Abstract
Background: Mallet finger is a common injury of the extensor tendon insertion causing an extension lag of the distal interphalangeal joint. Methods: We reviewed the most current literature on the epidemiology, diagnosis, and management of mallet finger injuries focusing on the indications and outcomes of surgical intervention. Results: Nonoperative management has been advocated for almost all mallet finger injuries; however, complex injuries are usually treated surgically. There is still controversy regarding the absolute indications for surgical intervention. Conclusions: Although surgery is generally indicated in the case of mallet fractures involving more than one-third of the articular surface as well as in all patients who develop volar subluxation of the distal phalanx, a significant advantage of surgical management even in those complicated cases has yet to be clearly proven.
Keywords: mallet finger, extensor tendon, bony mallet, distal interphalangeal joint, distal phalanx fracture
Introduction
The term mallet finger refers to a common injury of the terminal extensor mechanism resulting in loss of active extension at the level of the distal interphalangeal joint.30 Frequently encountered in sports, the injury results following forceful flexion or hyperextension of an extended distal phalanx, causing extensor tendon disruption, either isolated or in combination with a distal phalanx avulsion fracture.6,30 The resulting deformity is an extension lag at the distal interphalangeal joint. If left untreated, a mallet finger can be complicated by development of osteoarthritis at the distal interphalangeal joint or possibly hyperextension (swan-neck) deformity at the level of the proximal interphalangeal joint as a result of proximal retraction of the central slip.28 The treatment of the mallet finger ranges from nonoperative with prolonged splinting and immobilization to open reduction and rigid fixation depending on the extent of the injury as well as the time from injury to presentation.4,6 Some of the indications for surgical intervention remain controversial to this date.4,29
Epidemiology, Classification, and Diagnosis
Mallet finger injuries are frequently sustained during either work or participation in sports.4,28-30 A recent large retrospective study on the incidence of tendinous and ligamentous injuries confirmed the previously described findings that mallet finger is most common in young males.7 Incidence begins to drop after the fifth decade while at that point it becomes equal to the incidence in females. The injury usually involves the long, ring, or small finger of the dominant hand4,7 and can occur not only with major but in some cases with minor inflicted force.4,7,15 A noticed high incidence of mallet finger in a familial distribution has suggested a genetic disposition making individuals susceptible to sustaining such injuries even following minor trauma, although this has not been proven.15
Although in the majority of cases mallet injuries are closed, open mallet fingers can present as well, often as a result of crash injuries or lacerations in the dorsal aspect of the distal phalanx.4,6,28,30 Mallet injuries are usually classified according to the Doyle system9 into 4 types: closed injury (with or without avulsion fracture) (type 1), open injury with tendon laceration (type 2), open injury with tendon substance and soft tissue loss (type 3), and mallet fracture (type 4), which is further subdivided into three types: transphyseal fracture in children (type A), hyperflexion injury with involvement of 20% to 50% of the articular surface (type B), and hyperextension injury involving more than 50% of the articular surface (type C). A different classification system described by Wehbe and Schneider35 is also frequently used describing the severity of the injuries: no distal interphalangeal joint subluxation (type 1), distal interphalangeal joint subluxation (type 2), and physeal or epiphyseal injuries (type 3), while all injuries are further subdivided based on the involvement of articular surface: less than 30% (subtype A), 30% to 60% (subtype B), and more than 60% (subtype C).
Reaching the diagnosis of mallet finger is relatively straightforward. The main complains patients present with are pain in the affected joint, deformity, and a functional deficit.4,30 The history usually provides the typical mechanism of injury, ie, forced flexion or hyperextension of the distal interphalangeal joint, and physical exam will usually reveal an extension lag at the distal interphalangeal joint.4,30 In the case of chronic injuries, hyperextension at the proximal interphalangeal joint might develop as a result of migration of the extensor apparatus proximally and increased extension tone across the proximal interphalangeal joint. Once the extension force by the central slip and lateral bands overcomes the flexion force by the superficial and deep flexor tendon across the proximal interphalangeal joint, a Swan neck deformity is created.3,4,30 Radiographic images of the affected finger will assess the existence of a concomitant avulsion fracture and the possibility of subluxation of the distal phalanx.3 Regardless of whether the injury only involves the extensor tendon or the base of the distal phalanx as well, the main functional deficit will be an extension lag.4 In either case, the goal of treatment is restoring the normal joint anatomy so that the tendon can heal with minimal residual extension lag.4 In the pediatric patient population specifically, one must also rule out a Seymour-type fracture as the mechanism of injury, and presentation in the acute setting is similar to that of mallet finger.1 Seymour fractures are open, displaced distal phalangeal fractures involving the physis with an associated nail bed laceration and sometimes part of the germinal matrix of the nail complex interposed in the fracture site. On imaging, Seymour fractures are extra-articular with widening of the physis and variable displacement between the epiphysis and metaphysis. Treatment is always surgical as the entrapment of the germinal matrix in the fracture site can lead to nail plate deformity, physeal arrest, or chronic osteomyelitis.1
Treatment Options
Nonoperative management has been suggested as first-line treatment option for almost all mallet finger injuries.35 It is currently considered the standard of care for all injuries with no associated fracture, no volar subluxation of the distal phalanx, or cases with involvement of less than one-third of the articular surface.3,4,29 Treatment involves complete immobilization of the involved joint in full extension or slight overextension for at least 6 weeks, followed by 2 weeks of nighttime splinting.3,4,6,9,28,29,35 Importance of compliance with maintaining complete and continuous immobilization of the affected joint cannot be overstressed, as if the distal interphalangeal joint is allowed to flex during the course of 6 weeks, the course needs to be restarted.3,4,6,9,28,29,35 Despite the initial concept that the proximal interphalangeal joint had to remain immobilized as well, it is now well accepted that flexion of the proximal interphalangeal joint does not result in retraction of the proximal part of the extensor tendon and thus does not affect the healing process.17
Despite the many different types of splints available for the management of mallet finger injuries, none has been proven to be superior to another.4,6,29 Regardless of the material it is made of or whether it is applied on the volar or dorsal aspect of the finger, any type of splint maintaining the distal interphalangeal joint in extension and subsequently the ruptured extensor tendon in apposition is effective.4,6,29 The most commonly used one is the stack splint (plastic or custom-made thermoplastic) while aluminum foam (placed on dorsally or volarly) and the Abouna metal splint are also frequently used. Several studies have been performed to compare the different types of splints.4,6,29 Two recent prospective, randomized clinical trials comparing different types of splints found no difference in the residual extension lag following treatment, although the custom-made thermoplastic splint was found to be less likely to result in treatment failure and was associated with higher treatment compliance rates.23,26 Complications associated with splint application include skin ulceration of maceration, development of allergic reaction to tape, and splint-related pain.17,23,26
Although nonoperative management appears to be the mainstay of treatment for closed injuries only involving the extensor tendon, surgery does have a role in cases of patients with poor compliance to continuous splinting or certain professionals (musicians, surgeons).5 In those cases, the distal interphalangeal joint is fixed in extension using a K-wire, which is removed after 8 weeks to be followed by 2 weeks of external splinting during nighttime.3 Furthermore, operative management has been suggested for all open injuries, using a K-wire for immobilization of the distal interphalangeal joint and direct repair of the extensor tendon, although only few reports exist in the literature.3,22 Alternatively, the skin edges and underlying lacerated tendon can be approximated with a continuous running suture and an extension splint applied for 6 weeks.9
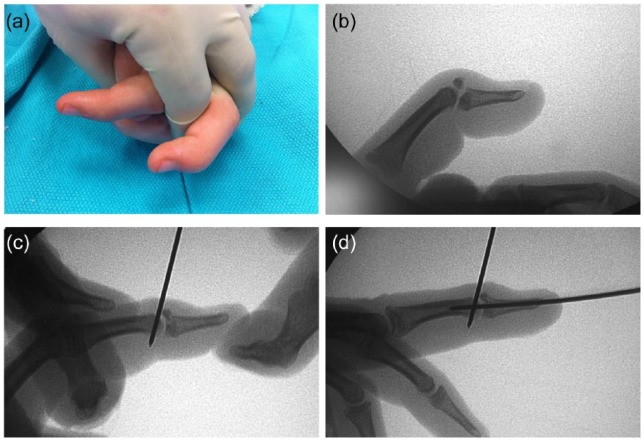
In the case of mallet finger associated with an underlying distal phalanx fracture, surgery is recommended if the fracture involves more than 30% of the articular surface or if there is palmar subluxation of the distal phalanx.3,4,6,9,28-30,35 Options for surgical management include either closed reduction with percutaneous pinning or open reduction and fixation. Closed reduction can be performed with the use of an extension block K-wire to reduce the fracture fragment and stabilize the extensor tendon followed by placement of another K-wire across the distal interphalangeal joint to secure the reduction (Figure 1).12 Several variations of the technique have been described in the literature with very good results.4,6 Wire fixation of the distal interphalangeal joint is usually followed by 6 weeks of immobilization, although some techniques do allow earlier mobilization as they use compression fixation pins36 or the use of a single K-wire shaped into an umbrella handle to maintain reduction of the fracture fragment despite immediate postoperative mobilization.27
Figure 1.
Management of closed bony mallet finger injury.
Note. A 13-year-old male was referred to clinic 1 week after sustaining a hyperflexion injury in his right long finger while playing football. On examination, he was noted to have tenderness and swelling over the dorsal aspect of the distal phalanx, a flexion deformity, as well as complete loss of active extension of the distal interphalangeal joint (a). On imaging, he was found to have a bony mallet injury of the right long finger with 50% joint surface in the dorsal fragment, without volar subluxation of the distal fragment (b). Based on the extent of the injury involving more than 30% of the articular surface and following discussion with the family, we decided to proceed with closed reduction and percutaneous pinning of the fracture. At the time of the operation, an extension block wire was initially placed, entering at the dorsal middle phalanx just behind the fracture fragment, keeping the fragment and extensor tendon into position. The distal phalanx was extended to reduce the dorsal fragment (c). A K-wire was then placed through the distal phalanx, crossing the interphalangeal joint to secure the reduction. The tip of the wire was buried underneath the skin of the distal phalanx (d). The postoperative course was uneventful, and the patient regained excellent function after removal of the percutaneous wires after 6 weeks of immobilization of the joint.
Open reduction techniques for mallet injuries associated with distal phalanx fracture have also been used with similar efficacy.3,6,30,35 The use of open technique offers better access to the fracture site with direct visualization of the fracture fragments and theoretically easier reduction and fixation.4 The open reduction and fixation can be performed under direct vision using a K-wire driven across the distal interphalangeal joint as well as the fracture fragment.10 Fixation of the fracture has also been described using either a hook plate32 or screws.20 Besides rigid fixation, techniques using pull-through wires2 or sutures8 have also been described. Although open repair techniques are reported to have good results, they appear to have a higher complication rate compared with closed repair techniques,3,4,6,9,29,35 stressing the need for delicate soft tissue handling and meticulous surgical technique while performing open repair of mallet finger injuries.3,4
Chronic mallet finger represents a different clinical entity defined as mallet injuries seen at least 4 weeks after the injury.3 As with acute injuries, treatment options include prolonged external splinting as well as surgical intervention. Although several studies report excellent results arguing for at least a trial of splinting for all chronic mallet injuries,3,5,25 surgical intervention is recommend if there is an extensor lag of 40 degrees or if injury limits function in an effort to improve active distal interphalangeal joint extension.3,5,25 Among the most commonly performed procedures, shortening of the terminal extensor tendon entails transection and immediate repair of the extensor tendon near the dorsal interphalangeal joint allowing the resultant scar formation to correct the flexion deformity.21 Another technique addressing the extension lag seen in chronic mallet injuries is tenodermodesis, which involves wedge resection of the scar on the distal aspect of the affected finger along with the underlying tendon and approximation of all tissues together with interrupted sutures.14 Alternatively, chronic mallet finger can be managed with central slip tenotomy13 or with reconstruction of the spiral oblique retinacular ligament using a tendon graft.33 Surgical procedures performed for chronic mallet finger aim to address the length loss of the extensor tendon system and ultimately the resulting imbalance between flexion and extension systems across the proximal and distal interphalangeal joints.3,5,25
In case of persistent symptoms, deformity, and functional impairment following splinting and surgical management, arthrodesis is the primary salvage procedure used.3,4,6,9,28-30,35 Fixation of the distal interphalangeal joint can be performed in this case using K-wires or intramedullary screws while the joint is usually fixed in slight flexion to increase function.18 Arthrodesis has been reported to have good results in mallet injuries and is effective in treating chronic pain associated with this condition.3,9,35
Discussion
Although, nonoperative management has been advocated for almost all mallet finger injuries,35 complex injuries are usually treated surgically.3,4,9,29 There is still controversy regarding the absolute indications for surgical intervention. The most commonly reported indications for surgical intervention are open mallet finger injuries, patients who are incompliant or unable to adhere to continuous extension splinting, and cases with a large dorsal fracture fragment or palmar subluxation of the distal phalanx.11
Multiple different techniques for surgical management of mallet finger injuries have been described2,8,10,12-14,20,21,25,27,32,33,36 with good results. A head-to-head comparison of different techniques was performed in a randomized cadaveric study assessing the stability of fracture reduction.8 The group of injured fingers treated with pull-through sutures was the only one where no irreversible loss of fracture reduction was seen following mobilization of the joint after fixation. Loss of reduction was seen in half of the injuries fixed with figure-of-8 wires, two-thirds of the fingers fixed with pull-through wires, and all the fingers fixed with K-wires.8 Regardless of whether the injury is limited to the extensor tendon or it also involves a fragment of the distal phalanx, the durable proper anatomic alignment of involved structures is essential for the healing process.29,34 In isolated tendon injuries, the distal tendon stump is usually friable and retracted, making suturing difficult. In cases with an associated avulsion fracture, wire fixation requires hitting the point of a small triangular fragment, making closed or open manipulation difficult and a lasting reduction challenging.34
In addition, operative management of mallet finger is associated with a high rate of complications.19,29,31,34 The soft tissues surrounding the distal interphalangeal joint are thin, and the germinal matrix of the nail is nearby and easily damaged. Both closed and open repairs can be complicated by infection, hardware failure, nail deformities, a persistent extension lag, and the need for additional surgeries.19 In a retrospective study comparing complications following splinting versus operative repair of mallet finger injuries, overall complication rate for splinting was 45% versus 53% for cases managed operatively. However, complications associated with splinting were mostly skin related and transient as opposed to complications associated with operative interventions which persisted in a mean follow-up of 38 months.31
Despite the numerous studies describing the different techniques for operative management of bony mallet finger injuries, there are no studies comparing operative management to external splinting.29 Nonoperative management of mallet fractures involving more than one-third of the articular surface has been found to have similar long-term results regardless of whether the initial injury also included palmar subluxation of the distal phalanx.19 In a retrospective study of 22 closet mallet finger fractures treated with extension splinting only, patients reported minimal difficulties with activities of daily living and high satisfaction with treatment outcome 2 years after the injury while no statistically significant differences could be identified between the isolated fracture group and the group with associated subluxation of the distal phalanx.16 Furthermore, another retrospective study of 31 patients with mallet finger deformities treated with extension splinting alone reported 90% patient satisfaction rate, while 68% of patients reported no impairment in precision functions 5 years after their injury.24 Based on the above, one could argue that subluxation is not necessarily an absolute indication for operative management, especially taking into consideration the minimal complications associated with splinting.29
The present study carries certain limitations. First, as this is a review of the existing literature that mostly consists of single-institution small case series, case reports, and retrospective reviews, we must consider the possibility of publication bias as well as surgeon bias with regard to selection of treatment plan impacting the data. Furthermore, one must take into consideration that these studies cannot control for many factors that influence the decision making for surgical intervention; one could argue that patients who decide to have surgery are a different cohort to those who do not have surgery, making it problematic to read the data in reverse. Another component of the decision-making algorithm is the patient’s tolerance for intervention, possible complications, or having protruding hardware for several weeks, which is also very hard to measure. In addition, as the information we could find in each study was heterogeneous, we were not able to perform subgroup analysis to identify comorbidities that could potentially affect the surgical outcome. Most importantly, as we did not have access to the raw data from all the studies, we were not able to generate well-organized treatment guidelines for the management of mallet finger injuries.
At the same time, based on the extensive review of the existing literature, we can definitely recommend a delicate balance between intervention–complications–aesthetics of the hand. The body has a remarkable ability to heal these mallet fractures even with a fair amount of displacement, and assuming that splinting is strictly adhered to, the range of motion and extension lag results are not significantly different following operative versus nonoperative management. That being said, the deformity resulting when displaced fractures are allowed to heal without reduction is much more prominent compared with nondisplaced fractures.
In conclusion, mallet finger injuries are common injuries of the extensor tendon mechanism. In the majority of cases, management is nonoperative with prolonged extension splinting of the dorsal interphalangeal joint. Although surgery is generally indicated in the case of mallet fractures involving more than one-third of the articular surface as well as in all patients who develop volar subluxation of the distal phalanx, a significant advantage of surgical approach even in those complicated cases has yet to be clearly proven. Surgical interventions often have a high incidence of complications while nonoperative management has been found to result in minimal functional impairment of the affected joint. Future studies will need to assess the indications for surgical intervention and the optimal treatment for complex mallet injuries where the optimal treatment modality is still under debate.
Footnotes
Ethical Approval: The single case report that appears in Figure 1 describes a patient who received the standard of care for his injury; hence, an approval from the Ethics Committee of our institution was not obtained.
Statement of Human and Animal Rights: No experiments on animals were performed for this study. No experimental procedures were performed in any human subject for this study.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Abzug JM, Kozin SH. Seymour fractures. J Hand Surg Am. 2013;38(11):2267-2270. [DOI] [PubMed] [Google Scholar]
- 2. Bauze A, Bain GI. Internal suture for mallet finger fracture. J Hand Surg Br. 1999;24:668-692. [DOI] [PubMed] [Google Scholar]
- 3. Bendre AA, Hartigan BJ, Kalainov DM. Mallet finger. J Am Acad Orthop Surg. 2005;13(5):336-344. [DOI] [PubMed] [Google Scholar]
- 4. Bloom JMP, Khouri JS, Hammert WC. Current concepts in the evaluation and treatment of mallet finger injury. Plast Reconstr Surg. 2013;132(4):560e-566e. [DOI] [PubMed] [Google Scholar]
- 5. Brzeziensky MA, Schneider LH. Extensor tendon injuries at the distal interphalangeal joint. Hand Clin. 1995;11:373-386. [PubMed] [Google Scholar]
- 6. Cheung JPY, Fung B, Ip WY. Review on mallet finger treatment. Hand Surg. 2012;17(3):439-447. [DOI] [PubMed] [Google Scholar]
- 7. Clayton RA, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39(12):1338-1344. [DOI] [PubMed] [Google Scholar]
- 8. Damron TA, Engber WD, Lange RH, et al. Biomechanical analysis of mallet finger fracture fixation techniques. J Hand Surg Am. 1993;18:600-608. [DOI] [PubMed] [Google Scholar]
- 9. Doyle JR. Extensor tendons: acute injuries. In: Green DP, Pederson CW, Hotchkiss RN, eds. Green’s Operative Hand Surgery. 4th ed. New York, NY: Churchill Livingstone; 1999:195-198. [Google Scholar]
- 10. Fritz D, Lutz M, Arora R, Gabl M, Wambacher M, Pechlaner S. Delayed single Kirschner wire compression technique for mallet fracture. J Hand Surg Br. 2005;30:180-184. [DOI] [PubMed] [Google Scholar]
- 11. Hanz KR, Saint-Cyr M, Semmler MJ, Rohrich RJ. Extensor tendon injuries: acute management and secondary reconstruction. Plast Reconstr Surg. 2008;121(3):109-120. [DOI] [PubMed] [Google Scholar]
- 12. Hofmeister EP, Mazurek MT, Shin AY, Bishop AT. Extension block pinning for large mallet fractures. J Hand Surg Am. 2003. 28:453-459. [DOI] [PubMed] [Google Scholar]
- 13. Houpt P, Dijkstra R, Storm van Leeuwen JB. Fowler’s tenotomy for mallet deformity. J Hand Surg Br. 1993;18:499-500. [DOI] [PubMed] [Google Scholar]
- 14. Iselin F, Levame J, Godoy J. A simplified technique for treating mallet fingers: tenodermodesis. J Hand Surg Am. 1977;2:118-121. [DOI] [PubMed] [Google Scholar]
- 15. Jones NF, Peterson J. Epidemiologic study of the mallet finger deformity. J Hand Surg Am. 1988;13(3):334-338. [DOI] [PubMed] [Google Scholar]
- 16. Kalainov DM, Hoepfner PE, Hartigan BJ, Carroll C, IV, Genuario J. Nonsurgical treatment of closed mallet finger fractures. J Hand Surg Am. 2005;30(3):580-586. [DOI] [PubMed] [Google Scholar]
- 17. Katzman BM, Klein DM, Mesa J, Geller J, Caligiuri DA. Immobilization of the mallet finger: effects on the extensor tendon. J Hand Surg. 1990;24:80-84. [DOI] [PubMed] [Google Scholar]
- 18. Katzman SS, Gibeault JD, Dickson K, Thompson JD. Use of a Herbert screw for interphalangeal joint arthrodesis. Clin Orthop. 1993;296:127-132. [PubMed] [Google Scholar]
- 19. King HJ, Shin SJ, Kang ES. Complications of operative treatment for mallet fractures of the distal phalanx. J Hand Surg Br. 2001;26(1):28-31. [DOI] [PubMed] [Google Scholar]
- 20. Kronlage SC, Faust D. Open reduction and screw fixation of mallet fractures. J Hand Surg Br. 2004;29:135-138. [DOI] [PubMed] [Google Scholar]
- 21. Lind J, Hansen LB. Abbrevatio: a new operation for chronic mallet finger. J Hand Surg Br. 1989;14:347-349. [DOI] [PubMed] [Google Scholar]
- 22. Nakamura K, Nanjyo B. Reassessment of surgery for mallet finger. Plast Reconstr Surg. 1994;93:141-149. [PubMed] [Google Scholar]
- 23. O’Brien LJ, Bailey MJ. Single blind, prospective, randomized controlled trial comparing dorsal aluminum and custom thermoplastic splints to stack splint for acute mallet finger. Arch Phys Med Rehabil. 2011;92(2):191-198. [DOI] [PubMed] [Google Scholar]
- 24. Okafor B, Mbubaegbu C, Munshi I, Williams DJ. Mallet deformity of the finger. Five-year follow-up of conservative treatment. J Bone Joint Surg Br. 1997;79(4):544-547. [DOI] [PubMed] [Google Scholar]
- 25. Patel MR, Desai SS, Bassini-Lipson L. Conservative management of chronic mallet finger. J Hand Surg Am. 1986;11:570-573. [DOI] [PubMed] [Google Scholar]
- 26. Pike J, Mulpuri K, Metzger M, Ng G, Wells N, Goetz T. Blinded, prospective, randomized clinical trial comparing volar, dorsal, and custom thermoplastic splinting in treatment of acute mallet finger. J Hand Surg Am. 2010;35(4):580-588. [DOI] [PubMed] [Google Scholar]
- 27. Rocchi L, Genitiempo M, Fanfani F. Percutaneous fixation of mallet fractures by the “umbrella handle” technique. J Hand Surg Br. 2006;31:407-412. [DOI] [PubMed] [Google Scholar]
- 28. Rockwell WB, Butler PN, Byrne BA. Extensor tendon: anatomy, injury and reconstruction. Plast Reconstr Surg. 2000;106:1592-1603. [DOI] [PubMed] [Google Scholar]
- 29. Smit JM, Beets MR, Zeebregts CJ, Rood A, Welters CF. Treatment options for mallet finger: a review. Plast Reconstr Surg. 2010;126(5):1624-1629. [DOI] [PubMed] [Google Scholar]
- 30. Stack HG. Mallet finger. Hand. 1969;1:83-89. [Google Scholar]
- 31. Stern PJ, Kastrup JJ. Complications and prognosis of treatment of mallet finger. J Hand Surg Am. 1998;13(3):329-334. [DOI] [PubMed] [Google Scholar]
- 32. Teoh LC, Lee JY. Mallet fractures: a novel approach to internal fixation using a hook plate. J Hand Sug Eur. 2007;32:24-30. [DOI] [PubMed] [Google Scholar]
- 33. Thompson JS, Littler JW, Upton J. The spiral oblique retinacular ligament. J Hand Surg Am. 1978;3:482-487. [DOI] [PubMed] [Google Scholar]
- 34. Ulusoy MG, Karalezli N, Koçer U, et al. Pull-in suture technique for the treatment of mallet finger. Plast Reconstr Surg. 2006;118(3):696-702. [DOI] [PubMed] [Google Scholar]
- 35. Wehbe MA, Schneider LH. Mallet fractures. J Bone Joint Surg Am. 1984;66:658-669. [PubMed] [Google Scholar]
- 36. Yamanaka K, Sasaki T. Treatment of mallet fractures using compression fixation pins. J Hand Surg Br. 1999;24:358-360. [DOI] [PubMed] [Google Scholar]