Abstract
Background
Anterior cruciate ligament (ACL) injuries are among the most common knee injuries. Patient outcomes, rate of subsequent operations, and rate of subsequent ACL reconstruction following primary ACL reconstruction need to be evaluated.
Questions/Purposes
This study was designed to answer the following questions: (1) What is the return to surgery (OR) rate following primary ACL reconstruction and (2) what is the revision ACL reconstruction rate?
Methods
Data was drawn from the Hospital for Special Surgery (HSS) ACL Registry. International Knee Documentation Committee (IKDC) Subjective Knee Evaluation, Lysholm-Tegner Scales, Marx Activity Scale, and SF12 were completed by patients at baseline, 1-, and 2-year follow-up. Clinical data and intraoperative data were registered by surgeons on an intraoperative form. Subsequent surgery rates were determined by evaluating the medical records for subsequent surgery, laterality, surgeon, procedure description, and type of anesthesia.
Results
The majority of the ACL reconstructions performed were autograft (76.6%) with the most common graft being bone-patellar tendon-bone (BTB) autograft (47.2%), hamstring autograft (21.9%), and Achilles allograft (18.2%). Average IKDC score improved from 51.9 (SD 16.1) at baseline to 83.5 (SD 14.2) at 2-year follow-up. Females had a 2.5-point lower IKDC and 1.4-point Marx scores compared to males. Of the enrolled patients, 7.3% had revision ACL surgery with 70.4% being ipsilateral ACL surgery. Of the enrolled patients, 10.3% had subsequent knee surgery with 72.3% being ipsilateral knee surgery. Multivariable logistic regression analysis showed that patients less than 18 years of age at the time of their index surgery were over three times more likely to undergo a revision ACL reconstruction compared to older patients and were at four times higher risk than older patients for any subsequent knee surgery.
Conclusion
Understanding ACL surgery, patient outcomes, and risk factors for revision ACL surgery and subsequent knee surgery after primary ACL reconstruction is essential. Patients less than 18 years of age have a higher risk of subsequent knee surgery and subsequent ACL surgery than older patients.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9532-6) contains supplementary material, which is available to authorized users.
Keywords: ACL, ACL Registry, anterior cruciate ligament
Introduction
Anterior cruciate ligament (ACL) injury is one of the most frequently treated knee conditions and is prevalent in sports that require pivoting and cutting motions [4]. A 2008 study estimated that 175,000 ACL reconstructions were performed per year in the USA, and the rate of ACL reconstruction increased 21.5% in New York State between 1997 and 2006 [18, 22]. This increase in ACL reconstruction may reflect a change in practice with a trend toward operative management of ACL injury [8]. With more patients undergoing surgery for ACL injury, it is increasingly important to evaluate the risk of subsequent surgery associated with ACL reconstruction. Previous studies have largely examined the success of technical aspects of the procedure, post-operative treatment, management of complications, and patient satisfaction; however, the frequency of subsequent surgery after primary ACL reconstruction over the short and long term has only recently been explored [5, 7, 11, 14, 19].
In the current literature, reoperation rates, both subsequent surgeries, and ACL revisions have varied. In a study of 980 patients undergoing ACL reconstruction, Hettrich et al. reported 6-year subsequent surgery rates of 18.9% in patients requiring a subsequent operation on the ipsilateral leg and 10.2% in patients requiring a subsequent procedure on the contralateral leg [11]. The rate of graft rupture was similar to the rate of contralateral ACL tear (7.7 vs. 6.4%). In another study of the Kaiser Permanente ACL Registry, Csintalan et al. reported a non-revision 3.9% reoperation rate on the same knee within a mean follow-up of 1.9 ± 1.5 years [7]. In 70,547 ACL reconstructions in New York State, 6.5% of patients in the study cohort returned for at least one subsequent surgery on either knee within a year of primary ACL reconstruction [18].
Given the negative effects of subsequent surgery after ACL reconstruction on healthcare costs and patient satisfaction, the Hospital for Special Surgery (HSS) ACL Registry seeks to examine the outcomes of patients who have undergone ACL reconstruction at this institution. This is modeled after other ACL registries such as the Danish Knee Ligament Reconstruction Registry, which has tracked 85% of the ACL reconstructions done in that country since 2005 and reports a 4.1% ACL reconstruction revision within 5 years of primary reconstruction with the highest risk being within 2 years of primary reconstruction [17].
The ACL Registry is essential for determining patient outcomes, patient satisfaction, and rates of subsequent operations and subsequent ACL reconstructions at our institution. This study aims to determine the revision rate for ACL reconstruction, the return to OR rate following ACL reconstruction, and the reasons for return to the OR at HSS. We hypothesize that our institution has a low return to OR rate following primary ACL reconstruction and a low revision ACL reconstruction rate.
Patients and Methods
Participants and Data Extraction
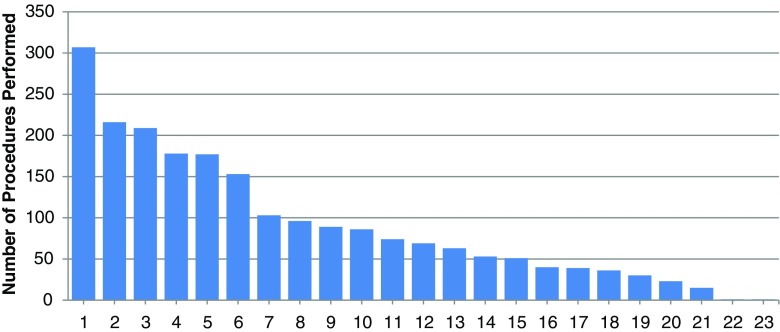
Data for this study was drawn from the Hospital for Special Surgery (HSS) ACL Registry, which enrolled 2109 patients between June 1, 2009, and September 6, 2013. There were a total of 2993 ACL reconstructions performed at the hospital during this time for an enrollment percentage of 70.4%. Twenty-three surgeons were included in the registry data (Fig. 1). The study team obtained Institutional Review Board approval to invite all patients scheduled for ACL Reconstruction with a HSS Sports Service surgeon to preoperatively enroll in the registry. We included all patients diagnosed with an ACL tear and were scheduled for ACL Reconstruction at HSS, with or without concomitant procedures. Written consent was obtained from all patients.
Fig. 1.
Surgeon ACL volume.
Each consenting patient completed a preoperative baseline questionnaire consisting of the following validated patient outcome surveys: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation, Lysholm-Tegner Scales, Marx Activity Scale, and SF12. Patients completed this same combination of outcome surveys at the baseline, 1-year, and 2-year follow-up time points. Clinical data was contributed by surgeons in an intra-operative form based upon patient examination under anesthesia. After determining which registry participants had a definite index surgery date, complete baseline surveys, and intra-operative data, the researchers requested medical record data in order to determine if the patients returned to HSS for surgery after their ACL reconstruction. If patients did return for subsequent surgery at HSS, the researchers extracted the following surgical information from the medical records: date of subsequent surgery, laterality, case number, surgeon, procedure description, and type of anesthesia. Data was not collected if the patient did not return to HSS for evaluation.
Two thousand one hundred nine patients were enrolled into the ACL Registry and achieved a 2-year follow-up (Table 1). Average age of patients at the time of enrollment was 29.6 ± 12.0 years with the highest proportion of patients aged between 26 and 39 years (31.6%). The registry consisted primarily of males who made up 57.4% of the population. The mean body mass index (BMI) of the registry was 24.8 ± 3.9, and patients with normal BMI levels (BMI <25) made up 58% of the population. Over three quarters (75.4%) of the population were involved in a high-risk sport, as defined previously in the literature, at the time of their injury, and 81.7% of the injuries were non-contact injuries [3]. Recreational sports made up 71.2% of the level of activity in the registry population and professional sports, 1.5%.
Table 1.
Demographic data for patients enrolled in the ACL Registry for primary ACL reconstruction (total N = 2109)
| Total N | Mean or N | SD or % | |
|---|---|---|---|
| Age at enrolled (years) | 2109 | 29.6 | 12.0 |
| <18 | 2109 | 407 | 19.3% |
| 18–25 | 2109 | 524 | 24.8% |
| 26–39 | 2109 | 667 | 31.6% |
| ≥40 | 2109 | 511 | 24.2% |
| Female sex | 2109 | 898 | 42.6% |
| BMI at baseline | 1947 | 24.8 | 3.9 |
| <25 | 1947 | 1129 | 58.0% |
| 25–29 | 1947 | 654 | 33.6% |
| ≥30 | 1947 | 164 | 8.4% |
| What sport were you playing when you injured your knee? | |||
| Low risk | 1607 | 395 | 24.6% |
| High riska | 1607 | 1212 | 75.4% |
| Mechanism of injury | |||
| Contact | 1665 | 305 | 18.3% |
| Non-contact | 1665 | 1360 | 81.7% |
| Level of activity | |||
| Recreational | 1647 | 1172 | 71.2% |
| High school | 1647 | 310 | 18.8% |
| College | 1647 | 141 | 8.6% |
| Professional | 1647 | 24 | 1.5% |
aHigh-risk sport: basketball, soccer, football, lacrosse, skiing, or volleyball
The majority of the ACL reconstructions were performed using autograft at 76.6%. Overall, the most common graft used was bone-patellar tendon-bone (BTB) at 47.2%, followed by both hamstring tendons (semitendinosus and gracilis) at 21.9% and Achilles allograft at 18.2%. The most common autograft type was BTB at 61.5% followed by hamstring at 38.3%. The most common allograft type was Achilles at 80.9% (Table 2). Allograft patients were typically older than autograft patients (40.3 vs. 26.2 years) (Table 2).
Table 2.
Graft-type data for primary ACL reconstruction in patients enrolled in the ACL Registry (total N = 2109)
| Total | N | % | Mean age | SD | Min | Max | |
|---|---|---|---|---|---|---|---|
| Autograft | 1753 | 1343 | 76.6 | 26.2 | 10.5 | 12.0 | 69.0 |
| Autograft BTB | 1343 | 826 | 61.5 | 23.7 | 8.5 | 13.0 | 69.0 |
| Autograft hamstring | 1343 | 515 | 38.3 | 30.3 | 12.1 | 12.0 | 63.0 |
| Autograft quad bone | 1343 | 2 | 0.1 | 17.5 | 0.7 | 17.0 | 18.0 |
| Allograft | 1753 | 409 | 23.3 | 40.3 | 10.5 | 14.0 | 72.0 |
| Allograft hamstring | 397 | 29 | 7.3 | 41.1 | 11.7 | 14.0 | 69.0 |
| Allograft Achilles | 397 | 321 | 80.9 | 39.9 | 10.3 | 16.0 | 72.0 |
| Allograft tibialis anterior | 397 | 31 | 7.8 | 41.0 | 12.0 | 21.0 | 61.0 |
| Allograft tibialis posterior | 397 | 16 | 4.0 | 43.8 | 10.7 | 16.0 | 61.0 |
| Contralateral | 1753 | 1 | 0.1 | ||||
| Graft type | |||||||
| BTB | 1760 | 830 | 47.2 | ||||
| Hamstring semitendinosus | 1760 | 159 | 9.0 | ||||
| Hamstring semitendinosus + | 1760 | 386 | 21.9 | ||||
| Quadriceps bone | 1760 | 9 | 0.5 | ||||
| Achilles | 1760 | 321 | 18.2 | ||||
| Tibialis anterior | 1760 | 31 | 1.8 | ||||
| Tibialis posterior | 1760 | 16 | 0.9 | ||||
Statistics
Descriptive statistics were calculated using means and standard deviations for continuous variables and frequencies and percentages for discrete variables. Comparative differences between study groups were conducted using independent sample t tests for continuous variable and chi-square or Fisher’s exact test for discrete variables. Variables that did not meet the assumption of normality according to the Shapiro-Wilk test were evaluated using their non-parametric equivalent. All variables analyzed in the univariate analyses were considered for analysis in the development of the multivariable regression models. Stepwise, multivariable regression models were developed to identify potential risk factors for subsequent ACL surgery or any subsequent knee procedure while adjusting for any confounding from the other variables. Because of the exploratory nature of the analysis, variables that reach a p value of 0.10 or below were retained in the final model and those variables with p values of 0.05 or below were deemed statistically significant risk factors. All statistical analyses were performed using SPSS software version 22.0 (IBM Corp., Armonk, NY).
Results
The majority of patients presented with meniscal tears requiring treatment at the time of the primary ACL reconstruction (Table 3) 40.4% had no meniscal pathology. Lateral meniscal tear alone was most common at 24.2% with combined medial and lateral tears occurring 14.4% of the time. Medial meniscal tears were most commonly treated with meniscectomy (46.6%) or repair (46.4%). Lateral meniscal tears were most often treated with meniscectomy (59.7%) followed by repair (27.0%). Meniscus repair patients were typically younger than meniscectomy patients (26 vs. 38 for medical meniscus; 25 vs. 30 for lateral meniscus) (Table 3). Of the patients, 24.6% had a cartilage defect with the medial femoral condyle being the most common (48.4%) followed by the patella (37.9%) and the lateral tibial plateau (23.1%) (Table 3).
Table 3.
Presence of meniscal defect (and treatment) and cartilage defect at the time of primary ACL reconstruction (total N = 2109)
| Meniscus | Total N | N | % | Cartilage | Total N | N | % |
| Meniscal tear | Cartilage defects | ||||||
| Medial and lateral tear | 1711 | 246 | 14.4 | Any defect | 1737 | 427 | 24.6 |
| Medial tear only | 1711 | 360 | 21.0 | Medial femoral condyle | 417 | 202 | 48.4 |
| Lateral tear only | 1711 | 414 | 24.2 | Lateral femoral condyle | 419 | 59 | 14.1 |
| Trochlea | 417 | 55 | 13.2 | ||||
| Medial tibial plateau | 414 | 38 | 9.2 | ||||
| Lateral tibial plateau | 416 | 96 | 23.1 | ||||
| Lesion patella | 422 | 160 | 37.9 | ||||
| Meniscus | Total N | N | % | Mean age | SD | Min | Max |
| Medial meniscal treatment | |||||||
| No treatment | 603 | 36 | 6.0 | 28.7 | 12.6 | 13.0 | 63.0 |
| Excision | 603 | 281 | 46.6 | 38.2 | 12.2 | 14.0 | 72.0 |
| Healing response | 603 | 6 | 1.0 | 37.0 | 10.0 | 24.0 | 51.0 |
| Repair | 603 | 280 | 46.4 | 26.4 | 10.3 | 12.0 | 61.0 |
| Lateral meniscal treatment | |||||||
| No treatment | 653 | 79 | 12.1 | 31.1 | 13.9 | 13.0 | 69.0 |
| Excision | 653 | 390 | 59.7 | 29.9 | 11.8 | 12.0 | 63.0 |
| Healing response | 653 | 8 | 1.2 | 24.8 | 8.4 | 14.0 | 33.0 |
| Repair | 653 | 176 | 27.0 | 24.5 | 10.9 | 12.0 | 61.0 |
There were 650 and 648 patients who had baseline and 2-year follow-up on IKDC and Marx scores, respectively. This represented a response rate of 31% for both outcome measures. Average IKDC score improved from 51.9 ± 16.1 at baseline to 83.5 ± 14.2 at 2-year follow-up. The average Marx score, which rates the activity in the month prior to the injury, decreased from 11.5 (±4.9) to 8.9 (±5.0) (p < 0.001).
Demographic and clinical variables, which analyzed regression models, included age, sex, BMI, high- or low-risk sport type, contact or non-contact mechanism of injury, allograft or autograft graft type, and presence of any meniscal or articular cartilage injury at the time of surgery. Results of the multivariable linear regression analysis yielded the following results at 2-year follow-up after adjusting for all other variables in the model (Table 4). Patients less than 18 years of age had about seven- and five-point improvement in their IKDC and Marx scores, respectively, compared to patients who were 40 years and older (p < 0.001). Similarly, patients aged 18 to 25 also had significant improvement in their IKDC and Marx scores compared to the older population (p = 0.016 and p < 0.001, respectively). Females had about a 2.5-point lower IKDC (p = 0.047) and 1.4-point Marx (p < 0.001) scores compared to males. Increased BMI levels were correlated with reduced IKDC scores at the time of follow-up (p = 0.003). Patients with a non-contact mechanism of injury had worse Marx scores at 2 years (p = 0.005), and patients with an allograft reconstruction were more likely to have worse Marx scores at 2 years (p = 0.050). High-risk sports, meniscal tears, and cartilage injury were not indicative of any of the follow-up outcomes.
Table 4.
Multivariable regression results for factors affecting patient-reported outcomes in the ACL Registry
| IKDC at 2 years | Marx at 2 years | ||||||
|---|---|---|---|---|---|---|---|
| Variable type | Variable | Beta | SE | P value | Beta | SE | P value |
| (Constant) | 95.92 | 4.657 | <0.001 | 9.499 | 0.527 | <0.001 | |
| Demographic | Age <18 | 7.625 | 1.628 | <0.001 | 5.731 | 0.561 | <0.001 |
| Age 18–25 | 3.59 | 1.481 | 0.016 | 2.745 | 0.506 | <0.001 | |
| Age 26–39 | – | – | – | – | – | – | |
| Female (vs. male) | -2.503 | 1.255 | 0.047 | -1.441 | 0.399 | <0.001 | |
| BMI at baseline | -0.528 | 0.174 | 0.003 | – | – | – | |
| High-risk sporta | – | – | – | – | – | – | |
| Non-contact mechanism | – | – | – | -1.43 | 0.503 | 0.005 | |
| Graft type | Allograft (vs. autograft) | – | – | – | -0.922 | 0.47 | 0.050 |
| Concomitant injury | Any meniscal tear | – | – | – | – | – | – |
| Any cartilage injury | – | – | – | – | – | – | |
Age group reference: age 40+; R 2 IKDC 0.343; R 2 Marx 0.508
aHigh-risk sport: basketball, soccer, football, lacrosse, skiing, or volleyball
Of the patients enrolled in the ACL Registry, 142 patients (7.3%) had revision ACL surgery and 202 patients (10.3%) had a subsequent knee procedure that included non-ACL procedures (Table 5). Patients who had revision ACL or a subsequent knee procedure were younger than those who did not have a subsequent ACL (p < 0.001), particularly those patients who were 18 years or younger. Patients who underwent a revision ACL were primarily female (50.7%, p = 0.037); however, for those who underwent any subsequent knee procedure, there was no significant difference between males and females (p = 0.471). Additionally, BMI had no effect on reoperation. Baseline IKDC scores were not significantly different between revision ACL patients and non-revision ACL patients (p = 0.485) as well as between subsequent knee procedure patients and patients who did not undergo a subsequent procedure (p = 0.232). IKDC scores at 2-year follow-up showed that all subsequent knee procedure patients had lower scores compared to patients who did not have another procedure performed. Marx scores at baseline were higher for both revision ACL patients and those who underwent a repeat knee surgery (p < 0.001 for both). At 2-year follow-up, revision ACL patients saw no difference in Marx scores, while patients who had repeat knee surgery showed significantly higher scores (p = 0.020). The professional athlete population had comparable baseline and follow-up IKDC scores compared to the non-professional athlete population. Baseline Marx scores were higher in the professional athletes (14 vs. 12, p = 0.008), but by 2-year follow-up, there was no significant difference between groups (11 vs. 9, p = 0.386).
Table 5.
Outcome and demographic data of patients with and without subsequent ACLR and any knee procedure
| Revision ACL? | Subsequent knee procedure? | |||||
|---|---|---|---|---|---|---|
| No (N = 1816) | Yes (N = 142) | P value | No (N = 1755) | Yes (N = 202) | P value | |
| IKDC baseline | 52.0 (16.1) | 51.0 (15.2) | 0.485 | 52.0 (16.1) | 50.6 (15.6) | 0.232 |
| IKDC 1 year | 80.8 (14.4) | 77.5 (19.3) | 0.822b | 81.2 (14.1) | 76.2 (18.7) | 0.178b |
| IKDC 2 years | 84.4 (12.2) | 76.4 (19.1) | 0.015b | 84.3 (12.1) | 78.5 (19.0) | 0.122b |
| Marx baseline | 11.3 (5.0) | 13.4 (4.2) | <0.001b | 11.3 (4.9) | 13.0 (4.5) | <0.001b |
| Marx 1 year | 8.9 (5.0) | 10.5 (5.3) | 0.057b | 8.8 (4.9) | 10.9 (5.3) | 0.003b |
| Marx 2 years | 8.7 (5.0) | 9.9 (5.9) | 0.124b | 8.6 (5.0) | 10.4 (5.5) | 0.015b |
| Age at enrollment (years) | 30.1 (11.9) | 23.5 (9.9) | <0.001b | 30.2 (11.9) | 25.2 (10.7) | <0.001b |
| <18 | 312 (17.4%) | 56 (40.0%) | <0.001 | 297 (17.1%) | 71 (35.7%) | <0.001 |
| 18–25 | 443 (24.6%) | 39 (27.9%) | 0.396 | 435 (25.0%) | 47 (23.6%) | 0.663 |
| 26–39 | 594 (33.0%) | 30 (21.4%) | 0.005 | 571 (32.9%) | 53 (26.6%) | 0.092 |
| ≥40 | 449 (25.0%) | 15 (10.7%) | <0.001 | 435 (25.0%) | 28 (14.1%) | 0.001 |
| Female sex | 749 (41.7%) | 71 (50.7%) | 0.037 | 731 (42.1%) | 89 (44.7%) | 0.471 |
| BMI at baseline | 24.8 (3.9) | 24.1 (4.0) | 0.053 | 24.8 (3.9) | 24.2 (4.1) | 0.068 |
| <25 | 974 (57.6%) | 85 (64.9%) | 0.105 | 937 (57.3%) | 121 (65.4%) | 0.034 |
| 25–29 | 574 (34.0%) | 35 (26.7%) | 0.090 | 562 (34.4%) | 47 (25.4%) | 0.014 |
| ≥30 | 142 (8.4%) | 11 (8.4%) | 0.998 | 136 (8.3%) | 17 (9.2%) | 0.686 |
| Days index to subsequent surgery | 0 (0) | 406.2 (261.9) | N/A | 0.0 (0.0) | 401.5 (254.0) | N/A |
| What sport were you playing when you injured your knee? | ||||||
| Low risk | 786 (43.3%) | 52 (36.6%) | 0.122 | 762 (43.4%) | 75 (37.1%) | 0.087 |
| High riska | 1030 (56.7%) | 90 (63.4%) | 993 (56.6%) | 127 (62.9%) | ||
| Mechanism of injury | ||||||
| Contact | 254 (17.9%) | 30 (24.6%) | 0.069 | 246 (18.0%) | 38 (22.2%) | 0.179 |
| Non-contact | 1163 (82.1%) | 92 (75.4%) | 1121 (82.0%) | 133 (77.8%) | ||
aHigh-risk sport: basketball, soccer, football, lacrosse, skiing, or volleyball
b P value resulting from non-parametric Mann-Whitney U test
Meniscal pathology was not found to be associated with revision ACL procedures. However, meniscal pathology was associated with any second knee procedure, particularly patients with medical meniscal tears (p = 0.037). Lesions of the articular cartilage were found to be associated with revision ACL (p = 0.031). Cartilage lesions of the medial femoral condyle were associated with a second knee procedure (p = 0.015) (Table 6).
Table 6.
Clinical characteristics of patients with and without subsequent ACLR and any knee procedure
| Revision ACL? | Subsequent knee procedure? | |||||
|---|---|---|---|---|---|---|
| No (N = 1816) | Yes (N = 142) | P value | No (N = 1755) | Yes (N = 202) | P value | |
| Graft type | ||||||
| Autograft | 1140 (76.4%) | 103 (81.7%) | 0.173 | 1096 (76.3%) | 147 (81.7%) | 0.106 |
| Allograft | 351 (23.5%) | 23 (18.3%) | 0.178 | 340 (23.7%) | 33 (18.3%) | 0.110 |
| Contralateral | 1 (0.1%) | 0 (0.0%) | >0.999a | 1 (0.1%) | 0 (0.0%) | >0.999a |
| Autograft type | ||||||
| Autograft BTB | 702 (61.6%) | 63 (61.2%) | 0.934 | 680 (62.0%) | 85 (57.8%) | 0.323 |
| Autograft hamstring | 437 (38.3%) | 39 (37.9%) | 0.925 | 415 (37.9%) | 61 (41.5%) | 0.395 |
| Autograft quad bone | 1 (0.1%) | 1 (1.0%) | 0.318a | 1 (0.1%) | 1 (0.7%) | 0.445a |
| Allograft type | ||||||
| Allograft hamstring | 22 (6.4%) | 1 (4.5%) | >0.999a | 22 (6.6%) | 1 (3.2%) | 0.791a |
| Allograft Achilles | 283 (82.5%) | 16 (72.7%) | 0.235 | 273 (82.0%) | 25 (80.6%) | 0.826 |
| Allograft tibialis anterior | 27 (7.9%) | 3 (13.6%) | 0.536a | 27 (8.1%) | 3 (9.7%) | 0.834 |
| Allograft tibialis posterior | 10 (2.9%) | 2 (9.1%) | 0.319 | 10 (3.0%) | 2 (6.5%) | 0.546 |
| Meniscal tear | ||||||
| Any meniscal tear | 902 (60.9%) | 73 (57.5%) | 0.448 | 854 (59.9%) | 120 (66.3%) | 0.096 |
| Medial meniscal tear | 541 (36.5%) | 40 (31.5%) | 0.259 | 502 (35.2%) | 78 (43.1%) | 0.037 |
| Lateral meniscal tear | 582 (39.5%) | 44 (34.9%) | 0.311 | 559 (39.3%) | 66 (37.3%) | 0.598 |
| Medial meniscal treatment | ||||||
| None/healing response | 17 (8.1%) | 1 (8.3%) | >0.999a | 37 (7.6%) | 4 (5.3%) | 0.674a |
| Meniscectomy | 90 (42.7%) | 4 (33.3%) | 0.749 | 236 (48.5%) | 23 (30.7%) | 0.004 |
| Meniscus repair | 104 (49.3%) | 7 (58.3%) | 0.542 | 214 (43.9%) | 48 (64.0%) | 0.001 |
| Lateral meniscal treatment | ||||||
| None/healing response | 76 (13.2%) | 9 (20.9%) | 0.155 | 75 (13.6%) | 10 (15.4%) | 0.687 |
| Meniscectomy | 351 (60.9%) | 21 (48.8%) | 0.118 | 340 (61.5%) | 31 (47.7%) | 0.032 |
| Meniscus repair | 149 (25.9%) | 13 (30.2%) | 0.530 | 138 (25.0%) | 24 (36.9%) | 0.038 |
| Cartilage defects | ||||||
| Any defect | 386 (26.2%) | 22 (17.5%) | 0.031 | 370 (26.1%) | 37 (20.6%) | 0.110 |
| Medial femoral condyle | 179 (47.4%) | 15 (68.2%) | 0.057 | 169 (46.7%) | 25 (67.6%) | 0.015 |
| Lateral femoral condyle | 53 (13.7%) | 4 (18.2%) | 0.528 | 51 (13.7%) | 6 (16%) | 0.679 |
| Trochlea | 50 (13.2%) | 2 (9.5%) | >0.999 | 49 (13.5%) | 3 (8.3%) | 0.602 |
| Medial tibial plateau | 34 (9.0%) | 4 (19.0%) | 0.129 | 33 (9.1%) | 5 (13.9%) | 0.356 |
| Lateral tibial plateau | 90 (23.7%) | 4 (20.0%) | >0.999 | 86 (23.6%) | 8 (22.9%) | 0.918 |
| Lesion patella | 147 (38.2%) | 4 (20.0%) | >0.999 | 140 (37.9%) | 10 (28.6%) | 0.273 |
a P value resulting from Fisher’s exact test
One hundred forty-two patients required revision ACL reconstruction (ACLR) and subsequent knee procedures (Table 7). Timing to subsequent procedures is included in Table 7. Of the 142 revision ACL patients, 100 (70.4%) were ipsilateral procedures. There were 21 patients who needed a third revision ACL procedure, which represented 1% of the entire cohort and 14.8% of the revision ACL population. Similarly, of the 202 patients who required a subsequent knee procedure, 72.3% were performed on the ipsilateral side. Of those patients, 27 required a third surgery which represented 1% of the entire population and 13.4% of the second knee procedure population. Of the patients who had a revision ACL reconstruction, 56.3% had an isolated ACL reoperation, while 14.1% had an ACL revision with concomitant meniscal procedure, and 26.6% had an operation that treated the ACL, meniscus, and articular cartilage. For any subsequent knee procedure, isolated meniscal procedures made up 25.7% of the procedures with procedures addressing the articular cartilage were only 3% of the cases. Of the patients who had an ipsilateral revision ACLR, 51.0% had an isolated ACL operation, while 40.0% had an operation that treated the ACL, cartilage, and meniscus. Of those who had a contralateral revision ACLR, 69.0% were an ACL reconstruction only. Subsequent surgery on the ipsilateral knee was most commonly an ACL procedure at 34.9% followed by ACL, meniscus, and cartilage procedures at 27.4%. Subsequent surgery on the contralateral knee was most commonly ACL surgery at 51.8% followed by meniscus only surgery at 23.2% (Table 8).
Table 7.
Properties of subsequent knee procedures
| Revision ACL? | Subsequent knee procedure? | |||
|---|---|---|---|---|
| Second surgery (N = 142) | Third surgery (N = 21) | Second surgery (N = 202) | Third surgery (N = 27) | |
| Days from index surgery to second surgery (SD) | 406.2 (261.9) | 523.7 (282.4) | 401.5 (254.0) | 576.1 (302.7) |
| Days from second surgery to third surgery (SD) | 250.3 (238.2) | 267.0 (233.9) | ||
| Subsequent surgery side (%) | ||||
| Ipsilateral | 100 (70.4%) | 15 (71.4%) | 146 (72.3%) | 18 (66.7%) |
| Contralateral | 42 (29.6%) | 6 (28.6%) | 56 (27.7%) | 9 (33.3%) |
| Subsequent procedure (%) | ||||
| ACL isolated | 80 (56.3%) | 10 (47.6%) | 80 (39.6%) | 10 (37.0%) |
| ACL concomitant meniscal | 20 (14.1%) | 5 (23.8%) | 20 (9.9%) | 5 (18.5%) |
| ACL concomitant meniscal and cartilage | 42 (26.6%) | 6 (28.6%) | 42 (20.8%) | 6 (22.2%) |
| Meniscal procedure isolated | 52 (25.7%) | 4 (14.8%) | ||
| Cartilage procedure isolated | 6 (3.0%) | 1 (3.7%) | ||
| Days from index surgery to second surgery (SD) | 406.2 (261.9) | 523.7 (282.4) | 401.5 (254.0) | 576.1 (302.7) |
| Ipsilateral | 365.8 (254.5) | 495.1 (285.8) | 377.8 (249.2) | 522.3 (280.6) |
| Contralateral | 502.4 (256.9) | 615.2 (280.2) | 463.2 (258.3) | 704.0 (333.6) |
| Days from second surgery to third surgery (SD) | 250.3 (238.2) | 267.0 (233.9) | ||
| Ipsilateral | 194.2 (48.6) | 237.4 (208.0) | ||
| Contralateral | 372.2 (166.5) | 337.4 (289.8) | ||
Table 8.
Properties of subsequent knee procedures by surgical side
| Second surgery | Third surgery | |||
|---|---|---|---|---|
| Ipsilateral | Contralateral | Ipsilateral | Contralateral | |
| Revision ACL (%) | 100 | 42 | 15 | 6 |
| ACL isolated | 51 (51.0%) | 29 (69.0%) | 8 (53.3%) | 2 (33.3%) |
| ACL concomitant meniscal | 9 (9.0%) | 11 (26.2%) | 2 (13.3%) | 3 (50.0%) |
| ACL concomitant meniscal and cartilage | 40 (40.0%) | 2 (2.8%) | 5 (33.3%) | 1 (16.7%) |
| Subsequent knee procedure (%) | 146 | 56 | 18 | 9 |
| ACL isolated | 51 (34.9%) | 29 (51.8%) | 8 (44.4%) | 2 (22.2%) |
| ACL concomitant meniscal | 9 (6.2%) | 11 (19.6%) | 2 (11.1%) | 3 (33.3%) |
| ACL concomitant meniscal and cartilage | 40 (27.4%) | 2 (3.6%) | 5 (27.8%) | 1 (11.1%) |
| Meniscal procedure isolated | 39 (26.7%) | 13 (23.2%) | 1 (5.6%) | 3 (33.3%) |
| Cartilage procedure isolated | 5 (3.4%) | 1 (1.8%) | 1 (5.6%) | 0 (0%) |
| Meniscal and cartilage procedure | 2 (1.4%) | 0 (0%) | 0 (0%) | 0 (0%) |
Multivariable logistic regression model for revision ACL reconstruction showed that patients who were less than 18 years of age at the time of their index surgery were over three times more likely to undergo a revision ACLR compared to older patients (Adjusted Odds Ratio (aOR) 3.77, p = 0.004). Patients with higher IKDC scores at 1 year were less likely to have revision ACLR after adjusting for all other variables in the model (aOR 0.97, p = 0.026). Similarly, for patients undergoing any subsequent knee procedure, patients less than 18 years of age were at four times higher risk than older patients in the cohort (aOR 4.54, p < 0.001). While patients with higher IKDC scores were less likely to undergo any subsequent knee procedure (aOR 0.96, p < 0.001), patients with higher Marx activity scores at 1 year were more likely to need a subsequent knee procedure (aOR 1.09, p = 0.039) (Table 9 and Fig. 2).
Table 9.
Multivariable regression models for factors affecting subsequent knee procedures
| aOR | 95% CI Lower |
95% CI Upper |
p value | |
|---|---|---|---|---|
| Subsequent ACL reconstruction | ||||
| Age group <18 | 3.773 | 1.531 | 9.295 | 0.004 |
| IKDC at 1 year | 0.973 | 0.951 | 0.997 | 0.026 |
| Constant | 0.728 | |||
| Subsequent knee procedure | ||||
| Age group <18 | 4.543 | 1.993 | 10.355 | <0.001 |
| IKDC at 1 year | 0.955 | 0.934 | 0.976 | <0.001 |
| Marx at 1 year | 1.088 | 1.004 | 1.178 | 0.039 |
| Constant | 1.897 | |||
Age group reference: age 40+
Fig. 2.
Multivariable regression models for factors affecting subsequent knee procedures.
Discussion
The first publication of the ACL Registry at the HSS was designed to provide an understanding of the population that is receiving a primary ACL reconstruction and the rates of subsequent surgery following primary ACL reconstruction. The demographics of the HSS registry are similar to those previously published with a slight predominance of male patients of 57.4% and an average age of just under 30 years [7, 11]. Most of the patients in this registry were involved in recreational athletics at the time of injury with 1.5% of professional athletes. The outcome scores in professional athletes and non-professional athletes were similar by 2 years.
There are several limitations to this study. This is the first ACL Registry at our hospital, and there are instances of incomplete surgical data and incomplete follow-up. We observed a 31% follow-up rate on outcome scores, which may limit the generalizability of our results; however, this follow-up rate is similar to what is reported in other registries [6, 9, 15, 16]. This study looked at the 2-year follow-up of primary ACL reconstructions, but longer-term data may ultimately be essential to capture the true reoperation rate following primary ACL reconstruction. This study looked at the reoperation rate at our hospital only. Some patients may seek subsequent knee surgery or subsequent ACL reconstruction at a different hospital or institution. Additionally, we were unable to determine the skeletal maturity of younger patients, which may impact outcome results. Lastly, this study looks at reoperation rates and not reinjury rates, so it may underestimate the overall rates of subsequent ACL or knee injuries.
The majority of patients undergoing primary ACL reconstruction in our registry had an autograft at 76.6%, which is consistent with the data provided by the MOON Group, the Swedish ACL Register, and the Norwegian Registry, but inconsistent with the Kaiser Permanente Registry which used 41.8% allografts [7, 11, 15, 20]. The presence and treatment of meniscal and chondral pathology in our registry data are similar to that previously published [1, 2, 7, 11, 15, 20].
This registry found a 7.3% rate of subsequent ACL reconstruction and 10.3% rate of subsequent operation following a primary ACL reconstruction for patients in this registry. Specifically, there was an overall 7.3% rate of subsequent ACL reconstruction with 5.1% ipsilateral ACL reconstruction (revision) and a 2.2% contralateral ACL reconstruction. The literature varies on the rate of revision ACL and contralateral ACL rupture. Wright et al. reported a 5.8% rate of ACL graft ruptures and an 11.8% contralateral ACL rupture rate in a recent systematic review [23]. Hettrich and the MOON Group reported a 7.7% rate of graft ruptures and 6.4% rate of contralateral ACL ruptures in their cohort at 6-year follow-up [11]. In a more recent report of the MOON Group’s retear rate at 2 years, ipsilateral graft retears occurred in 4.4% of patients and contralateral ACL tears occurred in 3.5% of patients [12]. Shelbourne reported a rate of 5.3% for contralateral ACL injuries and a 4.3% rate of graft ruptures [21]. The Swedish ACL Registry reported a 2-year ACL revision incidence of 1.60 and a 3% contralateral ACL reconstruction [1, 2]. All of these rates are very consistent with our findings of a relatively similar rate of subsequent ACL surgery. Surgeon volume was divided into high volume (52+) versus not high volume (<52). Generally, high-volume surgeons had a lower proportion of a subsequent revision ACL or knee surgery, but only the proportion of revision ACL was statistically significant (p = 0.011). With a lower number of a third procedure, it is difficult to make a definitive conclusion on surgeon volume on this outcome. What we find so far is that there is no consistent association of higher surgeon volume and subsequent revision ACL/subsequent knee surgery. There does not appear to be any difference in case mix as both high- and non-high-volume surgeons’ case mix was 19% <18 years of age.
In our registry, females and younger patients were at higher risk of subsequent ACL reconstruction surgery following a primary ACL reconstruction. Shelbourne reported a higher incidence of reoperations in female patients in the contralateral knee only [21]. Lyman reported on the ambulatory surgery data from New York State and noted that predictors of subsequent knee surgery following primary ACL reconstruction included being female, having a concomitant knee surgery, and being operated on by a lower-volume surgeon [18]. Similar to our findings, increasing age was a negative predictor for both ipsilateral retears and contralateral ACL tears in the MOON Group; however, in this same analysis, females were not noted to have a higher risk [12]. In the Swedish ACL Registry, there was also no noted difference between male and female ACL revisions [1]. The estimated risk of revision ACL or subsequent knee procedure was higher in females in the univariate analysis (OR 1.43 and 1.10, respectively). However, when put into the regression models, there was no difference in risk for subsequent knee procedures between males and females. The effect of age (particularly with patients <18 years of age) had a much larger effects as shown. It may be difficult to ascertain if there were any surgical factors like graft type that made our population less risk prone to other registries. What may be the driving force for the increased risk is that younger people are more likely to have increased athletic exposures after their index ACLR compared to the comparative 40+ older group. This is partially supported by the effect of 1-year Marx scores in the model that show that increased score (frequency of athletic movements that are measured in the Marx survey) is a risk factor for a subsequent knee procedure (aOR 1.09, p = 0.039).
As Hettrich and the MOON Group were the first to point out, subsequent ACL surgeries are only a percentage of the subsequent knee surgeries that ACL reconstruction patients undergo. In our registry, there was a 10.3% rate of subsequent surgery. The MOON Group had a subsequent surgery rate of 18.9% at 6 years [11].
Subsequent knee surgery rates were higher in patients less than 18 years of age, patients who had a meniscal repair, and patients who had a chondral lesion of the medial femoral condyle. Shelbourne reported that the rates of subsequent surgery were highest for patients less than 18 years of age and least for patients greater than 25 years of age [21]. Our regression analysis found that patients less than 18 years of age were more likely to have a subsequent knee operation and a subsequent ACL reconstruction and patients over age 40 were less likely to have subsequent ACL and subsequent knee operations. The increased risk for reoperation seen in younger patients may be due to higher levels of activity in this population and increased demands placed on the graft as well as a higher rate of recurrent instability [13]. Our analysis showed that there was no effect of graft type on the risk for subsequent operations. The fact that graft did not have any effect on outcomes is in contrast to that of the MOON Group who found that the use of an allograft was a major predictor for a subsequent surgery and ipsilateral retear and that of the Norwegian Registry and Scandinavian Registry that found lower risk of revision ACL reconstruction with patella tendon autografts versus hamstring autografts [10–12, 20]. There was a skewed distribution of graft type used for the <18 age group. Of all allografts used, only 1% was used in patients <18 years of age, compared to 26% of patients in the autograft group that were in that same age group.
Overall, this is a first step to evaluate the demographics and short-term outcomes in patients undergoing primary ACL reconstruction at our institution. There is a low reoperation rate and a low subsequent ACL reconstruction rate at our institution.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgments
The authors would like to acknowledge the HSS ACL Registry Group for their contribution to this research.
Compliance with Ethical Standards
Conflict of Interest
Moira McCarthy, MD, Katherine Mallett, BA, Matthew Abola, BA, Sherrie Vassallo, and Joseph Nguyen, PhD, have declared that they have no conflict of interest.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Therapeutic Study Level III
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9532-6) contains supplementary material, which is available to authorized users.
References
- 1.Andernord D, Björnsson H, Petzold M, et al. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish national knee ligament register on 13,102 patients. Am J Sports Med. 2014;42:1574–1582. doi: 10.1177/0363546514531396. [DOI] [PubMed] [Google Scholar]
- 2.Andernord D, Desai N, Björnsson H, Gillén S, Karlsson J, Samuelsson K. Predictors of contralateral anterior cruciate ligament reconstruction: a cohort study of 9061 patients with 5-year follow-up. Am J Sports Med. 2015;43:295–302. doi: 10.1177/0363546514557245. [DOI] [PubMed] [Google Scholar]
- 3.Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42:1806–1812. doi: 10.1177/0363546514540862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bollen SR, Scott BW. Rupture of the anterior cruciate ligament—a quiet epidemic? Injury. 1996;27:407–409. doi: 10.1016/0020-1383(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 5.Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the national football league: epidemiology and current treatment trends among team physicians. Arthrosc J Arthrosc Relat Surg. 2002;18:502–509. doi: 10.1053/jars.2002.30649. [DOI] [PubMed] [Google Scholar]
- 6.Clarnette R, Graves S, Lekkas C (2016) Overview of the AOA national joint replacement registry ACL registry pilot study. Orthop J Sports Med. 4. doi:10.1177/2325967116S00007.
- 7.Csintalan RP, Inacio MCS, Funahashi TT, Maletis GB. Risk factors of subsequent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:619–625. doi: 10.1177/0363546513511416. [DOI] [PubMed] [Google Scholar]
- 8.Dunn WR, Lyman S, Lincoln AE, Amoroso PJ, Wickiewicz T, Marx RG. The effect of anterior cruciate ligament reconstruction on the risk of knee reinjury. Am J Sports Med. 2004;32:1906–1914. doi: 10.1177/0363546504265006. [DOI] [PubMed] [Google Scholar]
- 9.Faunø P, Rahr-Wagner L, Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents. Orthop J Sports Med. 2014 doi: 10.1177/2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42:2319–2328. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 11.Hettrich CM, Dunn WR, Reinke EK, Spindler KP. The rate of subsequent surgery and predictors following ACL reconstruction: two- and six-year follow-up from a multicenter cohort. Am J Sports Med. 2013;41:1534–1540. doi: 10.1177/0363546513490277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, MOON Consortium. Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41:1808–1812. doi: 10.1177/0363546513493896. [DOI] [PubMed] [Google Scholar]
- 14.Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and the ACL Study Group. J Pediatr Orthop. 2002;22:452–457. [PubMed] [Google Scholar]
- 15.Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish national anterior cruciate ligament register. Arthrosc J Arthrosc Relat Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2014;30:803–810. doi: 10.1016/j.arthro.2014.02.036. [DOI] [PubMed] [Google Scholar]
- 16.LaPrade CM, Dornan GJ, Granan L-P, LaPrade RF, Engebretsen L. Outcomes after anterior cruciate ligament reconstruction using the Norwegian knee ligament registry of 4691 patients how does meniscal repair or resection affect short-term outcomes? Am J Sports Med. 2015;43:1591–1597. doi: 10.1177/0363546515577364. [DOI] [PubMed] [Google Scholar]
- 17.Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012;40:1551–1557. doi: 10.1177/0363546512446000. [DOI] [PubMed] [Google Scholar]
- 18.Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321–2328. doi: 10.2106/JBJS.H.00539. [DOI] [PubMed] [Google Scholar]
- 19.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthrosc J Arthrosc Relat Surg. 2003;19:762–770. doi: 10.1016/S0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 20.Persson A, Fjeldsgaard K, Gjertsen J-E, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction a study of 12,643 patients from the Norwegian cruciate ligament registry, 2004–2012. Am J Sports Med. 2014;42:285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 21.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 22.Spindler KP, Wright RW. Anterior cruciate ligament (ACL) tear. N Engl J Med. 2008;359:2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction. J Bone Joint Surg Am. 2011;93:1159–1165. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)