Abstract
The etiological agent most commonly associated with bacillary dysentery is Shigella. As part of its mandate, the Bacteriology and Enteric Disease Program of Health Canada identifies and serotypes unusual isolates of Shigella received from provincial laboratories of public health. In this report, six unusual isolates from three provinces were analyzed biochemically and serologically using slide and tube agglutinations and molecularly using standard pulsed-filed gel electrophoresis (PFGE), PCR, and PCR-restriction fragment length polymorphism (RFLP) techniques. All six isolates were identical. PFGE analysis grouped these strains; biochemically, they were mannitol negative and consistent with the profile of Shigella. Serologically, these strains produced weak reactions in Shigella dysenteriae serovars 4 and 16 and Escherichia coli O159 and O173 antisera. Molecular serotyping by PCR-RFLP of the rfb gene produced an S. dysenteriae serovar 2/E. coli O112ac pattern. They were positive by PCR for ipaH and ial enteroinvasive genes but negative for all other genes tested. Antiserum was prepared from one of the isolates and tested against Shigella and E. coli reference strains as well as the other isolates. The antiserum reacted with the five remaining isolates and showed cross-reactivity with S. dysenteriae serovars 1, 4, and 16; Shigella flexneri type 3; and E. coli O118, O159, O168, O172, and O173 antigens. Absorbing the sera with E. coli O159 and S. dysenteriae serovar 4 antigen removed all cross-reactions and only slightly reduced the homologous titer. Based on biochemical, molecular, and complete serological analysis, we propose that these six isolates represent a new provisional serovar of S. dysenteriae, type strain BEDP 02-5104.
The genus Shigella is divided into four groups, A, B, C, and D, with the common nomenclature of Shigella dysenteriae, S. flexneri, S. boydii, and S. sonnei, respectively (2). There are 49 recognized serovars, representing subtypes from three of the four groups (2). In addition, as a Canadian national reference laboratory, the Bacteriology and Enteric Disease Program (BEDP) has further characterized six provisional Shigella serovars (6). As a human pathogen, Shigella causes bacillary dysentery (2). Infection and outbreaks associated with this organism are prominent in developing countries and are strongly associated with overcrowding and poor hygienic conditions (5, 9). Shigellosis is also travel associated, and several outbreaks have been reported in developed countries such as Canada and the United States (3, 6, 24). In the United States, the National Shigella Surveillance Report, prepared by the Foodborne and Diarrheal Disease Branch of the National Center for Infectious Diseases at the Centers for Disease Control and Prevention (CDC) in Atlanta, Ga., has been compiled yearly since 1995. In Canada, Shigella is a reportable disease and included in Health Canada's annual surveillance reports. Indeed, the importance of monitoring the trends and presence of this organism in the global population is acutely recognized.
One complicating factor in monitoring the prevalence of Shigella is the difficulty in speciating suspected isolates. Speciation of Shigella is often subjective. Intraspecies phenotypic variability is not uncommon and often contributes to the arbitrary identification of many suspected Shigella isolates. In the United States, the frequency of unspecified Shigella is consistently third in the number of reported Shigella species (24). To further complicate the issue, several phenotypic and genotypic similarities, including pathogenesis, virulence, biochemical profile, and DNA homology, between enteroinvasive Escherichia coli (EIEC) and Shigella species have been identified (8, 28, 30, 31). Fortunately, antigenic expression observed through serotyping remains the “gold standard ” in identifying, subtyping, and monitoring organisms such as Shigella. In instances where all other discriminatory tools are exhausted, such as differentiating EIEC from Shigella, serotyping has remained the finite comparative analysis. Antigenic investigations such as this one provide an important venue for both accurate identification and surveillance of shigellosis in Canada and worldwide.
Herein, we describe a group of bacterial strains isolated from humans living in different geographical locations across Canada which were identical and consistent with the description of Shigella. Our analysis of antigenic expression via serotyping revealed that these isolates, even though their exact speciation remained arbitrary, harbored unique immunological epitopes. In light of the data presented, we suggest in this report that these strains represent a novel serovar of Shigella dysenteria.
MATERIALS AND METHODS
Strains.
The clinical isolates characterized in this report were submitted to the BEDP by three provincial laboratories of public health located in Canada (Table 1). Reference strains referred to in this study are part of the culture collection of the BEDP at the National Microbiology Laboratory of Health Canada. This culture collection includes strains of all internationally recognized and Canadian provisional Shigella serovars as well as 181 internationally recognized E. coli O serovars.
TABLE 1.
Clinical isolates
| Specimen | Province | Date collected | Source | Age | Gender |
|---|---|---|---|---|---|
| 01-8115 | Quebec | 27 Sept 01 | Stool | 4 | Male |
| 02-5104 | Alberta | 08 Aug 02 | Stool | 8 | Female |
| 02-5105 | Alberta | 02 Aug 02 | Stool | 8 | Female |
| 02-8626 | British Columbia | 29 Nov 02 | Stool | 17 | Female |
| 03-2342 | British Columbia | 31 Mar 03 | Stool | 36 | Female |
| 03-7463 | British Columbia | 29 Sept 03 | Unknown | 55 | Male |
Biochemical tests and serotyping.
The biochemical reactions of the isolates were determined by employing the methods described previously by Ewing et al. (15). Reference Identification (REFID) software (version 97; Microbiology Department, University Hospital, London, Ontario, Canada) was used to facilitate the biochemical identification of the isolates. Quality-assured in-house diagnostic antisera to all Shigella and E. coli reference cultures and the type strain of this group of isolates, 02-5104, were made as per the methods of Ewing et al. (15, 16). Antiserum was absorbed at a ratio of confluent growth from five nutrient agar plates (150 mm) to 1 ml of antisera. Briefly, cells were harvested with 0.01 M phosphate-buffered saline, boiled for 1 h, and washed three times with a combined 75 ml of phosphate-buffered saline, and centrifugation was employed at 15,000 × g for 15 min. Harvested cells were incubated with sera for 2 h at 50°C. Absorbed antiserum was collected by centrifuging the absorption slurry at 15,000 × g for 30 min and harvesting the supernatant. Serological identification was performed by tube and slide agglutination with polyvalent somatic (O) antigen grouping sera followed by testing with monovalent antisera for specific serovar. The applied Shigella serotyping scheme consisted of S. dysenteriae poly A (serovars 1 to 7) and poly A1 (serovars 8 to 12) antisera and their monovalent components as well as monovalent antisera to S. dysenteriae serovars 13, 14, 15, and 16 and provisional S. dysenteriae serovars designated SH-93 (CDCE670-74) and SH-103 (CDC95011241); S. flexneri poly B antiserum and its monovalent types 1 to 6, monovalent S. flexneri groups Y (types 3 and 4) and X (types 7 and 8) and type 6 antisera, and monovalent antisera to S. flexneri provisional SH-101 (CDC95011236) and SH-104 (CDC95011240); S. boydii poly C (serovars 1 to 7), C1 (serovars 8 to 11), C2 (serovars 12 to15), and C3 (serovars 16 to 18) antisera and their monovalent components as well as monovalent S. boydii serovars 19 and 20 and S. boydii provisional serovar SH-92 (CDC1621-54) and SH-96 (CDC E28938) antisera; and finally, S. sonnei phase I and phase II antisera. Shigella and E. coli are known to share antigenic determinants, so the antigenic natures of these isolates were also analyzed with E. coli antisera to the recognized 181 serovars as polyvalent grouped sera and monovalent antisera.
rfb-RFLP.
Analysis of the rfb gene cluster by restriction fragment length polymorphism (RFLP) was done as described previously by Coimbra et al. (10, 11). Modifications to improve the efficiency and analytical capabilities of the method were applied as described previously by Allen et al. (1). Patterns were analyzed and compared against an established Shigella and E. coli database at the BEDP representing reference serovars using Bionumerics software version 2.0 (Applied Maths, Kortrijk, Belgium). Band position tolerance of 3.5% and optimization values of 1.5% were used for all analyses. Similarity coefficients were obtained within Bionumerics by calculating Dice coefficients. Cluster analysis was performed by using the unweighted pair group method with arithmetic averages.
PCR tests.
Clinical isolates were tested for the presence of the invasion plasmid antigen H (ipaH) and for the invasion-associated locus (ial) genes of Shigella and EIEC as described previously by Sethabutr et al. (32). PCRs to demonstrate the presence of cytolethal distending toxin (cdt), cytotoxic necrotizing factor, attaching and effacing mechanisms (eae), enteroaggregative mechanisms (Eagg), enterohemorrhagic hemolysin (hyl), heat-labile toxin, heat-stable toxin, and verotoxin genes were performed as previously described (26, 27).
Tissue culture.
Vero (African green monkey kidney cells), CHO (Chinese hamster ovary), and Y1 (mouse adrenal cells) cell lines were exposed to culture supernatants from the overnight growth of the clinical isolates in brain heart infusion broth at 37°C to determine the presence of verotoxin, cytotoxic necrotizing factor, and heat-labile toxin as described previously (13, 20, 21, 29). Overnight growth of the clinical isolates in brain heart infusion broth at 37°C was diluted and incubated with HEp-2 (human epithelial) cells to observe invasiveness as previously described (12, 14).
PFGE.
Pulsed-field gel electrophoresis (PFGE) was done according to international standards set by the CDC (7). The XbaI patterns were interpreted using the principles outlined by Tenover et al. (33). The S. sonnei F2353 standard strain was used as the size marker for this analysis. Band position tolerances and optimization values of 1.5% were used for all analyses. Similarity coefficients were obtained within Bionumerics by calculating Dice coefficients. Cluster analysis was done with the unweighted pair group method with arithmetic averages.
RESULTS
Biochemical tests and serotyping.
The biochemical profiles of the clinical isolates are summarized in Table 2 and compared to the four groups of Shigella as well as the biochemically similar EIEC group. Reactions for the comparative strains are displayed in a percent-positive format as was depicted in their respective sources (17, 23). The profiles for the clinical isolates were identical and identified as 99.7% Shigella groups A, B, and C with REFID software. The clinical isolates were mannitol negative, a classical indication of the S. dysenteriae group; however, these isolates were also positive for melibiose and raffinose, two biochemical traits not previously seen in the S. dysenteriae group.
TABLE 2.
Biochemical profile of the novel serovar, Shigella species, and EIEC
| Biochemical reactionb | % Positive strainsa
|
|||||
|---|---|---|---|---|---|---|
| Novel serovar | S. dysenteriaec | S. flexneric | S. boydiic | S. sonneic | EIECd | |
| Adonitol | − | − | − | − | − | − |
| Alpha-methyl glucoside | − | − | − | − | − | − |
| Arabinose | − | 45 | 60 | 94 | 95 | + |
| Arabitol | − | − | 1 | − | − | ND |
| Arginine | − | 2 | 5 | 18 | 2 | 14 |
| Cellobiose | − | − | − | − | 5 | − |
| Christensen citrate | − | − | − | − | − | − |
| Dulcitol | − | 5 | 1 | 5 | − | 12 |
| Esculin | − | − | − | − | − | NA |
| Glucose | + | + | + | + | + | + |
| Glucose gas | − | − | 3 | − | − | 43 |
| Glycerol | − | 10 | 10 | 50 | 15 | 94 |
| Indol | + | 45 | 50 | 25 | − | + |
| Inositol | − | − | − | − | − | − |
| Jordan's tartrate | + | 75 | 30 | 50 | 90 | NA |
| KCN | − | − | − | − | − | NA |
| Lactose | − | − | 1 | 1 | 2 | 51 |
| Lysine | − | − | − | − | − | − |
| Malonate | − | − | − | − | − | − |
| Maltose | − | 15 | 30 | 20 | 90 | 94 |
| Mannitol | − | − | 95 | 97 | + | 94 |
| Mannose | + | + | + | + | + | + |
| Melibiose | + | − | 55 | 15 | 25 | NA |
| Methly red | + | 99 | + | + | + | + |
| Motility | − | − | − | − | − | 1 |
| Mucate | − | − | − | − | 10 | − |
| ONPG | − | 30 | 1 | 10 | 90 | 81 |
| Ornithine | − | − | − | 2 | 98 | 37 |
| PPA | − | − | − | − | − | − |
| Raffinose | + | − | 40 | − | 3 | 1 |
| Rhamnose | + | 30 | 5 | 1 | 75 | 63 |
| Salicin | − | − | − | − | − | 3 |
| Simmon's citrate | − | − | − | − | − | − |
| Sodium acetate | − | − | 8 | − | − | 44 |
| Sorbitol | − | 30 | 29 | 43 | 2 | 97 |
| Sucrose | − | − | 1 | − | 1 | 1 |
| Trehalose | + | 90 | 65 | 85 | + | 97 |
| TSI | − | − | − | − | − | − |
| Urease | − | − | − | − | − | − |
| VP | − | − | − | − | − | − |
| Xylose | − | 4 | 2 | 11 | 2 | 99 |
Numbers refer to a percent positive for the biochemical reaction. ND, not done; NA, not available; +, all strains positive; −, all strains negative.
KCN, potassium cyanide; ONPG, O-nitrophenyl-β-d-galactopyranoside; PPA, phenylalanine deaminase; TSI, triple sugar ion; VP, Voges-Proskauer.
Data from Farmer et al. (17).
Data from Matsushita et al. (23).
Serotyping by slide and tube agglutination was inconclusive but consistent among this group of clinical isolates. All isolates reacted moderately with S. dysenteriae poly A sera (serovars 1 to 7), and weak reactions were seen with S. dysenteriae serovar 4 and S. dysenteriae serovar 16 antisera. No further reactivity was observed with any other Shigella antisera. The isolates reacted with both E. coli O159 and O173 antisera, more prominently in the O159 antiserum. Confirmatory analysis of the type strain of these isolates by the World Health Organization collaborative center for Shigella (CDC) supported our findings by designating the strain to be an untypeable S. dysenteriae serovar.
All clinical isolates agglutinated well with the antisera prepared from the type strain for this group, both by slide and tube agglutination. The reactivities of the antisera against all antigens represented in the Shigella and E. coli serotyping schemes of our laboratory are summarized in Table 3. The antisera reacted to Shigella antigens from S. dysenteriae serovars 1, 4, and 16 as well as S. flexneri type 3 and E. coli antigens from serovars O118, O159, O168, O172, and O173. The antisera were absorbed with representative Shigella and E. coli strains, S. dysenteriae serovar 4 and E. coli O159, based on the extent of the cross-reactivity of these particular antigens with the prepared antisera. Absorption of the antisera with these two reference antigens removed the cross-reactivity of the antisera to all E. coli and Shigella reference antigens. Reactivity of the antisera to the group of clinical isolates under study did diminish postabsorption but remained at a level that was significant enough to earmark antigenic singularity (Table 3). Absorption of the in-house S. dysenteriae serovars 4 and 16 and E. coli O159 and O173 antisera with the type strain of this group of isolates removed the initially observed serological cross-reactions (data not shown).
TABLE 3.
Antiserum cross-reactions
| Antigen | Slide serology (dilution)a
|
Tube serology (dilution)b
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Undiluted | 1/2 | 1/4 | 1/8 | 1/16 | 1/100 | 1/200 | 1/400 | 1/800 | 1/1,600 | 1/3,200 | 1/6,400 | 1/12,800 | |
| S. dysenteriae serovar 1 | 2 | 1 | N | N | N | 3 | 1 | N | N | N | N | N | N |
| S. dysenteriae serovar 4 | 3 | 2 | N | N | N | 4 | 2 | 1 | N | N | N | N | N |
| S. dysenteriae serovar 16 | 3 | 2 | N | N | N | 4 | 2 | 1 | N | N | N | N | N |
| S. fexneri serovar 3 | 2 | N | N | N | N | 3 | 1 | N | N | N | N | N | N |
| E. coli O118 | Tr | N | N | N | N | 2 | N | N | N | N | N | N | N |
| E. coli O159 | 4 | 4 | 2 | N | N | 4 | 4 | 4 | 3 | 1 | N | N | N |
| E. coli O168 | 2 | N | N | N | N | 3 | 1 | N | N | N | N | N | N |
| E. coli O172 | 3 | 2 | N | N | N | 4 | 2 | 1 | N | N | N | N | N |
| E. coli O173 | 4 | 4 | 1 | N | N | 4 | 4 | 4 | 2 | Tr | N | N | N |
| Novel serovar | 4 | 4 | 4b | 4 | 3 | 4 | 4 | 4 | 4b | 4 | 3 | 2 | 1 |
Reactions were recorded on a scale of 1 to 4, with 1 being the lowest level of agglutination and 4 being the highest level of agglutination; Tr is indicative of a trace level of agglutination, and N is indicative of no agglutination.
Postabsorption with E. coli O159 and S. dysenteriae serovar 4 end titer with a level of agglutination of 4.
rfb-RFLP.
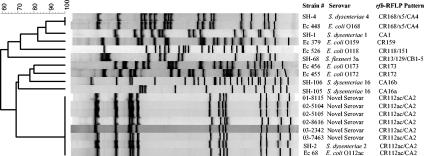
All isolates produced the same pattern when subjected to amplification and restriction enzyme digestion of the rfb gene cluster. When compared to the in-house database, the pattern was identical to that of E. coli O112ac and S. dysenteriae serovar 2, which share the same pattern. Figure 1 outlines this comparison as well as the relationship of this pattern to other patterns representative of serovars where antigenic similarities were observed by slide and tube agglutination. All rfb-RFLP patterns representing the cross-reactive antigens were substantially different.
FIG. 1.
Comparative rfb-RFLP analysis of the novel Shigella serovar and related Shigella and E. coli.
PCR.
All the clinical isolates were positive for the ial and ipaH invasive genes as well as the cdt-1A gene but negative for the presence of the other virulence genes tested for in this study.
Tissue culture.
The six isolates were phenotypically invasive when cultured with HEp-2 cells. Cytotoxicity was also observed with CHO cells, indicating cytolethal distending toxin activity.
PFGE.
All six of the novel isolates were clonal by PFGE analysis. A comparative analysis is depicted in Fig. 2. Strain 02-5105 differed by one band, but with the application of Tenover's principles for interpreting PFGE patterns, this isolate would be considered closely related and clonal with respect to the other isolates.
FIG. 2.
PFGE-XbaI analysis of the six novel S. dysenteriae serovars.
DISCUSSION
In the presented biochemical comparison, a speciation of S. flexneri for this group of isolates is the only identification that cannot be excluded. The probability, however, is low considering the percentage that is positive for the biochemical reactions of the S. flexneri profile. The group of isolates under study were negative for arabinose; a negative arabinose reaction is an uncommon trait for S. flexneri, which is described as 60% positive. This group of isolates was also positive for Jordan's tartrate and utilized rhamnose, which are rare traits among S. flexneri isolates. Most notable is that S. flexneri isolates are described as 95% mannitol positive, and this group of isolates was mannitol negative. S. dysenteriae is classically described as mannitol negative, but the isolates under study were raffinose and melibiose positive, which are uniformly negative in the group A designation. An interesting note, however, is that melibiose and raffinose utilizations have been described as plasmid-coded characteristics in E. coli and Salmonella (4, 25). This could explain the acquisition of these biochemical traits in a mannitol-negative Shigella sp., but further analysis, such as identification and characterization of such a plasmid, would be necessary to support this claim. S. boydii is characteristically mannitol positive, but serovars 4, 6, 9, 10, 14, and 15 have been described as mannitol negative. However, like group A Shigella, S. boydii is invariably raffinose negative (2, 15). The profile of S. sonnei is described as indole negative and mannitol positive and would seem the only nomenclature under the present considerations that could be excluded with a reasonable certainty. By phenotypic analysis, this leaves the speciation somewhat unclear; however, if one were to observe the classical taxonomy of Shigella species, the mannitol-negative characteristic would group this set of strains within the Shigella group A designation.
Combining the serological data and rfb-RFLP data for these strains would further suggest that these isolates were within Shigella group A. This group of isolates reacted with poly A sera and S. dysenteriae serovars 4 and 16 antisera, suggesting a group A similarity. The rfb-RFLP pattern of the clinical isolates was identical to that of S. dysenteriae serovar 2, so even though serological identity of these isolates was not observed with S. dysenteriae serovar 2, a genetic relationship was shown to exist. The serological reactivity observed for these isolates suggests, however, that the expression of the rfb gene cluster differs. Indeed, genes located on plasmids or on other locations of the chromosome as well as phage conversion have been cited as possible effectors of rfb gene expression (18, 19, 22). Genetic changes such as single nucleotide differences can also affect the expression of the rfb gene cluster, and these differences can fall outside the detectable range of the employed RFLP analysis. Regardless, an identical rfb-RFLP pattern and antigenic similarity to Shigella group A suggest that these organisms fall with in that group. The serological uniqueness, however, indicates that these isolates represent a novel subgroup of group A Shigella.
The six isolates characterized in this report were considered identical by way of biochemical, molecular, and serological analyses. The distinct and diverse geographical origins of the specimens and the short time span in which they were isolated raise questions about the epidemiology of this strain and its potentially widespread public health significance. The BEDP at the National Microbiology Laboratory participates in a passive surveillance program for enteric pathogens in which data on severe incidents of disease, such as outbreaks or sporadic cases of disease in known populations, are collected. Traditionally, passive systems do not provide a comprehensive view of the present situation but provide more of a “tip-of-the-iceberg” picture. Under such a surveillance system, the isolation of these six strains is an important event, as it could be an indication of an underlying health threat to Canadians. The production of new diagnostic antisera to identify this emerging strain is equally important. As a result of this investigation and production of new diagnostic antiserum, our laboratory has since been able to report three additional cases of infection by this strain of Shigella (data not shown).
This report describes a group of gram-negative bacterial isolates fitting the description of the family Enterobacteriacae that are consistent with the characteristic traits of the genus Shigella. These isolates were shown to be biochemically and antigenically unique and consistent with a group A designation. Cross-reactivity was observed with other Shigella and E. coli strains; however, by absorbing out the cross-reacting antibodies, these isolates were shown to harbor an immunological epitope that is exclusive and discriminatory and sets this group apart from all other recognized strains of Shigella. As a result of the findings of this study, we propose that these strains represent a novel emerging serovar of S. dysenteriae, type strain BEDP 02-5104.
Acknowledgments
We thank the World Health Organization collaborative center for Shigella at the CDC for the confirmatory analysis they conducted on the representative strain.
REFERENCES
- 1.Allen, J. K., C. G. Clark, D. L. Woodward, R. A. Foster, H. A. Tabor, and F. G. Rodgers. 2002. Extension of the rfb-RFLP method for determining O-serogroups of Escherichia coli and Shigella spp., poster presentation C-268. 102nd Gen. Meet. Am Soc. Microbiol. 2002. American Society for Microbiology, Washington, D.C.
- 2.Bopp, C. A., F. W. Brenner, P. I. Fields, J. G. Wells, and N. A. Strockbine. 2003. Escherichia, Shigella, and Salmonella, p. 654-671. In P. R. Murray, E. J. Baron, J. H. Jorgensen, M. A. Pfaller, and R. H. Yolken (ed.), Manual of clinical microbiology, 8th ed. ASM Press, Washington, D.C.
- 3.Bowman, C., J. Flint, and F. Pollari. 2003. Canadian Integrated Surveillance Report: Salmonella, Campylobacter, pathogenic E. coli and Shigella from 1996-1999. Can. Commun. Dis. Rep. 29(Suppl. 1):20-29. [PubMed] [Google Scholar]
- 4.Buissive, J., C. Coynault, and L. Minor. 1977. Study of the raffinose character in Escherichia coli and Salmonella. Ann. Microbiol. 128:167-183. [PubMed] [Google Scholar]
- 5.Butler, T. 2000. Shigellosis, p. 1685-1687. In L. Goldman and J. C. Bennett (ed.), Cecil textbook of medicine, 21st ed. W. B. Saunders Co., Philadelphia, Pa.
- 6.Caldeira, R. A., D. L. Woodward, W. M. Johnson, and F. G. Rodgers. 1999. Incidence of shigellosis in Canada and the emergence of new provisional serotypes. Can. J. Infect. Dis. 10:56D. [Google Scholar]
- 7.Centers for Disease Control and Prevention. 2000. Standardized molecular subtyping of foodborne bacterial pathogens by pulsed-field gel electrophoresis: training manual. Centers for Disease Control and Prevention, Atlanta, Ga.
- 8.Cheasty, T., and B. Rowe. 1983. Antigenic relationships between the enteroinvasive Escherichia coli O antigens O28ac, O112ac, O124, O136, O143, O144, O152, and O164 and Shigella O antigens. J. Clin. Microbiol. 17:681-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chin, J. (ed.). 2000. Shigellosis, p. 451-454. Control of communicable disease manual, 17th ed. American Public Health Association, Washington, D.C.
- 10.Coimbra, R. S., F. Grimont, and P. A. D. Grimont. 1999. Identification of Shigella serotypes by restriction of amplified O-antigen gene cluster. Res. Microbiol. 150:543-553. [DOI] [PubMed] [Google Scholar]
- 11.Coimbra, R. S., F. Grimont, P. Burguire, P. Lenormand, L. Beautin, and P. A. D. Grimont. 2000. Identification of Escherichia coli O-serogroups by restriction of amplified O-antigen gene cluster. Res. Microbiol. 151:639-654. [DOI] [PubMed] [Google Scholar]
- 12.Day, N. P., S. M. Scotland, and B. Rowe. 1981. Comparisons of a Hep-2 tissue culture test with the Sereny test for the detection of enteroinvasiveness in Shigella spp. and Escherichia coli. J. Clin. Microbiol. 13:596-597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donta, S. T., H. W. Moon, and S. C. Whip. 1974. Detection of heat-labile Escherichia coli enterotoxin with the use of adrenal cells in tissue culture. Science 183:334-336. [DOI] [PubMed] [Google Scholar]
- 14.Elsinghorst, E. 1994. Measurement of invasion by gentamicin resistance. Methods Enzymol. 236:405-420. [DOI] [PubMed] [Google Scholar]
- 15.Ewing, W. H. 1986. Identification of Enterobacteriacae, 4th ed. Elsevier Science Publishing Co. Inc., New York, N.Y.
- 16.Ewing, W. H., and A. A. Lindberg. 1984. Serology of Shigella. Methods Microbiol. 14:113-142. [Google Scholar]
- 17.Farmer, J. J. 2003. Enterobacteriaceae: introduction and identification, p. 636-653. In P. R. Murray, E. J. Baron, J. H. Jorgensen, M. A. Pfaller, and R. H. Yolken (ed.), Manual of clinical microbiology, 8th ed. ASM Press Washington, D.C.
- 18.Gemski, P., Jr., D. E. Koeltzow, and S. B. Formal. 1975. Phage conversion of Shigella flexneri group antigens. Infect. Immun. 11:685-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gohmann, S., P. A. Manning, C. A. Alpert, M. J. Walker, and K. N. Timmis. 1994. Lipopolysaccharide O-antigen biosynthesis in Shigella dysenteriae serotype 1: analysis of the plasmid-carried rfp determinant. Microb. Pathog. 16:53-64. [DOI] [PubMed] [Google Scholar]
- 20.Guerrant, R. L., L. L. Brunton, T. C. Schnaitman, L. I. Rebhun, and A. G. Gilman. 1974. Cyclic adenosine monophosphate and alteration of Chinese hamster ovary cell morphology: a rapid, sensitive in vitro assay for the enterotoxins of Vibrio cholerae and Escherichia coli. Infect. Immun. 10:320-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnson, W. M., and H. Lior. 1988. A new heat-labile cytolethal-distending toxin (CLDT) produced by Escherichia coli isolates from clinical material. Microb. Pathog. 4:103-113. [DOI] [PubMed] [Google Scholar]
- 22.Lai, V., L. Wang, and P. R. Reeves. 1998. Escherichia coli clone Sonnei (Shigella sonnei) had a chromosomal O-antigen gene cluster prior to gaining its current plasmid-borne O-antigen genes. J. Bacteriol. 180:2983-2986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matsushita, S., S. Yamada, Y. Kudoh, and M. Ohashi. 1990. Biochemical characteristics, growth on selective media, antimicrobial susceptibility, and diarrheagenic toxin production of enteroinvasive Escherichia coli. Kansenshogaku Zasshi 64:734-740. [DOI] [PubMed] [Google Scholar]
- 24.Mintz, E., N. Strockbine, N. H. Bean, and R. V. Tauxe. 2002. Shigella surveillance: annual summary, 2001. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, Ga.
- 25.Orskov, I., and F. Orskov. 1973. Plasmid-determined character in Escherichia coli and its relation to plasmid-carried raffinose fermentation and tetracycline resistance characters: examination of 32 H2S-positive strains isolated during the years 1950-1971. J. Gen. Microbiol. 77:487-499. [DOI] [PubMed] [Google Scholar]
- 26.Pass, M. A., R. Odedra, and R. M. Batt. 2000. Multiplex PCRs for identification of Escherichia coli virulence genes. J. Clin. Microbiol. 38:2001-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paton, A. W., and J. C. Paton. 1998. Detection and Characterization of Shiga toxigenic Escherichia coli by using multiplex PCR assays for stx1, stx2, eaeA, enterohemorrhagic E. coli hlyA, rfbO111, and rfbO157. J. Clin. Microbiol. 36:598-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pupo, G. M., R. Lan, and P. R. Reeves. 2000. Multiple independent origins of Shigella clones of E. coli and convergent evolution of many of their characteristics. Proc. Natl. Acad. Sci. USA 97:10567-10572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rahn, K., J. B. Wilson, K. A. McFadden, S. C. Read, A. G. Ellis, S. A. Renwick, R. C. Clarke, and R. P. Johnson. 1996. Comparison of Vero cell assay and PCR as indicators of the presence of verotoxigenic Escherichia coli in bovine and human fecal samples. Appl. Environ. Microbiol. 62:4314-4317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rolland, K., N. Lambert-Zechovsky, P. B. Picard, and E. Denamur. 1998. Shigella and enteroinvasive Escherichia coli strains are derived from distinct ancestral strains of E. coli. Microbiology 144:2667-2672. [DOI] [PubMed] [Google Scholar]
- 31.Sansonetti, P. J., H. d'Hauteville, C. Ecobichon, and C. Pourcel. 1983. Molecular comparisons of virulence plasmids in Shigella and enteroinvasive Escherichia coli. Ann. Microbiol. 134A:295-318. [PubMed] [Google Scholar]
- 32.Sethabutr, O., M. Venkatesan, G. S. Murphy, B. Eampokalap, C. W. Hoge, and P. Echeverria. 1993. Detection of Shigellae and enteroinvasive Escherichia coli by amplification of the invasion plasmid antigen H DNA sequence in patients with dysentery. J. Infect. Dis. 167:458-461. [DOI] [PubMed] [Google Scholar]
- 33.Tenover, F. C., R. D. Arbeit, R. V. Goering, P. A. Mickelsen, B. E. Murray, D. H. Persing, and B. Swaminathan. 1995. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J. Clin. Microbiol. 33:2233-2239. [DOI] [PMC free article] [PubMed] [Google Scholar]