Abstract
Background
The advent of modular shoulder arthroplasty systems has allowed the conversion of hemiarthroplasty or total shoulder arthroplasty to reverse total shoulder arthroplasty (RTSA) without removing a well-fixed stem.
Questions/Purposes
To determine the feasibility, functional outcome, and complication profile of RTSA modular conversion.
Methods
A prospective shoulder arthroplasty registry was queried for consecutive patients scheduled for a modular conversion from January 1, 2007, to April 1, 2015. Eligible patients had medical charts and operative records reviewed for preoperative diagnosis, age, medical comorbidities, preoperative American Shoulder and Elbow Society (ASES) score, preoperative Visual Analogue Scale (VAS) pain and instability scores, and intraoperative findings. Each patient was then contacted by telephone or mail to complete up-to-date ASES and VAS questionnaires.
Results
Seventeen patients underwent a modular conversion. Nine patients were scheduled for modular conversion but underwent humeral revision due to excessive soft tissue tension (65.3% modular conversion rate). Average follow-up was 37.4 months (range 10.0–67.6 months). Pain scores improved from 5.3 (range 0.4 to 8.0) to 2.4 (range 0 to 9.3) (p < 0.01), instability VAS from 5.2 (range 0 to 10) to 1.1 (range 0 to 6.8) (p < 0.01), and ASES scores improved from 35.2 (range 20.7 to 61.3) to 65.6 (range 11.8 to 92) (p < 0.01).
Conclusions
Modular conversion of an anatomic to a RTSA is feasible in a majority of patients. Despite the complexity of the procedure, modular conversion of hemiarthroplasty or TSA to RTSA can significantly improve functional outcomes with a low rate of complications.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9546-8) contains supplementary material, which is available to authorized users.
Keywords: hemiarthroplasty, total shoulder arthroplasty, reverse total arthroplasty, modular, revision
Introduction
Total shoulder arthroplasty (TSA) and hemiarthroplasty are important surgical options in the setting of debilitating glenohumeral joint osteoarthritis and select proximal humerus fractures not amenable to open reduction and internal fixation [7, 18, 20]. However, complications can arise that necessitate revision such as component loosening, instability, infection, peri-prosthetic fracture, and rotator cuff deficiency [2, 13, 27, 28]. Historically, these patients would have been candidates for a salvage procedure, such as conversion to hemiarthroplasty, resection arthroplasty, or even arthrodesis; however, these procedures did not have predictable outcomes in terms of pain and function. More recently, conversion to reverse total shoulder arthroplasty (RTSA) has been increasingly utilized in these patients with favorable short- and mid-term outcomes reported in multiple studies [2, 6, 17, 19].
The leading causes for TSA and hemiarthroplasty revision are glenoid loosening, instability, and rotator cuff deficiency [2, 24]. Conversion to RTSA may be utilized in many of these revision settings. In the past, conversion would require removal of the humeral stem, even if well-fixed. However, newer modular systems allow for conversion of an anatomic arthroplasty to a RTSA without humeral stem exchange [5]. Thus, modular systems may be advantageous by avoiding the risks inherent to exchanging a well-fixed humeral stem, such as bone loss, nerve injury, fracture, and/or osteotomy nonunion [5, 27].
In this retrospective study, we sought to determine the feasibility, functional outcome, and complication profile of RTSA modular conversion from hemiarthroplasty and TSA. Furthermore, we were interested in which clinical scenarios (e.g., fixed humeral head subluxation) may inhibit the ability to perform RTSA modular conversion.
Patients and Methods
The authors’ institutional review board approved this study. A prospective shoulder arthroplasty registry was queried for consecutive patients who underwent a modular conversion from a TSA or hemiarthroplasty to a RTSA from January 1, 2007, to April 1, 2015. All preexisting stems were either the Biomet Bio-Modular stem which was converted using a Bio-Modular to Comprehensive Reverse Adapter (Warsaw, Indiana), or the stem was a Biomet Comprehensive in which the stem of the preexisting shoulder replacement remains fitted. All patients had a preoperative aspiration which ruled out infection prior to the revision surgery. No patient had positive intraoperative cultures.
Eligible patients had their medical charts and operative records reviewed for preoperative diagnosis, age, medical comorbidities, preoperative American Shoulder and Elbow Society (ASES) score, preoperative Visual Analogue Scale (VAS) pain and instability scores, and intraoperative findings. Each patient was then contacted by telephone or mail in order to complete up-to-date ASES and VAS questionnaires. Patients who were unreachable after five attempts were considered lost to follow-up.
Surgical Technique
All procedures were performed by the senior surgeons using the Biomet Reverse Comprehensive Shoulder System (Warsaw, Indiana). The patient was placed in the beach chair position and a deltopectoral approach was utilized after administration of general anesthesia in combination with an interscalene block. All patients received perioperative intravenous antibiotic prophylaxis after appropriate cultures were taken. The subscapularis tendon (if present) was tenotomized or elevated off the lesser tuberosity. The prosthetic head was detached from the stem with a manufacturer-specific extraction instrument. Proximal humeral bone was prepared to allow placement of the humeral tray flush with the existing metaphyseal bone.
Next, the glenoid was exposed and any remaining labrum excised. Glenoid implants and cement from the previous component were removed carefully. The guidewire for the glenoid reamer was positioned utilizing the glenoid surface guide on the most advantageous area of glenoid. The glenoid was minimally reamed and a baseplate was impacted into the prepared bone. A central compression screw was used to achieve bicortical fixation, and peripheral locking screws were utilized. The glenosphere was assembled and impacted into the reverse morse taper in the center of the baseplate. Attention was then returned to the humeral side where the humeral tray and polyethylene liner of appropriate thickness were assembled and implanted. The shoulder was reduced and soft tissue tension assessed. The humeral stem was left in place so long as the shoulder was able to be reduced without excessive tension. It should be noted that the primary humeral stem was placed in 30° of retroversion in all cases. If this could not be attained, then humeral revision was initiated. After the humeral stem was removed, a lower humeral cut was made and a new stem was placed in order to attain adequate soft tissue tensioning. The subscapularis was repaired, when appropriate and tendon was present to repair, with heavy nonabsorbable braided sutures through drill holes in the lesser tuberosity.
Patients were placed in a sling for 2 to 4 weeks postoperatively, and physical therapy and range of motion protocols were begun immediately.
Statistical Analysis
Preoperative clinical examination scores were compared with postoperative clinical scores by paired Student’s t test. Statistical significance was set at p < .05.
Results
A review of the registry identified 26 patients who underwent revision arthroplasty with the intention of modularly converting an anatomic shoulder arthroplasty to a reverse shoulder arthroplasty. At the time of surgery, 17 patients were able to undergo modular conversion of the humeral stem (65.3%). The primary implant was a TSA (10) and hemiarthroplasty (7). Nine patients required humeral revision due to excessive soft tissue tension that either prohibited reduction of the trial components or resulted in limited motion and deltoid strain once reduced. Of the nine patients who were unable to be converted, 1 had static anterior subluxation, 2 had a posterior dislocation, 2 had superior migration with abutment of the acromion, and 4 had a preexisting BioModular component. All patients in which modular conversion was not feasible had either fixed humeral head subluxation or dislocation, or had a preexisting BioModular stem. Of the 17 patients in which modular conversion was feasible, 1 had static anterior subluxation, 4 had superior migration of the humeral head such that was abutting the acromion, and 2 had a preexisting BioModular stem.
For patients who underwent modular conversion, the average age at surgery was 70.3 years (range 45 to 91 years). There were 11 females and 6 males. Average time to modular conversion was 31.9 months (range 3.0 to 119.8 months). The average length of follow-up was 37.4 months (range 10.0 to 67.6 months). The etiology of revision surgery is indicated in Table 1. Blood loss averaged 225 mL (range 100–500; SD 129 mL). All patients underwent surgery with the intention of modular conversion. The only reason that this was not performed was because it was not possible or deemed to be safe. Therefore, given this scenario, a comparison of the outcomes of the two groups would most likely not be instructive.
Table 1.
Indications for revision
| Indications for revision | |
|---|---|
| Glenoid arthrosis following hemiarthroplasty | 2 (12%) |
| Rotator cuff failure | 10 (59%) |
| Instability | 1 (6%) |
| Trauma | 2 (12%) |
| Other | 2 (12%) |
All outcome scores significantly improved postoperatively. Pain scores improved from a mean of 5.3 (range 0.4 to 8.0) to 2.4 (range 0 to 9.3) (p = .0084). There was an improvement in instability VAS from a mean of 5.2 (range 0 to 10) to 1.1 (range 0 to 6.8) (p = .0006). ASES scores improved from 35.2 (range 20.7 to 61.3) to 65.6 (range 11.8 to 92) (p = 0.0001). There was one complication. One patient experienced transient brachial plexus neuropraxia that resolved after 6 weeks.
Discussion
The purpose of this paper was to examine the feasibility and postoperative outcomes of patients who underwent modular conversions of hemiarthroplasty and TSA to RTSA. In this series, 65.3% of patients were able to be modularly converted. Factors associated with inability to modularly convert were static humeral head subluxation or dislocation, or a preexisting BioModular humeral stem.
The finding that conversion was difficult in the setting of a preexisting BioModular stem is not surprising. The neck-shaft angle of the Comprehensive Reverse is 147°. The neck-shaft angle of the Comprehensive stem is 135° where the neck-shaft angle of the BioModular is 125°. By converting a neck-shaft angle of 125° to 147°, the humerus is distalized thereby putting more tension on the surrounding soft tissues. However, it was still possible to convert a BioModular to a reverse in two instances, so an attempt should be made and the soft tissue tension should be addressed with trialing. Likewise, static humeral head subluxation or dislocation leads to soft tissue contracture which impedes RTSR reduction.
Despite the complex nature of the modular conversion procedure, we found significant improvements in ASES, pain VAS, and instability VAS scores at an average follow-up of 37.4 months. Intraoperative blood loss averaged 225 mL and there was only one intraoperative complication (transient brachial plexus palsy) that resolved spontaneously.
It is clear that failure of an anatomic shoulder arthroplasty presents problematic revision prospects for surgeons. There are inherent advantages to converting a failed hemiarthroplasty or TSA to a RTSA without stem extraction. For example, removing a well-fixed humeral stem can be difficult and necessitate an osteotomy which may be susceptible to malunion, or nonunion. Also, there may be bone loss, periprosthetic facture, and humeral component loosening not to mention increased bleeding and neurovascular complications [6, 9, 23]. Avoiding these complications would be expected to improve postoperative outcomes.
The indications for conversion to RTSA in this study were symptomatic glenoid wear, trauma, instability, and rotator cuff deficiency. There are several causes of instability in prosthetic shoulders. The rate of instability after TSA has been reported to be approximately 4% [10, 22]. Rotator cuff dysfunction is one of the most common causes for instability following a TSA. The failure of the subscapularis leads to the characteristic anterior pattern of instability (Fig. 1) [22]. Of the multiple techniques for taking down the subscapularis (i.e., osteotomy, tenotomy, peel), none has proven to be superior [8, 14–16]. Due to the violation of the subscapularis, some degree of functional loss in the muscle often occurs. Miller et al. found that 67.5 and 66.6% of a cohort of 41 TSA patients had abnormal lift off and belly press tests, respectively [21].
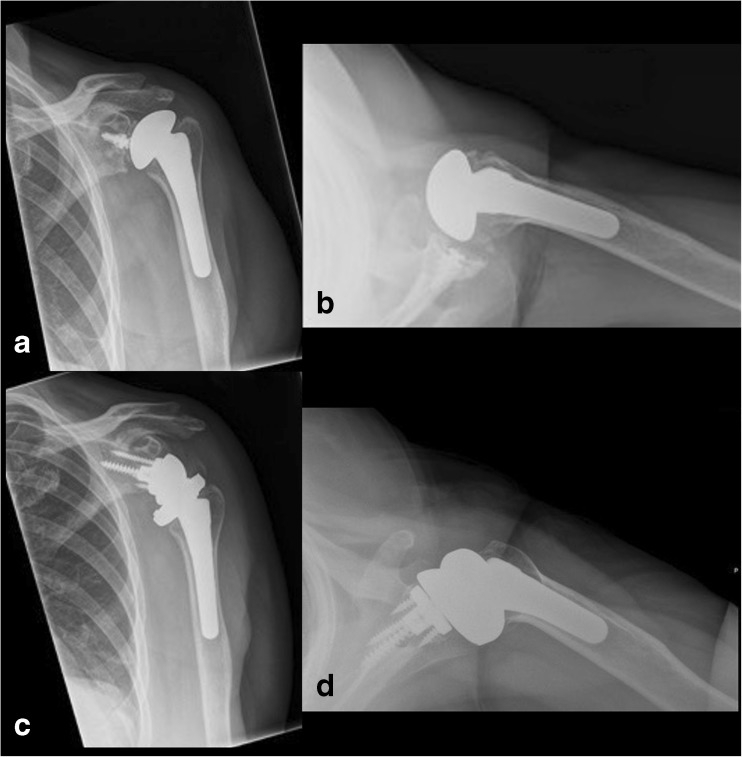
Fig. 1.
Seventy-one-year-old woman presented with anterior instability from failure of the subscapularis 1 year after TSA. Her a AP and b axillary radiographs demonstrate characteristic anterior migration of the humeral component with a well-fixed stem. Following modular conversion to a RTSA, the patient had an excellent functional result and good positioning on the c AP and d axillary radiographs.
Another pattern of postoperative TSA instability is caused by tears of the supraspinatus and infraspinatus. This allows the humeral head to migrate superiorly. Eventually, this instability pattern can lead to glenoid loosening and anterosuperior escape once the coracohumeral arch is violated (Fig. 2). In cases of instability from rotator cuff dysfunction, proper tensioning of the deltoid and soft tissues is paramount in order to achieve the ideal joint compressive forces [12].Similarly, rotator cuff dysfunction with instability was the leading indication for surgery in a modular conversion study by Wieser et al. [27]. They compared a cohort of 13 hemiarthroplasty or TSA patients who retained their stem and 43 patients who had the stem removed at the time of conversion to RTSA. The patients who retained their stem had significantly less intraoperative blood loss, decreased operative time, and fewer complications. Moreover, there were no functional differences between the two groups. Although the study makes a strong argument that stem retention has numerous benefits, an editorial by Chuinard [4] questions the short 38-month duration from the index procedure to the revision. If failure occurred so quickly, the original indication for a hemiarthroplasty or TSA should be reexamined. It is possible that these cases may have been best served by a primary RTSA [4].
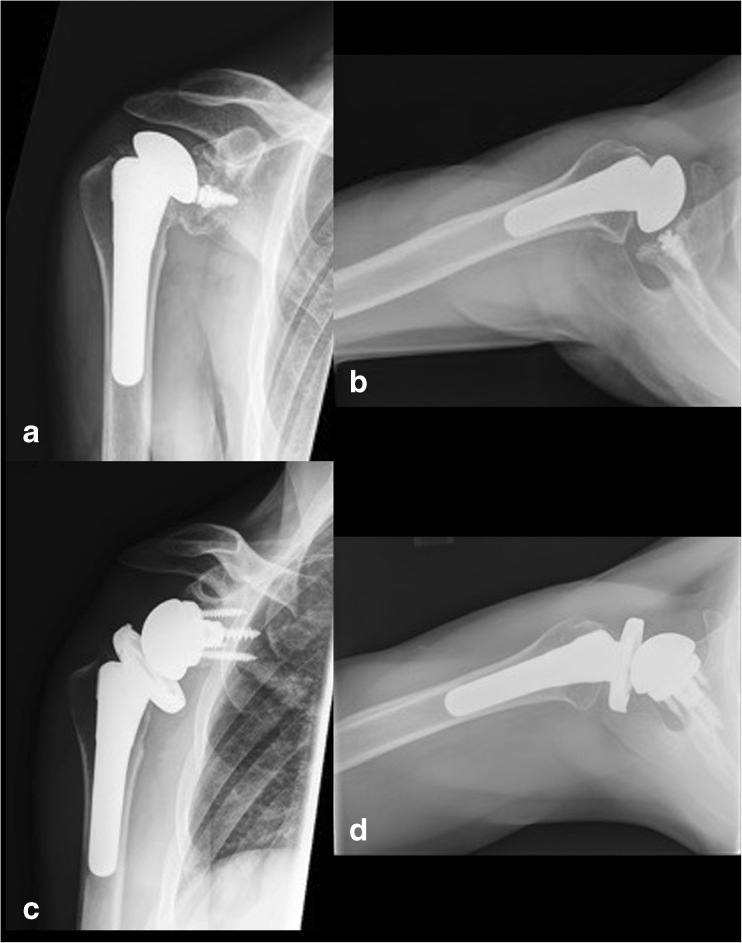
Fig. 2.
Fifty-seven-year-old man presented with anterosuperior escape from subscapularis and supraspinatus tears 1 year after TSA. His a AP and b axillary radiographs demonstrate a well-fixed humeral stem with instability secondary to rotator cuff failure. Following modular conversion to a RTSA, the patient had good functional recovery and good component positioning on the c AP and d axillary radiographs.
Werner et al. studied 14 hemiarthroplasty patients who had revision to RTSA without stem removal and found they had significantly improved function at a mean follow-up of 2.5 years. Mean Constant score improved from 8.9 to 41 points [26]. Patient satisfaction was assessed using a survey and five patients were very satisfied, five patients were satisfied, two patients rated the outcome as fair, and two were disappointed. There were two postoperative complications: one infection and one patient with persistent pain. Interestingly, five cases had positive intraoperative biopsies and joint aspirations which required 6 weeks of antibiotics. Although there was significant functional improvement in this study, 28% of the patients were dissatisfied with their outcome.
It is well-known that there are generally poorer functional results and higher complications in revision RTSA than primary RTSA [3, 11, 25]. However, in a recent retrospective case-control of patients 65 years or younger undergoing RTSA as either a primary or revision arthroplasty procedure, Black et al. [1] found no significant differences between the two groups in postoperative pain, Simple Shoulder Test, and ASES scores. The primary shoulder group reported significantly higher Subjective Shoulder Values than the revision group, and the number of patients who stated that they would have the procedure again approached significance (p = .082). Overall postoperative satisfaction was 81% in the revision group but 94% in the primary group.
This study has several limitations. First, the cohort of 26 patients is small and included both hemiarthroplasty and TSA failures. Second, the indications for revision were heterogeneous with cuff tear as the most common, followed by glenoid arthrosis, trauma, and instability. Third, there was a short follow-up at 37.4 months. Later, complications and further clinical deterioration may not have had sufficient time to manifest during this period. Fourth, preoperative and postoperative physical examination data were not included given variable documentation inherent in a retrospective study. Additionally, formal satisfaction surveys were not administered, so patient expectations were not directly assessed. Lastly, there was no formal radiographic analysis to determine the status of the implant, positioning, and likelihood of failure.
Despite these limitations, this study found that modular conversion is feasible in the majority of patients, and that ASES, pain VAS, and instability VAS scores all improved significantly. Although these positive results are encouraging, it should be emphasized that these procedures are extremely technically demanding and require extensive experience in shoulder reconstruction. The benefit of the modular component design of shoulder systems allows more revision options for complex hemiarthroplasty and TSA failures. Further well-designed studies of modular conversion patients will help determine whether the improvements demonstrated in this study persist over long-term follow-up.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)
Compliance with Ethical Standards
Conflict of Interest
Phillip N. Williams, MD, Samir K. Trehan, MD, and Nicholas Tsouris, BA, have declared that they have no conflict of interest. David M. Dines, MD, reports personal fees from Zimmer Biomet and Thieme Inc., outside the work. Joshua S. Dines, MD, reports personal fees from Arthrex, Conmed Linvate and Trice Medical, outside the work. Lawrence V. Gulotta, MD, reports personal fees from Zimmer Biomet, Inc., outside the work. Edward V. Craig, MD, MPH, reports personal fees from Zimmer Biomet and Wolters-Kluwer Health, outside the work. Russell F. Warren, MD, reports other from BIOMET, during the conduct of the study, and other from BIOMET, outside the work, and receives royalties for a patent with BIOMET.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Investigations performed at the Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, NY.
Level of Evidence: Level IV Retrospective Study
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9546-8) contains supplementary material, which is available to authorized users.
References
- 1.Black EM, Roberts SM, Siegel E, Yannopoulos P, Higgins LD, Warner JJP. Reverse shoulder arthroplasty as salvage for failed prior arthroplasty in patients 65years of age or younger. J Shoulder Elb Surg. 2014;23(7):1036–1042. doi: 10.1016/j.jse.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 2.Bohsali KI, Wirth MA, Rockwood CA. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88(10):2279–2292. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. 2005 Jan;14(1 Suppl S):147S–161S. doi:10.1016/j.jse.2004.10.006. [DOI] [PubMed]
- 4.Chuinard C. CORR Insights®: conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res. 2014;473(2):661–662. doi: 10.1007/s11999-014-4043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fenlin JM, Ramsey ML, Allardyce TJ, Frieman BG. Modular total shoulder replacement. Design rationale, indications, and results. Clin Orthop Relat Res. 1994;307:37–46. [PubMed] [Google Scholar]
- 6.Flury MP, Frey P, Goldhahn J, Schwyzer H-K, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure--midterm results. Int Orthop. 2011;35(1):53–60. doi: 10.1007/s00264-010-0990-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am. 2000;82(1):26–34. doi: 10.2106/00004623-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Giuseffi SA, Wongtriratanachai P, Omae H, Cil A, Zobitz ME, An K-N, et al. Biomechanical comparison of lesser tuberosity osteotomy versus subscapularis tenotomy in total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(8):1087–1095. doi: 10.1016/j.jse.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 9.Gohlke F, Rolf O. [Revision of failed fracture hemiarthroplasties to reverse total shoulder prosthesis through the transhumeral approach: method incorporating a pectoralis-major-pedicled bone window] Operative Orthop\"adie und Traumatologie. 2007;19(2):185–208. doi: 10.1007/s00064-007-1202-x. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez J-F, Alami GB, Baque F, Walch G, Boileau P. Complications of unconstrained shoulder prostheses. J Shoulder Elb Surg. 2011;20(4):666–682. doi: 10.1016/j.jse.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 11.Guery J, Favard L, Sirveaux FCO, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742–1747. doi: 10.2106/JBJS.E.00851. [DOI] [PubMed] [Google Scholar]
- 12.Gutiérrez S, Keller TS, Levy JC, Lee WE, III, Luo Z-P. Hierarchy of Stability Factors in Reverse Shoulder Arthroplasty. Clin Orthop Relat Res. 2008;466(3):670–676. doi: 10.1007/s11999-007-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.13. Hasan SS, Leith JM, Campbell B, Kapil R, Kapil c R, Smith KL, et al. Characteristics of unsatisfactory shoulder arthroplasties. 2002 Sep;11(5):431–441. [DOI] [PubMed]
- 14.Jandhyala S, Unnithan A, Hughes S, Hong T. Subscapularis tenotomy versus lesser tuberosity osteotomy during total shoulder replacement: a comparison of patient outcomes. J Shoulder Elbow Surg. 2011;20(7):1102–1107. doi: 10.1016/j.jse.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 15.Lapner PLC, Sabri E, Rakhra K, Bell K, Athwal GS. Healing rates and subscapularis fatty infiltration after lesser tuberosity osteotomy versus subscapularis peel for exposure during shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(3):396–402. doi: 10.1016/j.jse.2012.05.031. [DOI] [PubMed] [Google Scholar]
- 16.Lapner PLC, Sabri E, Rakhra K, Bell K, Athwal GS. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg. 2012;94(24):2239–2246. doi: 10.2106/JBJS.K.01365. [DOI] [PubMed] [Google Scholar]
- 17.Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007;89(2):292–300. doi: 10.2106/JBJS.E.01310. [DOI] [PubMed] [Google Scholar]
- 18.Lo IKY, Litchfield RB, Griffin S, Faber K, Patterson SD, Kirkley A. Quality-of-life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis. A prospective, randomized trial. J Bone Joint Surg Am. 2005;87(10):2178–2185. doi: 10.2106/JBJS.D.02198. [DOI] [PubMed] [Google Scholar]
- 19.Melis B, Bonnevialle N, Neyton L. L e vigne C, Favard L, Walch G, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21(3):342–349. doi: 10.1016/j.jse.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 20.Mighell MA, Kolm GP, Collinge CA, Frankle MA. Outcomes of hemiarthroplasty for fractures of the proximal humerus. J Shoulder Elb Surg. 2003;12(6):569–577. doi: 10.1016/S1058-2746(03)00213-1. [DOI] [PubMed] [Google Scholar]
- 21.Miller BS, Joseph TA, Noonan TJ, Horan MP, Hawkins RJ. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elb Surg. 2005;14(5):492–496. doi: 10.1016/j.jse.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 22.Moeckel BH, Altchek DW, Warren RF, Wickiewicz TL, Dines DM. Instability of the shoulder after arthroplasty. J Bone Joint Surg Am. 1993;75(4):492–497. doi: 10.2106/00004623-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Sperling JW, Hawkins RJ, Walch G, Zuckerman JD. Complications in Total Shoulder Arthroplasty. J Bone Joint Surg Am. 2013;95(6):563–569. doi: 10.2106/00004623-201303200-00012. [DOI] [PubMed] [Google Scholar]
- 24.Teschner H, Albrecht U-V, Meller R, Liodakis E, Wiebking U, Krettek C, et al. Conversion of hemi into reverse shoulder arthroplasty: implant design limitations. Arch Orthop Trauma Surg. 2014;134(12):1683–1689. doi: 10.1007/s00402-014-2098-1. [DOI] [PubMed] [Google Scholar]
- 25.Wall B, Nove Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 26.Werner BS, Boehm D, Gohlke F. Revision to reverse shoulder arthroplasty with retention of the humeral component. Acta Orthop. 2013;84(5):473–478. doi: 10.3109/17453674.2013.842433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wieser K, Borbas P, Ek ET, Meyer DC, Gerber C. Conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res. 2014;473(2):651–660. doi: 10.1007/s11999-014-3985-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Young AA, Walch G, Pape G, Gohlke F, Favard L. Secondary rotator cuff dysfunction following total shoulder arthroplasty for primary glenohumeral osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg. 2012;94(8):685–693. doi: 10.2106/JBJS.J.00727. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1225 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1225 kb)