Abstract
A collection of 33 Escherichia coli serogroup O15 strains was studied with regard to O:H serotypes and virulence markers and for detection of the O-antigen-specific genes wzx and wzy. The strains were from nine different countries, originated from healthy or diseased humans and animals and from food, and were isolated between 1941 and 2003. On the basis of virulence markers and clinical data the strains could be split into different pathogroups, such as uropathogenic E. coli, enteropathogenic E. coli, Shiga toxin-producing E. coli, and enteroaggregative E. coli. H serotyping and genotyping of the flagellin (fliC) gene revealed 11 different H types and a close association between certain H types, virulence markers, and pathogroups was found. Nucleotide sequence analysis of the O-antigen gene cluster revealed putative genes for biosynthesis of O15 antigen. PCR assays were developed for sensitive and specific detection of the O15-antigen-specific genes wzx and wzy. The high pathotype diversity found in the collection of 33 O15 strains contrasted with the high level of similarity found in the genes specific to the O15 antigen. This might indicate that the O15 determinant has been spread by horizontal gene transfer to a number of genetically unrelated strains of E. coli.
Escherichia coli serogroup O15 was defined in 1944 by F. Kauffmann, who established the method of serotyping of E. coli O and H antigens (reviewed in reference 37). Pathogenic E. coli O15 strains were first described in 1952 as causative agents of septicemia in newborn calves (35). The identification of virulence markers in E. coli extraintestinal and intestinal pathogenic strains resulted in further characterization of E. coli O15 and other strains as agents of disease in humans and animals. O15:K52:H1 strains were identified as a globally occurring clonal group of uropathogenic E. coli causing cystitis and bacteremia in humans. Uropathogenic O15:K52:H1 strains were isolated from single cases and outbreaks in hospitals and are characterized by the expression of P fimbriae, a consensus virulence profile, and a high percentage of multidrug-resistant isolates (20, 21, 32, 33, 44). A second pathogenic clone of E. coli O15 strains is represented by O15:NM (nonmotile) strains which were identified as causative agents of diarrhea in rabbits (11, 31, 42). Like human enteropathogenic E. coli (EPEC), rabbit EPEC strains cause attaching and effacing lesions in the intestinal mucosa of the infected host (42, 46). The genes responsible for the attaching and effacing lesion are located on the locus of enterocyte effacement (LEE) and the nucleotide sequence of the LEE from the prototype O15:NM rabbit EPEC strain was analyzed and found to be similar in the core region to LEE sequences from human EPEC and enterohemorrhagic E. coli (EHEC) strains (53, 62). Subtyping of the LEE encoded eae (intimin) genes in the rabbit EPEC O15:NM protype strain RDEC-1 and in a bovine EPEC O15:NM revealed the intimin beta type (23, 39). Intimin-positive E. coli O15 strains were also occasionally isolated from human patients with diarrhea (10, 60), but the relationship between O15 EPEC from humans and animals is not well known.
Other types of E. coli O15 strains were found to produce cytotoxins such as Shiga toxins (Stx) and cytotoxic necrotizing factors (CNF) or heat-labile and heat-stable enterotoxins (LT and ST). Stx-producing E. coli (STEC) O15 strains were isolated from humans, cattle, and sheep in different countries and on different continents (9, 13, 25, 40). Necrotoxins such as CNF1 were found in E. coli O15 strains from cases of human urinary tract infection (21), and CNF2-producing E. coli O15 strains were isolated from healthy and diarrheic cattle (8, 34). Enterotoxigenic E. coli (ETEC) O15 strains are mainly represented by serotypes O15:H11 and O15:H45 and were isolated in different geographic locations at different time periods (38, 59). Finally, enteroaggregative E. coli (EAEC) of serotype O15:H18 were isolated from patients with diarrhea in Chile and Thailand (reviewed in reference 28).
Published data indicate that the serogroup O15 is associated with E. coli strains showing a high diversity in both their flagellar antigens and their virulence attributes. In the present study, we were interested in analyzing a representative collection of E. coli O15 strains for their virulence markers, for their H serotypes and fliC genotypes, and for the sequence and specific genes of the O-antigen gene cluster. The O antigen, which consists of repeats of oligosaccharide unit (O unit), is part of the lipopolysaccharide in the outer membrane of gram-negative bacteria and contributes major antigenic variability to the cell surface. In E. coli, genes for O-antigen synthesis are normally clustered and mapped between two housekeeping genes, galF and gnd (www.microbio.usyd.edu.au/BPGD/default.htm). The O-antigen gene cluster includes genes for the synthesis of nucleotide sugar precursors, genes encoding transferases for the addition of sugars sequentially, and genes for flipping and polymerizing the O unit into O antigen. The O unit processing genes (the flippase gene wzx and the polymerase gene wzy) are normally specific to particular O antigen. We analyzed the O-antigen gene cluster of E. coli O15 by sequencing and assigned functions to putative genes based on sequence similarity and conserved domains. Based on the sequence of E. coli O15 O-antigen gene cluster, we developed PCR assays for rapid identification of E. coli O15 strains from clinical, environmental, and food samples. Our results also indicate that the different pathotypes among E. coli O15 strains are associated with distinct H serotypes and fliC genotypes but that genes specific to O15 antigen synthesis are highly conserved among the different strains.
MATERIALS AND METHODS
Bacteria.
The E. coli clinical strains were mainly from the collection of the Robert Koch Institute, Berlin, Germany, except five E. coli O15 isolates which were from James R. Johnson (Medical Service, Veterans Affairs Medical Center, Minneapolis, Minn.). A group of 33 E. coli O15 strains that were isolated between 1941 and 2003 and originated from nine different countries were investigated for serotype, virulence markers, and O15-antigen-specific genes. The strains originated from humans (n = 25), cattle (n = 3), meat (n = 3), milk (n = 1), and a rabbit (n = 1) (Table 1). The E. coli O15 O serogroup reference strain F 7902-41 (G1201) for nucleotide sequence analysis of the O-antigen gene cluster were obtained from the Institute of Medical and Veterinary Science, Adelaide, Australia. Strains P12b, F 7902-41, N234, K50, and C107-74 from the collection of the International Escherichia and Klebsiella Reference Center, Statens Serum Institute, Copenhagen, Denmark, were also used as reference strains for the O15 antigen (36). Strain TB209E was from Phillip Tarr, University of Washington, Seattle; RDEC-1 was from Eric Oswald, INRA, Toulouse, France; and strain PE42 was from Francine Grimont, Institut Pasteur, Paris, France. All plasmids used in the present study were maintained in E. coli K-12 strain DH5α, which was purchased from Beijing Dingguo Biotechnology Development Center (Beijing, People's Republic of China). Other E. coli and Shigella O serogroup reference strains used are listed in Table 2.
TABLE 1.
Relevant properties of E. coli O15 strains
| Culture | Strain, reference(s) | Origin, yr of isolationa | Diseaseb | Host, sourcec | Serotyped | Virulence markerse | Pathotypef |
|---|---|---|---|---|---|---|---|
| G1384 | 2P9 (21, 44) | SP, 1994/95 | UTI | Hu, U | O15:K52:H1 | - | UPEC |
| G1386 | V32 (21) | USA, 2002g | UTI | Hu, U | O15:K+:H1h | α-hlyA, cnfi | UPEC |
| G1388 | 29/P (21, 44) | SP, 1994/95 | UTI | Hu, U | O15:K52:H1 | - | UPEC |
| G1400 | CB2092 | D, 1992 | D | Hu, F | O15:H2 | eae-β1 | EPEC |
| G1427 | CB3304 | AUS, 1993 | AS | Hu, F | O15:H2 | eae-β1 | EPEC |
| G1415 | CB3657 | D, 1994 | HUS | Hu, F | O15:H2 | eae-β1 | EPEC |
| G1425 | CB3938 | D, 1994 | HUS | Hu, F | O15:H2 | eae-β1, stx2 | STEC |
| G1401 | CB3939 | D, 1994 | HUS | Hu, F | O15:H2 | eae-β1, stx2 | STEC |
| G1407 | CB3940 | D, 1994 | HUS | Hu, F | O15:H2 | eae-β1, stx2 | STEC |
| G1421 | CB9796 | D, 2003 | D | Hu, F | O15:H2 | eae-β1 | EPEC |
| G1406 | CB9798 | D, 2003 | AS | Hu, F | O15:H2 | eae-β1 | EPEC |
| G1418 | CB9253 | D, 2002 | AS | Ca, meat | O15:H2 | eae-β1 | EPEC |
| G1411 | CB9263 | D, 2002 | AS | Ca, meat | O15:H2 | eae-β1 | EPEC |
| G1422 | PE42 | F, 1995 | HUS | Hu, F | O15:[H4] | - | - |
| G1417 | CB749 | D, 1989 | BM | Ca, milk | O15:[H4] | - | - |
| G1201 | F7902-41 (37) | DK, 1941 | ND | Hu, F | O15:K14:H4 | - | - |
| G1403 | C107-74 | YU, 1974 | ND | Hu, F | O15:H4 | - | - |
| G1391 | P12b (37) | DK, 1944 | ND | Hu, F | O15:H17 | - | - |
| G1413 | CB8515 | PL, 2000 | D | Hu, F | O15:[H11] | - | - |
| G1416 | DG5/4 | D, 1989 | AS | Ca, F | O15:H11 | E-hlyA, eae-β1 | EPEC |
| G1429 | RDEC-1 (11) | USA, 1977 | D | Ra, F | O15:[H11] | eae-β1 | EPEC |
| G1405 | CB8581 | D, 2000 | UTI | Hu, U | O15:H12 | - | - |
| G1419 | CB9587 | D, 2003 | D | Hu, F | O15:H12 | - | - |
| G1428 | CB9633 | D, 2003 | D | Hu, F | O15:[H12] | - | - |
| G1410 | CB1703 | D, 1991 | D | Hu, F | O15:H12 | - | - |
| G1387 | ECOR 24 (30) | S, 1984g | AS | Hu, F | O15:[H14] | α-hlyA | - |
| G1426 | CB5664 | D, 1996 | D | Hu, F | O15:[H18] | - | - |
| G1385 | CA017 (19) | USA, 2002g | UTI | Hu, U | O15:H18 | α-hlyA, EAECp | EAEC |
| G1420 | C4605 | D, 1990 | D | Hu, F | O15:H18 | α-hlyA, EAECp | EAEC |
| G1423 | TB209E (10) | USA, 1991 | D | Hu, F | O15:H20 | eae-β1 | AEEC |
| G1390 | N234 (35) | DK, 1952 | ND | Ca, F | O15:H25 | - | - |
| G1389 | K50 (35) | DK, 1952 | CS | Ca, LN | O15:H27 | - | - |
| G1409 | CB6105 | D, 1996 | AS | Ca, meat | O15:H27 | stx2 | STEC |
SP, Spain; USA, United States; D, Germany; AUS, Australia; F, France; DK, Denmark; YU, Yugoslavia; PL, Poland; S, Sweden.
D, diarrhea; HUS, hemolytic-uremic syndrome; AS, asymptomatic; BM, bovine mastitis; ND, no data; CS, calf septicemia.
Hu, human; Ca, cattle; Ra, rabbit. Source: U, urine; F, feces; LN, lymph nodes.
An H type in brackets indicates that the strain was NM and the fliC genotype was determined by PCR as described. K antigens were not explored in this study, and K designations are indicated as reported elsewhere (21, 30, 37).
The strains were investigated for the following virulence markers by PCR: alpha- hemolysin (α-hlyA), EHEC-hemolysin (E-hlyA), CNF (cnf) cytolethal distending toxins (cdt), intimin (eae), bundle-forming pili (bfpA), Shiga toxins (stx), EAEC virulence plasmid sequences (EAEC-p), heat-labile enterotoxin (LT-I), and heat-stable enterotoxin (STI). Subtyping of stx and eae genes was performed as described in Materials and Methods. -, Negative for the virulence markers investigated in this study.
Pathotype according to virulence markers and disease.
Year of publication.
Strain V32 was originally described as O15/40:K+:H1 (21).
Strain V32 was reported to carry the gene encoding CNF1 (21).
TABLE 2.
E. coli and Shigella reference strains and PCR pools used for testing of E. coli O15-specific primers
| Pool no. | Strains for which chromosomal DNA is included in the pool | Source |
|---|---|---|
| 1 | E. coli type strains for O serotypes 1, 2, 5, 7, 12, 13, 14, 15, 16, 17, 19ab, 20, 21, 22, 23, 24, 59, 3, and 11 | IMVSa |
| 2 | E. coli type strains for O serotypes 25, 26, 27, 28, 29, 30, 32, 31, 33, 35, 36, 37, 38, 40, 41, 42, 43, 39, and 59 | IMVS |
| 3 | E. coli type strains for O serotypes 44, 45, 46, 48, 49, 50, 51, 52, 54, 55, 56, 57, 58, 60, 61, 62, 64, and 73 | IMVS |
| 4 | E. coli type strains for O serotypes 63, 65, 66, 69, 70, 71, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 96, and 95 | IMVS |
| 5 | E. coli type strains for O serotypes 84, 85, 86, 87, 88, 89, 91, 92, 98, 99, 101, 102, 103, 104, 105, 106, 100, and 151 | IMVS |
| 6 | E. coli type strains for O serotypes 107, 108, 109, 110, 111, 112ab, 112ac, 113, 115, 116, 118, 120, 123, 125, 126, and 128 | IMVS |
| 7 | E. coli type strains for O serotypes 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139, 140, 141, 142, 143, 144, and 145 | IMVS |
| 8 | E. coli type strains for O serotypes 146, 147, 148, 150, 152, 154, 156, 157, 158, 159, 160, 161, 163, 164, 165, and 166 | IMVSb |
| 9 | E. coli type strains for O serotypes 168, 169, 170, 171, 172, 173, 155, and 124 and S. dysenteriae type strains for O serotypes D1, D2, D3, D4, D5, D6, D7, D8, D9, D10, D11, and D12 | IMVSc NICDCPd |
| 10 | S. boydii type strains for O serotypes B1, B2, B3, B4, B6, B7, B8, B9, B10, B11, B12, B13, B14, B15, B16, B17, and B18 | NICDCP |
| 11 | S. flexneri type strains for O serotypes F1a, F1b, F2a, F2b, F3, F4b, F5(v:4), F5(v:7), F6, FX variation, and FY variation and S. sonnei type strains for O serotypes DS and DR | NICDCP |
| 12 | E. coli type strains for O serotypes 3, 11, 39, 59, 64, 73, 96, 95, 100, 114, 151, 167, 162, 121, 127, 149, and 119 | IMVSe |
| 13 | Same as pool 1 but lacks E. coli O15, used as a control | IMVS |
Institute of Medical and Veterinary Science, Adelaide, Australia.
E. coli O165 and O166 were from the Statens Serum Institute, Copenhagen, Denmark; all other strains were from the IMVS.
E. coli O155 and O124 were from the IMVS; all other strains from the Statens Serum Institute.
National Institute for Communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, People's Republic of China.
E. coli O167 was from the Statens Serum Institute; all other strains were from the IMVS.
The E. coli strains that were used as positive and negative controls for detection of EAEC, bundle-forming pili (bfp), intimins (eae family), Shiga toxins (stx family), and hemolysins (α-hlyA and EHEC-hlyA) are listed elsewhere (6), as well as the reference strains for cytolethal distending toxins and CNF (55). ETEC strains that were used as controls for PCR detection of genes encoding heat-labile and heat-stable enterotoxins were described previously (5, 43).
Serotyping of O and H antigens and molecular typing of flagellar (fliC) genes.
Production of antisera and typing of O (lipopolysaccharide) and H (flagellar) antigens was performed as described previously (36). O-antigen typing was performed by titration of boiled cultures of bacteria with serial twofold dilutions of rabbit antiserum, followed by incubation overnight at 50°C as described previously (36). Strain F7902-41 (O15:K14:H4) was used for production of O15-antigen-specific antiserum. H serotyping was performed by titration of formalin-inactivated motile cultures of bacteria and the reference strains for the 53 different H antigens (H1 to H56) (36). NM E. coli strains were investigated for their H-type-specific (fliC) genes by PCR, followed by HhaI digestion of fliC PCR products and evaluation of RFLP patterns as described previously (6, 26).
Detection of virulence properties and associated genes.
All strains were investigated for production of cytotoxins by the Vero cell toxicity test as described previously (6). Verotoxic strains were investigated for production of Shiga toxins by the VTEC-RPLA assay (i.e., reverse passive latex agglutination test for detection of Stx1 [VT1] and Stx2 [VT2]; Denka-Seiken, Tokyo, Japan) and for the presence of stx genes and stx gene variants by PCR and restriction endonuclease digestion of PCR products as described previously (6). Hemolytic activity was detected by growing bacteria on washed sheep blood agar plates (enterohemolysin agar; Oxoid, Wesel, Germany) an indicator medium used for the phenotypic characterization of enterohemolytic and alpha-hemolytic strains of E. coli (7). Strains showing hemolytic activity were analyzed for α- and EHEC-hemolysin-specific genes by PCR (6). Detection and subtyping of intimin (eae) genes was performed as recently described (61). Bundle-forming pili genes (bfpA) which are associated with classical EPEC strains were investigated by PCR (6). The presence of DNA sequences associated with virulence plasmids present in EAEC was investigated by PCR specific for plasmid pCVD432 as described previously (6, 48). Multiplex PCRs detecting all known genetic variants of cytolethal distending toxins (cdt) and CNF (cnf) were used for detection of cdt- and cnf-specific sequences (55). Genes encoding heat-labile enterotoxin (LT-I) encompassing antigenic groups LTh-I and LTp-I (29) were detected by PCR as described previously (16). Specific PCRs for detection of the heat-stable enterotoxins STI (STa) of human (STIh) and porcine (STIp) types (29) were developed on the basis of published nucleotide sequences. Primers STIh-Start (5′-TCC CTC AGG ATG CTA AAC-3′) and STIh-Stop (5′-GCA ACA GGT ACA TAC GTT-3′) were developed from GenBank sequence M34916 and used for PCR amplification of a 244-bp product specific for the STIh variant (30 cycles of 94°C for 40 s, 47°C for 60 s, and 72°C for 40 s). Primers STIp-Start (5′-TTC TGT ATT ATC TTT CCC C-3′) and STIp-Stop (5′-TTA TGA TTT TCT CAG CAC C-3′) were developed from GenBank sequence M25607 and amplified a 258-bp stretch of DNA specific for the STIp variant (30 cycles of 94°C for 40 s, 51.3°C for 60 s, and 72°C for 40 s).
Construction of DNase I shotgun bank, sequencing, and analysis of O-antigen gene cluster.
Chromosomal DNA was prepared as previously described (3). The O-antigen gene cluster DNA of E. coli O15 reference strain G1201 (O15:K14:H4) was amplified by using the primer pairs WL-912 (5′-ATT GTG GCT GCA GGG ATC AAA GAA AT-3′) and WL-913 (5′-TAG TCG CGT GNG CCT GGA TTA AGT TCG C-3′), which were designed based on housekeeping genes galF and gnd, respectively (12) (30 cycles of 94°C for 10 s, 60°C for 30 s, and 68°C for 15 min). The PCR products were digested by DNase I, and the resulting DNA fragments were cloned into pGEM-T Easy (Promega) to produce a shotgun bank as described previously (57).
Sequencing was carried out by using an ABI 3730 automated DNA sequencer. Sequence data were assembled by using the Staden Package (49). The program Artemis was used to find open reading frames (ORFs) (47). BLAST and PSI-BLAST were used for searching the GenBank database (2). The program BlockMaker was used for searching conserved regions in protein sequences (18). The protein domain databases COG and Pfam were searched by program HMMER to find potential protein domains (4, 52). The program TMHMM 2.0 was used for identification of potential transmembrane segments in protein sequences (24). The program CLUSTAL W was used for performing sequence alignment (54).
Specificity and sensitivity test of O15 serogroup-specific PCR assay.
DNA from each reference strain was prepared as described previously (3). The quality of chromosomal DNA prepared from 186 reference strains to represent the broadest range of O antigens of E. coli (including Shigella) was examined by PCR amplification of the mdh gene with the primer pairs WL-101 (5′-TTC ATC CTA AAC TCC TTA TT) and WL-102 (5′-TAA TCG CAG GGG AAA GCA GG) (45). A total of 13 pools of DNA were made, each containing DNA from 12 to 19 strains (Table 2). Pools were screened with four primer pairs based on wzx and wzy genes of E. coli O15 (30 cycles of 95°C for 30 s, annealing for 30 s, and 72°C for 1 min; the annealing temperatures of respective primer pairs are listed in Table 3). Pools of 63 clinical E. coli isolates representing different O antigens, including all 33 E. coli O15 strains, were also screened in a double-blind test. Each strain was cultured in Luria-Bertani medium at 200 rpm in 37°C for 12 h, and 3 ml of culture were centrifuged at 5,000 × g for 5 min. The pellet was mixed with 100 μl of Milli-Q water, boiled at 100°C for 15 min, and centrifuged at 12,000 × g for 10 min. The supernatant was used as a template in the PCR assays with four primer pairs based on wzx and wzy genes of E. coli O15 (30 cycles of 95°C for 30 s, annealing for 45 s, and 72°C for 1 min, annealing temperatures of respective primer pairs are listed in Table 3). PCRs were carried out in a total volume of 25 μl, including 1 μl of template DNA.
TABLE 3.
PCR testing of E. coli O15-specific genes
| Gene | Positions | Name (position), oligonucleotide sequence of:
|
Annealing temp (°C) | |
|---|---|---|---|---|
| Forward primers | Reverse primers | |||
| wzx | 2430-3674 | WL-947 (3092-3112), 5′-TAGTGCATACACAATGTTGAC-3′; WL-950 (2475-2492), 5′-GGTGCCAATTACCTACTG-3′ | WL-948 (3429-3450), 5′-CAACTGTATTAAAACCTATGAA-3′; WL-951 (2966-2984), 5′-AACGCCACAGAATGAATAC-3′ | 58 62 |
| wzy | 4707-5885 | WL-952 (5464-5483), 5′-ATGATGAGTTCGTTTCTGGA-3′; WL-954 (4996-5016), 5′-TTTTATTTTCATTTGTTCCTG-3′ | WL-953 (5840-5860), 5′-TTAGTAATTGAACTCTGTCCA-3′; WL-955 (5444-5461), 5′-AATCGAGGGAAGAACACC-3′ | 56 58 |
Serial dilution of chromosomal DNA from E. coli O15 strain G1384 (Table 1) was detected by using four primer pairs specific to E. coli O15. A 10-fold serial dilution of E. coli O15 strain G1384 in pork and water samples were also detected by using the primer pairs WL-950-WL-951 and WL-952-WL-953. The methods for testing the sensitivity of O-serogroup-specific PCR assay in pork and water were described previously (17). For each primer, the experiment was performed in triplicate.
Nucleotide sequence accession number.
The DNA sequence of the E. coli O15 O antigen gene cluster has been deposited in GenBank under the accession number AY647261.
RESULTS AND DISCUSSION
Serotypes.
Agglutination of boiled cultures of the strains listed in Table 1 with O15 antiserum resulted in homologous O titers between 1:3,200 to 1:6,400 and were thus not significantly different from the O15 reference strains which showed agglutination titers up to 1:6,400. The O15 antigen was described to show cross-reactivities with O12, O40, O45, O51, O60, and O143 antiserum (14, 37). In our study, the most important serological cross-reactivity was found with O40 antiserum, which showed agglutinating titers between 1:800 and 1:1,600 with E. coli O15 strains. Of the 33 O15 strains, 27 were motile and could be analyzed for their H serotypes. H serotyping was completed by analysis of the flagellar (fliC) genotype of motile and NM O15 strains by HhaI digestion of fliC PCR products as described in Materials and Methods. The strains were grouped into 11 different H serotypes/fliC types (H1, H2, H4, H11, H12, H14, H17, H18, H20, H25, and H27) as shown in Table 1. Flagellar types H4 and H17 were previously reported to be closely related for the nucleotide sequences of their flagellin (fliC) genes and were also shown to be serologically related (14, 36, 58).
Association of virulence markers with pathogroups and with flagellar types in E. coli O15 strains.
All strains were investigated for production of cytotoxins and hemolysins as described in Materials and Methods. The presence of virulence genes was investigated by PCR as listed in Table 1. Of the 33 O15 strains, 19 were assigned to four different pathotypes on the basis of published data, clinical picture, and virulence markers found in the strains. The uropathogenic E. coli clones were represented by three O15:H1 strains, and two of these were shown to carry the capsular antigen K52. A group of seven O15:H2 strains that were isolated from humans and cattle that carried the eae-β1 gene were grouped as EPEC strains. A second group of EPEC strains included O15:[H11] (eae-β1) strains. Among these strains was the NM rabbit EPEC strain RDEC-1, which was shown to harbor the fliC gene encoding flagellar type H11. Two other O15:[H11] strains were found, one was from a human diarrheal case and the other from cattle feces. A third group of O15 EPEC is represented by strain TB209E (O15:H20) (eae-β1), which was isolated from a child with diarrhea in Seattle, Wash. (10). Two groups of STEC were found; one is represented by O15:H2 (eae-β1, stx2) strains that were isolated from an outbreak with HUS hemolytic-uremic syndrome in Germany, and the second is represented by an O15:H27 strain (stx2) that originated from bovine meat. Three O15:[H18] strains were found; two of these were positive for EAEC-plasmid specific sequences and for alpha-hemolysin, and these were classified as EAEC. EAEC of serotype O15:H18 were previously reported as human pathogens (28).
Eleven strains belonging to flagellar types H4/H17, H12, H25, and H27 were negative for all virulence markers investigated in the present study, and it is not clear whether these are pathogens. However, four of these were isolated from cases of disease, namely, CB749 (bovine mastitis), PE42 (hemolytic-uremic syndrome), CB8581 (urinary tract infection [UTI]), and K50 (calf septicemia). None of the E. coli O15 strains investigated in our study carried genes for enterotoxins, cytolethal distending toxin, or bundle-forming pili; the latter are associated with class-I (typical) EPEC strains (56).
Sequencing of E. coli O15 O-antigen gene cluster.
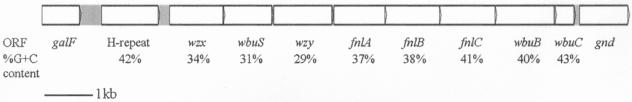
The O antigen gene cluster DNA of E. coli O15 was PCR amplified with primer pairs based on sequences of housekeeping genes galF and gnd, which flank the O-antigen gene cluster in E. coli. Five individual PCR products were combined to construct the shotgun bank for sequencing analysis to avoid PCR errors. A sequence of 11,893 bases from galF (positions 1 to 765) to gnd (positions 10,909 to 11,893) was obtained, and nine ORFs were found. All ORFs have the same transcriptional direction from galF to gnd (Fig. 1) and start with an ATG codon except for orf3 that probably starts from TTG, with a potential Shine-Dalgarno ribosomal binding site GGGG. Five ORFs ended with a TGA codon, two ORFs ended with a TAA codon, and two ORFs ended with a TAG codon. Noncoding sequences of 78, 49, 41, and 1 bp were found preceding the start codons of orf2, -4, -5, and -6, respectively. All other ORF junctions have overlapping termination and initiation codons. In E. coli O15, ORFs share low G+C% content of 29 to 43% (Fig. 1), significantly lower than that of E. coli genome (50%), as the situation in all reported E. coli O-antigen gene clusters.
FIG. 1.
O-antigen gene cluster of E. coli O15. All of the genes are transcribed in a direction from galF to gnd.
Sequence analysis of E. coli O15 O-antigen gene cluster.
Putative gene designations were made for all of the genes in the O-antigen gene cluster based on knowledge of previously characterized O-antigen genes and homology comparisons made by using available databases (Table 4).
TABLE 4.
ORFs in the O-antigen gene cluster of E. coli O15
| Gene | Location in sequence | % G+C content | Conserved domain (Pfam accession no.), E value | Similar proteins, strain (accession no.) | % Identity/% similarity (aa overlap)a | Putative function |
|---|---|---|---|---|---|---|
| H repeat | 1215-2351 | 41.6 | Transposase_11 (PF01609), 5.1 × e−48 | H-repeat-associated protein, E. coli (AAC61885) | 97/98 (378) | H-repeat transposase |
| wzx | 2430-3674 | 33.6 | Polysacc_synt (PF01943), 2 × e−5 | Putative O-antigen transporter, E. coli (BAA15879) | 27/49 (359) | O-antigen flippase |
| wbuS | 3671-4657 | 30.8 | Glycos_transf_2 (PF00535), 7 × e−15 | Putative glucosyl transferase, P. aeruginosa (AAD45263) | 35/53 (333) | Glycosyltransferase |
| wzy | 4707-5885 | 29.2 | O-antigen polymerase, S. boydii O11 (AAS98031) | 20/41 (247) | O-antigen polymerase | |
| fnlA | 5927-6961 | 37.4 | Polysacc_synt_2 (PF02719), 1.6 × e−11 | Fnl1 protein, E. coli O26 (AAN60461) | 90/95 (344) | l-Fucosamine synthetase |
| fnlB | 6963-8066 | 38.1 | Fnl2 protein, E. coli O26 (AAN60462) | 71/81 (367) | l-Fucosamine synthetase | |
| fnlC | 8066-9196 | 41.2 | Epimerase_2 (PF02350), 7.6 × e−122 | Fnl3 protein, E. coli O26 (AAN60463) | 89/95 (370) | l-Fucosamine synthetase |
| wbuB | 9196-10407 | 40.3 | Putative l-fucosamine transferase, E. coli O26 (AAN60464) | 72/84 (398) | l-Fucosamine transferase | |
| wbuC | 10394-10792 | 42.6 | WbuC protein, E. coli O26 (AAN60465) | 70/87 (131) | Unknown |
aa, amino acid.
(i) Genes for biosynthesis of 2-acetylamino-2,6-dideoxy-l-galactose (FucNAc).
Genes for the synthesis of the nucleotide form of common sugars are located outside O-antigen gene cluster and only genes for unique NDP-sugars were expected within the O-antigen gene cluster.
ORFs 5, 6, and 7 showed 90, 71, and 89% identity to FnlA (Fnl1), FnlB (Fnl2), and FnlC (Fnl3), respectively, of the E. coli O26 O antigen gene cluster (GenBank entries AAN60461, AAN60462 and AAN60463) and showed 83, 56, and 70% identity to FnlA (WbjB), FnlB (WbjC), and FnlC (WbjD), respectively, of the Pseudomonas aeruginosa O11 O-antigen gene cluster (GenBank entries AAF72954, AAF72955, and AAF72956), and showed 68, 42, and 50% identity to FnlA (Cap5E), FnlB (Cap5F), and FnlC (Cap5G), respectively, of the Staphylococcus aureus type 5 capsule gene cluster (GenBank entries AAC46088, AAC46089, and AAC46090). FnlA, FnlB, and FnlC are enzymes of the UDP-l-FucNAc biosynthesis pathway. Therefore, we propose l-FucNAc is a component of the E. coli O15 O antigen and orf5, orf6, and orf7 were named fnlA, fnlB, and fnlC, respectively.
(ii) Genes for O-unit processing.
orf2 and orf4 were the only two genes predicted to encode proteins with several transmembrane regions. Orf2 has 12 predicted transmembrane segments. It showed 30% identity or 52% similarity to the Wzx protein of E. coli K-12 (O16) (50) and showed 26% identity or 49% similarity to the Wzx protein of Shigella dysenteriae type 1 (22). Orf2 was related to the protein family Pfam01943 and COG2244 (E values of 2 × e−18 and 2 × e−12, respectively), which both include Wzx proteins of the O-antigen biosynthesis. These facts indicated that orf2 was the O-unit flippase gene (wzx).
Orf4 had 10 predicted transmembrane segments with a large periplasmic loop of 53 amino acid residues, which is the typical topology of Wzy proteins. It showed 22% identity or 43% similarity to the putative Wzy protein of S. boydii type 13 (15) and showed 20% identity or 41% similarity to the Wzy protein of S. boydii type 11 (51).
These facts indicated that orf4 was the O-antigen polymerase gene (wzy).
(iii) Putative glycosyltransferase genes.
The wecA gene located in the enterobacterial common antigen gene cluster is responsible for adding the first sugar GlcNAc onto the lipid acceptor UndP in the assembly of GlcNAc-containing O units of E. coli (1), whereas genes in the O-antigen gene cluster encode the remaining glycosyltransferases for synthesis of O unit.
Orf8 showed 72% identity to WbuB, a putative l-FucNAc transferase of the E. coli O26 O-antigen gene cluster (12), and was in the glycosyltransferase family 1 (pfam00534, E value = 2 × e−5). orf8, therefore also a putative l-FucNAc transferase gene, is downstream of the fnl gene set, as is wbuB in E. coli O26. We propose orf8 is an l-FucNAc transferase gene and named it wbuB.
Orf3 shared 43 to 53% similarity with many putative glycosyltransferases involved in polysaccharide or oligosaccharide antigen synthesis. Orf3 was also in the glycosyltransferase family 2 (pfam00535, E value = 8 × e−11). Therefore, orf3 is proposed to encode a glycosyltransferase and is named wbuS.
(iv) H repeat.
Orf1 was related to the H-repeat-associated protein of E. coli K-12. The sequence between positions 1,071 to 2,361 shared 96% identity to the H-repeat element of E. coli K-12. Therefore, this region was identified as an H-repeat element. Orf1, the putative H-repeat-associated protein, has no indel or stop codon, indicating that the H-repeat element was inserted recently.
(v) Putatively nonfunctional ORF.
orf9 shared 72% identity to wbuC of E. coli O26, which was proposed to be a gene remnant (12). Its length of 132 amino acids is also significantly less than those of normal O-antigen genes. Therefore, it is likely that orf9 is no longer functional and is named wbuC.
(vi) Intervening sequences next to galF and gnd.
The sequence of length 305 bp between the galF gene and the H-repeat element (positions 766 to 1,070) shares high-level identity (between 94 and 98%) to the sequences next to the galF gene in S. boydii type 4, type 5, and type 9 and E. coli K-12 (O16), O6, O26, and O128. The putative promoter sequence was found between positions 931 and 964 and shares 89% sequence identity and identical −35 and −10 signals and transcription initiation site to the promoter sequence of the O-antigen gene cluster in E. coli O7 (27). The 39-bp JUMP-Start sequence was found between positions 1,024 and 1,062 and shares 95 to 97.5% identity to those of reported E. coli and Shigella O-antigen gene clusters.
There is a 116-bp region between wbuC and gnd. No stem-loop structure or putative promoter sequence was found in this region, as is the case described in the O-antigen gene cluster of E. coli O113 (41).
Identification of E. coli O15 serogroup-specific genes.
Primers based on the proposed O-unit processing genes wzx and wzy, which are normally specific to different O antigen, were designed (Table 3). Two primer pairs for each gene were used to screen DNA pools of E. coli and Shigella reference strains from 186 different O serogroups (Table 2), of which reference strains for O serogroups O12, O40, O45, O51, O60, and O143 were reported to show serological cross-reactivity with the O15 antigen (14, 37). All of the four primer pairs based on wzx and wzy produced bands of correct sizes only with the pool containing E. coli O15 chromosomal DNA, and no band was detected with any other pools. The four primer pairs based on wzx and wzy, respectively (Table 3), were further used to detect the 33 E. coli O15 strains listed in Table 1 and 30 E. coli clinical isolates that belonged to other E. coli O serogroups (data not shown). A double-blind test was performed, and all 33 E. coli O15 strains from Table 1 gave the expected PCR products corresponding to each primer pair. In contrast, no PCR product was obtained from non-O15 strains, including those that showed serological cross-reactivity with the O15 serum. Combining the test in type strains and clinical isolates, all of the four primer pairs designed show high-level specificity to E. coli O15 strains.
By amplifying a dilution series of chromosomal DNA from E. coli O15 strain G1384, a sensitivity of 1 pg μl−1 was obtained for all of the four primer pairs. The sensitivities of primer pairs WL-950-WL-951 and WL-952-WL-953 were tested with pork meat samples or water contaminated with E. coli O15 strain G1384, and the detection limit was determined as 0.2 CFU g−1 for both primer pairs. The lysate of boiled cells was directly used as a template of PCR assay, and the total process can be finished within 16 h (17).
It was shown that the wzx and wzy genes are highly specific to E. coli O15 and can be used as target DNAs in the identification and detection of E. coli O15 strains belonging to different clonal groups, serotypes, and pathotypes. The O-antigen-specific PCR assay is faster and more accurate than conventional serotyping because cross-reactions with other O sera (here O40) that might lead to misinterpretation of the O type, as in the case of strain V32 (21), were clearly excluded by the PCR assay. Another advantage of the PCR typing method over serotyping is the fact that some types of capsular (K) antigens are known to block the lipopolysaccharide (O antigen) detection and the selection of K derivatives is sometimes required for serological detection of the O antigen in such strains (36). The O15-specific PCR assay could be extremely useful in future investigations of hospital and community outbreaks which have occurred with uropathogenic O15 strains (20, 33). The PCR assay bears the advantage that multiple samples of different origin can be rapidly investigated for the presence of the organism. In contrast, sample screening by O serotyping would require availability of an O15 specific antiserum and culturing of suspected E. coli isolates that is more laborious and time-consuming than the PCR assay.
Our data indicated that the genes encoding the O15 antigen could have been spread by horizontal gene transfer to unrelated strains of E. coli which were found to be heterogeneous in their flagellar and capsular antigens and which express different virulence markers. This possibility could be explored by investigating the genetic relationship between the O15 strains by comparing them for the nucleotide sequences of their housekeeping genes. As in previous studies, the H type was shown to be a good indicator for strains belonging to particular (patho)groups and virulence profiles, and the molecular analysis of fliC genes permits the grouping of NM strains that are frequently found among pathogenic E. coli isolates (6).
Acknowledgments
We thank James R. Johnson, Medical Service, Veterans Affairs Medical Center, Minneapolis, Minn.; Francine Grimont, Institut Pasteur, Paris, France; Eric Oswald, INRA, Toulouse, France; and Phillip Tarr, University of Washington, Seattle, for supplying E. coli O15 strains. We thank the Institute of Medical and Veterinary Science, Adelaide, Australia; the National Institute for Communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, People's Republic of China; and the Statens Serum Institute, Copenhagen, Denmark, for kindly supplying E. coli and Shigella type strains. We thank David Bastin for critical reading of the manuscript. We are grateful to Peter R. Reeves, School of Molecular and Microbial Biosciences, University of Sydney, Sydney, Australia, for helpful suggestions.
This study was supported by the Chinese National Science Fund for Distinguished Young Scholars (30125001), the NSFC General Program (30270029, 30370339, and 30370023), the NSFC International Cooperation Program (30125001), the 863 Program (2002AA2Z2051), the Cooperation Research Fund for Nankai and Tianjin Universities from Chinese Ministry of Education, and funding from the Science and Technology Committee of Tianjin City (013181711) to L.F. and L.W. L.B., G.K., and S.Z. were supported by funds from the European Commission project “Attaching and Effacing Escherichia coli Infections” (QLK2-CT-2000-00600).
REFERENCES
- 1.Alexander, D. C., and M. A. Valvano. 1994. Role of the rfe gene in the biosynthesis of the Escherichia coli O7-specific lipopolysaccharide and other O-specific polysaccharides containing N-acetylglucosamine. J. Bacteriol. 176:7079-7084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altschul, S. F., T. L. Madden, A. A. Schaffer, J. Zhang, Z. Zhang, W. Miller, and D. J. Lipman. 1997. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 25:3389-3402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bastin, D. A., and P. R. Reeves. 1995. Sequence and analysis of the O antigen gene (rfb) cluster of Escherichia coli O111. Gene 164:17-23. [DOI] [PubMed] [Google Scholar]
- 4.Bateman, A., L. Coin, R. Durbin, R. D. Finn, V. Hollich, S. Griffiths-Jones, A. Khanna, M. Marshall, S. Moxon, E. L. Sonnhammer, D. J. Studholme, C. Yeats, and S. R. Eddy. 2004. The Pfam protein families database. Nucleic Acids Res. 32(Database Issue):D138-D141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beutin, L., L. Bode, T. Richter, G. Peltre, and R. Stephan. 1984. Rapid visual detection of Escherichia coli and Vibrio cholerae Heat-labile enterotoxins by nitrocellulose enzyme-linked immunosorbent assay. J. Clin. Microbiol. 19:371-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beutin, L., G. Krause, S. Zimmermann, S. Kaulfuss, and K. Gleier. 2004. Characterization of Shiga toxin-producing Escherichia coli strains isolated from human patients in Germany over a 3-year period. J. Clin. Microbiol. 42:1099-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beutin, L., S. Zimmermann, and K. Gleier. 1996. Rapid detection and isolation of Shiga-like toxin (verocytotoxin)-producing Escherichia coli by direct testing of individual enterohemolytic colonies from washed sheep blood agar plates in the VTEC-RPLA assay. J. Clin. Microbiol. 34:2812-2814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blanco, M., J. E. Blanco, A. Mora, and J. Blanco. 1998. Distribution and characterization of faecal necrotoxigenic Escherichia coli CNF1+ and CNF2+ isolated from healthy cows and calves. Vet. Microbiol. 59:183-192. [DOI] [PubMed] [Google Scholar]
- 9.Blanco, M., J. E. Blanco, A. Mora, G. Dahbi, M. P. Alonso, E. A. Gonzalez, M. I. Bernardez, and J. Blanco. 2004. Serotypes, virulence genes, and intimin types of Shiga toxin (verotoxin)-producing Escherichia coli isolates from cattle in Spain and identification of a new intimin variant gene (eae-xi). J. Clin. Microbiol. 42:645-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bokete, T. N., T. S. Whittam, R. A. Wilson, C. R. Clausen, C.M. O'Callahan, S. L. Moseley, T. R. Fritsche, and P. I. Tarr. 1997. Genetic and phenotypic analysis of Escherichia coli with enteropathogenic characteristics isolated from Seattle children. J. Infect. Dis. 175:1382-1389. [DOI] [PubMed] [Google Scholar]
- 11.Cantey, J. R., and R. K. Blake. 1977. Diarrhea due to Escherichia coli in the rabbit: a novel mechanism. J. Infect. Dis. 135:454-462. [DOI] [PubMed] [Google Scholar]
- 12.D'Souza, J. M., L. Wang, and P. Reeves. 2002. Sequence of the Escherichia coli O26 O antigen gene cluster and identification of O26 specific genes. Gene 297:123-127. [DOI] [PubMed] [Google Scholar]
- 13.Eklund, M., F. Scheutz, and A. Siitonen. 2001. Clinical isolates of non-O157 Shiga toxin-producing Escherichia coli: serotypes, virulence characteristics, and molecular profiles of strains of the same serotype. J. Clin. Microbiol. 39:2829-2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ewing, W.H. 1986. The genus Escherichia, p. 93-134. In W. H. Ewing (ed.), Edwards and Ewing's identification of Enterobacteriaceae. Elsevier Science Publishing Co., New York, N.Y.
- 15.Feng, L., S. N. Senchenkova, J. Yang, A. S. Shashkov, J. Tao, H. Guo, G. Zhao, Y. A. Knirel, P. Reeves, and L. Wang. 2004. Structural and genetic characterization of the Shigella boydii type 13 O antigen. J. Bacteriol. 186:383-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Furrer, B., U. Candrian, and J. Luthy. 1990. Detection and identification of Escherichia coli producing heat-labile enterotoxin type I by enzymatic amplification of a specific DNA fragment. Lett. Appl. Microbiol. 10:31-34. [DOI] [PubMed] [Google Scholar]
- 17.Guo, H., L. Feng, J. Tao, C. Zhang, and L. Wang. 2004. Identification of Escherichia coli O172 O-antigen gene cluster and development of a serogroup-specific PCR assay. J. Appl. Microbiol. 97:181-190. [DOI] [PubMed] [Google Scholar]
- 18.Henikoff, S., J. G. Henikoff, W. J. Alford, and S. Pietrokovski. 1995. Automated construction and graphical presentation of protein blocks from unaligned sequences. Gene 163:GC17-GC26. [DOI] [PubMed] [Google Scholar]
- 19.Johnson, J. R., M. A. Kuskowski, K. Owens, A. Gajewski, and P. L. Winokur. 2003. Phylogenetic origin and virulence genotype in relation to resistance to fluoroquinolones and/or extended-spectrum cephalosporins and cephamycins among Escherichia coli isolates from animals and humans. J. Infect. Dis. 188:759-768. [DOI] [PubMed] [Google Scholar]
- 20.Johnson, J. R., A. R. Manges, T. T. O'Bryan, and L. W. Riley. 2002. A disseminated multidrug-resistant clonal group of uropathogenic Escherichia coli in pyelonephritis. Lancet 359:2249-2251. [DOI] [PubMed] [Google Scholar]
- 21.Johnson, J. R., A. L. Stell, T. T. O'Bryan, M. Kuskowski, B. Nowicki, C. Johnson, J. N. Maslow, A. Kaul, J. Kavle, and G. Prats. 2002. Global molecular epidemiology of the O15:K52:H1 extraintestinal pathogenic Escherichia coli clonal group: evidence of distribution beyond Europe. J. Clin. Microbiol. 40:1913-1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klena, J. D., and C. A. Schnaitman. 1993. Function of the rfb gene cluster and the rfe gene in the synthesis of O antigen by Shigella dysenteriae 1. Mol. Microbiol. 9:393-402. [DOI] [PubMed] [Google Scholar]
- 23.Kobayashi, H., A. Miura, H. Hayashi, T. Ogawa, T. Endo, E. Hata, M. Eguchi, and K. Yamamoto. 2003. Prevalence and characteristics of eae-positive Escherichia coli from healthy cattle in Japan. Appl. Environ. Microbiol. 69:5690-5692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krogh, A., B. Larsson, G. von Heijne, and E. L. Sonnhammer. 2001. Predicting transmembrane protein topology with a hidden Markov model: application to complete genomes. J. Mol. Biol. 305:567-580. [DOI] [PubMed] [Google Scholar]
- 25.Leung, P. H., W. C. Yam, W. W. Ng, and J. S. Peiris. 2001. The prevalence and characterization of verotoxin-producing Escherichia coli isolated from cattle and pigs in an abattoir in Hong Kong. Epidemiol. Infect. 126:173-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Machado, J., F. Grimont, and P. A. Grimont. 2000. Identification of Escherichia coli flagellar types by restriction of the amplified fliC gene. Res. Microbiol. 151:535-546. [DOI] [PubMed] [Google Scholar]
- 27.Marolda, C. L., and M. A. Valvano. 1998. Promoter region of the Escherichia coli O7-specific lipopolysaccharide gene cluster: structural and functional characterization of an upstream untranslated mRNA sequence. J. Bacteriol. 180:3070-3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nataro, J.P. 1995. Enteroaggregative and diffusely adherent Escherichia coli, p. 727-737. In M. J. Blaser, P. D. Smith, J. I. Ravdin, H. B. Greenberg, and R. L. Guerrant (ed.), Infections of the gastrointestinal tract. Raven Press, New York, N.Y.
- 29.O'Brien, A. D., and R. K. Holmes. 1996. Protein toxins of Escherichia coli and Salmonella, p. 2788-2802. In F. C. Neidhardt, R. Curtiss III, J. L. Ingraham, E. C. C. Lin, K. B. Low, B. Magasanik, W. S. Reznikoff, M. Riley, M. Schaechter, and H. E. Umbarger (ed.), Escherichia coli and Salmonella: cellular and molecular biology, 2nd ed. American Society for Microbiology, Washington, D.C.
- 30.Ochman, H., and R. K. Selander. 1984. Standard reference strains of Escherichia coli from natural populations. J. Bacteriol. 157:690-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okerman, L., and L. A. Devriese. 1985. Biotypes of enteropathogenic Escherichia coli strains from rabbits. J. Clin. Microbiol. 22:955-958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olesen, B., H. J. Kolmos, F. Orskov, and I. Orskov. 1995. A comparative study of nosocomial and community-acquired strains of Escherichia coli causing bacteraemia in a Danish University Hospital. J. Hosp. Infect. 31:295-304. [DOI] [PubMed] [Google Scholar]
- 33.O'Neill, P. M., C. A. Talboys, A. P. Roberts, and B. S. Azadian. 1990. The rise and fall of Escherichia coli O15 in a London teaching hospital. J. Med. Microbiol. 33:23-27. [DOI] [PubMed] [Google Scholar]
- 34.Orden, J. A., S. Q. J. Ruiz, D. Cid, S. Garcia, and R. de la Fuente. 1999. Prevalence and characteristics of necrotoxigenic Escherichia coli (NTEC) strains isolated from diarrhoeic dairy calves. Vet. Microbiol. 66:265-273. [DOI] [PubMed] [Google Scholar]
- 35.Orskov, F. 1952. Antigenic relationships between H antigens 1-22 of Escherichia coli and Wramby's H antigens 23w-36w. Acta Pathol. Microbiol. Scand. 32:241-244. [PubMed] [Google Scholar]
- 36.Orskov, F., and I. Orskov. 1984. Serotyping of Escherichia coli. Methods Microbiol. 14:43-112. [Google Scholar]
- 37.Orskov, F., I. Orskov, B. Jann, and K. Jann. 1977. Serology, chemistry, and genetics of O and K antigens of Escherichia coli. Bacteriol. Rev. 41:667-710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Orskov, I., and F. Orskov. 1978. Significance of surface antigens in relation to enterotoxigenicity of Escherichia coli, p. 134-141. In Ö. Ouchterlony and J. Holmgren (ed.), Cholera and related diarrheas: molecular aspects of a global health problem. S. Karger, Basel, Switzerland.
- 39.Oswald, E., H. Schmidt, S. Morabito, H. Karch, O. Marches, and A. Caprioli. 2000. Typing of intimin genes in human and animal enterohemorrhagic and enteropathogenic Escherichia coli: characterization of a new intimin variant. Infect. Immun. 68:64-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Padola, N. L., M. E. Sanz, J. E. Blanco, M. Blanco, J. Blanco, A. I. Etcheverria, G. H. Arroyo, M. A. Usera, and A. E. Parma. 2004. Serotypes and virulence genes of bovine Shiga toxigenic Escherichia coli (STEC) isolated from a feedlot in Argentina. Vet. Microbiol. 100:3-9. [DOI] [PubMed] [Google Scholar]
- 41.Paton, A. W., and J. C. Paton. 1999. Molecular characterization of the locus encoding biosynthesis of the lipopolysaccharide O antigen of Escherichia coli serotype O113. Infect. Immun. 67:5930-5937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peeters, J. E., R. Geeroms, and F. Orskov. 1988. Biotype, serotype, and pathogenicity of attaching and effacing enteropathogenic Escherichia coli strains isolated from diarrheic commercial rabbits. Infect. Immun. 56:1442-1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Prada, J., G. Baljer, J. De Rycke, H. Steinruck, S. Zimmermann, R. Stephan, and L. Beutin. 1991. Characteristics of alpha-hemolytic strains of Escherichia coli isolated from dogs with gastroenteritis. Vet. Microbiol. 29:59-73. [DOI] [PubMed] [Google Scholar]
- 44.Prats, G., F. Navarro, B. Mirelis, D. Dalmau, N. Margall, P. Coll, A. Stell, and J. R. Johnson. 2000. Escherichia coli serotype O15:K52:H1 as a uropathogenic clone. J. Clin. Microbiol. 38:201-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pupo, G. M., D. K. Karaolis, R. Lan, and P. R. Reeves. 1997. Evolutionary relationships among pathogenic and nonpathogenic Escherichia coli strains inferred from multilocus enzyme electrophoresis and mdh sequence studies. Infect. Immun. 65:2685-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robins-Browne, R. M., A. M. Tokhi, L. M. Adams, and V. Bennett-Wood. 1994. Host specificity of enteropathogenic Escherichia coli from rabbits: lack of correlation between adherence in vitro and pathogenicity for laboratory animals. Infect. Immun. 62:3329-3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rutherford, K., J. Parkhill, J. Crook, T. Horsnell, P. Rice, M. A. Rajandream, and B. Barrell. 2000. Artemis: sequence visualization and annotation. Bioinformatics 16:944-945. [DOI] [PubMed] [Google Scholar]
- 48.Schmidt, H., C. Knop, S. Franke, S. Aleksic, J. Heesemann, and H. Karch. 1995. Development of PCR for screening of enteroaggregative Escherichia coli. J. Clin. Microbiol. 33:701-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Staden, R. 1996. The Staden sequence analysis package. Mol. Biotechnol. 5:233-241. [DOI] [PubMed] [Google Scholar]
- 50.Stevenson, G., B. Neal, D. Liu, M. Hobbs, N. H. Packer, M. Batley, J. W. Redmond, L. Lindquist, and P. Reeves. 1994. Structure of the O antigen of Escherichia coli K-12 and the sequence of its rfb gene cluster. J. Bacteriol. 176:4144-4156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tao, J., L. Feng, H. Guo, Y. Li, and L. Wang. 2004. The O-antigen gene cluster of Shigella boydii O11 and functional identification of its wzy gene. FEMS Microbiol. Lett. 234:125-132. [DOI] [PubMed] [Google Scholar]
- 52.Tatusov, R. L., D. A. Natale, I. V. Garkavtsev, T. A. Tatusova, U. T. Shankavaram, B. S. Rao, B. Kiryutin, M. Y. Galperin, N. D. Fedorova, and E. V. Koonin. 2001. The COG database: new developments in phylogenetic classification of proteins from complete genomes. Nucleic Acids Res. 29:22-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tauschek, M., R. A. Strugnell, and R. M. Robins-Browne. 2002. Characterization and evidence of mobilization of the LEE pathogenicity island of rabbit-specific strains of enteropathogenic Escherichia coli. Mol. Microbiol. 44:1533-1550. [DOI] [PubMed] [Google Scholar]
- 54.Thompson, J. D., D. G. Higgins, and T. J. Gibson. 1994. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 22:4673-4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Toth, I., F. Herault, L. Beutin, and E. Oswald. 2003. Production of cytolethal distending toxins by pathogenic Escherichia coli strains isolated from human and animal sources: establishment of the existence of a new cdt variant (type IV). J. Clin. Microbiol. 41:4285-4291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Trabulsi, L. R., R. Keller, and G. T. Tardelli. 2002. Typical and atypical enteropathogenic Escherichia coli. Emerg. Infect. Dis. 8:508-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang, L., and P. R. Reeves. 1998. Organization of Escherichia coli O157 O antigen gene cluster and identification of its specific genes. Infect. Immun. 66:3545-3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang, L., D. Rothemund, H. Curd, and P. R. Reeves. 2003. Species-wide variation in the Escherichia coli flagellin (H-antigen) gene. J. Bacteriol. 185:2936-2943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wolf, M. K. 1997. Occurrence, distribution, and associations of O and H serogroups, colonization factor antigens, and toxins of enterotoxigenic Escherichia coli. Clin. Microbiol. Rev. 10:569-584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yamazaki, M., M. Saito, K. Inuzuka, S. Shima, H. Taniwaki, and K. Ito. 1997. eaeA genes in Escherichia coli derived from Japanese patients with sporadic diarrhea. Kansenshogaku. Zasshi. 71:1059-1065. [DOI] [PubMed] [Google Scholar]
- 61.Zhang, W. L., B. Kohler, E. Oswald, L. Beutin, H. Karch, S. Morabito, A. Caprioli, S. Suerbaum, and H. Schmidt. 2002. Genetic diversity of intimin genes of attaching and effacing Escherichia coli strains. J. Clin. Microbiol. 40:4486-4492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhu, C., T. S. Agin, S. J. Elliott, L. A. Johnson, T. E. Thate, J. B. Kaper, and E. C. Boedeker. 2001. Complete nucleotide sequence and analysis of the locus of enterocyte Effacement from rabbit diarrheagenic Escherichia coli RDEC-1. Infect. Immun. 69:2107-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]