Abstract
Recent studies suggest that e-cigarette use among youth may be associated with increased risk of cigarette initiation. The goal of this study was to test the hypothesis that use of e-cigarettes among young adult non-daily cigarette smokers would be associated with increased cigarette consumption.
Participants (n = 391; 52% male) were 18-24 year-old non-daily cigarette smokers recruited from across California. Cigarette and e-cigarette use were assessed online or via mobile phone every three months for one year between March 2015 and December 2016.
Longitudinal negative binomial regression models showed that, adjusted for propensity for baseline e-cigarette use, non-daily smokers who reported more frequent use of e-cigarettes upon study entry reported greater quantity and frequency of cigarette smoking at baseline and greater increases in cigarette quantity over 12 months than non-daily cigarette only smokers (ps < .01). During the 12 months of assessment, more consistent consumption of e-cigarettes was associated with greater quantity and frequency of cigarette use (ps < .01); these effects did not vary over time.
Findings suggest that among non-daily smokers, young adults who use e-cigarettes tend to smoke more cigarettes and to do so more frequently. Such individuals may be at greater risk for chronic tobacco use and dependence.
Keywords: young adult, e-cigarette, cigarette, dual tobacco
Introduction
Cigarette smoking in the US has declined for decades. Nevertheless, 20% of adults and high school students use cigarettes, and tobacco remains the primary cause of premature death (DHHS, 2014). Although there is consensus in the scientific and public health community in favor of continued effort to reduce tobacco use, the recent explosion in prevalence of newer products, particularly e-cigarettes, has complicated the picture.
Early research has focused on whether e-cigarettes aid smoking cessation. This is an important question. E-cigarettes are not risk-free but evidence suggests reduced risk relative to cigarettes (Goniewicz et al., 2014; Hecht et al., 2015). If e-cigarettes help smokers reduce consumption or quit, they could be a key public health tool. In contrast, if e-cigarettes are a barrier to reducing or quitting cigarettes, they represent a substantial risk to public health. Studies evaluating this question have yielded mixed results, but a meta-analysis found e-cigarette use was associated with 28% lower likelihood of quitting cigarettes (Kalkhoran and Glantz, 2016).
As highlighted by the U.S. Surgeon General (DHHS, 2016), there is also concern about e-cigarette use among irregular and non-smokers, particularly youth and young adults. E-cigarette use in these groups has increased dramatically (Bunnell et al., 2015), now exceeding cigarette prevalence (Johnston et al., 2016). The public health impact of e-cigarettes is in part evaluated by the potential to decrease exposure to combusted tobacco harms among dual users. It is plausible that e-cigarettes could decrease smoking by providing an alternative nicotine delivery system. Conversely, e-cigarettes may provide an additional nicotine source and thereby increase risk for dependence and increasing cigarette consumption (Durmowicz, 2014; Rigotti, 2015). In fact, recent studies suggest dual users smoke more cigarettes compared with cigarette-only users (Goniewicz et al., 2016).
Studies of the association between e-cigarette and cigarette use have focused on cigarette initiation. Among never-smoking respondents to the 2011-13 National Youth Tobacco Surveys, intent to smoke cigarettes was 70% higher among ever e-cigarette users compared with never-users (Bunnell et al., 2015). Longitudinal studies of cigarette-naïve youth and young adults found baseline e-cigarette users substantially more likely to have initiated cigarette use 6-12 months later (Barrington-Trimis et al., 2016; Leventhal et al., 2015; Primack et al., 2015; Unger et al., 2016; Wills et al., in press).
E-cigarette patterns among youth and young adults who progress to regular cigarette smoking are poorly understood. As patterns are established, individuals may favor one product over another or use e-cigarettes to limit cigarette use. The foremost potential risk of e-cigarettes is that dual users may progress more rapidly towards persistent cigarette use. Although studies suggest e-cigarette use is associated with risk for trying cigarettes, a better understanding of relationships between e-cigarette and cigarette use among dual users is needed.
The purpose of this study was to examine the relationship between e-cigarette and cigarette consumption over 12 months among young adult non-daily smokers. First, we tested the hypothesis that more frequent use of e-cigarettes during the six months prior to baseline would predict greater cigarette quantity and frequency over the next year. Second, we predicted that more consistent e-cigarette use during the 12 months of assessment would be associated with greater cigarette quantity and frequency. Supplemental analyses tested the hypothesis that e-cigarette use at any timepoint would predict greater cigarette quantity and frequency at the next timepoint.
Methods
Participants
Participants (n = 391, 52% male) were 18-24 years old (M = 20.5, SD = 1.8) and recruited for a study of young adult cigarette use. Approximately 45% identified as non-Hispanic Caucasian, 20% as Asian American, 26% as Hispanic/Latino, and 9% as other or from multiple backgrounds. Eligibility criteria included smoking cigarettes ≥ monthly for ≥ the past six months, never smoking daily for ≥ 30 days, and California residency. All assessments were conducted online or via mobile phone via SurveyMonkey (San Mateo, CA); thus, regular internet access was required.
Procedure
Participants were recruited via paid online advertisements, primarily on Facebook. Advertisements appeared to users with profiles indicating they met age and residency criteria. Accompanying text indicated that eligibility criteria included recent smoking. Eligible and interested individuals provided informed consent, then completed the baseline assessment. Additional assessments were completed 3, 6, 9, and 12 months later. Participants were compensated $25 at baseline and 12 months, and up to $40 each at 3, 6, and 9 months. Procedures were approved by the University of California, San Diego Institutional Review Board. Data were collected March 2015-December 2016. In June 2016 the legal age for purchasing cigarettes and e-cigarettes in California increased from 18 to 21 (State of California, 2016). Approximately 85% of assessments occurred before this change. Of the assessments that took place subsequently, 44% (i.e., approximately 7% of all study assessments) were of individuals aged 18-20 at the time.
Measures
Demographic characteristics were measured by self-report at baseline, and included age, sex, race, ethnicity, and student status. Student status was collapsed into a binary variable comparing full-time students (59%; any participant who reported a full-time school schedule, regardless of employment) versus others.
Cigarette and e-cigarette use were assessed at screening, baseline, and 3, 6, 9, and 12 months post-baseline. At screening, participants were asked “How frequently have you used e-cigarettes in the past 6 months?” Response options included: 0 times; 1-3 times; 1-2 times per month; weekly; 2-4 times per week; and daily/almost daily (pre-baseline e-cigarette frequency). A comparable item was used to assess cigarette frequency over the previous 6 months (pre-baseline cigarette frequency).
At baseline and 12 months, the Timeline Follow Back (TLFB) (Sobell and Sobell, 1992, 1996) was used to evaluate whether participants used e-cigarettes, as well as number of cigarettes smoked, on each of the past 14 days. The TLFB has good reliability and validity for intermittent smokers (Harris et al., 2009), and has been validated for online use (Pedersen et al., 2012; Ramo et al., 2011). At the 3, 6, and 9 month timepoints, participants completed a daily measure that included number of cigarettes smoked and whether they had used e-cigarettes in the past 24 hours. The measure was completed on 9 consecutive days, beginning on a Saturday and ending the following Sunday. Baseline and 12 month assessments included use on four weekend days and ten weekdays, whereas 3, 6, and 9 month assessments included use on four weekend days and five weekdays. In sum, raw data included the number of cigarettes smoked, and whether e-cigarettes were used, on each day assessed within each timepoint.
Raw data were collapsed to create variables reflecting cigarette quantity (total cigarettes) and frequency (cigarette days) at each timepoint: baseline and 3, 6, 9, and 12 months. Total cigarettes and cigarette days were the primary outcomes in hypothesis tests. Raw e-cigarette data were collapsed to create a binary variable for each timepoint reflecting whether participants reported any e-cigarette use. These values were used to calculate a time-varying variable reflecting the number of timepoints, up to and including the one being assessed, at which e-cigarettes were used (e-cigarette stability). For example, a participant who endorsed e-cigarette use at every timepoint would have baseline, 3, 6, 9, and 12 month e-cigarette stability values of 1, 2, 3, 4, and 5, respectively. A participant who reported e-cigarette use only at 3 and 12 months would have values of 0, 1, 1, 1, and 2. We assume that, if e-cigarette use predicts increasing cigarette consumption over time, those who use e-cigarettes more consistently across multiple timepoints are more vulnerable to this effect. Thus, our analyses included e-cigarette stability as a predictor measuring aggregate e-cigarette use over time, rather than current or recent, but not cumulative, use. To account for differences in quantity and frequency of use due to variability between timepoints in the number of assessment days, we created a time-varying variable (assessment days) measuring the number of days on which use was assessed at each timepoint.
Statistical Analyses
Bivariate tests were used to assess relationships between demographic, predictor and outcome variables, and to assess the impact of age restrictions enacted during data collection. We also examined whether cigarette and e-cigarette use differed on weekends versus weekdays, and whether outcomes differed for timepoints with a greater proportion of weekend days.
To reduce the possibility of confounding due to baseline differences we used covariate adjustment for propensity scores (Austin, 2008, 2009). The purpose of this was to maximize the similarity of measured baseline covariates between cigarette-only and dual cigarette and e-cigarette users, minimizing the possibility that effects could be explained by pre-existing differences (Austin, 2011). Logistic regression was used to model the probability of dual use at baseline. Predictors included binary (sex, student status, significant other who smoked), categorical (race/ethnicity), count (smokers in participants' households), and continuous (intent to quit cigarettes in the next year, 1-7 scale) variables. We used this model to calculate propensity scores for each participant; this variable was included as a covariate in all hypothesis tests.
Hypothesis tests were performed by fitting separate models of the associations of each predictor (pre-baseline e-cigarette use, e-cigarette stability) with each time-varying outcome (total cigarettes, cigarette days). Longitudinal negative binomial models with time-varying and time-invariant covariates were used because comparisons indicated a better fit relative to alternative choices (e.g., Poisson). Assessment days was a covariate in all analyses. In models with e-cigarette stability as the predictor, pre-baseline cigarette and e-cigarette frequency were included as covariates. Each model initially included time, time2, and their interactions with predictors. Nonsignificant interactions were not retained. All analyses were conducted using the xtnbreg module in Stata 14.0 (StataCorp LP, College Station, TX), with α = .05.
Results
Missing data
Baseline surveys were set to require responses to each item, thus there were no missing data for demographic or pre-baseline variables, or baseline cigarette or e-cigarette use. In terms of cigarette and e-cigarette use over time, the proportions of data missing at 3 month, 6 month, 9 month, and 12 month timepoints were relatively low:3%, 11%, 14%, and 9%, respectively. Eighty-seven participants (22%) had missing data at ≥ 1 assessments, but in most cases this reflected intermittent missingness. Nineteen participants (5%) were missing data at 9 and 12 months and were considered to have dropped out. Those who had missing data did not differ from the rest of the sample in terms of demographics or pre-baseline or baseline cigarette or e-cigarette use. All 87 participants with missing data were included in the analyses below, with missing data coded as missing. Missing data were not imputed because relatively few data were missing, and participants with missing data did not appear to differ from the rest of the sample (Cheema, 2014).
Preliminary analyses
During the six months pre-baseline, 19% of participants reported no e-cigarette use, 32% 1-3 uses, 27% 1-2 uses/month, 10% weekly use, 6% 2-4 uses/week, and 6% daily/almost daily use. During the 12-month study, 53% reported any e-cigarette use. Across timepoints, participants used e-cigarettes on 9-14% and cigarettes on 30-46% of days assessed. Average cigarettes/day ranged from 0.9 to 1.3. While cessation was not directly assessed, 44 participants (11.2%) denied smoking in the past 14 days at 12 months, and 23 of these (5.9%) had given the same response for the 9 days of assessment at 9 months. E-cigarette use was more frequent among males and non-students (ps<05). Older participants reported greater quantity and frequency of cigarette consumption (ps<05). Consequently, sex, age, and student status were included as covariates in hypothesis tests.
We examined whether cigarette and e-cigarette use changed following the new age restriction on tobacco. Neither cigarette nor e-cigarette use differed for those who were 18-20 when the law was enacted compared to older participants. Among the former, there were no changes in use after the restriction was implemented. Both products were used more frequently on weekends than weekdays (ps<.05). However, the likelihood and frequency of use of either product were not significantly different for timepoints that included a greater proportion of weekend days. Correlations between e-cigarette and cigarette frequency ranged from r = .07-.13 (ps<.05).
Pre-baseline e-cigarette use
Cigarette Quantity
The model of total cigarettes is shown in Table 1. There was a significant main effect of e-cigarette frequency [z=2.26, p=.024, Incidence Rate Ratio (IRR)=1.13 (95% confidence interval 1.06-1.21)], and a significant interaction with time [z=2.79, p=.005, IRR=1.16 (1.09-1.23)]. The main effect indicates that each one-category increase in e-cigarette frequency (e.g., from 1-3 uses in 6 months to monthly use) predicted a 13% increase in total cigarettes at baseline (i.e., at time=0). The significant interaction indicates that this gap widened over time. That is, for those who used e-cigarettes more often during the six months prior to the study, the slope measuring change in cigarette quantity over time was significantly higher. At baseline, those who reported ≥ 4 e-cigarette uses in the previous 6 months were smoking 1.15 cigarettes per day, compared with 0.96 for less frequent e-cigarette users. At 12 months, the group means were 1.47 and 0.42, respectively. Effect size calculations indicated that this was a large difference (d=0.72).
Table 1.
Negative binomial model of pre-baseline e-cigarette frequency and total cigarettes smoked over time.
| Predictor | Coefficient | Std. Error | z | p-value | IRR (95% ci) |
|---|---|---|---|---|---|
| Propensity score | 0.07 | 0.04 | 1.56 | .120 | 1.07 (0.98, 1.17) |
| Assessment days | 0.10 | 0.22 | 4.75 | <.001 | 1.11 (1.06, 1.16) |
| Sex | 0.30 | 0.36 | 0.84 | .401 | 1.04 (0.95, 1.14) |
| Student status | -0.32 | 0.11 | -2.77 | .006 | 0.73 (0.58, 0.91) |
| Time | 0.27 | 0.16 | 1.69 | .091 | 1.29 (0.94, 1.81) |
| Time2 | -0.11 | 0.04 | -2.65 | .008 | 0.90 (0.83, 0.97) |
| E-cigarette frequency | 0.04 | 0.02 | 2.26 | .024 | 1.13 (1.06, 1.21) |
| E-cigarette frequency × Time | 0.03 | 0.01 | 2.79 | .005 | 1.16 (1.09, 1.23) |
Cigarette Frequency
We next examined the effect of pre-baseline e-cigarette use on cigarette days over time, with similar results. The e-cigarette use × time interaction was not significant. There was a main effect of e-cigarette use [z=2.61, p=.007, IRR=1.17 (1.05-1.30)], such that each one-category increase in e-cigarette frequency predicted 17% more cigarette days. In other words, more frequent pre-baseline use of e-cigarettes was associated with more frequent cigarette smoking over the next 12 months, but the effect size did not change over that period.
E-cigarette stability over time
Cigarette Quantity
E-cigarette stability × time terms were not significant, indicating the association between e-cigarette stability and cigarette quantity was of similar magnitude across timepoints. The time2 effect was significant [z=-2.36, p=.018, IRR=0.91 (0.84-0.98)], indicating an increase in cigarette quantity from baseline to 3 months that subsequently declined. More stable e-cigarette use was associated with smoking more cigarettes [z=3.32, p=.001, IRR=1.18 (1.07-1.30); Table 2]: across the year of follow-up, each additional timepoint at which e-cigarette use was reported predicted 18% more cigarettes smoked. Comparing the opposite tails of e-cigarette stability, a participant who used e-cigarettes at every timepoint smoked more than twice as many cigarettes as a participant who never used e-cigarettes.
Table 2.
Negative binomial model of e-cigarette stability and total cigarettes smoked over time.
| Predictor | Coefficient | Std. Error | z | p-value | IRR (95% ci) |
|---|---|---|---|---|---|
| Propensity score | 0.03 | 0.02 | 1.60 | .109 | 1.03 (0.99, 1.07) |
| Assessment days | 0.10 | 0.02 | 4.74 | <.001 | 1.11 (1.06, 1.16) |
| Sex | -0.26 | 0.11 | -2.35 | .019 | 0.77 (0.62, 0.96) |
| Student status | -0.19 | 0.12 | -1.64 | .100 | 0.83 (0.66, 1.04) |
| Pre-baseline cigarette frequency | 0.62 | 0.13 | 4.65 | <.001 | 1.67 (1.32, 2.15) |
| Pre-baseline e-cigarette frequency | 0.02 | 0.05 | 0.42 | .676 | 1.02 (0.93, 1.12) |
| Time | 0.21 | 0.16 | 1.28 | .201 | 1.23 (0.89, 1.70) |
| Time2 | -0.10 | 0.04 | -2.36 | .018 | 0.91 (0.84, 0.98) |
| E-cigarette stability | 0.16 | 0.05 | 3.32 | .001 | 1.18 (1.07, 1.30) |
Cigarette Frequency
The model of cigarette frequency yielded similar results. The time [z=2.96, p=.003, IRR=1.39 (1.12-1.73)] and time2 [z=-4.21, p<.001, IRR=0.89 (0.84-0.94)] terms were both significant, indicating an initial, sample-wide increase in cigarette frequency followed by reduction over time. Interactions between time and e-cigarette stability were not significant. However, there was a main effect of e-cigarette stability [z=4.24, p<.001, IRR=1.12 (1.07-1.19)], indicating that each one-timepoint increase in e-cigarette stability predicted a 12% increase in cigarette days.
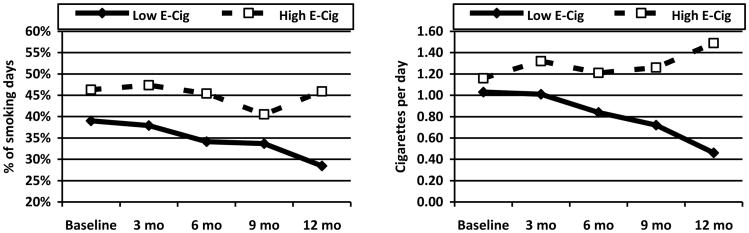
To better visualize the association between e-cigarette stability and cigarette use, we stratified the sample to compare stable e-cigarette users (e-cigarette use at ≥ 3 of 5 assessments) to light/non-users (used e-cigarettes at < 3 assessments). The former reported e-cigarette use on 30-52% of days across 12 months, compared with 2-5% for light/non-users. We plotted cigarette quantity (cigarettes per day of assessment) and frequency (proportion of days on which cigarettes were used) for both groups (Figure 1). Consistent with analyses, more stable e-cigarette users had greater cigarette quantity and frequency at each timepoint. For light and non-users of e-cigarettes, there was a negligible increase in cigarette quantity and frequency from baseline to three months, followed by a steady decline in both measures for the next nine months. In contrast, frequent e-cigarette users reported larger increases in cigarette quantity and frequency at three months. Both measures declined slightly between three and nine months, but at twelve months exceeded baseline levels.
Figure 1.
Proportion of days using cigarettes and mean cigarettes per assessment day over time by e-cigarette frequency.
Note: Low E-Cig = used e-cigarettes at two or fewer of the five assessments; High E-Cig = used e-cigarettes on three or more of the five assessments.
Supplemental analyses
To supplement hypothesis tests, we fit negative binomial models with lagged e-cigarette use as a predictor of cigarette quantity and frequency over time, including the same covariates. In both models, e-cigarette use was a binary, time-varying predictor indicating whether participants reported any e-cigarette use at each timepoint, and was lagged by one timepoint to predict cigarette outcomes at the next timepoint. Lagged e-cigarette use predicted both cigarette quantity [z=3.60, IRR=1.40 (1.17-1.68), p<.001] and frequency [z=2.33, IRR=1.18 (1.03-1.37), p=.020], such that those who used e-cigarettes at one timepoint smoked 40% more cigarettes, and used cigarettes on 18% more days, at the next timepoint.
Discussion
The goal of this study was to test the hypothesis that, among young adult non-daily cigarette smokers, more stable e-cigarette users would report increasing cigarette smoking over one year. We tested pre-baseline and contemporaneous e-cigarette use as prospective predictors of two outcomes. As expected, those who used e-cigarettes more frequently over six pre-baseline months reported more cigarettes at baseline, and the gap grew larger over 12 months. More frequent pre-baseline use of e-cigarettes also predicted greater frequency of cigarette days, but this effect did not change over time. Similarly, after accounting for pre-baseline cigarette and e-cigarette frequency, those who used e-cigarettes more consistently over 12 months also reported greater cigarette quantity and frequency. The magnitude of these effects was substantial and consistent over time–frequency increased by 12% and quantity by 18% for each additional timepoint with e-cigarette use. Lagged analyses produced similar results, with e-cigarette use at one timepoint predicting 18% greater frequency and 40% greater quantity of cigarettes at the next timepoint. Importantly, hypothesis tests controlled for propensity for dual use, reducing the possibility that differences in smoking between dual and cigarette-only users resulted from preexisting confounds (Morgan and Winship, 2007).
These data provide new evidence about the relationship between e-cigarette and cigarette use. Findings suggest young adult dual users smoke more cigarettes compared to peers who only use cigarettes. Dual users may thus be exposed to higher levels of nicotine, and accrue greater risk for chronic tobacco use and dependence. These data complement reports suggesting e-cigarette use increases risk for cigarette initiation (Leventhal et al., 2015; Wills et al., in press). Taken together, these findings suggest the popularity of e-cigarettes among younger populations is a barrier to efforts to reduce cigarette prevalence and consequences. The fact that lagged analyses produced larger effects than the analyses accounting for e-cigarette use over 12 months suggests recent e-cigarette use may have greater impact on cigarette smoking than consistency of e-cigarette use over a longer period.
Contrary to hypotheses, e-cigarette stability was not consistently associated with 12-month growth in cigarette consumption. There are multiple mechanisms that could explain this inconsistency. One possibility is that young adults who use more cigarettes may find e-cigarettes more attractive than lighter-smoking peers. That is, cigarette use may increase likelihood of e-cigarette use, rather than vice versa, although the use of propensity scores and low correlations (rs=.07-.13) between e-cigarette and cigarette frequencies at individual timepoints make this less likely. It is also possible that young adults who smoke more cigarettes use e-cigarettes to quit or reduce smoking. This cannot be addressed directly in the current study, because e-cigarette motives were not directly assessed. However, more stable e-cigarette users consistently smoked more cigarettes over 12 months, suggesting participants did not reduce smoking due to e-cigarette use. Finally, it may be that heavier e-cigarette use increases risk for progressive smoking, but the study was not sufficiently sensitive to detect it. Figure 1 suggests the possibility of continuing smoking decline among non/light users of e-cigarettes, but stable or increasing smoking among heavier e-cigarette users. If these patterns were to continue, a longer follow-up or larger sample may be necessary to detect differences.
Risk-taking research has primarily focused on minors (Steinberg, 2004, 2008), but the context of young adulthood make decisions to engage in immediately pleasurable but potentially maladaptive behavior more likely during the latter period as well (Mulye et al., 2009; Park et al., 2006). Young adults may be less likely to consider the consequences of using multiple tobacco products. This may be especially true for e-cigarettes, given the lower concern about their health effects (Kong et al., 2015). Evidence suggests that dual users smoke as many or more cigarettes than cigarette-only users (Goniewicz et al., 2016; Jorenby et al., 2017), which may result in higher levels of nicotine intake and greater risk of dependence.
Some aspects of the study limit the conclusions that can be drawn. Participants were young adults who had smoked cigarettes recently, limiting generalizability to other age groups or non-smokers. E-cigarette items did not explicitly define the product, or assess nicotine content. However, when we added an item at 12 months to address the latter, 90% of the 48 participants who completed it reported usually or always using nicotine products. Finally, the sample was recruited using Facebook advertisements targeted toward specific demographic characteristics. Participants were those who opted to learn more and to enroll; whether they are representative of non-daily smokers is unknown. Strengths of the study include the longitudinal design, including multiple days of assessment at each timepoint, analyses that accounted for propensity for dual use, and the use of continuous measures of cigarette and e-cigarette consumption. The sample included college students and other young adults, in contrast to the use of school-based samples in most previous studies of young adult e-cigarette use. Additionally, the study addresses an important public health question.
Conclusions
This study tested contrasting hypotheses regarding e-cigarette use among non-daily smokers: (1) e-cigarette use reduces smoking; (2) e-cigarette use serves to maintain but not increase smoking; and (3) e-cigarette use leads to increased smoking. E-cigarette use was consistently positively associated with cigarette quantity and frequency, thus findings contradict hypothesis 1. Results did not consistently differentiate between hypotheses 2 and 3. The effect of e-cigarettes on smoking appears unlikely to be confounded by pre-existing differences. Findings suggest e-cigarette use by young adult non-daily smokers leads to greater cigarette consumption, and thus greater risk for tobacco dependence. Additional research is needed to better understand whether this is a causal relationship and to identify long-term tobacco outcomes.
Highlights.
In young adults, e-cigarettes fostered continued or increased smoking over time
Past and concurrent e-cigarette use were similarly predictive of smoking
E-cigarettes may increase risk of chronic smoking and dependence
Acknowledgments
Funding: this work was supported by the National Institutes of Health (grant R01 DA037217 to N.D.), who provided financial support but had no other role in this project.
Footnotes
Conflicts of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Austin P. Goodness-of-fit diagnostics for the propensity score model when estimating treatment effects using covariate adjustment with the propensity score. Pharmacoepidem Dr S. 2008;17:1202–17. doi: 10.1002/pds.1673. [DOI] [PubMed] [Google Scholar]
- Austin P. An introduction to propensity score methods for reducing the effects of confounding in observatinal studies. Multivar Behav Res. 2009;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin P. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrington-Trimis J, Urman R, Berhane K, Unger J, Boley Cruz T, Pentz M, Samet J, Leventhal A, McConnell R. E-cigarettes and future cigarette use. Pediatrics. 2016;138:e20160379. doi: 10.1542/peds.2016-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunnell R, Agaku I, Arrazola R, Apelberg B, Caraballo R, Corey C, Coleman B, Dube S, King B. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013. Nicotine Tob Res. 2015;17:228–35. doi: 10.1093/ntr/ntu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheema J. Some general guidelines for choosing missing data handling methods in educational research. 2014;13:3. [Google Scholar]
- DHHS. The Health Consequences of Smoking - 50 Years of Progress: A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta: 2014. [Google Scholar]
- DHHS. Know the risks: E-cigarettes and young people. [Accessed December 12, 2014];Office of the US Surgeon General and the Centers for Disease Control and Prevention Office on Smoking and Health. 2016 at https://e-cigarettes.surgeongeneral.gov.
- Durmowicz E. The impact of electronic cigarettes on the paediatric population. Tob Control. 2014;23:ii41–ii46. doi: 10.1136/tobaccocontrol-2013-051468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goniewicz M, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tobacco Control. 2014;23:133–39. doi: 10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goniewicz M, Leigh N, Gawron M, Nadolska J, Balwicki L, McGuire C, Sobczak A. Dual use of electronic and tobacco cigarettes among adolescents: A cross-sectional study in Poland. Intl J Pub Health. 2016;61:189–97. doi: 10.1007/s00038-015-0756-x. [DOI] [PubMed] [Google Scholar]
- Harris K, Golbeck A, Cronk N, Catley D, Conway K, Williams K. Timeline follow-back versus global self-reports of tobacco smoking: A comparison of findings with nondaily smokers. Psychol Addict Behav. 2009;23:368–72. doi: 10.1037/a0015270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht S, Carmella S, Kotandeniya D, Pillsbury M, Chen M, Ransom B. Evaluation of toxicant and carcinogen metabolites in the urine of e-cigarette users versus cigarette smokers. Nicotine and Tobacco Research. 2015;17:704–09. doi: 10.1093/ntr/ntu218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston L, O'Malley P, Bachman J, Schulenberg J, Miech R. College students and adults ages 19-25. Ann Arbor: Institute for Social Research, University of Michigan; 2016. Monitoring the Future national survey results on drug use, 1975-2015: volume 2. [Google Scholar]
- Jorenby D, Smith S, Fiore M, Baker T. Nicotine levels, withdrawal symptoms, and smoking reduction success in real world use: A comparison of cigarette smokers and dual users of both cigarettes and e-cigarettes. Drug Alc Dep. 2017;170:93–101. doi: 10.1016/j.drugalcdep.2016.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. The Lancet Respiratory Medicine. 2016;4:116–28. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong G, Morean M, Cavallo D, Camenga D, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17:847–54. doi: 10.1093/ntr/ntu257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal A, Strong D, Kirkpatrick M, Unger J, Sussman S, Riggs N, Stone M, Khoddam R, Samet J, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314:700–07. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan S, Winship C. Counterfactuals and Causal Inference: Methods and Principles for Social Research. Cambridge University Press; New York: 2007. [Google Scholar]
- Mulye T, Park M, Nelson C, Adams S, Irwin C, Brindis C. Trends in adolescent and young adult health in the United States. J Adolescent Health. 2009;45:8–24. doi: 10.1016/j.jadohealth.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Park M, Mulye T, Adams S, Brindis C, Irwin C. The health status of young adults in the United States. J Adolescent Health. 2006;39:305–17. doi: 10.1016/j.jadohealth.2006.04.017. [DOI] [PubMed] [Google Scholar]
- Pedersen ER, Grow J, Duncan S, Neighbors C, Larimer ME. Concurrent validity of an online version of the Timeline Followback assessment. Psychol Addict Behav. 2012;26:672. doi: 10.1037/a0027945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack B, Soneji S, Stoolmiller M, Fine M, Sargent J. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatrics. 2015;169:1018–23. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo DE, Hall S, Prochaska JJ. Reliability and validity of self-reported smoking in an anonymous online survey with young adults. Health Psychology. 2011;30:693–701. doi: 10.1037/a0023443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigotti N. e-Cigarette use and subsequent tobacco use by adolescents: New evidence about a potential risk of e-cigarettes. JAMA. 2015;314:673–74. doi: 10.1001/jama.2015.8382. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A calendar method for assessing alcohol and drug use. Addiction Research Foundation; Toronto: 1996. [Google Scholar]
- State of California. SB-7 Tobacco products: minimum legal age. Sacramento 2016 [Google Scholar]
- Steinberg L. Risk taking in adolescence: What changes, and why? Ann NY Acad Sci. 2004;1021:51–58. doi: 10.1196/annals.1308.005. [DOI] [PubMed] [Google Scholar]
- Steinberg L. A social neuroscience perspective on adolescent risk-taking. Dev Rev. 2008;28:78–106. doi: 10.1016/j.dr.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger J, Soto D, Leventhal A. E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug Alc Dep. 2016;163:261–64. doi: 10.1016/j.drugalcdep.2016.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills T, Knight R, Sargent J, Gibbons F, Pagano I, Williams R. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. doi: 10.1136/tobaccocontrol-2015-052705. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]