Abstract
Background
There is a renewed interest in joint preservation surgery, and lateral opening wedge distal femoral osteotomy (DFO), a joint-preserving procedure, has been used to treat symptomatic genu valgum when the deformity originates in the distal femur.
Questions/Purposes
This study aimed to measure the accuracy of lateral opening wedge DFO in achieving deformity correction using radiographic parameters. In addition, the ability of lateral opening wedge DFO to improve patient outcomes as measured by Short Form Health Survey (SF-36) scores and American Academy of Orthopedic Surgeons (AAOS) lower limb module (LLM) scores leading to successful joint preservation was assessed.
Methods
The clinical charts and radiographs of 28 consecutive patients that underwent 41 DFOs (15 unilateral and 13 staged bilateral) using a locking plate construct were retrospectively reviewed. The mean age of patients undergoing DFO was 44 years (range 22–72), and 22 of the patients were female. The mean follow-up was 26 months (range 12–57 months). Preoperative and postoperative radiographs were evaluated for mechanical axis deviation (MAD), lateral distal femoral angle (LDFA), and the patella congruence angle (PCA). These measurements were compared to determine the accuracy of deformity correction. Clinical outcomes were assessed with preoperative and postoperative SF-36 and AAOS LLM, as well as Oxford knee scores at follow-up.
Results
The accuracy of deformity correction was 95%. The MAD significantly improved from 25.3 mm lateral to the midline to 8 mm medial to the midline (p < 0.01). The LDFA significantly improved from 83.4° to 91.7° (p < 0.01). The PCA significantly improved from 30.4° lateral to 5.7° lateral (p = 0.02). Mean SF-36 scores significantly improved from 37.5 to 50.2 (p = 0.01); mean LLM scores improved from 71.6 to 85.9 (p = 0.021), and the mean postoperative Oxford knee score was 35 ± 6.2 (range 23–46). No patients required total knee arthroplasty at the time of final follow-up.
Conclusion
Opening wedge lateral DFO is a reliable procedure for the treatment of valgus knee malalignment with or without arthritic changes in the lateral compartment. Deformity correction is accurate, and patient outcomes reveal significant improvement after surgery. Longer follow-up is required to access the survivorship of this procedure.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9516-6) contains supplementary material, which is available to authorized users.
Keywords: genu valgum, lateral opening wedge, distal femoral osteotomy (DFO), lateral patella subluxation, lateral patellar retinacular release
Introduction
Symptomatic genu valgum is a common deformity that can affect patients of all ages. It often causes pain and progressive osteoarthritis from overloading of the lateral joint compartment [8]. When osteoarthritis becomes advanced, partial or total knee arthroplasty may be indicated to treat this condition. While arthroplasty is reliable for elderly patients with advanced arthritis, there are distinct advantages for a joint preservation approach for younger and more active individuals with mild or moderate joint degeneration. Common problems associated with partial or total knee replacement in younger patients include limited durability and function over time as well as an increased risk of revision surgery [5, 15]. Subsequently, there has been a renewed interest in joint-preserving osteotomies around the knee. Realignment osteotomies can offload the affected joint compartment and subsequently reduce the pain associated with knee osteoarthritis, delay the progression of the arthritis, and improve aesthetics.
Distal femoral osteotomy (DFO) has been used to correct genu valgum when the deformity originates from the distal femur [3, 5, 8, 16]. Furthermore, genu valgum can be associated with lateral patella subluxation or even dislocation [10, 14]. Combined with a lateral retinacular release, a varus producing DFO will correct the Q angle and improve patellar tracking. There are two ways to perform a DFO: a medial closing wedge or a lateral opening wedge osteotomy. A common technique that has been performed to correct genu valgum is medial closing wedge DFO given its predictable bony union and recovery [17–19]. However, most surgeons consider this procedure to be technically difficult, and there are reports of several complications such as non-union, hardware failure, as well as overcorrection and undercorrection [5]. Conversely, lateral opening wedge DFO requires only a single bone cut sparing the medial cortex followed by incremental spreading of the lateral cortex, making the procedure theoretically easier and more accurate since it offers better control of the deformity correction [3].
The majority of previous studies have focused on medial closing wedge DFO [7, 9, 11, 16–19], and there is limited literature on the use of lateral opening wedge DFO to correct symptomatic genu valgum. In addition, previous studies evaluating the accuracy of deformity correction use only one radiographic parameter [3, 5, 8, 15, 18], and very few studies describe clinical outcomes after surgery. Similarly, few studies describe deformity correction and clinical outcomes using the Tomofix® plate (Synthes, West Chester, PA, USA), since the majority of previous reports describe the use of the Puddu plate (Arthrex, Naples, Florida, USA) [5, 18].
The purpose of this study is to describe our technique of DFO, review a consecutive series of patients, and assess the accuracy of deformity correction and clinical outcomes after a lateral opening wedge DFO. Specifically, we wished to assess how accurate is lateral opening wedge DFO in achieving deformity correction for symptomatic genu valgum with or without patellar instability based on radiographic parameters. In addition, we studied how well lateral opening wedge DFO improves patient outcomes and leads to successful joint preservation as measured by Short Form Health Survey (SF-36) scores, American Academy of Orthopedic Surgeons (AAOS) lower limb module (LLM) scores, and the Oxford knee score.
Patients and Methods
This study is a retrospective review of a consecutive series of 28 patients that underwent a lateral opening wedge DFO at a major academic medical center. These patients underwent 41 DFOs (15 unilateral and 13 staged bilateral) between June 2010 and October 2014. Patients had a mean age of 44 years (range 22–72), and 22 patients were female. All patients were treated with the lateral opening wedge DFO using a locking titanium plate and screws. The indication for osteotomy was lateral knee pain and genu valgum deformity. In all cases, the deformity was idiopathic, and patients had a primary complaint of pain. Patients with Kelligren-Lawrence grade 3 and 4 changes were not indicated for joint-preserving surgery. More specifically, patients with severe osteoarthritis characterized by marked joint space narrowing, multiple osteophytes, and joint line obliquity were not considered for this procedure. Mean follow-up for all patients was 26 months (range 12–57 months).
The goals for coronal plane correction were based on the absence or presence of degenerative changes in the lateral compartment, and they were determined preoperatively. The goal for patients without degenerative changes was to restore mechanical axis to neutral, while the goal for patients with degenerative changes was to overcorrect the mechanical axis to the medial aspect of the joint. Mechanical axis planning was used [6, 13]. The distal mechanical axis of the femur was drawn, and a retrograde line was generated. The proximal femur mechanical axis was drawn, and an antegrade line was generated. The intersection of these lines determined the center of rotation and angulation (CORA) and the magnitude of the deformity [13]. If the location of the CORA was not at the optimal location for the DFO or if overcorrection was the goal, then intentional placement of the apex of deformity was performed as described by Fabricant et al. [6].
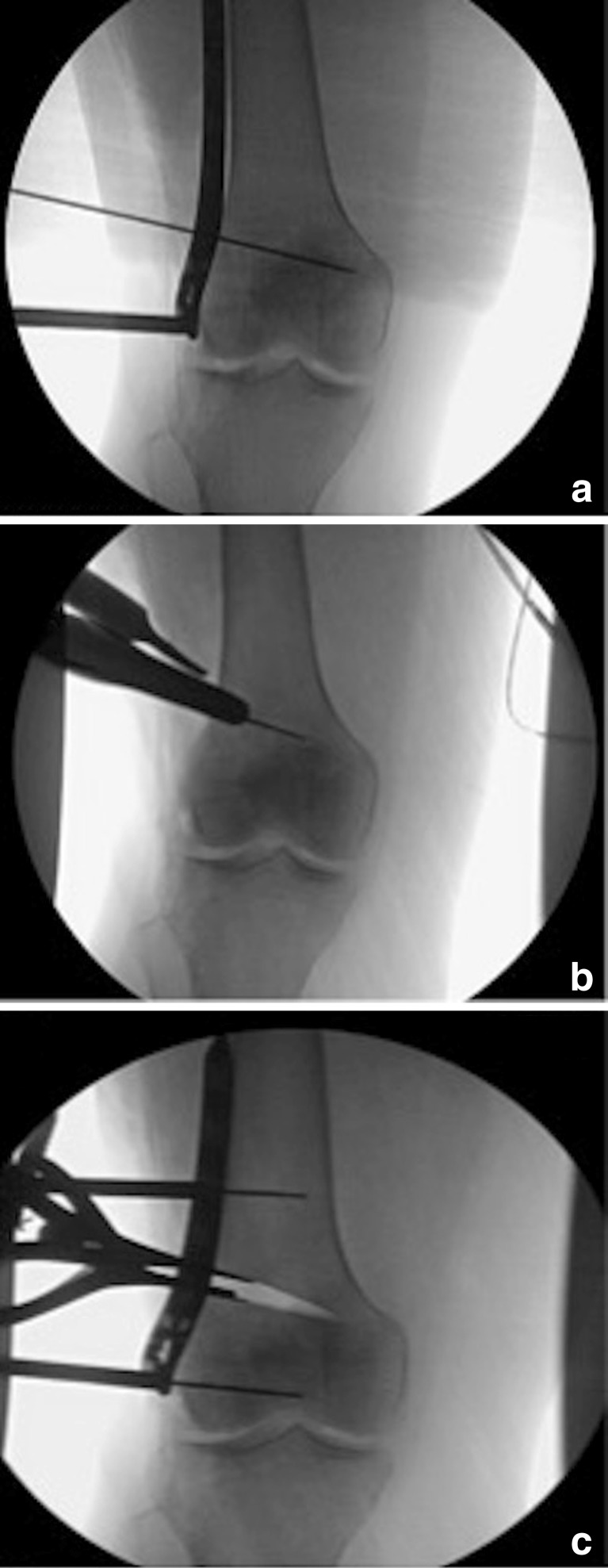
All patients received spinal anesthesia and were then positioned supine on a radiolucent table. A bump was placed under the ipsilateral buttock to maintain the leg in a neutral rotational position. The entire limb was prepped and draped into the field, and a sterile tourniquet was used. A 6-in incision was made over the lateral distal femur. The iliotibial band was incised, and the vastus lateralis was elevated and dissected off the lateral intermuscular septum to expose the lateral distal femoral shaft. If needed, lateral patellar retinacular release for patellar instability was performed through the same incision. Under fluoroscopic guidance, the starting point for the osteotomy was identified approximately 3 cm proximal to the lateral femoral epicondyle. The plate was temporarily placed on the lateral cortex to help confirm the location of the osteotomy, and the goal was to place five screws in the distal fragment. A K wire was inserted through the plate as a guide for the osteotomy, and this wire was aimed toward the base of the metaphyseal flare proximal to the medial epicondyle. The wire was inserted in an oblique manner and not parallel to the joint, since the medial metaphyseal bone is elastic and less likely to crack when opening the lateral wedge. This wire was also parallel to the floor with the patella pointing straight up, and its trajectory remained proximal to the articular surface of the trochlea. The osteotomy was performed using a 40-mm microsagittal saw while cooled with saline. Approximately 1 cm of the medial cortex was left intact in order to hinge the osteotomy and provide additional stability. Laminar spreaders were used to create an opening wedge at the osteotomy site based on preoperative planning (Fig. 1a–c). Once the amount of planned correction was obtained, lateral fluoroscopic images were obtained to ensure that there was no flexion or extension at the osteotomy site. If indicated, sagittal plane correction was performed at this time by opening the osteotomy anteriorly or posteriorly as needed. Limb alignment was then checked fluoroscopically and clinically using a metal rod placed over the center of the hip and ankle. Neutral mechanical axis was defined by the rod passed through the center of the knee, and in some cases, medial overcorrection was the desired goal (Fig. 2). Once alignment was confirmed, the locking Tomofix® plate (Synthes, West Chester, PA, USA) was placed and fixed with screws. After plate fixation, bone grafting was performed using allograft freeze-dried cancellous chips and grafton demineralized bone matrix (DBM) putty (Medtronic, Dublin, Ireland). Five patients had additional bone marrow aspirate concentrate (BMAC) injected into the osteotomy site, and one patient had grafton DBM putty and BMAC without freeze-dried cancellous chips. Closure was performed in layers.
Fig. 1.
Intraoperative fluoroscopy images showing a guide pin insertion in the designated trajectory of the osteotomy, b the osteotomy performed by microsagittal saw, and c laminar spreaders used to create an opening wedge at the osteotomy site based on preoperative planning.
Fig. 2.
Intraoperative picture showing alignment check under fluoroscopy using a metal rod.
In total, eight patients had concomitant sagittal plane correction through flexion or extension at the osteotomy site, and four patients underwent tibial osteotomy for simultaneous correction of valgus tibial deformity using a circular hexapod frame. Additionally, three patients had concomitant knee arthroscopy, and eight patients underwent lateral retinacular release for patellar instability. Lastly, two patients underwent a tibial tubercle transfer for patella realignment.
A standard postoperative protocol was used for all patients. This protocol included 30 lb partial weight-bearing for 6 weeks, in addition to immediate range of motion (ROM) exercises of the knee using a continuous passive motion (CPM) device. Weight-bearing was gradually advanced over the next 6 weeks based on radiographic progression of bone healing, and full weight-bearing was usually achieved by 6 weeks. All patients performed postoperative physical therapy for strengthening, stretching, as well as active and passive ROM of the knee. Follow-up with radiographs was performed at 2 weeks, 6 weeks, 3 months, and 6 months postoperatively. No bracing or casting was performed.
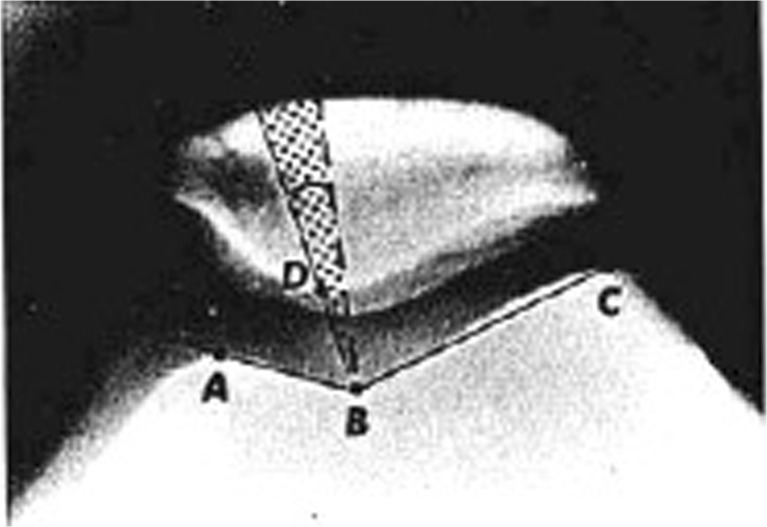
All patients had 51″ full-length, standing AP radiographs preoperatively and postoperatively. All radiographic measurements including the mechanical axis deviation (MAD), lateral distal femoral angle (LDFA) [13], and patella congruency angle (PCA) [2] were performed by a limb lengthening and reconstructive surgery fellow (OME) using the methods described by Paley [13]. In order to determine the PCA, a Merchant knee X-ray of the patient’s knees was obtained. The PCA was measured by drawing a line bisecting the sulcus angle and then measuring the angle between the bisecting line and another line connecting the apex of the sulcus to the lowest aspect of the patellar ridge (Fig. 3). By convention, the PCA is negative since the lowest part of the patella is medial to the bisecting line; however, normal values are −6° ± 11° [2]. Bone healing was assessed radiographically and clinically by assessing for pain and tenderness on history and exam.
Fig. 3.
Plain axial knee radiograph showing measurements of the sulcus angle (angle between lines AB–BC) and the patella congruence angle (PCA) between a line bisecting the sulcus angle and a line connecting the apex of the sulcus to the lowest part of patellar ridge (BD) (normal value of PCA −6 ± 11). Figure obtained with permission from Wolters Kluwer Health, Aglietti P, Insall JN, Cerulli G. Patellar Pain and Incongruence. I: Measurements of Incongruence. Clin Orthop Relat Res. 1983; 176: 217–224.
To determine the accuracy of correction, Eq. 1 was used. First, the error of the correction was calculated by subtracting the achieved MAD from the goal MAD divided by the goal MAD. For the neutral group, the goal was 0 ± 5 mm (acceptable range was between 5 mm lateral and 5 mm medial). For the overcorrection group, the goal was 10 mm medial ± 5 mm (acceptable range was between 5 mm medial and 15 mm medial). Once the error was calculated, the accuracy was determined by subtracting the error from 1.
| 1 |
SF-36, American Academy of Orthopedic Surgeons LLM, and Oxford knee scores were used to assess patient outcomes. The SF-36 is commonly used to measure general health status, and scores range from 0 to 100, with 100 representing the optimal score [12]. LLM scores measure general lower limb problems and range from 0 to 100, with 100 representing the best possible outcome [1]. The Oxford knee score is knee specific and used to assess outcomes after knee surgery, including osteotomies. Oxford knee scores range from 0 to 48 with higher scores indicating better joint function [4]. Preoperative scores were obtained at a patient’s initial visit, and postoperative scores were obtained at the most recent visit; however, some patients did not complete the surveys. Preoperative and postoperative SF-36 and LLM scores were available for 9 patients (15 knees), and postoperative Oxford knee scores were available for 16 patients (25 knees).
Continuous variables are reported in means, standard deviations, and ranges. Evaluation of radiographic measures for deformity correction accuracy was done using paired samples t tests. Similarly, the change in patient-reported outcome measures was also assessed using paired samples t tests. As the Oxford knee score was only recorded postoperatively, simple descriptive statistic of the score was reported. Statistical significance was defined as a p value of 0.05 or less. All analyses were conducted using SPSS version 22.0 (IBM Corp., Armonk, NY). Post hoc power analyses performed for all outcome measures found that the sample sizes used were sufficiently powered to detect the statistical differences found for all preoperative and postoperative measures of change. Minimally clinically important difference was exceeded for the AAOS lower limb module, and, on average, a normative SF-36 score was achieved postoperatively for the study population.
Results
All patients achieved bony union, and the mean time to union was 3.2 months (range 2.5–6 months). The average accuracy of deformity correction was 95% (range 33.3–100%). The MAD significantly improved from 25.3 ± 12.6 mm lateral to the midline (range 4–54) to 8 ± 8 mm medial to the midline (range 0–29) (p < 0.001). The LDFA significantly improved from 83.4° ± 2° (range 77°–86°) to 91.7° ± 2.5° (range 86°–96°) (p < 0.001) (Table 1).
Table 1.
Average preoperative and postoperative mechanical axis deviation (MAD), lateral distal femoral angle (LDFA), and patella congruency angle (PCA) measurements
| Radiographic parameters | Average preop | Average postop | p value |
|---|---|---|---|
| MAD | 25.3 ± 12.6 mm lateral (range 4–54) | 8 ± 8 mm medial (range 0–29) | <0.001 |
| LDFA | 83.4° ± 2° (range 77°–86°) | 91.7° ± 2.5° (range 86°–96°) | <0.001 |
| PCA | 30.4° ± 16.8° lateral (range 14°–53°) | 5.7° ± 17.8° lateral (range: 15° medial–35° lateral) | 0.018 |
In our case series, eight patients (10 knees) had concomitant patellar instability that was diagnosed clinically and radiographically. In addition to a lateral opening wedge DFO, these patients underwent a lateral retinacular release to restore normal patellar alignment. Preoperative measurements were performed for all 10 knees; however, postoperative merchant radiographs were performed for only seven knees. Compared to preoperative measurements, the PCA significantly improved from 30.4° ± 16.8° lateral (range 14°–53°) to 5.7° ± 17.8° lateral (range 15° medial–35° lateral) (p = 0.016) (Table 1). Based on normal PCA values, four out of the seven knees normalized after surgery and all patients had an improvement in patellar tracking.
As mentioned above, preoperative and postoperative SF-36 and LLM scores were available for 9 patients (15 knees), and postoperative Oxford knee scores were available for 16 patients (25 knees). SF-36 scores significantly improved from 37.5 ± 14.5 preoperatively to 50.2 ± 7.6 postoperatively (p = 0.012). LLM scores significantly improved from 71.6 ± 16.4 preoperatively to 85.9 ± 9.3 postoperatively (p = 0.021). The mean postoperative Oxford knee score was 35 ± 6.2 (range 23–46) (Tables 2 and 3). According to the Oxford score outcomes, none of the patients were considered to have severe arthritis at follow-up (Table 3).
Table 2.
Short Form (36) Health Survey (SF-36), American Academy of Orthopedic Surgeons lower limb module (LLM) and Oxford knee scores
| Outcome Scores | Preop | Postop | p value |
|---|---|---|---|
| SF-36 | 37.5 ± 14.5 | 50.2 ± 7.6 | 0.012 |
| LLM | 71.6 ± 16.4 | 85.9 ± 9.3 | 0.021 |
| Oxford | 35 ± 6.2 (range 23–46) | n/a |
Table 3.
Postoperative Oxford knee scores
| Oxford score | Interpretation | Number of patients |
|---|---|---|
| 0–19 | Severe arthritis | 0 |
| 20–29 | Moderate to severe arthritis | 4 |
| 30–39 | Mild to moderate arthritis | 7 |
| 40–48 | Satisfactory joint function | 5 |
Complications were noted in three patients and included deep venous thrombosis (DVT), knee contracture treated with manipulation under anesthesia (MUA), and delayed bony union treated with iliac crest bone graft and bone morphogenic protein. The delayed union occurred in the patient treated without freeze-dried allograft chips. At the time of final follow-up, none of the patients have undergone total knee replacement.
Discussion
Given the increased interest in joint preservation techniques, it is important to study the accuracy and outcomes of osteotomies around the knee [15]. Lateral opening wedge DFO is an accurate and successful procedure at correcting symptomatic genu valgum deformity. Furthermore, there is a significant improvement in patient outcomes after surgery.
Our study had several limitations. To begin with, we did not have patient outcome scores on all patients, and only postoperative Oxford knee scores were obtained. Secondly, this study is a retrospective review of 28 patients, which limits its generalizability, and larger studies may be helpful in the future. Furthermore, a handful of patients had secondary procedures which may affect outcomes. Finally, longer follow-up is required to determine long-term outcomes and further evaluate the survivorship of lateral opening wedge DFO.
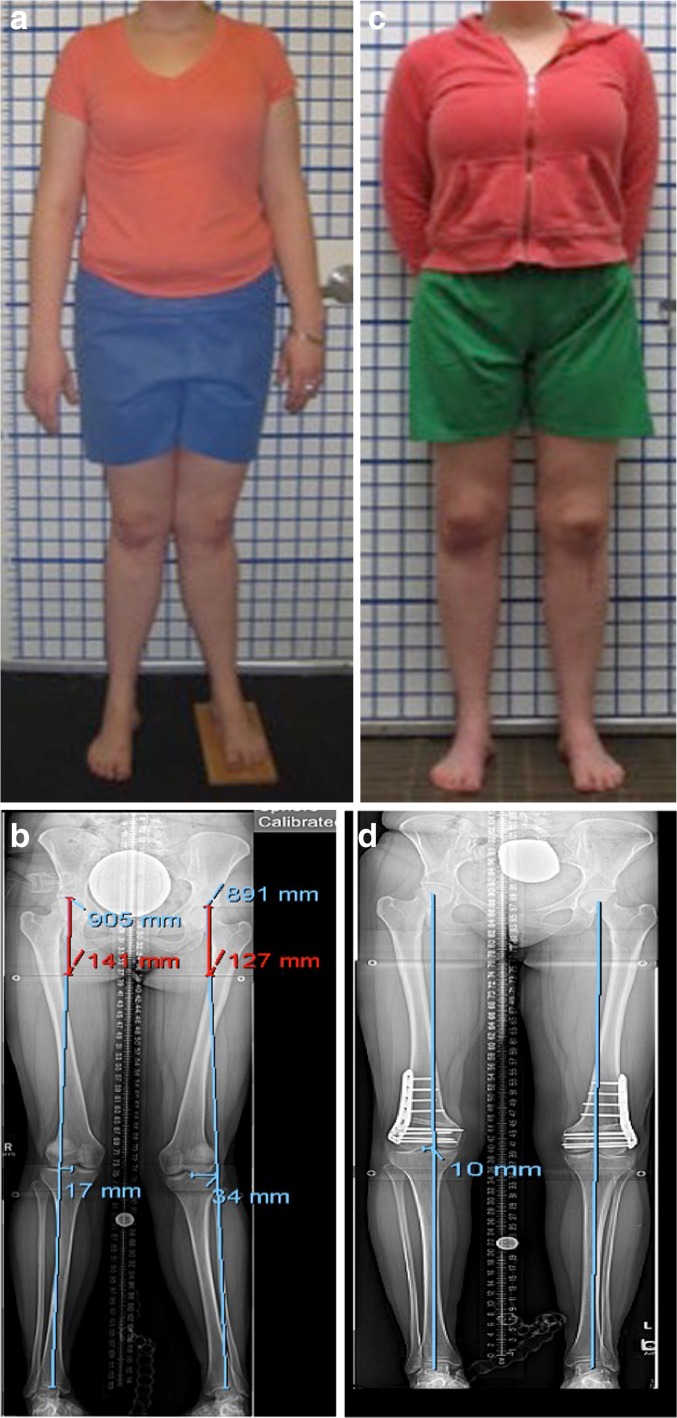
We were able to achieve our goal of neutral or overcorrected mechanical alignment with a high degree of accuracy (95%) (Fig. 4a–d). The accuracy was confirmed based on the use of two radiographic measurements of deformity: MAD and LDFA. Only a handful of studies on this technique have been published within the past 5 years (Table 4). The majority of these studies used only one radiographic parameter to measure accuracy, most commonly the tibio-femoral angle or the mechanical axis [3, 5, 8, 15, 18]. Cameron et al. reported that the lateral opening wedge DFO was less accurate in correction of valgus deformity when using MAD [3]. Conversely, Dewilde et al. reported that lateral opening wedge DFO was comparable to the medial closing wedge technique with good results [5]. Our findings provide additional confidence to joint preservation surgeons performing lateral opening wedge DFO.
Fig. 4.
Case illustration: a preoperative clinical picture, b preoperative radiograph, c postoperative clinical picture, and d postoperative radiograph of a patient with symptomatic genu valgum.
Table 4.
Reports of lateral opening wedge DFO published within the past 5 years
| Authors | No. of knees | Fixation plate | Radiographic measure(s) | Bone graft used | Outcome scores used | Complications |
|---|---|---|---|---|---|---|
| Jacobi et al. [7] | 14 | Tomofix | None | Iliac crest autograft (7 out of 14) | • Knee Injury and Osteoarthritis Outcome Score (KOOS) (31 ± 17 preop to 69 ± 22 postop) | • Hardware irritation (12) • Delayed/non-union (7) |
| Thein et al. [16] | 7 | Puddu | • Tibiofemoral angle (13.5 ± 4.1 to 1.6 ± 2.1) • Insall-salvati index (no alteration in patellar height) • Kellgren-Lawrence Grading Scale (unchanged) |
Iliac crest allograft | • Oxford knee score (13.1 ± 8.6 to 26 ± 12.5) | • No hardware failures, delayed or non-union |
| Dewilde et al. [5] | 19 | Puddu | • Tibiofemoral angle (5.3 ± 2.5 to −1.3 ± 4.0) | Calcium phosphate bone cement | • Knee Society Knee Score (43 ± 8 to 78 ± 23) • Kellgren-Lawrence osteoarthritis score (unchanged) |
• Hardware irritation (4) |
| Cameron et al. [3] | 31 | Dynafix (23), Puddu (6), Tomofix (1) | • Mechanical axis (arthritis group 7° valgus preop to 2° varus postop; joint preservation group: 5° valgus preop to varus postop) | Iliac crest autograft + cancellous allograft | • International Knee Documentation Committee (IKDC) [arthritis group: 47 preop to 67 postop; joint preservation group: 36 preop to 62 postop] | • Hardware irritation (5) • Non-union (1) |
| Saithna et al. [14] | 21 | Puddu (16), TomoFix (5) | • Mechanical axis [% from medial to lateral 75% (range 60–90) preop to 37% (range 10–58) postop] | No grafts unless opening was greater than 12 mm | • IKDC (36.4 to 52.6) • KOOS pain (49.1 to 70.3) • SF-36 (79.8 to 88.7) • Lysholm score (48.5 to 54) • Tegner Score (2.8 to 3.2) |
• Hardware irritation (10) • Non-union (1) • Delayed union (1) • Loss of correction (2) |
| Elattar et al.a | 41 | Tomofix | • Mechanical axis (25.3 ± 12.6 mm lateral preop to 8 ± 8 mm medial postop) • LDFA (83.4° ± 2° preop to 91.7° ± 2.5° postop) • PCA (30.4° ± 16.8° lateral preop to 5.7° ± 17.8° lateral postop) |
Allograft cancellous chips + grafton DBM putty | • SF-36 scores (37.5 to 50.2) • LLM scores (71.6 to 85.9) • Oxford knee score (35 postop) |
• Delayed union (1) |
Dynafix1 VS plates (Biomet, Warsaw, IN, USA), calcium phosphate bone cement (Biobon, Biomet Merck, Darmstadt, Germany)
aCurrent study
To our knowledge, no large studies have been published on the use of lateral opening wedge DFO to address patellar instability associated with genu valgum. There are two case reports discussing the use of DFO for patellar instability [10, 14]; however, these studies do not report patella-specific radiographic outcomes or validated patient outcomes. In our study, we found significant improvement in the PCA, as well as normalization of PCA in approximately half of the patients with patellar instability. These findings suggest that lateral opening wedge DFO with a lateral release is a reasonable surgical option in patients with patellar instability associated with genu valgum.
Similar to previous studies, we found significant improvements in patient outcomes after lateral opening wedge DFO. Using the International Knee Documentation Committee (IKDC) score, Cameron et al. reported improved pain and function outcomes [3]. Likewise, even though Jacobi et al. observed delayed union, patient satisfaction, pain, and function scores improved postoperatively when using the Knee Injury and Osteoarthritis Outcome Score (KOOS). Our findings confirm that significant improvement can be expected after a lateral opening wedge DFO, and patients with symptomatic genu valgum may benefit from this joint-preserving technique. Furthermore, postoperative Oxford knee scores in our study are identical to 2-year scores after total knee arthroplasty from a large observational study [20]. Additional follow-up is needed to better understand long-term trends in these patients.
Additionally, all patients except for one in our study progressed to union without additional surgery. This was contrary to what has been reported in some studies. Jacobi et al. experienced significant delayed union while using the same technique and fixation [8]. As a result, the author abandoned the use of a lateral opening wedge osteotomy. However, the delayed union may have been attributed to the type of bone graft used to fill the osteotomy site, since only iliac crest graft was used and not all patients received bone graft. In a study by Dewilde et al., a calcium phosphate bone cement graft was used and delayed union was not observed [5]. It is important to note that the majority of published studies use the Puddu plate [Arthrex, Naples, FL, USA] for fixation. Aside from Jacobi et al., this study is one of the few studies to evaluate the accuracy and outcome of lateral opening wedge DFO using only the Tomofix plate. The Tomofix plate is a sturdy, locking plate that uses 5-mm screws. Intraoperatively, the distal segment is stabilized with five screws, and the proximal segment is stabilized with four bicortical screws.
Moreover, failure of fixation and infection was not observed in any of our patients. In this study, only one patient required a re-operation, and this was secondary to delayed union. In this patient, BMAC and DBM without allograft chips were used in the index procedure, which again underscores the importance of the type of bone graft. We feel that the use of an osteoinductive scaffold like freeze-dried allograft chips is essential in this environment given the presence of excellent blood supply, large surface area, and adequate stability.
Other authors have reported varying re-operation rates primarily due to complications of hardware irritation. In a study by Dewilde et al., 4 out of 19 knees required hardware removal [5], and Cameron et al. reported hardware removal in 5 out of the 31 knees [3]. Similarly, Jacobi et al. reported hardware removal in 12 out of 14 knees [8], and Saithna et al. reported hardware removal in 10 out of 21 knees [15]. In this study, 16 out of 41 knees had hardware removed. However, unlike the other studies, we did not consider this a complication, since it is considered to be a part of our standard protocol.
Lateral opening wedge DFO with locked plate fixation is a reliable and accurate procedure for the treatment of symptomatic genu valgum. This procedure provides improved pain and functional outcomes in patients, as well as predictable bone healing at the osteotomy site. Overall, the findings from this study improve our understanding of surgical and patient outcomes after lateral opening wedge DFO, and it allows joint preservation surgeons to better counsel patients regarding outcomes. Future studies should focus on larger cohorts with longer follow-up to assess survivorship and long-term outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Osama Elattar, MD, Ishaan Swarup, MD, Aaron Lam, BS, and Joseph Nguyen, MPH have declared that they have no conflict of interest. Austin Fragomen, MD, reports personal fees from Synthes, Smith & Nephew, and NuVasive, outside the work. S. Robert Rozbruch, MD, reports personal fees from NuVasive/Ellipse, Smith & Nephew, and Stryker, outside the work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
This study was completed at Hospital for Special Surgery, New York, NY.
Level of Evidence: IV: Therapeutic Study
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9516-6) contains supplementary material, which is available to authorized users.
References
- 1.AAOS. Web. 23 Dec 2015. http://www.aaos.org/outcomesinstruments/
- 2.Aglietti P, Insall JN, Cerulli G. Patellar Pain and Incongruence. I: Measurements of Incongruence. Clin Orthop Relat Res. 1983;176:217–224. [PubMed] [Google Scholar]
- 3.Cameron JI, McCauley JC, Kermanshahi AY, Bugbee WD. Lateral Opening-wedge Distal Femoral Osteotomy: Pain Relief, Functional Improvement, and Survivorship at 5 Years. Clin Orthop Relat Res. 2014;473(6):2009–2015. doi: 10.1007/s11999-014-4106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg (Br) 1998;80-B(1):63–69. doi: 10.1302/0301-620X.80B1.7859. [DOI] [PubMed] [Google Scholar]
- 5.Dewilde TR, Dauw J, Vandenneucker H, Bellemans J. Opening wedge distal femoral varus osteotomy using the Puddu plate and calcium phosphate bone cement. Knee Surg Sports Traumatol Arthosc. 2013;21:249–254. doi: 10.1007/s00167-012-2156-6. [DOI] [PubMed] [Google Scholar]
- 6.Fabricant PD, Camara JM, Rozbruch SR. Femoral Deformity Planning: Intentional Placement of the Apex of Deformity. Orthopedics. 2013;36(5):e533–7. doi: 10.3928/01477447-20130426-11. [DOI] [PubMed] [Google Scholar]
- 7.Freiling D, Lobenhoffer P, Staubli AE, Van Heerwaarden RJ. Medial closed-wedge varus osteotomy of the distal femur. Arthroskopie. 2008;21:6–14. doi: 10.1007/s00142-007-0416-0. [DOI] [PubMed] [Google Scholar]
- 8.Jacobi M, Wahl P, Bouaicha S, Jakob RP, Gautier E. Distal femoral varus osteotomy: problems associated with the lateral open-wedge technique. Arch Orthop Trauma Surg. 2011;131:725–728. doi: 10.1007/s00402-010-1193-1. [DOI] [PubMed] [Google Scholar]
- 9.Kosashvili Y, Safir O, Gross A, Morag G, Lakstein D, Backstein D. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: a minimum ten-year follow-up. Int Orthop. 2010;34:249–254. doi: 10.1007/s00264-009-0807-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwon JH, Kim JI, Seo DH, Kang KW, Nam JH, Nha KW. Patellar Dislocation With Genu Valgum Treated by DFO. Orthopedics. 2013;36(6):840–3. doi: 10.3928/01477447-20130523-35. [DOI] [PubMed] [Google Scholar]
- 11.McDermott AG, Finklestein JA, Farine I, Boynton EL, MacIntosh DL, Gross A. Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am. 1988;70:110–116. doi: 10.2106/00004623-198870010-00017. [DOI] [PubMed] [Google Scholar]
- 12.McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Paley D, Tetsworth K. Mechanical Axis Deviation of the Lower Limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res. 1992;280:48–64. [PubMed] [Google Scholar]
- 14.Purushothaman B, Agarwal A, Dawson M. Posttraumatic Chronic Patellar Dislocation Treated by Distal Femoral Osteotomy and Medial Patellofemoral Ligament Reconstruction. Orthopedics. 2012;35(11):e1668–72. doi: 10.3928/01477447-20121023-30. [DOI] [PubMed] [Google Scholar]
- 15.Saithna A, Kundra R, Getgood A, Spalding T. Opening wedge distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. Knee. 2014;21(1):172–175. doi: 10.1016/j.knee.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Seah KT, Shafi R, Fragomen AT, Rozbruch SR. Distal Femoral Osteotomy: Is Internal Fixation Better than External? Clin Orthop Relat Res. 2011;469:2003–2011. doi: 10.1007/s11999-010-1755-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sternheim A, Garbedian S, Backstein D. Distal femoral varus osteotomy: unloading the lateral compartment: long-term follow-up of 45 medial closing wedge osteotomies. Orthopedics. 2011;34:e488–490. doi: 10.3928/01477447-20110714-37. [DOI] [PubMed] [Google Scholar]
- 18.Thein R, Bronak S, Thein R, Haviv B. Distal femoral osteotomy for valgus arthritic knees. J Orthop Sci. 2012;17:745–749. doi: 10.1007/s00776-012-0273-1. [DOI] [PubMed] [Google Scholar]
- 19.van Heerwaarden RJ, Wymenga AB, Freiling D, Lobenhoffer P. Distal medial closed wedge varus femur osteotomy stabilized with the tomofix plate fixator. Oper Tech Orthop. 2007;17:12–21. doi: 10.1053/j.oto.2006.09.008. [DOI] [Google Scholar]
- 20.Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE. Long-term trends in the Oxford knee score following total knee replacement. Bone Joint J. 2013;95-B(1):45–5. doi: 10.1302/0301-620X.95B1.28573. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)