Abstract
Background
Optimal treatment of chronic scapholunate (SL) instability remains controversial. Many surgical techniques have been proposed with varied results in subsequent case series; however, there is limited evidence demonstrating the relative effectiveness of the different treatment options.
Questions/Purposes
We conducted a systematic review of the English literature to compare outcomes from capsulodesis and ligament reconstruction for treatment of chronic scapholunate instability.
Methods
An electronic database search using keywords associated with scapholunate ligament instability was performed. A total of 511 studies were identified. All studies with scapholunate ligament tears >4 weeks after the initial injury were included in the review. Data extracted included patient demographics, wrist range of motion, and radiographic outcome measures.
Results
A total of 308 patients from 11 studies met the inclusion criteria and were included in the study. The average time to surgery from initial injury was 11 months. There was no significant difference in wrist flexion or extension after capsulodesis or reconstruction. The weighted mean for postoperative wrist extension/flexion was 56°/45.6° in the capsulodesis group and 40.9°/47.3° in the reconstruction group. Pooled means of SL angle and SL gap were 60.3° and 3.44 mm after capsulodesis and 56.5 and 2.72 mm after reconstruction, respectively.
Conclusions
This systematic review failed to demonstrate any significant difference in outcomes from capsulodesis or reconstruction for treatment of chronic scapholunate instability. However, the retrospective studies examined were notably heterogeneous in design with high estimates of variance. Further prospective trials are necessary to determine an ideal treatment strategy.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9525-5) contains supplementary material, which is available to authorized users.
Keywords: scapholunate, scapholunate ligament, repair, capulodesis, tenodesis, reconstruction, brunelli
Introduction
Scapholunate ligament (SLL) tear represents the most frequent ligamentous injury of the wrist and is the most common etiology of carpal (wrist) instability [22]. Acute injury typically results in pain and impairment of functional activity. When left untreated, a complete tear leads to altered wrist biomechanics, eventual wrist arthritis, and further functional impairment [23]. Numerous studies have demonstrated that disruption of the ligamentous connection between the scaphoid and lunate causes rotatory subluxation of the scaphoid and increases contact pressure in the articulation between the scaphoid and radius [4, 5].
While there is substantial clinical concern about the long-term implications of this injury among treating physicians, surprisingly little is known about the natural history of the SLL tears or the therapeutic value of the procedures used to treat the injury. After the acute injury time period (4–6 weeks), surgical treatment focuses on minimizing the altered biomechanics that occur with this injury. Toward this goal, treatments generally involve one of two strategies; capsulodesis or ligament reconstruction. While some authors have attempted to establish treatment guidelines based on the severity and chronicity of the injury [12, 13], there is considerable variation in treatment strategy utilized among hand surgeons [27].
Despite interest in optimizing treatment of chronic scapholunate tears, studies addressing the relative effectiveness of different surgical options have been largely limited to small case series. To our knowledge, there is no systematic review to directly compare the outcomes of ligament reconstruction and capsulodesis in patients with chronic scapholunate tears. In attempt to address this knowledge gap, we performed a systematic review comparing patient outcomes between capsulodesis and ligament reconstruction for chronic tears of the scapholunate ligament. Our hypothesis was that there would be no difference in outcomes between capsulodesis and ligament reconstruction.
Methods
We performed a systematic review of literature available through the following electronic databases: PubMed (1946 to February 2015), Embase (1947 to February 2015), SCOPUS (1966 to February 2015), CINAHL (1937 to February 2015), the Cochrane Database (including Systematic Reviews, Cochrane Database of Abstracts of Review Effects [DARE], Cochrane Central Register of Controlled Trials [CENTRAL]), clinicaltrials.gov, Proquest Dissertations and Theses, and FirstSearch Proceedings. The search strategy was created by a medical librarian and consisted of keywords associated with scapholunate ligament tear, instability or dissociation, and terms related to the surgical treatments of interest. Searches were limited to English language and human studies using database-supplied limits. The search strategy was expanded by the medical librarian into appropriate medical subject heading terms (MESH): ((((((“Ligaments, Articular” [Mesh] OR Ligament OR Ligaments) AND (Scapholunate)) OR (“Scapholunate Ligament” OR “SL Ligament” OR “SLIL” OR “scapholunate dissociation” OR “scapholunate instability”))))) AND ((“Reconstructive Surgical Procedures” [Mesh] OR “Tenodesis” [Mesh] OR “reconstructive surgical procedure” OR repair OR Capsulodesis OR tenodesis OR fixation OR “autograft” [tiab] OR “brunelli” [tiab]))) NOT ((“Animals”[Mesh]) NOT (“Animals”[Mesh] AND “Humans”[Mesh])).
After removal of duplicate entries, 511 unique citations were obtained and exported to EndNote (Thomson Reuters, New York, NY). Review of the 511 manuscripts was performed by 3 investigators (JGS, TA, JW), using a data extraction form designed prior to study inception. Disagreement was resolved by discussion facilitated by the senior author. The study was performed in accordance with The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Studies that passed initial screening required (1) patients with scapholunate ligament tears >4 weeks after the initial injury, and (2) surgical fixation by either capsulodesis or ligament reconstruction. We excluded studies that (1) included patients with more severe injury patterns (carpal dislocations); (2) included patients with associated wrist injuries; and (3) did not provide a means to assess central tendency as we were unable to obtain unpublished datasets from previous investigators. Included studies were categorized as either capsulodesis or reconstruction. Variables extracted from studies included age, gender, hand dominance, tear subtype, duration of symptoms prior to surgery, length of clinical follow up, preoperative wrist range of motion (wrist flexion, extension, radial deviation, ulnar deviation), postoperative wrist range of motion, preoperative radiographic measurements (scapholunate angle, scapholunate gap [mm]), postoperative radiographic measurements, surgical technique (capsulodesis or ligament reconstruction), and patient-reported outcome measures. We calculated the pooled means and standard deviations, according to surgical technique, for primary endpoints of postoperative wrist range of motion and radiographic measurements at final follow-up.
Results
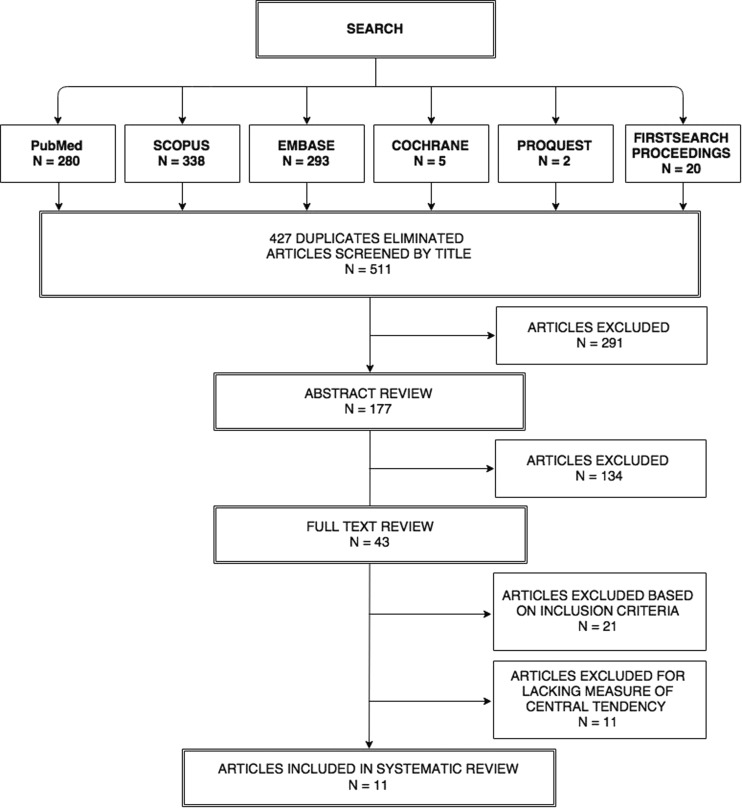
All 511 articles were screened by title to identify irrelevant articles generated from the search strategy. After title screening, 177 potentially relevant articles underwent an abstract review, which identified 43 articles for full text review. The full text review found 22 articles that met the inclusion criteria. Eleven articles were subsequently excluded due to insufficient documentation of central tendency estimation, leaving 11 available for data extraction (Fig. 1). Of the remaining studies, one lacked sufficient postoperative data to be included in the wrist flexion assessment. For similar reasons, one study was excluded from wrist extension assessment, four from scapholunate angle assessment, and four from scapholunate gap assessment.
Fig. 1.
Flowchart showing literature search and screening strategy for articles included in systematic review.
Of the 12 studies included in the systematic review, 6 evaluated capsulodesis only, 4 evaluated ligament reconstruction only, and 2 (Moran 2006, Rohman 2014) considered patients treated by both surgical techniques. Three studies in the ligament reconstruction group were designed as retrospective case-controls; all others were retrospective case series. Five studies investigated patients with static scapholunate instability only, two investigated dynamic instability, and the remaining studies included patients with both dynamic and static instability subtypes. The total number of wrists treated by capsulodesis was 174 (165 at final follow up) compared to 144 (143 at final follow up) that received ligament reconstruction. The duration of follow up ranged from 5 to 86 and 5 to 46 months for capsulodesis and ligament reconstruction, respectively. The pooled average age (SD) of the capsulodesis group was 38.6 (10.5) compared to 35.7 (7.5) in the ligament reconstruction group. Time to surgery with capsulodesis was on average 15.6 (12.8) months, versus 7.4 (8.0) months with ligament reconstruction (Tables 1 and 2).
Table 1.
Summary of studies included in systematic review, grouped by surgical technique
| Articles | n | Percent static/dynamic | Age (SD) | Average F/U months (SD) | Average months to treatment (SD) | |
|---|---|---|---|---|---|---|
| Ligament reconstruction | Garcia Elias [12] 3LT |
38 | 100/0 | 36 (12) | 46 (30.2) | Not reported |
| Links [2] Modified Brunelli |
21 | 100/0 | 30 (6.25) | 29 (4) | 12 (6) | |
| Links [2] 4BTW |
23 | 100/0 | 29 (4) | 29 (6) | 11 (6) | |
| Moran [14] Brunelli tenodesis |
15 | 40/60 | 39 | 36 (15) | 20 (5) | |
| Pauchard [17] 3LT |
19 | 58/42 | 43 (8.5) | 25 (9) | 13 (19.25) | |
| Rohman [9] Unspecified tenodesis |
27 | 60/40 | 38 | 5 | Not reported | |
| Capsulodesis | Gajendran [11] DILC |
15 | 100/0 | 42 (11) | 86 (11) | Not reported |
| Papdogeorgou [15] Dorsal capsulodesis |
32 | 100/0 | 39 (10.7) | 50 (10) | 31 (18) | |
| Wintman [24] Blatt’s dorsal capsulodesis |
18 | 0/100 | 28 (10) | 31 (18) | 17 (14) | |
| Moran [20] Blatt/Mayo’s dorsal capsulodesis |
31 | 42/58 | 38 (15) | 54 (18) | 20 (20) | |
| Moran [14] Berger-type dorsal capsulodesis |
14 | 43/57 | 41 | 38 (12.5) | 20 (6.5) | |
| Schweizer [1] Augmentation ligamentoplasty |
22 | 32/68 | 46 (10) | 63 (31) | 5 (4) | |
| Pomerance [18] Dorsal capsulodesis |
17 | 0/100 | 36 (9) | 66 (25) | 22 (5) | |
| Rohman [9] Blatt/Mayo/DILC |
16 | 60/40 | 38 | 5 | Not reported |
3LT three ligament tenodesis, 4BTW 4 bone tendon weave, DILC dorsal intercalated ligament capsulodesis
Table 2.
Summary statistics of capsulodesis and ligament reconstruction groups
| Capsulodesis group | Ligament reconstruction group | |
|---|---|---|
| Study summary | ||
| Total patients N | 174 165 at final follow up |
144 143 at final follow up |
| Duration of follow up | 49 (range 5–86) months | 28 (range 5–46) months |
| Age (SD) | 38.6 (10.5) years | 35.7 (7.5) SD |
| Time to surgery (SD) | 15.6 (12.8) months | 7.4 (8.0) months |
| Range of motion | ||
| Wrist flexion (SD) | 45.7 (14.8) degrees | 40.9 (15.3) degrees |
| Wrist extension (SD) | 56.0 (13.5) degrees | 47.3 (12.9) degrees |
| Radiographic outcomes | ||
| Postoperative SL gap (SD) | 3.44 (1.35) mm | 2.72 (1.53) mm |
| Postoperative SL angle (SD) | 60.3 (12.1) degrees | 56.5 (13.47) degrees |
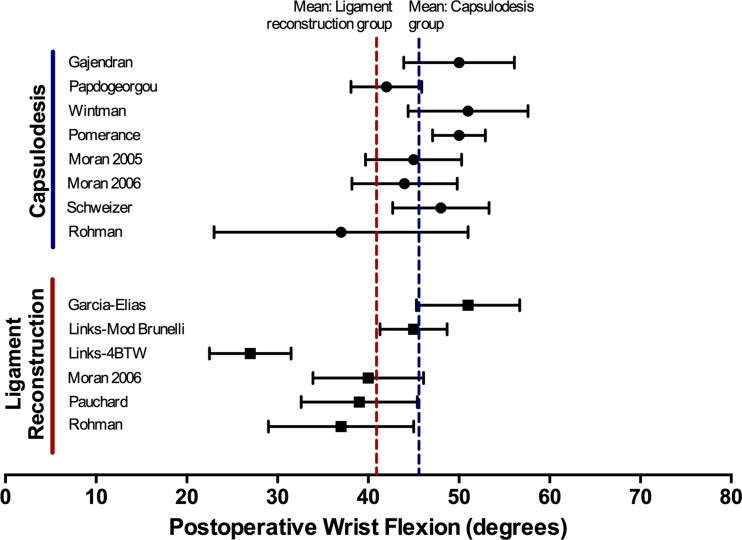
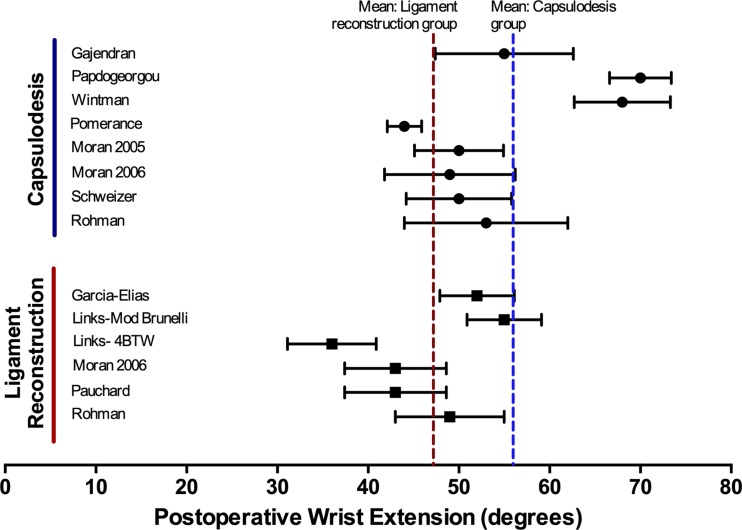
Analysis of wrist flexion after ligament reconstruction and after capsulodesis revealed weighted averages of 40.9° (95% CI 38.4–43.4) and 45.6° (95% CI 43.4–47.8), respectively (Fig. 2). Similarly, average wrist extension was 47.3° (95% CI 45.2–49.4) after ligament reconstruction and 56.0° (95% CI 54.0–58.0) after capsulodesis (Fig. 3).
Fig. 2.
Average postoperative wrist flexion for all studies reporting range of motion data, categorized by surgical technique. Dotted lines represent weighted average for capsulodesis (blue) and ligament reconstruction (red).
Fig. 3.
Average postoperative wrist extension for all studies reporting range of motion data, categorized by surgical technique. Dotted lines represent weighted average for capsulodesis (blue) and ligament reconstruction (red).
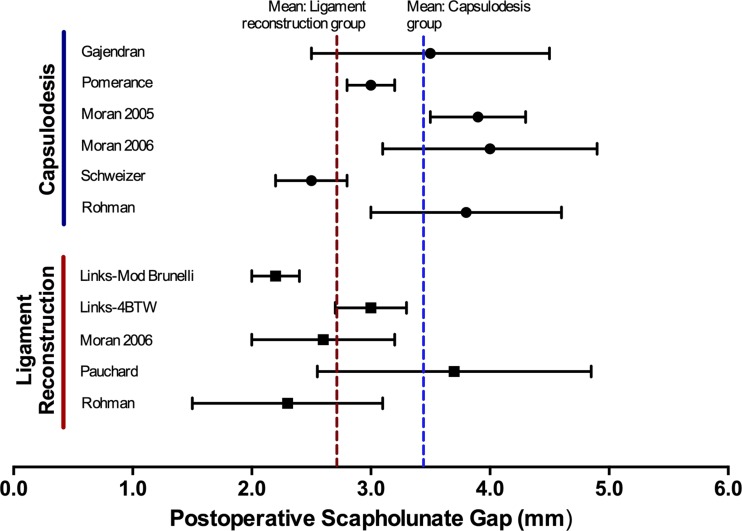
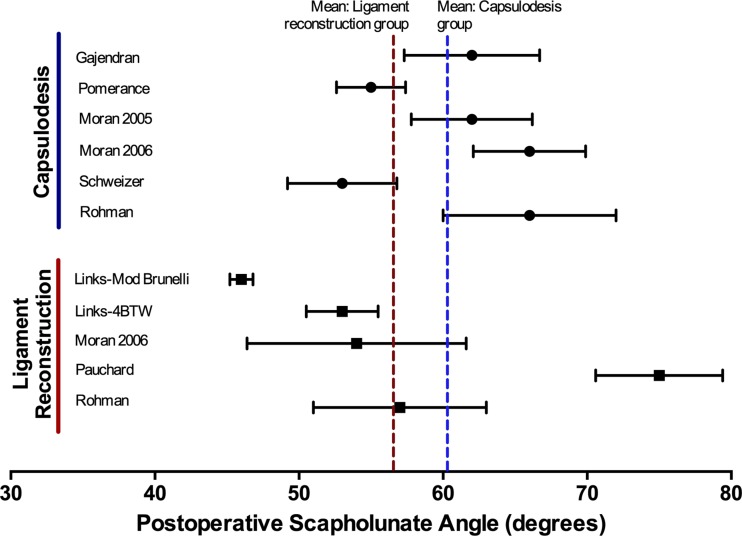
Radiologic measurements were available for five of the ligament reconstruction articles and six of the capsulodesis articles. The weighted averages of postoperative scapholunate (SL) gaps were 2.72 mm (95% CI 2.45–2.97) in the ligament reconstruction group and 3.44 mm (95% CI 3.24–3.64) in the capsulodesis group (Fig. 4). Weighted means of SL angle at follow-up after ligament reconstruction and after capsulodesis were 56.5° (95% CI 54.4–58.6) and 60.3° (95% CI 58.5–62.1), respectively (Fig. 5).
Fig. 4.
Average postoperative scapholunate gap for all studies reporting radiographic data, categorized by surgical technique. Dotted lines represent weighted average for capsulodesis (blue) and ligament reconstruction (red).
Fig. 5.
Average postoperative scapholunate angle for all studies reporting radiographic data, categorized by surgical technique. Dotted lines represent weighted average for capsulodesis (blue) and ligament reconstruction (red).
Articles reporting pre- and postoperative values showed a tendency toward improved SL gap and SL angle after ligament reconstruction, but not after capsulodesis.
Discussion
We performed this systematic review to determine if there is evidence of a functional difference when chronic scapholunate ligament tears are treated with ligament reconstruction or dorsal capsulodesis. The substantial inter-study variation found in our review lends credence to the long-standing controversy surrounding treatment of chronic SL injury. Although initial report favored Blatt’s dorsal capsulodesis for treatment of SL instability [3], subsequent studies have revealed mixed results, with many authors noting progressive deterioration of carpal alignment at later follow-up [7, 14, 24]. Other capsulodesis techniques have demonstrated similar limitations [16]. These unsatisfactory long-term outcomes have been attributed to poor recreation of palmar ligamentous stability [20] and failure to prevent recurrent scaphoid flexion and pronation leading to abnormal loading patterns [19]. Reconstructive techniques were subsequently proposed to more closely recreate the anatomical relationship of the SL ligament; however, use of tendon grafts has been criticized as more technically challenging with unreliable functional improvement [27]. Despite these criticisms, both types of procedures are still commonly performed [27]. Previous authors have cited individual studies reporting opposing results in efforts to illustrate the lack of gold standard [16]. Although restricted by the same inter-study variations in this review, we attempted to depict trends of postoperative outcomes aggregated from all available studies to date.
This study has several limitations. First, all available studies to us were either level 3 or 4 evidence. Of these, only two retrospective studies (Moran et al. 2006 and Rohman et al. 2014) directly compared capsulodesis and reconstruction. There were no prospective or randomized trials in which outcomes following capsulodesis or ligament reconstruction could be analyzed. Lack of consensus outcome measures further limited our ability to consolidate data for statistical comparison. Variables including grip strength, pain scale, and patient satisfaction scores (e.g., DASH, VAS, PRWE) were thus unable to be assessed. Secondly, inter-study variations within surgical techniques and patient characteristics may contribute to the heterogeneous outcomes presented. For the purposes of this systematic review, different reconstruction and capsulodesis techniques were broadly classified into two cohorts, which may confound the averaged outcomes of both groups. In addition, multivariate analysis would have been helpful to assess the effect of other patient risk factors on range of motion and radiographic outcomes. Age of patient and duration of symptoms have been previously implicated as a possible risk factor that predicts clinical outcome [12, 22]. Poorer outcomes have also been associated with surgical treatments of static deformities when compared to similar treatments of dynamic carpal instability [11, 25]. Certain techniques including Blatt’s capsulodesis has been theorized to fare worse compared to their reconstructive counterparts for the correction of static deformities [25, 28]. The varying proportion of patients with complete tears among included studies may help explain the heterogeneous results we observed; however, we were unable to statistically evaluate this bias with available data.
Our results demonstrate a tendency toward decreased wrist function after both capsulodesis and reconstruction. Although differences did not reach statistical significance, visual inspection of the data suggests that range of motion may be better preserved with capsulodesis group, and correction of SL gap may be better with ligament reconstruction. Among the studies excluded during our search strategy, many reveal similar outcomes, although none in this group directly compare both treatments. Chabas et al. reported an averaged extension/flexion of 50°/41° and SL gap of 2.4 mm after performing modified Brunelli tenodesis on 19 patients with chronic SL instability [6]. A similar study on 22 capsulodesis procedures by Szabo et al. demonstrated an improved mean extension/flexion of 53°/59°, but worse SL gap of 2.7 mm at final follow-up [21]. While our results remain consistent with the majority of case reports excluded by our search criteria, other studies demonstrate some differences in outcomes to those described here. In a review of eight patients with chronic SL instability, notably including those with combined distal radius fractures, Nienstedt found marginally worse wrist movement and similar radiographic trends after reconstruction compared to those reported in the present study [10]. The mean extension/flexion was 63°/37° and SL angle/gap was 63°/2.8 mm at final follow-up. Deshmukh et al. reported mean wrist extension/flexion of 38°/40° after performing 44 capsulodesis procedures for chronic SL instability, but was limited by a disproportionate number of worker compensation claims and prolonged injury-to-treatment time averaging 52 months [8]. Similar results were reported by Yang et al. after review of 12 wrists with chronic stable SL instability undergoing capsulodesis [26]. The latter study additionally noted almost immediate radiographic deterioration of the SL gap within 1 month, which is consistent with the poorer radiographic findings for capsulodesis in our present review.
This systematic review failed to demonstrate any significant difference in wrist range of motion and radiographic outcomes following capsulodesis or reconstruction for treatment of chronic scapholunate instability. However, the heterogeneous data presented in this study illustrates the knowledge gap in regards to ideal management of chronic scapholunate instabilities. An ideal surgical outcome should achieve a pain-free wrist with preserved wrist range of motion and grip strength while maintaining correct radiographic alignment of the carpal bones. None of the prevailing treatment options have shown unequivocal success; thus, adoption of standardized parameters for reporting outcomes would allow for better assessment of relative effectiveness of intervention. Future prospective studies of patients presenting with chronic SL tears, assessed by a set of consistent, pre- and postoperative measures, would allow for more direct comparison of the surgical techniques.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Pengcheng Wang, MD, Jeffrey G. Stepan, MD, and Tonya An, MD, MA have declared that they have no conflict of interest. Daniel A. Osei, MD reports grants from NIH/NCATS KL2 TR000450 and grants from BJHF/ICTS Pilot Award, outside the work.
Human/Animal Rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
N/A.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Work performed at Washington University in St Louis School of Medicine.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9525-5) contains supplementary material, which is available to authorized users.
References
- 1.Andreas S, Regula S. Long-term results after repair and augmentation ligamentoplasty of rotatory subluxation of the scaphoid. J Hand Surg. 2002;27:674–684. doi: 10.1053/jhsu.2002.34320. [DOI] [PubMed] [Google Scholar]
- 2.Annie CL, Simon HC, Thanapong W, Thomas ET. Scapholunate interosseous ligament reconstruction: results with a modified Brunelli technique versus four-bone weave. J Hand Surg. 2008;33:850–856. doi: 10.1016/j.jhsa.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 3.Blatt G. Capsulodesis in reconstructive hand surgery. Dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3:81–102. [PubMed] [Google Scholar]
- 4.Blevens AD, Light TR, Jablonsky WS, et al. Radiocarpal articular contact characteristics with scaphoid instability. J Hand Surg. 1989;14:781–790. doi: 10.1016/S0363-5023(89)80076-0. [DOI] [PubMed] [Google Scholar]
- 5.Burgess RC. The effect of rotatory subluxation of the scaphoid on radio-scaphoid contact. J Hand Surg. 1987;12:771–774. doi: 10.1016/S0363-5023(87)80066-7. [DOI] [PubMed] [Google Scholar]
- 6.Chabas J-F, Gay A, Valenti D, Guinard D, Legre R. Results of the modified Brunelli tenodesis for treatment of scapholunate instability: a retrospective study of 19 patients. J Hand Surg. 2008;33:1469–1477. doi: 10.1016/j.jhsa.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 7.De Carli P, Donndorff AG, Gallucci GL, Boretto JG, Alfie VAA. Chronic scapholunate dissociation: ligament reconstruction combining a new extensor carpi radialis longus tenodesis and a dorsal intercarpal ligament capsulodesis. Tech Hand Up Extrem Surg. 2011;15:6–11. doi: 10.1097/BTH.0b013e3181e6650c. [DOI] [PubMed] [Google Scholar]
- 8.Deshmukh SC, Givissis P, Belloso D. Blatt’s capsulodesis for chronic scapholunate dissociation. J Hand Surg. 1999;24:215–220. doi: 10.1054/jhsb.1998.0183. [DOI] [PubMed] [Google Scholar]
- 9.Eric MR, Julie A, Matthew DP, Julie EA. Scapholunate interosseous ligament injuries: a retrospective review of treatment and outcomes in 82 wrists. J Hand Surg. 2014;39:2020–2026. doi: 10.1016/j.jhsa.2014.06.139. [DOI] [PubMed] [Google Scholar]
- 10.Frank N. Treatment of static scapholunate instability with modified Brunelli Tenodesis: results over 10 years. J Hand Surg. 2013;38:887–892. doi: 10.1016/j.jhsa.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 11.Gajendran VK, Peterson B, Slater RR, Jr, Szabo RM. Long-term outcomes of dorsal intercarpal ligament capsulodesis for chronic scapholunate dissociation. J Hand Surg. 2007;32:1323–1333. doi: 10.1016/j.jhsa.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg. 2006;31:125–134. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Kuo CE, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg. 2008;33:998–1013. doi: 10.1016/j.jhsa.2008.04.027. [DOI] [PubMed] [Google Scholar]
- 14.Moran SL, Ford KS, Wulf CA, Cooney WP. Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg. 2006;31:1438–1446. doi: 10.1016/j.jhsa.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Papadogeorgou E, Mathoulin C. Extensor carpi radialis brevis ligamentoplasty and dorsal capsulodesis for the treatment of chronic post-traumatic scapholunate instability. Chir Main. 2010;29:172–179. doi: 10.1016/j.main.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 16.Pappou IP, Basel J, Deal DN. Scapholunate ligament injuries: a review of current concepts. Hand. 2013;8:146–156. doi: 10.1007/s11552-013-9499-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pauchard N, Dederichs A, Segret J, Barbary S, Dap F, Dautel G. The role of three-ligament tenodesis in the treatment of chronic scapholunate instability. J Hand Surg. 2013;38:758–766. doi: 10.1177/1753193413475753. [DOI] [PubMed] [Google Scholar]
- 18.Pomerance J. Outcome after repair of the scapholunate interosseous ligament and dorsal capsulodesis for dynamic scapholunate instability due to trauma. J Hand Surg. 2006;31:1380–1386. doi: 10.1016/j.jhsa.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Steve KL, Dan AZ, Anthony S, Raj K, Jeffrey Y. Biomechanical comparison of 3 methods of scapholunate ligament reconstruction. J Hand Surg. 2014;39:643–650. doi: 10.1016/j.jhsa.2013.12.033. [DOI] [PubMed] [Google Scholar]
- 20.Steven LM, William PC, Richard AB, Justin S. Capsulodesis for the treatment of chronic scapholunate instability. J Hand Surg. 2005;30:16–23. doi: 10.1016/j.jhsa.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 21.Szabo RM, Slater RR, Palumbo CF, Gerlach T. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: clinical results. J Hand Surg. 2002;27:978–984. doi: 10.1053/jhsu.2002.36523. [DOI] [PubMed] [Google Scholar]
- 22.Taleisnik J. Current concepts review. Carpal instability. J Bone Joint Surg. 1988;70:1262–1268. doi: 10.2106/00004623-198870080-00025. [DOI] [PubMed] [Google Scholar]
- 23.Watson HK, Brenner LH. Degenerative disorders of the wrist. J Hand Surg. 1985;10:1002–1006. doi: 10.1016/S0363-5023(85)80025-3. [DOI] [PubMed] [Google Scholar]
- 24.Wintman BI, Gelberman RH, Katz JN. Dynamic scapholunate instability: results of operative treatment with dorsal capsulodesis. J Hand Surg. 1995;20:971–979. doi: 10.1016/S0363-5023(05)80145-5. [DOI] [PubMed] [Google Scholar]
- 25.Wyrick JD, Youse BD, Kiefhaber TR. Scapholunate ligament repair and capsulodesis for the treatment of static scapholunate dissociation. J Hand Surg. 1998;23:776–780. doi: 10.1016/S0266-7681(98)80095-8. [DOI] [PubMed] [Google Scholar]
- 26.Yong Y, Kannan K, Tsu-Min T. Radiographic evaluation of chronic static scapholunate dissociation post soft tissue reconstruction. J Wrist Surg. 2013;02:155–159. doi: 10.1055/s-0033-1343079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zarkadas PC, Gropper PT, White NJ, Perey BH. A survey of the surgical management of acute and chronic scapholunate instability. J Hand Surg. 2004;29:848–857. doi: 10.1016/j.jhsa.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 28.Zyluk A, Piotuch B. The management of scapholunate wrist instability: a review. Pol Orthop Traumatol. 2012;77:83–89. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)