To the Editor
Hysterectomy is the second most common surgery among women in the United States, with approximately 600,000 performed annually for benign gynecologic conditions1. Trends in hysterectomy rates are an important marker for innovation and quality in gynecology as treatment alternatives increase and evidence of underuse of these alternative treatments emerges.2 Accurate identification of hysterectomy requires capture of both inpatient and outpatient services, given the shifting setting of care over recent years. Yet, the highest quality national trend estimates have been significantly limited by exclusion of outpatient surgery due to the use of databases restricted to inpatients.3,4 Prior studies that included inpatient and outpatient settings have focused on small geographic areas only, limiting their generalizability.5 The lack of national outpatient data is a critical gap, as rapid dissemination of robotic surgery has likely shifted the proportion of hysterectomy cases performed in outpatient settings.
The same shifting pattern may also be true for oophorectomy, another common procedure among US women. As with hysterectomy, the ability to analyze trends in oophorectomy is limited by use of data restricted to inpatients.
Methods
Using Truven Health Analytics Commercial Claims and Encounters Database, commercial insurance data representing over 50 million insured adults and containing both inpatient and outpatient procedures, we report long-term trends in hysterectomy and oophorectomy rates between 2000–2014. In particular, we estimate care received in inpatient and outpatient settings separately over this period to provide a comprehensive picture of gynecologic surgery receipt among commercially-insured US women.
We focused our analysis on women ages 18–64 who did not have cancer-related care during the period spanning one day before and thirty days after hysterectomy and/or oophorectomy, as this population is the most amenable to alternative treatment options. To calculate annual rates of use, we divided the number of women receiving each procedure by the total number of women ages 18–64 who were enrolled in the health plans in each month and multiplied this value by 100,000 to represent the rate per 100,000 health plan enrollees. This study was exempt from institutional review board review as it is a secondary analysis of de-identified data.
Results
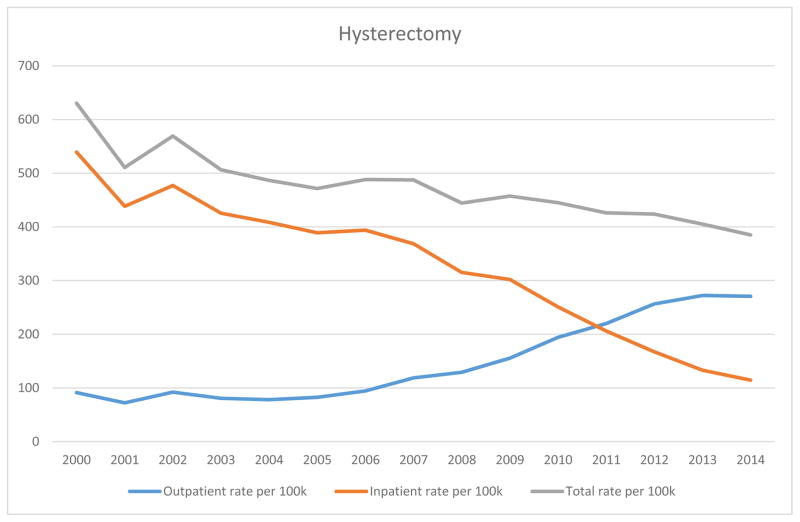
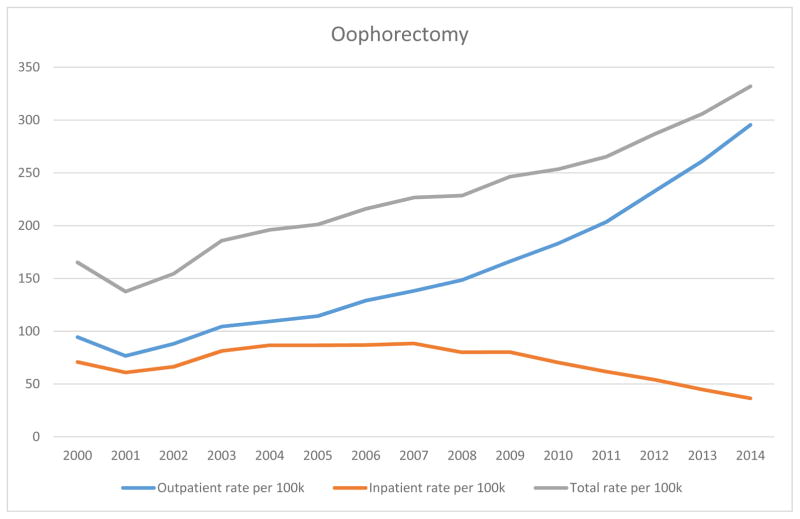
From 2000–2014 there were 809,905 hysterectomies and 257,573 oophorectomies recorded. Overall annual hysterectomy rates decreased 39% between 2000 and 2014 (631/100,000 to 385/100,000) (Figure 1). The proportion of hysterectomy performed in outpatient settings increased from 14% in 2000 to 70% in 2014. Over the same time period, overall annual oophorectomy rates decreased from 166/100,000 to 134/100,000. The proportion of outpatient oophorectomy cases increased from 57% to 84% (Figure 2).
Figure 1.
Rates of hysterectomy per 100,000 women aged 18–64 enrolled in Commercial Health Plans, 2000 – 2014.
Data are from Truven Health Analytics Commercial Claims and Encounters Database, Copyright 2016.
Figure 2.
Rates of oophorectomy per 100,000 women aged 18–64 enrolled in Commercial Health Plans, 2000 – 2014.
Data are from Truven Health Analytics Commercial Claims and Encounters Database, Copyright 2016.
Discussion
This work demonstrates a current gap in gynecologic surgery research. Analyses limited to inpatient procedures likely underestimate rates of hysterectomy and oophorectomy, providing an incomplete picture of overall trends. Falsely low hysterectomy rates based on inpatient-only data can imply a greater use of alternative therapies (to hysterectomy) than what may actually be occurring. In addition, with a shift in standard of care to outpatient surgery, inpatient populations may represent a biased group of sicker, poorer patients whose outcomes we should not generalize to the greater population.
To accurately assess changing treatment patterns in gynecology, studies should include inpatient and outpatient procedures. Given the often subjective indications6 and previously reported geographic, socioeconomic, and racial variation in surgery rates, tracking usage patterns is important. Our work highlights important trends in hysterectomy and oophorectomy use and the extent to which care has shifted largely to outpatient settings. Recognizing gaps in data that provide only a partial view of surgical care patterns may avoid drawing incorrect conclusions regarding access to or quality of care received.
Acknowledgments
We thank Tania Wilkins for her assistance with data management and analysis. Kemi Doll and Stacie Dusetzina had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Dr. Doll is supported by the National Cancer Institute of the National Institutes of Health under award number R25CA116339. Dr. Dusetzina is supported by the NIH Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) K12 Program and the North Carolina Translational and Clinical Sciences Institute (UL1TR001111). Dr. Robinson is supported by the National Institutes of Health under award number K01CA172717-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The database infrastructure used for this project was funded by the Department of Epidemiology, UNC Gillings School of Global Public Health; the Cecil G. Sheps Center for Health Services Research, UNC; the CER Strategic Initiative of UNC’s Clinical & Translational Science Award (UL1TR001111); and the UNC School of Medicine. We are grateful to the Carolina Population Center (R24 HD050924) for general support and the Carolina Community Network II Cancer Health Disparities Pilot Grant. The authors have no conflicts of interest to report.
References
- 1.Discharges with at least one procedure in nonfederal short-stay hospitals, by sex, age, and selected procedures: United States, selected years 1990 through 2009–2010. Hyattsville, MD: National Center for Health Statistics; 2015. [Google Scholar]
- 2.Corona LE, Swenson CW, Sheetz KH, et al. Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. American journal of obstetrics and gynecology. 2015 Mar;212(3):304, e301–307. doi: 10.1016/j.ajog.2014.11.031. [DOI] [PubMed] [Google Scholar]
- 3.Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstetrics and gynecology. 2013 Aug;122(2 Pt 1):233–241. doi: 10.1097/AOG.0b013e318299a6cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright JD, Ananth CV, Lewin SN, et al. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA : the journal of the American Medical Association. 2013 Feb 20;309(7):689–698. doi: 10.1001/jama.2013.186. [DOI] [PubMed] [Google Scholar]
- 5.Babalola EO, Bharucha AE, Schleck CD, Gebhart JB, Zinsmeister AR, Melton LJ., 3rd Decreasing utilization of hysterectomy: a population-based study in Olmsted County, Minnesota, 1965–2002. American journal of obstetrics and gynecology. 2007 Mar;196(3):214, e211–217. doi: 10.1016/j.ajog.2006.10.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ACOG Practice Bulletin No. 89. Elective and risk-reducing salpingo-oophorectomy. Obstetrics and gynecology. 2008 Jan;111(1):231–241. doi: 10.1097/01.AOG.0000291580.39618.cb. [DOI] [PubMed] [Google Scholar]