in cocaine addiction. Arch Gen Psychiatry. 2001;58:334–341. doi: 10.1001/archpsyc.58.4.334. [DOI] [PubMed] [Google Scholar]
- King AC, de Wit H, McNamara PJ, Cao D. REwarding, stimulant, and sedative alcohol responses and relationship to future binge drinking. Arch Gen Psychiatry. 2011;68:389–399. doi: 10.1001/archgenpsychiatry.2011.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk JM, Doty P, De Wit H. Effects of Expectancies on Subjective Responses to Oral Δ9-Tetrahydrocannabinol. Pharmacol Biochem Behav. 1998;59:287–293. doi: 10.1016/S0091-3057(97)00414-0. [DOI] [PubMed] [Google Scholar]
- Lambert NM, McLeod M, Schenk S. Subjective responses to initial experience with cocaine: an exploration of the incentive–sensitization theory of drug abuse. Addiction. 2006;101:713–725. doi: 10.1111/j.1360-0443.2006.01408.x. [DOI] [PubMed] [Google Scholar]
- Leeman RF, Corbin WR, Fromme K. Craving predicts within session drinking behavior following placebo. Personal Individ Differ. 2009;46:693–698. doi: 10.1016/j.paid.2009.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee NK, Pohlman S, Baker A, et al. It’s the thought that counts: Craving metacognitions and their role in abstinence from methamphetamine use. J Subst Abuse Treat. 2010;38:245–250. doi: 10.1016/j.jsat.2009.12.006. [DOI] [PubMed] [Google Scholar]
- Mitchell SH, Laurent CL. Wit H de Interaction of expectancy and the pharmacological effects ofd-amphetamine: subjective effects and self-administration. Psychopharmacology (Berl) 125:371–378. doi: 10.1007/BF02246020. [DOI] [PubMed] [Google Scholar]
- Monti PM, Binkoff JA, Abrams DB, et al. Reactivity of alcoholics and nonalcoholics to drinking cues. J Abnorm Psychol. 1987;96:122. doi: 10.1037//0021-843x.96.2.122. [DOI] [PubMed] [Google Scholar]
- Morean ME, de Wit H, King AC, et al. The drug effects questionnaire: psychometric support across three drug types. Psychopharmacology (Berl) 2013;227:177–192. doi: 10.1007/s00213-012-2954-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton TF, De La Garza R, II, Kalechstein AD, Nestor L. Cocaine and methamphetamine produce different patterns of subjective and cardiovascular effects. Pharmacol Biochem Behav. 2005;82:90–97. doi: 10.1016/j.pbb.2005.07.012. [DOI] [PubMed] [Google Scholar]
- Nicosia N, Pacula RL, Kilmer B, et al. The economic cost of methamphetamine use in the United States, 2005. DTIC Document 2009 [Google Scholar]
- Paliwal P, Hyman SM, Sinha R. Craving predicts time to cocaine relapse: further validation of the Now and Brief versions of the cocaine craving questionnaire. Drug Alcohol Depend. 2008;93:252–259. doi: 10.1016/j.drugalcdep.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlick M, Hoffmann E, Rosenberg H. A nationwide survey of American alcohol and drug craving assessment and treatment practices. Addict Res Theory. 2009;17:591–600. [Google Scholar]
- Preston KL, Epstein DH. Stress in the daily lives of cocaine and heroin users: relationship to mood, craving, relapse triggers, and cocaine use. Psychopharmacology (Berl) 2011;218:29–37. doi: 10.1007/s00213-011-2183-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray LA, Bujarski S, Courtney KE, et al. The effects of naltrexone on subjective response to methamphetamine in a clinical sample: a double-blind, placebo-controlled laboratory study. 2015 doi: 10.1038/npp.2015.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray LA, Bujarski S, Roche DJ. Subjective Response to Alcohol as a Research Domain Criterion. Alcohol Clin Exp Res. 2016;40:6–17. doi: 10.1111/acer.12927. [DOI] [PubMed] [Google Scholar]
- Richard JM, Castro DC, DiFeliceantonio AG, et al. Mapping brain circuits of reward and motivation: in the footsteps of Ann Kelley. Neurosci Biobehav Rev. 2013;37:1919–1931. doi: 10.1016/j.neubiorev.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. Incentive-sensitization and addiction. Addiction. 2001;96:103–114. doi: 10.1046/j.1360-0443.2001.9611038.x. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Flagel SB. Dissociating the predictive and incentive motivational properties of reward-related cues through the study of individual differences. Biol Psychiatry. 2009;65:869–873. doi: 10.1016/j.biopsych.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche DJ, Ray LA. Subjective response as a consideration in the pharmacogenetics of alcoholism treatment. Pharmacogenomics. 2015;16:721–736. doi: 10.2217/pgs.14.143. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Martin RA, Eaton CA, Monti PM. Cocaine craving as a predictor of treatment attrition and outcomes after residential treatment for cocaine dependence. J Stud Alcohol Drugs. 2007;68:641–648. doi: 10.15288/jsad.2007.68.641. [DOI] [PubMed] [Google Scholar]
- Saunders BT, Robinson TE. A cocaine cue acts as an incentive stimulus in some but not others: implications for addiction. Biol Psychiatry. 2010;67:730–736. doi: 10.1016/j.biopsych.2009.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders BT, Yager LM, Robinson TE. Cue-evoked cocaine “craving”: role of dopamine in the accumbens core. J Neurosci. 2013;33:13989–14000. doi: 10.1523/JNEUROSCI.0450-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple SJ, Patterson TL, Grant I. Binge use of methamphetamine among HIV-positive men who have sex with men: pilot data and HIV prevention implications. AIDS Educ Prev. 2003;15:133–147. doi: 10.1521/aeap.15.3.133.23835. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Ferguson SG, Gwaltney CJ. Immediate hedonic response to smoking lapses: relationship to smoking relapse, and effects of nicotine replacement therapy. Psychopharmacology (Berl) 2006;184:608–618. doi: 10.1007/s00213-005-0175-4. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, et al. First lapses to smoking: within-subjects analysis of real-time reports. J Consult Clin Psychol. 1996;64:366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ. Negative Affect and Smoking Lapses: A Prospective Analysis. J Consult Clin Psychol. 2004;72:192–201. doi: 10.1037/0022-006X.72.2.192. [DOI] [PubMed] [Google Scholar]
- Sinha R. The clinical neurobiology of drug craving. Curr Opin Neurobiol. 2013;23:649–654. doi: 10.1016/j.conb.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Söderpalm AHV, de Wit H. Effects of Stress and Alcohol on Subjective State in Humans. Alcohol Clin Exp Res. 2002;26:818–826. doi: 10.1111/j.1530-0277.2002.tb02610.x. [DOI] [PubMed] [Google Scholar]
- Söderpalm A, Nikolayev L, de Wit H. Effects of stress on responses to methamphetamine in humans. Psychopharmacology (Berl) 2003;170:188–199. doi: 10.1007/s00213-003-1536-5. [DOI] [PubMed] [Google Scholar]
- Tancer M, Johanson C-E. Reinforcing, subjective, and physiological effects of MDMA in humans: a comparison with d-amphetamine and mCPP. Drug Alcohol Depend. 2003;72:33–44. doi: 10.1016/s0376-8716(03)00172-8. [DOI] [PubMed] [Google Scholar]
- Treloar H, Piasecki TM, McCarthy DM, et al. Ecological evidence that affect and perceptions of drink effects depend on alcohol expectancies. Addiction. 2015;110:1432–1442. doi: 10.1111/add.12982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNODC. United Nations Office on Drugs and Crime World Drug Report 2015. United Nations publication; 2015. [Google Scholar]
- Vickers AJ, Altman DG. Analysing controlled trials with baseline and follow up measurements. Bmj. 2001;323:1123–1124. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Wang G-J, Ma Y, et al. Expectation Enhances the Regional Brain Metabolic and the Reinforcing Effects of Stimulants in Cocaine Abusers. J Neurosci. 2003;23:11461–11468. doi: 10.1523/JNEUROSCI.23-36-11461.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Wang G-J, Telang F, et al. Cocaine Cues and Dopamine in Dorsal Striatum: Mechanism of Craving in Cocaine Addiction. J Neurosci. 2006;26:6583–6588. doi: 10.1523/JNEUROSCI.1544-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G, Shi J, Chen N, et al. Effects of length of abstinence on decision-making and craving in methamphetamine abusers. PLoS One. 2013;8:e68791. doi: 10.1371/journal.pone.0068791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell JD, Ramchandani VA, Hendershot CS. Drinking Motives Predict Subjective Effects of Alcohol and Alcohol Wanting and Liking During Laboratory Alcohol Administration: A Mediated Pathway Analysis. Alcohol Clin Exp Res. 2016;40:2190–2198. doi: 10.1111/acer.13174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witteman J, Post H, Tarvainen M, et al. Cue reactivity and its relation to craving and relapse in alcohol dependence: a combined laboratory and field study. Psychopharmacology (Berl) 2015;232:3685–3696. doi: 10.1007/s00213-015-4027-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong DF, Kuwabara H, Schretlen DJ, et al. Increased occupancy of dopamine receptors in human striatum during cue-elicited cocaine craving. Neuropsychopharmacology. 2006;31:2716–2727. doi: 10.1038/sj.npp.1301194. [DOI] [PubMed] [Google Scholar]
- Yager LM, Pitchers KK, Flagel SB, Robinson TE. Individual variation in the motivational and neurobiological effects of an opioid cue. Neuropsychopharmacology. 2015;40:1269–1277. doi: 10.1038/npp.2014.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorick T, Nestor L, Miotto K, et al. Withdrawal symptoms in abstinent methamphetamine-dependent subjects. Addiction. 2010;105:1809–1818. doi: 10.1111/j.1360-0443.2010.03066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


