Abstract
Background: Endoscopic cubital tunnel release has been proposed as an alternative to open in situ release. However, it is difficult to analyze outcomes after endoscopic release, as only a few small case series exist. Methods: The electronic databases of PubMed (1960-June 2014) were systematically screened for studies related to endoscopic cubital tunnel release or open in situ cubital tunnel release. Baseline characteristics, clinical scores, and complication rates were abstracted. The binary outcome was defined as rate of excellent/good response versus fair/poor. Complications were recorded into 3 categories: wound problems, persistent ulnar nerve symptoms, and other. Results: We included 8 articles that reported the clinical outcomes after surgical intervention including a total of 494 patients (344 endoscopic, 150 open in situ). The pooled rate of excellent/good was 92.0% (88.8%-95.2%) for endoscopic and 82.7% (76.15%-89.2%) for open. We identified 18 articles that detailed complications including a total of 1108 patients (691 endoscopic, 417 open). The 4 articles that listed complication rates for both endoscopic and open techniques were analyzed and showed a pooled odds ratio of 0.280 (95% confidence interval, 0.125-0.625), indicating that endoscopic patients have reduced odds of complications. Conclusions: The results of this systematic review suggest that there is a difference in clinical outcomes between the open in situ and endoscopic cubital tunnel release, with the endoscopic technique being superior in regard to both complication rates along with patient satisfaction.
Keywords: cubital tunnel syndrome, open cubital tunnel release, endoscopic cubital tunnel release, cubital tunnel release complications, systematic review
Introduction
Ulnar nerve compression at the elbow, cubital tunnel syndrome, is the second most common compression neuropathy of the upper extremity19 with an incidence of 25 cases per 100 000 persons.24 Recent data suggest that more than 50 000 cubital tunnel decompressions are performed per year in the United States.20 Previous work has suggested anterior transposition as the gold standard; however, several studies showed no difference between anterior transposition techniques and open in situ decompression.3,11,16,24 Endoscopic cubital tunnel release (ECUTR) has been proposed as an alternative to open cubital tunnel release (OCUTR). Several authors have reported resolution of symptoms in 80% to 90% of patients at short-term follow-up with low complication rates.1,6,7,9,12,21,23 However, it is unclear whether these promising results are the product of a superior technique or bias inherent in studies performed by investigators promoting a specific technique or device. The purpose of this systematic review is to compare clinical outcomes and complications between ECUTR and OCUTR.
Materials and Methods
Eligibility Criteria
We identified articles in the literature that reported clinical outcomes and/or complications after open in situ ulnar nerve decompression and/or ECUTR. Reasons for exclusion of articles were review articles without data, not using the Bishop scale scores or not describing the grading scale used, not reporting data as 2 separate groups, and articles that could not be located.
Study Identification
The electronic databases of PubMed (1960-June 2014) were systematically screened for studies related to ECUTR or OCUTR. Two standard PubMed searches were made using the terms “Endoscopic Cubital Tunnel Release” and “Cubital Tunnel Release.” The results from the 3 MeSH terms of “Cubital Tunnel Syndrome,” “Ulnar Nerve Compression Syndromes,” and “Ulnar Nerve Compression Syndrome AND Endoscopy” were also used. If the abstracted suggested that it might meet the eligibility criteria, the full-text publication was retrieved and reviewed.
Data Abstraction and Analysis
Baseline characteristics, clinical scores, and complication rates were abstracted. The Bishop scale score was the most commonly reported outcome measure across the included studies and was used for this analysis. This scoring system combines subjective measures (severity of residual symptoms, postoperative improvement, postoperative work status) and objective measures (grip strength and 2-point discrimination) to give a final score used to denote the results as excellent, good, fair, or poor. A traditional meta-analysis was not performed because not enough articles reported this outcome for both endoscopic and open techniques. The binary outcome was defined as rate of excellent/good response versus fair/poor. Complications were recorded as listed in the articles and included wound problems (wound breakdown/dehiscence, hematomas, hypertrophic scars, peri-incisional pain, medial antebrachial cutaneous nerve paresthesias), persistent ulnar nerve symptoms (symptom recurrence, ulnar nerve subluxation), and other (thrombophlebitis).
A statistician was consulted from the Clinical and Translational Science Institute at the University of Pittsburgh. Data were pooled across studies, standard mean differences in effect sizes weighted by study sample size were calculated, and heterogeneity across studies was assessed. To run traditional meta-analyses, we included 4 articles that listed complications for both ECUTR and OCUTR.
Results
Literature Search
We identified 1256 citations in our electronic search (Figure 1), and 10 met the inclusion criteria and were included in the analysis (Table 1). We identified 8 studies that included the clinical outcomes after surgical intervention to treat cubital tunnel syndrome. We identified 4 studies that reported complication rates for both ECUTR and OCUTR.
Figure 1.
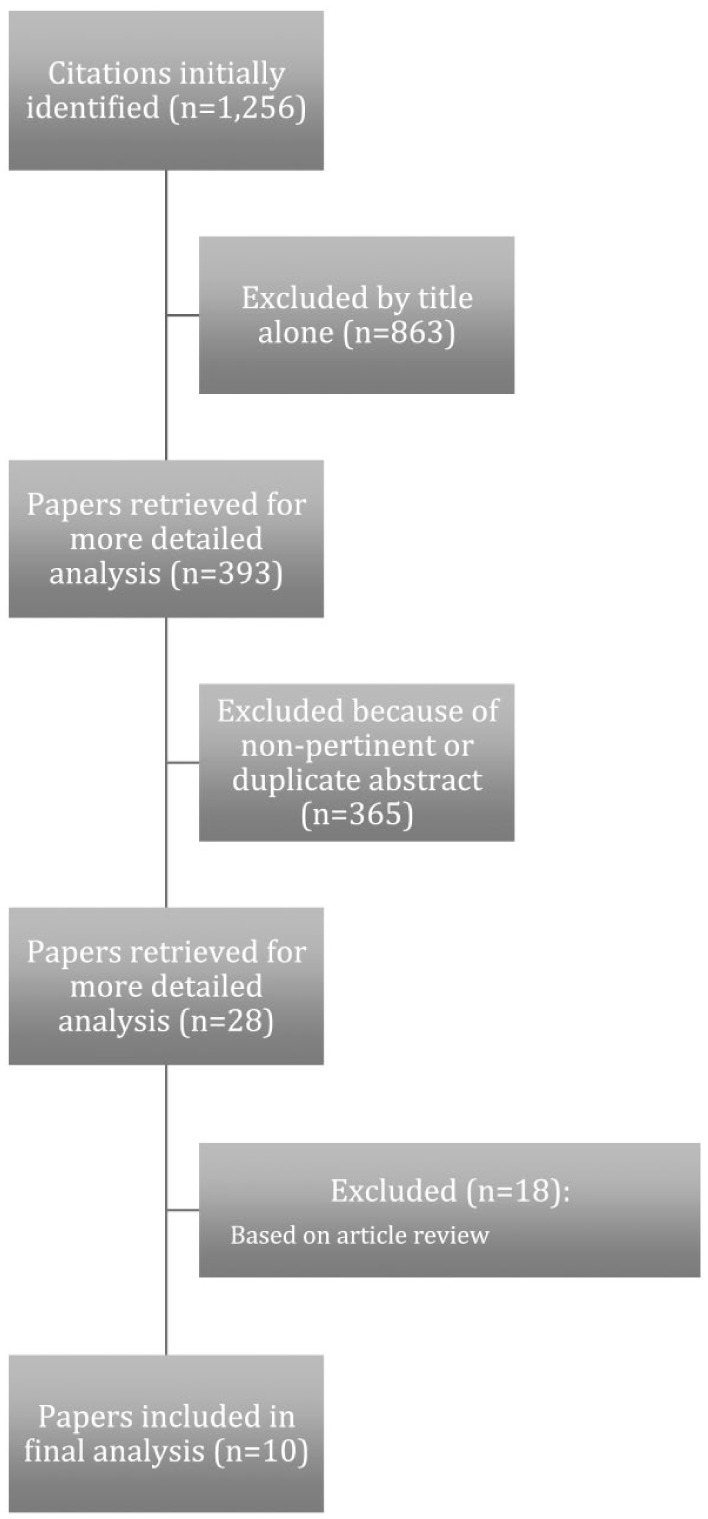
Systematically included studies.
Table 1.
Studies Included in the Systematic Review.
| Author | Year | Journal | Level of evidence |
|---|---|---|---|
| Dutzmann et al8 | 2013 | Neurosurgery | III |
| Bolster et al4 | 2014 | Journal of Hand Surgery | II |
| Hoffman and Siemionow12 | 2006 | Journal of Hand Surgery | III |
| Cobb6 | 2009 | Hand | III |
| Tsai et al21 | 1999 | Journal of Hand Surgery | III |
| Karthik et al13 | 2012 | Journal of Hand Surgery | III |
| Gervasio et al10 | 2005 | Neurosurgery | II |
| Ochi18 | 2013 | Journal of Hand Surgery | III |
| Bacle et al2 | 2014 | Orthopaedics & Traumatology: Surgery & Research | III |
| Watts and Bain22 | 2009 | Journal of Hand Surgery | III |
Clinical Outcomes, Bishop Scores
Excellent/good outcomes were obtained in 92.0% (88.8%-95.2%) of ECUTR patients and 82.7% (76.15%-89.2%) of OCUTR patients (Figure 2). For ECUTR, 5 studies with a total of 331 patients were included in the analysis. For OCUTR, 5 studies with a total of 150 patients were included in the analysis (Table 2).
Figure 2.
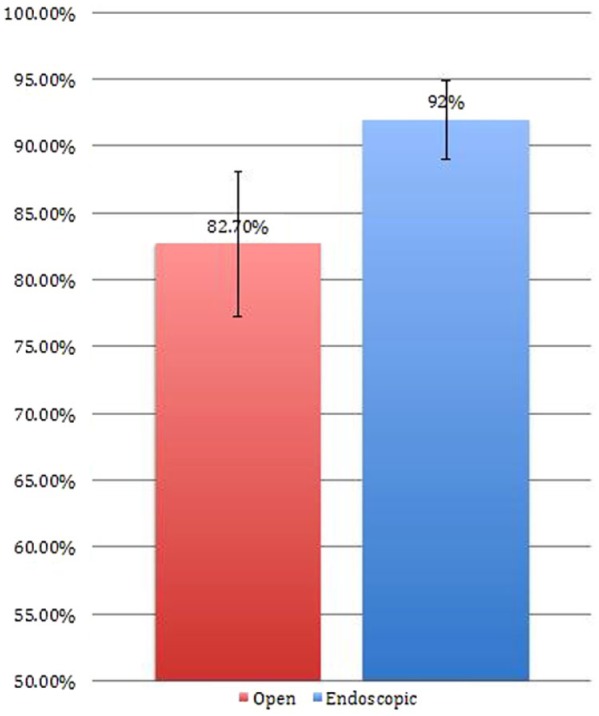
Endoscopic versus open in situ release: Clinical outcomes (as determined by rate of excellent/good scores on the Bishop scale).
Table 2.
Comparison of Outcomes Between Endoscopic and Open In Situ Release.
Complications
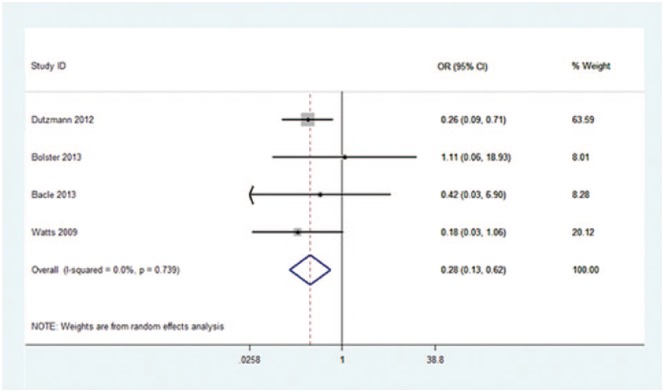
All the included studies, techniques employed, and listed complications are shown in Table 3. Four studies comparing complication rates stemming from both ECUTR and OCUTR were used in the analysis. When comparing the complication rates of ECUTR and OCUTR (Figure 3), the analysis showed a pooled odds ratio of 0.28 (0.13-0.62), P = .002, indicating that ECUTR has reduced odds of complications compared with OCUTR.
Table 3.
Included Studies, Techniques Employed, and Listed Complications.
| Study | Number of patients | Described surgical technique | Complications |
|---|---|---|---|
| Endoscopic | |||
| Tsai et al21 | 85 | 2-3 cm curvilinear, longitudinal incision is made along the course of the ulnar nerve at the cubital tunnel between the medial epicondyle and the olecranon. A 5-mm calibrated glass tube (Ace Glass Company, Louisville, Kentucky) is introduced distally between the fascia overlying the 2 heads of the FCU and the FCU muscle. A 3.5-mm, 30° endoscope is placed into the glass tube. The Smillie knife is introduced between the glass tube and the fascia, and divides the fascia as it is moved distally under visual guidance. A release of up to 10 cm distal and 10 cm proximal to the medial epicondyle is attempted in every case. | Superficial infection: 4 Symptom recurrence: 3 (treated with ulnar nerve transposition) Thrombophlebitis: 1 |
| Cobb6 | 104 | 2-cm incision is made over the cubital tunnel, posterior to the medial epicondyle. The ulnar nerve is then palpated in the cubital tunnel just posterior to the medial epicondyle. The roof is placed under tension with forceps and opened with a number 15 blade. The ulnar nerve is identified, and scissors are utilized to open the cubital tunnel for several centimeters. The endoscope is then placed within the cannula, and the ulnar nerve is identified through the inferior slots of the cannula. After the ulnar nerve is confirmed to be under the cannula throughout the entire course, a push knife is then utilized to divide the fascia at the superior slot of the cannula. This release is performed both proximally and distally. | Symptom recurrence: 3 (1 treated with ulnar nerve transposition; 2 treated with open release) |
| Hoffman and Siemionow12 | 76 | The ulnar nerve is palpated, and a 1.5- to 3.0-cm skin incision is made over the retrocondylar groove. The dissection is carried down to the retrocondylar tunnel roof, which is opened. The tunneling forceps is introduced distally about 10 to 12 cm and proximally about 8 to 10 cm (measured from the midpoint of the retrocondylar groove) into the space between the forearm fascia and the subcutaneous tissue. A 4 mm 301 Endoscope with a blunt dissector on its tip is now introduced and slowly advanced distally. All dissection and cutting is done with blunt-tipped scissors of a length between 17 and 23 cm. From the midpoint of the retrocondylar groove, constricting elements were divided 8 to 12 cm distally and 8 to 10 cm proximally. All instruments KARL STORZ (Tuttlingen, Germany). | Superficial hematoma: 4 Complex regional pain syndrome: 1 Hypesthesia in distribution of MABC: 9 |
| Dutzmann et al8 | 55 | A straight incision of approximately 1.5 to 2.0 cm in length is made directly on the sulcal ridge along the Langer skin tension lines. Here, the ulnar nerve is identified. The retractor-integrated endoscope is introduced, the fibrous ligaments overlying the ulnar nerve are transected longitudinally, and the nerve is deroofed. The proximal point is defined as the point of exit of the ulnar nerve from the MIS and distally along the course of the cubital tunnel, approximately 10 to 12 cm distal to the sulcus. If the MIS is found to be hypertrophic, it is resected. The elbow is flexed and extended, and at the same time, the gliding of the nerve is observed endoscopically. | Superficial hematoma: 2 Ulnar nerve subluxation: 4 (2 underwent transposition) |
| Bolster et al4 | 11 | A minimally invasive technique using an illuminated speculum. A 2.5-cm longitudinal incision was made midway between the medial epicondyle and the olecranon. The subcutaneous tissue was dissected bluntly down to the fascia of the forearm. The fascia over the ulnar nerve was released distally with the use of tunneling forceps. The ulnar nerve was released 12 cm both proximally and distally, ie, 24 cm in total. | Superficial infection: 1 |
| Bacle et al2 | 143 | A skin incision, of about 12 mm, was performed midway between the olecranon and the medial epicondyle. After exposure of the ulnar nerve and covering aponeurosis, endoscopy consisted in dilating the epicondylar groove to enable a cannula to be introduced between the ulnar nerve and the epicondylar groove roof. Tissue above the ulnar nerve trunk was resected 7 cm distally and proximally. | Peri-incisional tenderness: 1 |
| Watts and Bain22 | 15 | Not described. | New elbow pain: 1 Peri-incisional tenderness: 2 Numbness at elbow: 3 |
| Open | |||
| Ochi et al18 | 11 | The subcutaneous tissue was dissected until the superficial fascia overlying the ulnar nerve and aponeurosis of the flexor carpi ulnaris muscle were exposed. The ulnar nerve and its epineurium were exposed directly behind the medial epicondyle, where ulnar nerve strain has been shown to be the greatest. Two 5-0 nylon sutures were placed on the surface of the epineurium without injuring the ulnar nerve. The first suture was placed just posterior to medial epicondyle proximal to the cubital tunnel retinaculum (Osborne constriction band). A second suture was placed approximately 10 mm proximal to the first suture at maximal elbow extension. A simple decompression of the ulnar nerve was then performed by releasing the arcade of Struthers, intermuscular septum, cubital tunnel retinaculum, and fascia overlying the 2 heads of the flexor carpi ulnaris. | Not listed |
| Karthik et al13 | 30 | The ulnar nerve was palpated, and a 3-m longitudinal incision was made, starting from a point midway between the medial epicondyle and olecranon process and extending distally parallel to the medial border of ulna. The arcuate ligament was exposed by blunt dissection and released under direct vision The aponeurotic fascia of the FCU was split protecting the motor branches to the FCU. After distal release, the elbow was extended and the skin retracted so that the nerve was decompressed proximally. | Not listed |
| Gervasio et al10 | 35 | A slightly curvilinear, longitudinal skin incision was performed crossing an imaginary line between the medial epicondyle and the olecranon process and extending for approximately 4 cm proximally and 4 cm distally. The skin incision was placed 2 or 3 cm below the cutaneous projection of the nerve course to avoid contact between the surgical wound and the nerve and a development of fibrous adherences between the nerve and the scar. The subcutaneous tissue was carefully dissected to identify and preserve the medial cutaneous nerve of the forearm. Osborne ligament was identified and released, the fascia over the ulnar nerve was divided, and an accurate external neurolysis (paraneurectomy) was performed, freeing the nerve for 360°. The skin was retracted proximally and distally, and the nerve release was completed up to the MIS proximally and up to the deep flexor-pronator aponeurosis distally. | Peri-incisional tenderness: 2 Hypertrophic scar: 1 Wound dehiscence: 1 Superficial infection: 1 |
| Dutzmann et al8 | 59 | An approximately 6- to 8-cm-long curvilinear longitudinal skin incision is made around the medial epicondyle. The Osborne ligament is identified and transected. The fascia over the ulnar nerve is divided, and the nerve is deroofed. Care is taken to release the nerve from the intermuscular septum proximally to the deep flexor aponeurosis distally. The septum within the flexor carpi ulnaris muscle is gently separated if necessary. | Peri-incisional sensitivity: 4 Superficial infection: 1 Hypesthesia in distribution of MABC: 14 |
| Bolster et al4 | 15 | A 2.5-cm longitudinal incision was made midway between the medial epicondyle and the olecranon. An illuminated speculum was inserted. The subcutaneous tissue was dissected bluntly down to the fascia of the forearm. The fascia over the ulnar nerve was released distally with the use of tunneling forceps. The ulnar nerve was released 12 cm both proximally and distally, ie, 24 cm in total. | Symptom recurrence: 1 (underwent reoperation) |
| Bacle et al2 | 48 | A 3 cm skin incision was centered on the medial epicondyle. Proximally, the MIS was opened, with distal release up to the UN first motor branch. | None |
| Watts and Bain22 | 19 | Endoscopic technique utilizing Agee device. | Superficial hematoma: 1 |
Note. FCU = flexor carpi ulnaris; MIS = medial intermuscular septum; MABC = medial antebrachial cutaneous nerve; UN = ulnar nerve.
Figure 3.
Forest plot of complications comparing endoscopic cubital tunnel release and open cubital tunnel release.
Note. Weights are from random-effects analysis. OR = odds ratio; CI = confidence interval.
Discussion
Endoscopic cubital tunnel release has been proposed as an alternative to open in situ release with the purported benefits of increased patient satisfaction and decreased complications secondary to the use of smaller incisions. With the advent of new techniques, appropriate scrutiny is warranted. In the past decade, the effectiveness and safety of endoscopic techniques have been demonstrated through the publication of relatively small case series treating patients of different disease severity and using a myriad of endoscopic techniques.1,5,9,12,17 However, based on these series and in the absence of prospective studies comparing ECUTR with OCUTR, it is unclear whether ECUTR is superior to OCUTR with respect to outcomes and complication rates. The use of a systematic review to increase patient numbers and power is an accepted method to compare 2 treatment options. This study has found that patients treated with ECUTR are more likely to report excellent or good results through a Bishop scale compared with patients treated with OCUTR. In addition, patients treated with ECUTR had a lower incidence of complications than patients treated with OCUTR.
The medial antebrachial cutaneous nerves have been shown to be in close proximity to the surgical dissection posing an inherent danger during the procedure.14 Injury to these structures during an open approach is likely the reason that patients were found to have a significantly lower incidence of complications such as postoperative scar tenderness and peri-incisional sensation deficits and significantly less postoperative pain on a visual analog scale after endoscopic decompression.8,22 However, caution with either approach must be practiced as endoscopy does not eliminate the risk of these complications entirely.
This study has several limitations. A systematic review is subject to bias based on the inclusion and exclusion criteria. Macadam et al15 showed that there is a lack of reproducible and reliable outcome measures in the literature to assess results after cubital tunnel decompression. Similarly, the reporting of complications is dependent on each investigators perspective on the definition of an actual complication. One should always be aware of a reporting bias when a novel technique is being compared with a more traditional method. In an effort to reduce variability and to minimize the inherent bias in our review, only studies that reported outcomes using the Bishop scale were included. There is also variability in the technique utilized for the procedure in each study. Different instruments and methods have been employed by the authors who are also inventors or consultants of the devices utilized for the decompression. Thus, each study not only may possess a slight inherent bias but also may not convey complications that occur from a learning curve that accompanies the use of any new device.
The results of this study support the effectiveness of endoscopic decompression of the ulnar nerve in the cubital tunnel. This technique appears to reduce the complications attributed to longer incisions on the medial aspect of the elbow, indicating that it is as safe as or safer than the open technique. Patient satisfaction also appears to be slightly higher with this minimally invasive technique. Although further investigation is needed, these results suggest that endoscopic technique should continue to be utilized and developed.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This study was a meta-analysis of existing literature. As such, this article does not contain any experimentation with human or animal subjects.
Statement of Informed Consent: No informed consent was needed to carry out this study as no individual participants were investigated.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ahcan U, Zorman P. Endoscopic decompression of the ulnar nerve at the elbow. J Hand Surg Am. 2007;32(8):1171-1176. [DOI] [PubMed] [Google Scholar]
- 2. Bacle G, Marteau E, Freslon M, et al. Cubital tunnel syndrome: comparative results of a multicenter study of 4 surgical techniques with a mean follow-up of 92 months. Orthop Traumatol Surg Res. 2014;100:S205-S208. [DOI] [PubMed] [Google Scholar]
- 3. Bartels RH, Verhagen WI, van der Wilt GJ, Meulstee J, van Rossum LG, Grotenhuis JA. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: part 1. Neurosurgery. 2005;56(3):522-530; discussion 522-530. [DOI] [PubMed] [Google Scholar]
- 4. Bolster MA, Zöphel OT, van den Heuvel ER, Ruettermann M. Cubital tunnel syndrome: a comparison of an endoscopic technique with a minimal invasive open technique. J Hand Surg Eur. 2014;39(6):621-625. [DOI] [PubMed] [Google Scholar]
- 5. Cobb TK, Sterbank PT. Five year review of endoscopic cubital tunnel release. J Hand Surg Br. 2008;33E:49. [Google Scholar]
- 6. Cobb TK, Sterbank PT, Lemke JH. Endoscopic cubital tunnel recurrence rates. Hand. 2010;5(2):179-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cobb TK, Walden AL, Merrell PT, Lemke JH. Setting expectations following endoscopic cubital tunnel release. Hand. 2014;9:356-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dutzmann S, Martin KD, Sobottka S, et al. Open vs retractor-endoscopic in situ decompression of the ulnar nerve in cubital tunnel syndrome: a retrospective cohort study. Neurosurgery. 2013;72(4):605-616. [DOI] [PubMed] [Google Scholar]
- 9. Flores LP. Endoscopically assisted release of the ulnar nerve for cubital tunnel syndrome. Acta Neurochir (Wien). 2010;152(4):619-625. [DOI] [PubMed] [Google Scholar]
- 10. Gervasio O, Gambardella G, Zaccone C, Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56(1):108-117. [DOI] [PubMed] [Google Scholar]
- 11. Heithoff SJ. Cubital tunnel syndrome does not require transposition of the ulnar nerve. J Hand Surg Am. 1999;24(5):898-905. [DOI] [PubMed] [Google Scholar]
- 12. Hoffmann R, Siemionow M. The endoscopic management of cubital tunnel syndrome. J Hand Surg Br. 2006;31(1):23-29. [DOI] [PubMed] [Google Scholar]
- 13. Karthik K, Nanda R, Storey S, Stothard J. Severe ulnar nerve entrapment at the elbow: functional outcome after minimally invasive in situ decompression. J Hand Surg Eur. 2012;37(2):115-122. [DOI] [PubMed] [Google Scholar]
- 14. Lowe JB, Maggi SP, Mackinnon SE. The position of crossing branches of the medial antebrachial cutaneous nerve during cubital tunnel surgery in humans. Plast Reconstr Surg. 2004;114:692-696. [DOI] [PubMed] [Google Scholar]
- 15. Macadam SA, Bezuhly M, Lefaivre KA. Outcomes measures used to assess results after surgery for cubital tunnel syndrome: a systematic review of the literature. J Hand Surg Am. 2009;34:1482-1491.e5. [DOI] [PubMed] [Google Scholar]
- 16. Mowlavi A, Andrews K, Lille S, Verhulst S, Zook E, Milner S. The management of cubital tunnel syndrome: a meta-analysis of clinical studies. Plast Reconstr Surg. 2000;106(2):327-334. [DOI] [PubMed] [Google Scholar]
- 17. Nakao Y, Takayama S, Toyama Y. Cubital tunnel release with lift-type endoscopic surgery. Hand Surg. 2001;6:199-203. [DOI] [PubMed] [Google Scholar]
- 18. Ochi K, Horiuchi Y, Nakamura T, Sato K, Arino H, Koyanagi T. Ulnar Nerve strain at the elbow in patients with cubital tunnel syndrome: effect of simple decompression. J Hand Surg Eur. 2013;38(5):474-480. [DOI] [PubMed] [Google Scholar]
- 19. Palmer BA, Hughes TB. Cubital tunnel syndrome. J Hand Surg Am. 2010;35(1):153-163. [DOI] [PubMed] [Google Scholar]
- 20. Soltani AM, Best MJ, Francis CS, Allan BJ, Panthaki ZJ. Trends in the surgical treatment of cubital tunnel syndrome: an analysis of the national survey of ambulatory surgery database. J Hand Surg Am. 2013;38(8):1551-1556. [DOI] [PubMed] [Google Scholar]
- 21. Tsai TM, Chen IC, Majd ME, Lim BH. Cubital tunnel release with endoscopic assistance: results of a new technique. J Hand Surg Am. 1999;24(1):21-29. [DOI] [PubMed] [Google Scholar]
- 22. Watts AC, Bain GI. Patient-rated outcome of ulnar nerve decompression: a comparison of endoscopic and open in situ decompression. J Hand Surg Am. 2009;34:1492-1498. [DOI] [PubMed] [Google Scholar]
- 23. Yoshida A, Okutsu I, Hamanaka I. Endoscopic anatomical nerve observation and minimally invasive management of cubital tunnel syndrome. J Hand Surg Eur Vol. 2009;34(1):115-120. [DOI] [PubMed] [Google Scholar]
- 24. Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007;89(12):2591-2598. [DOI] [PubMed] [Google Scholar]