Abstract
Background
Pin infection continues to be a nuisance when using definitive external fixation. Prophylactic antibiotic treatment has been proposed in an effort to decrease pin complications.
Questions/Purposes
We performed a prospective, randomized, single-blinded study to answer the following questions: (1) what was the effect of a 10-day course of oral prophylactic antibiotics administered immediately after external fixation surgery on the incidence of a subsequent pin infection, (2) what was the effect on the severity of a subsequent pin infection, and (3) what was the effect on the timing of a subsequent pin infection?
Methods
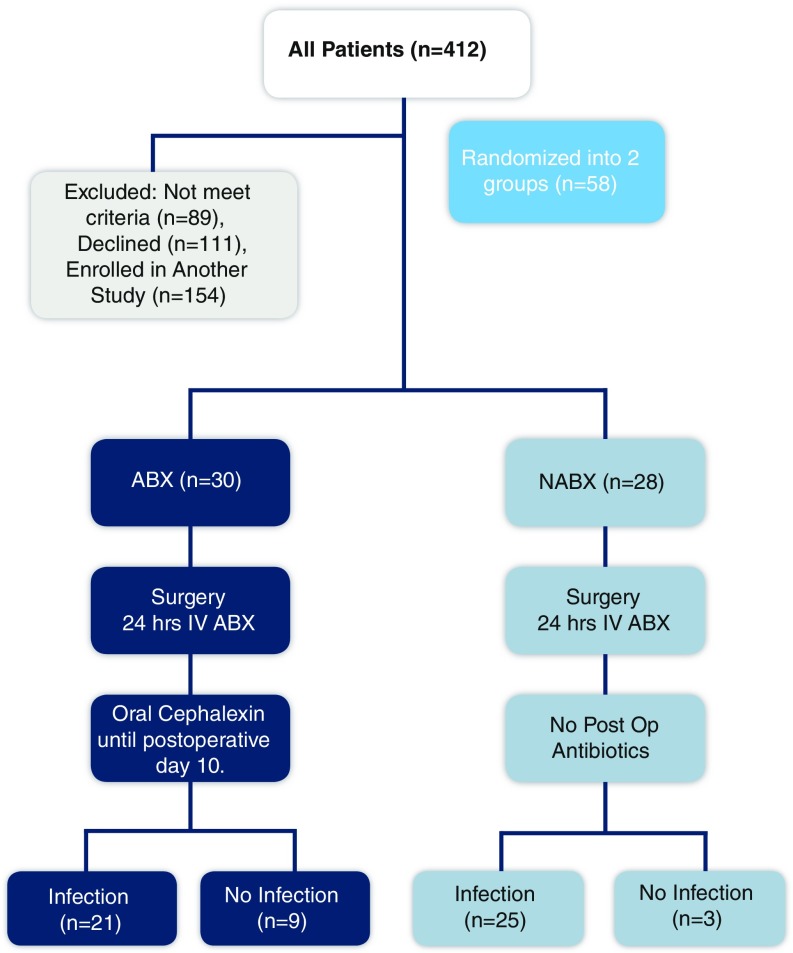
Patients were randomized into antibiotic treatment and control groups, and incidence, severity, and time of onset of pin infection were recorded.
Results
The incidence of pin infection for the entire cohort during the 90-day observation period was 46/58 (79%) without a statistically significant difference (p = 0.106). There was no statistical difference found (p = 0.512) in pin infection severity. There was no significant difference in the time of onset of infection between the two groups from the date of surgery (p = 0.553).
Conclusions
Our randomized data do not suggest that oral antibiotics alter the incidence, timing, or severity of pin infection. This study does not support the use of prophylactic oral antibiotics in healthy patients.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9539-z) contains supplementary material, which is available to authorized users.
Keywords: prophylactic antibiotics, pin infection, external fixation, Ilizarov
Introduction
Circular external fixators used as definitive bony fixation that utilize half pins and tensioned wires have proven to be extremely useful in modern orthopedic surgery particularly in the field of limb lengthening and complex reconstruction where osteomyelitis and deformity are treated [1, 5, 6, 10, 14, 15]. Despite the utility of these remarkable devices, the incidence of pin site infection during the course of external fixation is high with reports varying from 10 to 100% [4, 11, 16]. Typical pin site infections manifest as a superficial painful cellulitis at the point of skin entry, but if untreated, they can progress in severity, and they can hinder proper rehabilitation by reducing joint motion and weight bearing. In severe cases, pin site infection can lead to loosening of fixation and deep bone infection [8]. Many experts recognize that the vast majority of pin site infections are not true surgical site complications but, rather, expected nuisances highly responsive to short courses of oral antibiotics [12].
In an effort to decrease the incidence of pin infections, many surgeons commonly prescribe a course of prophylactic oral antibiotics (usually cephalexin) immediately following frame placement. The benefits and risks of routine multi-day courses of antibiotics to prevent pin site infection have not been studied in a systematic fashion. Not only is the efficacy undocumented, but these courses of antibiotics may increase the risk of Clostridium difficile [13], may have far reaching deleterious effects on the gut microbiome [9], and can increase the risk of acquisition of resistant pathogens [9]. They also represent additional cost to the patient and medical system.
We performed a prospective, randomized, single-blinded study to answer the following questions: (1) what was the effect of a 10-day course of oral prophylactic antibiotics administered immediately after external fixation surgery on the incidence of a subsequent pin infection, (2) what was the effect on the severity of a subsequent pin infection, and (3) what was the effect on the timing of a subsequent pin infection?
Patients and Methods
Institutional IRB approval was obtained, and informed consent was obtained from all enrolled patients. From March 2011 to May 2014, the operating surgeons performed 412 “application of external fixation” surgeries. Inclusion criteria included patients undergoing upper or lower limb reconstruction surgery with the use of an external fixator. Exclusion criteria included enrollment in another prospective study, a diagnosis of diabetes mellitus or rheumatoid arthritis, the active use of immunomodulators (prednisone or biologic immunosuppressive medications), a history of infection at the surgical site, known allergy to beta-lactam antibiotics, the use of any antibiotics within 3 months of surgery, and neuropathic arthropathy (Table 1).
Table 1.
Patient demographics
| Patient characteristic (N = 58) | n (%) |
|---|---|
| Study group | 58 |
| NABX | 28 (48.3%) |
| ABX | 30 (51.7%) |
| Age at time of surgery | 42.1 (14.2) |
| Height | 67.6 (4.1) |
| Weight | 185.2 (46.3) |
| BMI | 28.3 (6.3) |
| Days in frame | 98.9 (29.0) |
| Days out from surgery | 15.3 (6.9) |
| No. of days post-op before 1st infection | 30.2 (21.9) |
| Female sex | 30 (51.7%) |
| Smoker | 33 (61.1%) |
NABX no antibiotics, ABX antibiotics
Patients were randomized 1:1 to receive postoperative oral antibiotic therapy (ABX) or not (NABX) using a computer randomization program. The control group did not receive a placebo. Randomization was performed by the research coordinator and communicated to the team-dedicated inpatient physician assistant (PA) (Table 2). All patients underwent non-emergent limb reconstruction surgery including the application of an external fixator. Concomitant surgeries performed in the same setting are listed (Table 3). The half pins used were 6 mm tapered, hydroxyapatite (HA) coated, and stainless steel. These pins were inserted by hand after pre drilling through a soft-tissue protection sleeve. The wires used were 1.8 mm, stainless steel, K-wires. Wires were tensioned to 130 kg except talus drop-wires, which were tensioned to 70 kg. Tethered skin was released at the pin sites when necessary. Standard practices for frame application with stable fixation were followed ensuring there was no ring instability. All patients were treated with an identical pin care protocol. Pin site dressings were removed postoperative day 2 and pin care was initiated. The sites were cleaned with a solution of hydrogen peroxide diluted with sterile saline in a ratio of 1:1. Sterile elastic bandaging was wrapped around the pins.
Table 2.
Patient demographics by cohort
| Patient characteristic | NABX (N = 28) | ABX (N = 30) | p value |
|---|---|---|---|
| N (%) | Mean (SD) or n (%) | ||
| Age at time of surgery | 39.5 (12.9) | 44.4 (15.1) | 0.187 |
| Height | 68.3 (3.7) | 66.9 (4.3) | 0.215 |
| Weight | 189.3 (48.5) | 181.2 (44.7) | 0.530 |
| BMI | 28.3 (6.3) | 28.3 (6.4) | 0.992 |
| Days in frame | 94.4 (15.9) | 103.0 (37.2) | 0.255 |
| Female sex | 15 (53.6%) | 15 (50.0%) | 0.786 |
| Smoker | 3 (10.7%) | 4 (13.3%) | >0.999 |
Table 3.
Surgical procedure
| Surgery | NABX | ABX | p value |
|---|---|---|---|
| Frequency goals achieved (%) | Frequency goals achieved (%) | ||
| Ankle distraction (N = 27) | 13 (92.9%) | 13 (100%) | >0.999 |
| Tibia osteotomy (18) | 11 (100%) | 7 (100%) | N/A |
| Ankle fusion (6) | 4 (100%) | 2 (100%) | N/A |
| Femur osteoplasty (6) | 2 (100%) | 4 (100%) | N/A |
| Knee distraction (1) | 1 (100%) | 0 (0%) | N/A |
N /A not available
In accordance with our routine perioperative protocols, all patients received intravenous cefazolin within 1 h prior to the skin incision and then as necessary intraoperatively [2, 3]; IV cefazolin was then continued every 8 h to complete 24 h of perioperative IV antibiotics. Cephalexin 500 mg four times daily subsequently was prescribed to the experimental group (ABX) upon termination of the 24-h IV cefazolin course. ABX patients were given a prescription to complete a 10-day course of cephalexin upon hospital discharge. The surgeons and a registered nurse providing all outpatient postoperative care for the patients after discharge were unaware of the treatment arm assignment. The study was conducted prior to electronic medical records and e-prescribing making it easy to conceal the study group from the caregivers. There was no follow-up to ensure compliance with the four times per day dosing of antibiotic as this is not the standard of care in this practice.
Pin infection surveys were completed during a 2-week follow-up visit and at all subsequent visits for 90 days. The survey was filled out by either the primary nurse or one of the two treating surgeons for all patients during routine visits regardless of whether or not they had an infection. The survey included severity grading of the pin infection [7] (Table 4). If no infection was present, then that was noted. Patients were trained to recognize signs of pin infections including new onset pain at a pin site, increased drainage from a pin site, purulence at a pin site, or erythema at the site. When patients developed pin infections at home, they contacted one of the senior surgeons or the primary nurse. They were asked to come to the office within the next business day for grading of the infection, scoring, and treatment. Patients unable to return to the office on short notice were required to speak to the treating team by telephone and to email a digital image of the affected site. Grading was performed based on the clinical information provided. We recognize that the grading of a pin infection over the phone and through email introduced a margin of error in diagnostic accuracy. However, this method of establishing the presence of a pin infection is used clinically in our practice. We felt that adherence to our normal protocol would make this study most applicable to clinical practice. The ability of patients in the ABX group to adhere to the four times daily dosing was not recorded as this is not part of our standard practice.
Table 4.
Pin site infection severity
| Gordon Pin Infection Classification | Description |
|---|---|
| Grade 0 | Clean |
| Grade 1 | Pain or erythema, no drainage |
| Grade 2 | Pain, erythema, and serous drainage |
| Grade 3 | Pain, erythema, and purulent drainage |
| Grade 4 | Pain, erythema, purulent drainage with radiographic osteolysis |
| Grade 5 | Ring sequestrum or osteomyelitis |
Patients were followed at regular 2–4-week intervals as dictated by routine postoperative protocols. Routine radiographs were obtained at each visit. These films allowed for the visualization of the pin-bone interface, which enabled the diagnosis of pin loosening (stage 4–5 infection). Pin infection surveys were completed at each visit and for each phone call/email encounter until POD 90. The endpoint of 90 days was selected because most patients had the frame on the leg for a period of 90 days, and it was unlikely that an immediate postoperative course of antibiotics would have any influence more than 90 days after surgery. Development of diarrhea, thrush, and drug allergy symptoms was recorded during the postoperative visits. Pin cultures were taken only in instances of purulent drainage, as per clinical routine (Table 5).
Table 5.
Pin site culture results
| Culture identity | NABX | ABX | p value | ||
|---|---|---|---|---|---|
| Total N | n (%) | Total N | n (%) | ||
| No growth | 12 | 6 (50.0%) | 9 | 5 (55.6%) | 0.131 |
| Staph epi | 12 | 0 (0%) | 9 | 3 (33.3%) | |
| CONS | 12 | 3 (25.0%) | 9 | 0 (0%) | |
| P. acnes | 12 | 0 (0%) | 9 | 1 (11.1%) | |
| Strep | 12 | 1 (8.3%) | 9 | 0 (0%) | |
| Enterococcus | 12 | 1 (8.3%) | 9 | 0 (0%) | |
| Klebsiella | 12 | 1 (8.3%) | 9 | 0 (0%) | |
CONS coagulase negative staphylococci, P. acnes Propionibacterium acnes
Pin infections were generally treated with a 10-day course of oral cephalexin. In cases where the infection did not resolve quickly, additional antibiotics were used (typically including doxycycline or bactrim). The choice of additional antibiotic was left to the discretion of the treatment team.
Statistical Analysis
We hypothesized that receipt of postoperative antibiotics would not have a significant impact on the incidence or severity of postoperative pin infections. Our primary endpoint was pin site infection within 90 days of surgery. Secondary endpoints included severity of infection, achievement of orthopedic goals, incidence of readmission for infection, incidence of surgical site infectious complications other than pin infection, incidence of antibiotic toxicity, and frequency of isolation of multidrug-resistant organisms.
Statistical analysis comprised reporting of means and standard deviations for continuous variables and frequencies and percentages for discrete variables of the study population. Since continuous variables did not meet the assumption of normality, non-parametric Mann-Whitney U tests were used to evaluate differences in the continuous variables between antibiotic treatment group and control. Chi-square and Fisher’s exact tests were used to evaluate associations between categorical variables between the study groups. Statistical significance was set to p ≤ 0.05 and all analyses were performed using SPSS version 22.0 (IBM Corp., Armonk, NY).
Results
Fifty-eight patients, of whom 30 were randomized to the ABX group, enrolled. The mean age was 42, and the mean BMI was 38. There were 30 females (51%). All remained in the study for the 90-day observation period. Orthopedic goals were obtained in 57/58. Failed goals occurred in one patient who failed to benefit from ankle distraction and proceeded to have ankle replacement surgery. This failure was unrelated to pin infection. The patient was in the control group (NABX).
The incidence of pin infection for the entire cohort during the 90-day observation period was 46/58 (79%). ABX and NABX group incidence rates were 21/30 (70%) and 25/28 (89%), respectively, without a statistically significant difference (p = 0.106) (Fig. 1). Although there was no significant difference, there appears to be a trend suggesting that antibiotics lowered the number of infections. A post hoc power analysis showed 37.2% power. In order to achieve 80% power, the sample size would need to have been 75 in each arm of the study (total 150 participants). In cases where the first line of antibiotic was not working and drainage was present, pin site cultures were obtained (16/58).
Fig. 1.
This figure is a CONSORT group flow diagram demonstrating the prospective study design used.
The range of infection severity in this study population ranged from grade 1 to grade 3, with the highest proportion of infection severity in each group being grade 2. When comparing the differences in infection severity between the study groups, there was no statistical difference found (p = 0.512). Although it appears that there may have been more severe infections in the no antibiotic group, a post hoc power analysis of the severity of pin infection showed that we had 12% power. In order to achieve 80% power, 188 patients would have needed to be in each group (total 376).
The average onset of pin site infection for the entire cohort was 30 days (5–68 days) after surgery. The average onset of pin site infection for the ABX group was 32 days (9–68 days) after surgery. Controlling for the 10 days of antibiotic administration (calling POD 10 “day 0”), the onset of infection was 22 days (−1 to 58 days) from the date of last antibiotic dose. The average onset of infection for the NABX group was 28 days (5–65 days). There was no significant difference in the onset of infection between the two groups from the date of surgery. (p = 0.553). There was no significant difference in the timing of infection onset between the two groups measured from the date of antibiotic termination (p = 0.383) (Table 6).
Table 6.
Results
| Outcomes | NABX | ABX | p value | ||
|---|---|---|---|---|---|
| Total N | n (%) | Total N | n (%) | ||
| Infection present | 28 | 25 (89.3%) | 30 | 21 (70.0%) | 0.106 |
| No. of days post-op before 1st infection (unadjusted) | 23 | 28.3 (23.2) | 20 | 32.4 (20.8) | 0.553 |
| No. of days post-op before 1st infection (adjusted) | 23 | 28.3 (23.2) | 20 | 22.4 (20.8) | 0.383 |
| Max pin grade infection (max. 5) | |||||
| Grade 1 | 25 | 5 (20.0%) | 21 | 7 (33.3%) | 0.512 |
| Grade 2 | 25 | 11 (44.0%) | 21 | 9 (42.9%) | |
| Grade 3 | 25 | 9 (36.0%) | 21 | 5 (23.8%) | |
| Grade 4 | 25 | 0 (0%) | 21 | 0 (0%) | |
| Grade 5 | 25 | 0 (0%) | 21 | 0 (0%) | |
| Developed cellulitis | 28 | 2 (7.1%) | 30 | 2 (6.7%) | >0.999 |
Unadjusted = calculated using postoperative day. Adjusted = calculated not including the 10 days of oral antibiotics for the treatment group
No complications were observed as a result of the oral antibiotic intervention. No patients developed diarrhea, thrush, or an allergic reaction to the cephalosporin. Cellulitis of the leg that required treatment with IV antibiotics developed in 2/30 (6.7%) patients in the ABX group and in 2/28 (7.1%) patients in the NABX group. No significant difference was measured between the two groups regarding the development of cellulitis; each group had two patients develop cellulitis (p > 0.999). Finally, there were no severe infections of the reconstructed limbs and no isolation of multidrug-resistant pathogens from any patients in the study.
Discussion
Complex limb reconstruction is an evolving field, and the incidence of symptomatic pin site infection after external fixator placement is high. Any intervention that reduces this problem deserves study. Postoperative oral prophylactic antibiotics are routinely given after external fixator placement, but little evidence exists to support this practice. This prospective study aimed to identify whether a short course of oral postoperative antibiotics could reduce pin infections in healthy individuals after external fixator surgery. We found no significant difference between the two groups with regard to pin site infection incidence, severity, or timing of onset while recognizing that our data is underpowered.
There are some limitations to this study. While the study showed a 19% decrease in the proportion of infection onset between the NABX and ABX groups, the sample size did not allow for enough statistical power to demonstrate that difference to be a statistically significant difference. For all secondary outcomes, a post hoc power analysis revealed a need for almost three times the number of patients to be enrolled in the study to find statistical significance in the effect sizes that were found in our study. We recognize that even though we did not find significance in the primary outcome, this may have been because of lack of power. It was difficult to enroll patients in this study, and the prospect of tripling the enrollment was impossible. The patients were not blinded, as the control group was not given a placebo. Different procedures were performed in different bones, leading to subgroup heterogeneity. Finally, the role of antibiotics in immunocompromised patients undergoing external fixation surgery may be different, but this was not addressed in this study. Other limitations include no use of a placebo in the control group, no compliance data for the treatment group tracking adherence to the four times per day regimen, and not tracking how many patients were evaluated in person verses remotely for pin infections. Discrepancies between the groups could introduce bias.
Our randomized data show that prophylactic oral antibiotics do not significantly alter the incidence, timing, or severity of pin infection. Although underpowered, this study does not support the use of prophylactic oral antibiotics in healthy patients. We have discontinued this practice in our institution as a result of these data and have not noticed any increase in pin infection or severity since doing so over 2 years ago. Both the experimental and control groups had a high incidence of pin infection, a similar severity, and a similar timing of infection. Patients that became infected were treated successfully with antibiotics: oral antibiotics were effective in treating pin infection once present. W-Dahl et al. [17] studied the effect of administering 3 days of prophylactic antibiotics to patients compared with an historical control group in the setting of proximal tibial osteotomy using external fixation. The study examined 106 patients with a mean age of 52 years. Sixty patients were treated with pre-operative antibiotics and three additional days of postoperative antibiotics. A change in practice called for a single dose of IV antibiotics before surgery, which is how a second group of 46 patients was treated. The authors concluded that there were no differences between the groups with regard to the postoperative: incidence of pin infection, severity of pin infection, presence of Staphylococcus aureus, incidence of pin loosening, number and type of complication, or hospital length of stay. The authors concluded that a single dose of IV antibiotics within 60 min of surgery was adequate for infection prevention, and the addition of further antibiotics was of no benefit. These findings were similar to ours, in a group of patients undergoing like surgery.
While our study was powered to demonstrate a superior effect of oral antibiotics versus a standard control, future non-inferiority or equivalence studies need to be designed with the necessary sample size to truly demonstrate the equivalent effect of oral antibiotics compared to the standard control. Our study currently can conclude only that there was no difference between the antibiotic and non-antibiotic groups. Ultimately, the incidence of pin site infections is high, whether or not postoperative antibiotics are given. The higher incidence of infection in our study compared to others could have many etiologies including pin care protocol, patient demographics, or hyper vigilance by providers. It is important to explore whether future modalities of prevention (including changes to pin site and skin care protocols, early prediction and recognition of symptom onset, and improvements in anti-infective attributes of surgical materials) may offer benefits that postoperative oral antibiotics lack.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
Acknowledgements
We would like to thank, Erica Lenihan, RN, for her help with grading and treating pin infection; Lisa Halfen, RPA, for administering antibiotics postoperatively and keeping the treatment team blinded; Joseph T. Nguyen, MPH, for statistical analysis; and Eugene Borst, BS, for assistance with all workflow aspects of this study. You all contributed significantly to the success of this research project.
Compliance with Ethical Standards
Conflict of Interest
Andy O. Miller, MD, Barry D. Brause, MD, and Vladimir Goldman, MD, have declared that they have no conflict of interest. Austin T. Fragomen, MD, reports, other than Smith and Nephew, personal fees from NuVasive, Synthes, and Stryker, outside the work. S. Robert Rozbruch, MD, reports personal fees from Smith and Nephew, Stryker, and NuVasive, outside the work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Therapeutic Study Level I.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-016-9539-z) contains supplementary material, which is available to authorized users.
References
- 1.Bernstein M, Fragomen A, Sabharwal S, et al. Does integrated fixation provide benefit in the reconstruction of posttraumatic tibial bone defects? Clin Orthop Rel Res. 2015;473(10):3143–3153. doi: 10.1007/s11999-015-4326-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195–283. doi: 10.2146/ajhp120568. [DOI] [PubMed] [Google Scholar]
- 3.Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: an advisory statement from the national surgical infection prevention project. Clin Infect Dis. 2004;38(12):1706–1715. doi: 10.1086/421095. [DOI] [PubMed] [Google Scholar]
- 4.Davies R, Holt N, Nayagam S. The care of pin sites with external fixation. J Bone Joint Surg (Br) 2005;87B(5):716–719. doi: 10.1302/0301-620X.87B5.15623. [DOI] [PubMed] [Google Scholar]
- 5.Fourman M, Borst E, Bogner E, et al. Recombinant human BMP-2 increases the incidence and rate of healing in complex ankle arthrodesis. Clin Orthop Rel Res. 2014;472(2):732–739. doi: 10.1007/s11999-013-3261-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fragomen AT, Borst E, Schachter L, et al. Complex ankle arthrodesis using the Ilizarov method yields high rate of fusion. Clin Orthop Rel Res. 2012;470(10):2864–2873. doi: 10.1007/s11999-012-2470-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gordon JE, Kelly-Hahn J, Carpenter CJ, et al. Pin site care during external fixation in children: results of a nihilistic approach. J Pediatr Orthop. 2000;20:163–165. [PubMed] [Google Scholar]
- 8.Green SA. Complications of external skeletal fixation. Clin Orthop Rel Res. 1983;180:109–116. [PubMed] [Google Scholar]
- 9.Kavanagh KT, Calderon LE, Saman DM, et al. The use of surveillance and preventative measures for methicillin resistant staphylococcus aureus infections in surgical patients. Antimicrob Resist Infect Control. 2014;14(3):18. doi: 10.1186/2047-2994-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuchinad R, Fourman MS, Fragomen A, et al. Knee arthrodesis as limb salvage for complex failures of total knee arthroplasty. J Arthroplasty. 2014;29(11):2150–2155. doi: 10.1016/j.arth.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 11.Marsh DR, Shah S, Elliott J, et al. The Ilizarov method in nonunion, malunion, and infection of fractures. J Bone Joint Surg (Br) 1997;79B(2):273–279. doi: 10.1302/0301-620X.79B2.6636. [DOI] [PubMed] [Google Scholar]
- 12.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Rel Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 13.Poeran J, Mazumdar M, Rasul R, et al. Antibiotic prophylaxis and risk of Clostridium difficile infection after coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2015. [DOI] [PMC free article] [PubMed]
- 14.Rozbruch SR, Pugsley JS, Fragomen A, et al. Repair of tibial nonunions and bone defects with the Taylor Spatial Frame. J Orthop Trauma. 2008;22(2):88–95. doi: 10.1097/BOT.0b013e318162ab49. [DOI] [PubMed] [Google Scholar]
- 15.Schottel P, Muthusamy S, Rozbruch SR. Distal tibial periarticular nonunions: ankle salvage with bone transport. J Orthop Trauma. 2014;28(6):e146–e152. doi: 10.1097/BOT.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 16.Shtarker H, David R, Stolero J, et al. Treatment of open tibial fractures with primary suture and Ilizarov fixation. Clin Orthop Relat Res. 1997;335:268–274. [PubMed] [Google Scholar]
- 17.W-Dahl A, Toksvig-Larsen S. Infection prophylaxis: a prospective study in 106 patients operated on by tibial osteotomy using the hemicallotasis technique. Arch Orthop Trauma Surg. 2006;126:441–447. doi: 10.1007/s00402-006-0165-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1225 kb)
(PDF 1224 kb)