Abstract
The etiology of chronic fatigue syndrome (CFS) is unknown and no conventional medicine therapies are available. This report presents a clinical case of a patient suffering from CFS who was cured by traditional Korean medicine. A 33-year-old female patient had to take time off work because of terrible fatigue symptoms that did not respond to conventional treatments. Her disorder was significantly reduced by herbal medicine, acupuncture, and moxibustion. Changes in fatigue severity were evaluated using a visual analog scale (VAS) and a numerical rating scale (NRS). NRS and VAS scores decreased from 70 and 8.1 to 37 and 3.7, respectively, during 3 months. This case reveals the therapeutic potential of traditional Korean medicine for CFS and fatigue-associated disorders.
Keywords: chronic fatigue syndrome, herbal drug, Korean medicine, moxibustion
1. Introduction
Chronic fatigue syndrome (CFS) is defined as severe fatigue accompanied by other fatigue-associated specific symptoms lasting over 6 months.1 CFS is the most severe condition involving unexplained chronic fatigue, and patients are faced with a debilitating illness leading to serious changes in physical, mental, and occupational wellbeing, and often social isolation.2, 3 CFS reduces the workforce productivity of individuals by 54%.4 However, there is still a lack of adequate recognition of the importance of CFS. CFS has also been termed myalgic encephalomyelitis to arouse attention regarding this health problem and related research.5
The worldwide prevalence of chronic fatigue and CFS is estimated at approximately 10% and 1% of the general population, respectively,6 and 0.6–2% in Korea from studies of individuals who attended hospitals for medical examination.7 Several hypotheses have been proposed for the pathogenesis of CFS, such as oxidative stress, hypothalamic–pituitary–adrenal (HPA) axis abnormality, and immune dysfunction.8, 9, 10 However, the etiology of CFS is still unclear, and no objective diagnosis methods or effective therapies exist in conventional medicine.11, 12 Thus, patients suffering from CFS often rely on complementary and alternative medicine.13
In traditional Korean medicine, CFS is considered as imbalanced interorgan functions or Qi and Blood, two essential components in human body, and herbal drugs have traditionally been the major treatments for CFS or chronic fatigue-related disorders.14 Anti-fatigue effects in CFS patients have been demonstrated for several herbal remedies and acupuncture.15, 16
This study presents the case of a patient who was cured of serious CFS by traditional Korean medicine including moxibustion, acupuncture, and herbal drugs.
2. Case report
2.1. Patient characteristics and medical history
A 33-year-old woman attended an Oriental hospital with severe and persisting fatigue over 3 years. Six months before the visit, her fatigue-associated symptoms became extremely serious, which led her to take time off work as a government employee. She complained of complex symptoms, including indigestion, anorexia, frequent sighing, and easy exhaustion. The patient had previously taken Western drugs for treatment of vaginitis for 1 day and then became totally exhausted, leading to hospitalization for 7 days. No specific abnormality was observed in blood tests, radiographic inspection, endoscopy, and a psychological consult.
Because of the lack of response to various conventional treatments and medical examinations, the patient chose traditional Korean medicine as a cure for her disorder. The patient had not drunk alcohol or smoked and had not been under psychological stress. She had no specific family or past history of diseases including hypertension, diabetes mellitus, fatty liver, or hyperlipidemia. She had a slightly low weight, with a body mass index of 19.5.
2.2. Diagnosis and outcome evaluation
The patient's symptoms matched the criteria for CFS diagnosis according to the guidelines of the Centers for Disease Control and Prevention (CDC).17 She had never been diagnosed with CFS in any previous clinic or hospital visits. The symptom differentiation was Blood deficiency of heart and spleen according to her general symptoms, such as susceptibility to digestive disorders, cold hands and feet, easy tension, and high sensitivity to stress environments since a young age. Her Sasang constitutional classification was Soumin according to Questionnaire for the Sasang Constitution Classification II (QSCCII).
To assess changes in fatigue severity, a numerical rating scale (NRS) and visual analog scale (VAS) were used. The NRS score was measured using the Korean-translated Chalder fatigue severity questionnaire consisting of seven physical health and four mental health questions.18 Each item was scored by the patient on a 10-point scale (0 = not at all to 9 = unbearably severe condition). For the VAS score, the patient was asked to indicate her feeling of fatigue by marking a position on a 10-cm line.
2.3. Treatment and course of symptoms
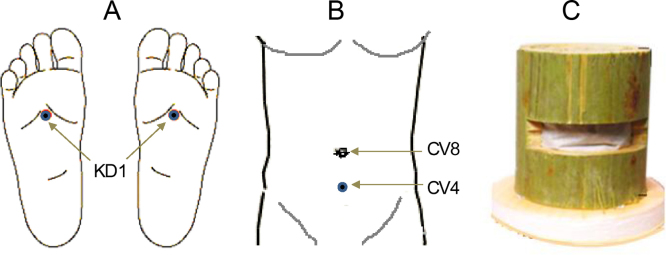
The patient was cared for as an inpatient for 7 days and an outpatient for 3 months. During hospitalization, she was administered herbal drugs (Samchulgunbitang and Myelophil, Table 1) and was treated with salt-indirect moxibustion on three acupoints (KD1, CV4 and CV8; Fig. 1) using moxa corn from KyeGoo Inc. (Incheon, South Korea) and acupuncture (mainly at HT7, LI4, and SP3). Thereafter, she visited the clinic monthly and took only Myelophil continuously.
Table 1.
Composition of prescribed drugs.
| Drug | Component and composition (g) |
|---|---|
| Myelophil | Astragali Radix (10), Salviae Radix (10) |
| Samchulgunbitang | Ginseng Radix (12), Atractylodis Macrocephalae Rhizoma (12), Hoelen (12), Diosoreae Radix (12), Glycyrrhizae Radix (12), Coicis Semen (6), Nelumbo Semen (6), Platicodi Radix (6), Amomi Semen (6), Dolichi Semen (6), Zingibeberis Rhizoma (4), Zizyhpi Fructus (2) |
Fig. 1.
Acupoints. (A,B) Acupoints for moxibustion and (C) picture of moxa corn.
After a 7-day hospitalization, the patient had recovered from complete exhaustion and subjectively reported a notable improvement in fatigue-related symptoms. Her NRS and VAS scores changed from 70 and 8.1 to 58 and 6.2, respectively (Table 2). Moreover, the severe anorexia moderately was improved, and then discharged. As an outpatient, she visited the clinic once a month, and had taken only Myelophil with treatments of moxibustion and acupuncture on visiting day. Over 3 months, her NRS and VAS scores significantly improved to 37 and 3.7, respectively, and the patient regained confidence regarding her physical health and mental attitude.
Table 2.
Changes in NRS and VAS scores.
| Question | Inpatient |
Outpatient | |
|---|---|---|---|
| Day 0 | Day 7 | Day 97 | |
| 1. How tired do you feel? | 7 | 6 | 3 |
| 2. How strongly do you currently feel the need to rest? | 8 | 6 | 3 |
| 3. How sleepy or drowsy do you feel? | 5 | 4 | 2 |
| 4. Do you have problems starting things? | 6 | 6 | 5 |
| 5. Do you lack energy? | 7 | 6 | 3 |
| 6. Do you have less muscle strength? | 8 | 5 | 3 |
| 7. Do you feel weak? | 8 | 6 | 4 |
| 8. Do you have difficulty concentrating? | 5 | 5 | 3 |
| 9. Do you have problems thinking clearly? | 4 | 4 | 3 |
| 10. Do you make slips of the tongue when speaking? | 5 | 4 | 4 |
| 11. How is your memory? | 7 | 6 | 5 |
| Total NRS score | 70 | 58 | 37 |
Please mark a position on the line below to indicate how you are feeling 
|
8.1 | 6.2 | 3.7 |
3. Discussion and conclusion
To date, conventional medicine has no therapeutics or drugs for treating CFS.18 Many patients suffering from CFS chose traditional Korean medicine after repeated examinations in hospital, like the patient in this case study. There were no specific factors regarding her social and familial environments or her physical and psychological status affecting her fatigue. Recent 1-day antibiotic use for vaginitis might have triggered exacerbation of her fatigue symptoms, after which the patient decided to take a 1-year leave of absence from her job because of the severity of her condition.
The patient received inpatient treatment consisting of herbal drugs, moxibustion, and acupuncture on a daily basis. Samchulgunbitang and Myelophil were prescribed based on the patient's symptom differentiation. Samchulgunbitang is composed of 12 herbs, and has been traditionally used for the patients with anorexia and digestive disorders.19 Myelophil is composed of Astragali Radix and Salviae Radix (used to treat Qi and Blood in traditional medicine) and has shown antifatigue effects in a clinical study.20 The main symptoms of anorexia and severe fatigue improved during inpatient treatment, and the patient took only Myelophil during outpatient treatment. An animal study revealed antioxidant effects, especially on stress-induced brain oxidative injury;21 brain oxidative stress is known to be linked to CFS.22
The patient complained of weakness of the digestive system, cold hands and feet, and easy tension related to stressful environments since a young age. Her symptom differentiation was Blood deficiency of heart and spleen and a Soumin Sasang constitution. According to this characterization, moxibustion and acupuncture were used to treat the patient. Moxibustion improves chronic pathological conditions associated with deficiency and coldness.23 The patient was treated with salt-based indirect moxibustion at KI1, CV4, and CV8, which are traditionally used in treating diverse fatigue-associated disorders.24 A clinical trial reported anti-fatigue effects of indirect moxibustion at CV4 and CV8 in patients with idiopathic chronic fatigue.25 Acupuncture treatment was performed at HT7, LI4, and SP3 to control the balance of spleen and kidney according to Sasang medicine. The patient's fatigue severity and associated symptoms gradually improved over a period of 3 months.
Diagnosis of CFS was the first for this patient, despite frequent visits to conventional hospitals. This might result from the mainly paying attention to identify the possible causes of chronic fatigue rather than diagnosis of CFS in medical practice. This case demonstrates that traditional Korean medicine could help patients with CFS. This may be because the comprehensive treatment strategy in traditional Korean medicine addresses the complex pathogenesis of CFS.
In summary, this report provides useful information on the potential of traditional Korean medicine for CFS treatment. Further study is needed to evaluate the therapeutic effects on CFS in randomized clinical trials.
Conflicts of Interest
None.
Acknowledgments
This study was supported by a grant from the Oriental Medicine R&D Project, Ministry of Health & Welfare (B100045), Republic of Korea.
References
- 1.Moss-Morris R., Deary V., Castell B. Chronic fatigue syndrome. Handb Clin Neurol. 2013;110:303–314. doi: 10.1016/B978-0-444-52901-5.00025-3. [DOI] [PubMed] [Google Scholar]
- 2.Wyller V.B. The chronic fatigue syndrome—an update. Acta Neurol Scand Suppl. 2007;187:7–14. doi: 10.1111/j.1600-0404.2007.00840.x. [DOI] [PubMed] [Google Scholar]
- 3.Schweitzer R., Kelly B., Foran A., Terry D., Whiting J. Quality of life in chronic fatigue syndrome. Soc Sci Med. 1995;41:1367–1372. doi: 10.1016/0277-9536(95)00124-p. [DOI] [PubMed] [Google Scholar]
- 4.Reynolds K.J., Vernon S.D., Bouchery E., Reeves W.C. The economic impact of chronic fatigue syndrome. Cost Eff Resour Alloc. 2004;2:4. doi: 10.1186/1478-7547-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharpe M. The report of the Chief Medical Officer's CFS/ME working group: what does it say and will it help? Clin Med. 2002;2:427–429. doi: 10.7861/clinmedicine.2-5-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reeves W.C., Jones J.F., Maloney E., Heim C., Hoaglin D.C., Boneva R.S. Prevalence of chronic fatigue syndrome in metropolitan, urban, and rural Georgia. Popul Health Metr. 2007;5:5. doi: 10.1186/1478-7954-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Son C.G. Review of the prevalence of chronic fatigue worldwide. J Korean Oriental Med. 2012;33:25–33. [Google Scholar]
- 8.Logan A.C., Wong C. Chronic fatigue syndrome: oxidative stress and dietary modifications. Altern Med Rev. 2001;6:450–459. [PubMed] [Google Scholar]
- 9.Papadopoulos A.S., Cleare A.J. Hypothalamic–pituitary–adrenal axis dysfunction in chronic fatigue syndrome. Nat Rev Endocrinol. 2011;8:22–32. doi: 10.1038/nrendo.2011.153. [DOI] [PubMed] [Google Scholar]
- 10.Rosenblum H., Shoenfeld Y., Amital H. The common immunogenic etiology of chronic fatigue syndrome: from infections to vaccines via adjuvants to the ASIA syndrome. Infect Dis Clin North Am. 2011;25:851–863. doi: 10.1016/j.idc.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Jorgensen R. Chronic fatigue: an evolutionary concept analysis. J Adv Nurs. 2008;63:199–207. doi: 10.1111/j.1365-2648.2008.04649.x. [DOI] [PubMed] [Google Scholar]
- 12.Martin A., Chalder T., Rief W., Braehler E. The relationship between chronic fatigue and somatization syndrome: a general population survey. J Psychosom Res. 2007;63:147–156. doi: 10.1016/j.jpsychores.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Adams D., Wu T., Yang X.S., Yang X., Tai S., Vohra S. Traditional Chinese medicinal herbs for the treatment of idiopathic chronic fatigue and chronic fatigue syndrome. Cochrane Database Syst Rev. 2009:CD006348. doi: 10.1002/14651858.CD006348.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Kwak K.K., Cho J.H., Son C.G. Study on chronic fatigue syndrome from Oriental medicine point of view. J Korean Oriental Med. 2008;29:962–969. [Google Scholar]
- 15.Sekiya N., Shimada Y., Shintani T., Tahara E., Kouta K., Shibahara N. Reduction of perception of chronic fatigue in an observational study of patients receiving 12 weeks of Kampo therapy. J Altern Complement Med. 2005;11:895–901. doi: 10.1089/acm.2005.11.895. [DOI] [PubMed] [Google Scholar]
- 16.Lijue Z. Acupuncture and Chinese patent drugs for treatment of chronic fatigue syndrome. J Tradit Chin Med. 2005;25:99–101. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Chronic fatigue syndrome. CDC Website. http://www.cdc.gov/cfs/diagnosis/index.html. Published 2012. Accessed January 7, 2013.
- 18.Morriss R.K., Wearden A.J., Mullis R. Exploring the validity of the Chalder Fatigue Scale in chronic fatigue syndrome. J Psychosom Res. 1998;45:411–417. doi: 10.1016/s0022-3999(98)00022-1. [DOI] [PubMed] [Google Scholar]
- 19.Kim T.G., Ko S.G., Baik T.H. An experimental study on the effect of Samchulgunbitang affecting gastro-intestine and central nervous system. J Korean Oriental Int Med. 1997;18:1–14. [Google Scholar]
- 20.Cho J.H., Cho C.K., Shin J.W., Son J.Y., Kang W., Son C.G. Myelophil, an extract mix of Astragali Radix and Salviae Radix, ameliorates chronic fatigue: a randomised, double-blind, controlled pilot study. Complement Ther Med. 2009;17:141–146. doi: 10.1016/j.ctim.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Lee J.S., Kim H.G., Han J.M., Lee J.S., Son S.W., Ahn Y.C. Myelophil ameliorates brain oxidative stress in mice subjected to restraint stress. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39:339–347. doi: 10.1016/j.pnpbp.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 22.Jason L.A., Sorenson M., Porter N., Belkairous N. An etiological model for myalgic encephalomyelitis/chronic fatigue syndrome. Neurosci Med. 2011;2:14–27. doi: 10.4236/nm.2011.21003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park H.J., Son C.G. Overview for moxibustion-related researches worldwide. J Meridian Acupoint. 2008;25:167–174. [Google Scholar]
- 24.Han C.H., Shin M.S., Kang K.W., Kang B.G., Park S.H., Choi S.M. An in-depth interview for use of moxibustion therapy in Korea. J Meridian Acupoint. 2008;25:85–97. [Google Scholar]
- 25.Kim H.G., Yoo S.R., Park H.J., Son C.G. Indirect moxibustion (CV4 and CV8) ameliorates chronic fatigue: a randomized, double-blind, controlled study. J Altern Complement Med. 2012;18:1–7. doi: 10.1089/acm.2011.0503. [DOI] [PMC free article] [PubMed] [Google Scholar]