Abstract
The objectives of this study were to summarize the curriculum, history, and clinical researches of Chuna in Korea and to ultimately introduce Chuna to Western medicine. Information about the history and insurance coverage of Chuna was collected from Chuna-related institutions and papers. Data on Chuna education in all 12 Korean medicine (KM) colleges in Korea were reconstructed based on previously published papers. All available randomized controlled trials (RCTs) of Chuna in clinical research were searched using seven Korean databases and six KM journals. As a result, during the modern Chuna era, one of the three periods of Chuna, which also include the traditional Chuna era and the suppressed Chuna era, Chuna developed considerably because of a solid Korean academic system, partial insurance coverage, and the establishment of a Chuna association in Korea. All of the KM colleges offered courses on Chuna-related subjects (CRSs); however, the total number of hours dedicated to lectures on CRSs was insufficient to master Chuna completely. Overall, 17 RCTs were reviewed. Of the 14 RCTs of Chuna in musculoskeletal diseases, six reported Chuna was more effective than a control condition, and another six RCTs proposed Chuna had the same effect as a control condition. One of these 14 RCTs made the comparison impossible because of unreported statistical difference; the last RCT reported Chuna was less effective than a control condition. In addition, three RCTs of Chuna in neurological diseases reported Chuna was superior to a control condition. In conclusion, Chuna was not included in the regular curriculum in KM colleges until the modern Chuna era; Chuna became more popular as the result of it being covered by Korean insurance carriers and after the establishment of a Chuna association. Meanwhile, the currently available evidence is insufficient to characterize the effectiveness of Chuna in musculoskeletal and neurological diseases.
Keywords: Chuna manual medicine, clinical research, education, history, insurance coverage, Korea
1. Introduction
Traditional medicine (TM) is defined as indigenous medical practices that are used to maintain health and prevent, diagnose, and treat physical and mental illnesses differently than allopathic medicine based on theories, beliefs, and experiences.1 In East Asian countries, especially China, Korea, and Japan, the main therapeutic TM practices are acupuncture, moxibustion, cupping, herbal medicines, and manual therapies (called Tuina in China, Chuna in Korea, and Anma-massage-Shiatsu and Judo therapy in Japan).2
Chuna is a therapeutic modality that addresses biomechanical function, pathology, diagnostics, and theories related to treatment in order to create a balance in orthopedic structure and function; Chuna states that both function and structure are systemically correlated.3 Chuna techniques include stimulation of the meridian system, correcting displacement of the osteoarticular structure, and prescribing exercises based on patient-reported symptoms and the results of a functional anatomical assessment.4 Representative techniques of Chuna are thrust, mobilization, distraction of the spine and joints, soft tissue release, visceral manipulation, craniosacral therapy, and the diaplasis technique. These techniques were developed by combining aspects of Chinese Tuina, Japanese Shiatsu, and chiropractic and osteopathic medicine from the United States.5
In Korea, there are 11 private Korean medicine (KM) colleges and one national school of KM that offer Chuna as part of the KM curriculum.6 Most KM doctors use Chuna to treat imbalances of the human body, relieve various types of pain, increase relaxation in patients by manipulating specific body parts (e.g., acupoints on the skin, myofascial trigger points, the spine and joints).7
Although Chuna is currently widely used by many KM doctors to treat patients in Korea, most foreign health and medical service providers are unaware of Chuna because few papers regarding its use are disseminated to the Western medical community.3, 8, 9
Therefore, information about Chuna education, its history, and effectiveness (in Korean literature) must be summarized and introduced to Western medicine.
2. Methods
2.1. Data sources
2.1.1. Data on the history of Chuna and its coverage by insurance carriers
The insurance coverage of Chuna in Korea was investigated using official documents collected from the Korean Society of Chuna Manual Medicine for Spine and Nerves (KSCMM), a KM association, and the website of the Health Insurance Review and Assessment Service, a national institution in Korea.10
Information about the history of Chuna in Korea was obtained from Chuna-related papers,11, 12, 13 books,14 and the KSCMM website.7
2.1.2. Data on the curriculum of Chuna-related subjects
A study by Park and Shin6 investigated the curriculum of Chuna-related subjects (CRSs) in Korea by collecting information from the 11 private KM colleges and the national school of KM in Korea with support from the KSCMM. After obtaining consent from these authors, we reexamined, reconstructed, and translated the contents of the study.
2.1.3. Data on clinical research of Chuna
A survey of the electronic literature was conducted in April 2013 using seven Korean databases (Korean Studies Information, DBpia, the Korea Institute of Science and Technology Information, the Research Information Service System, KoreaMed, the National Assembly Library, and the Oriental Medicine Advanced Searching Integrated System). The search terms were “Chuna” or “manipulation.” We also manually searched six KM journals, which include the Journal of Oriental Rehabilitation Medicine, the Journal of Korean Chuna Manual Medicine for Spine and Nerves, the Journal of Korean Acupuncture and Moxibustion, the Korean Journal of Meridian and Acupoint, the Journal of Oriental Medicine, and the Korean Journal of Physiology and Pathology (searched from their inception to April 2013).
Prospective randomized clinical trials (RCTs) related to Chuna for any types of diseases were included for analysis. The main outcome measure was pain reduction in clinical studies of musculoskeletal diseases, and improvement of neurological symptoms in neurological diseases. The overall result was classified as either (1) positive when Chuna was significantly more effective than the control condition in at least one of the outcome measures, (2) neutral when there was no significant difference between Chuna and the control condition, or (3) negative when Chuna was significantly less effective than the control condition. Results with p < 0.05 were considered statistically significant.
Trials were eligible for inclusion if Chuna was the sole treatment or an adjunct to other treatment. Control conditions were no treatment, drug treatment, and any other type of intervention. We excluded non-RCTs, uncontrolled observational studies, and case studies. Data screening, selection, and extraction were conducted by four independent reviewers (T.-W.M., T.-.Y.C., Y.-S.K., and J.-H.L.) and verified by another author (B.-C.S.). Hard copies of all the selected articles were obtained and read in full. Disagreements between raters were resolved through discussion between the coauthors as necessary.
Four authors (T.-Y.P., D.-C.C., E.-H.H., and K.-H.H.) extracted the data systematically using predefined standardized criteria according to the medical condition, treatment interventions, main outcome measure, intergroup differences, and authors’ conclusions. An assessment of each study's quality was conducted by two reviewers (T.-Y.P. and T.-W.M.) and was based on the Cochrane risk of bias criteria, including random sequence generation, allocation concealment, patient blinding, assessor blinding, reporting dropout or withdrawal, and selective outcome reporting.
3. Results and discussion
3.1. History and insurance coverage of Chuna
Physical manipulation of the body has been used to cure human ailments since ancient times. Although its origins remain unclear, manual procedures are evident in Thai artwork dating back as far as 4000 years.7 The history of Chuna is divided into the following three periods: the traditional Chuna era (ancient times through 1945), the suppressed Chuna era (1945 through the 1980s), and the modern Chuna era (the 1990s through the present). The history of Chuna and its coverage by insurance carriers are fully explained in Table 1. No Anma or Chuna-related publications existed during the traditional Chuna era. However, some books (Eui-Bang-Yoo-Chui, Hwal-In-Sim-Bang, and Dong-Eui-Bo-Gam) recorded Tao Yin, Anma, and Angyo as health-preservation techniques without using Chuna-related terminology.11 During the Japanese colonial era (the suppressed Chuna era), Anma was permitted only for the blind. In the modern Chuna era, Chuna-related terminology appeared for the first time, and Chuna techniques that had historically been handed down to others by individuals or groups were integrated to develop the Chuna practice. In 1991, the KSCMM was launched and the Ministry of Health and Society legalized Chuna14 (Chuna manual therapy is a type of traditional KM, and some of Chuna methods are similar or identical to chiropractic techniques. KM doctors may even use a chiropractic table when applying Chuna to patients) in 1994. Since 1995, Chuna has been accepted as an official part of the curriculum in KM colleges. Furthermore, the journal of the KSCMM has been published biannually since 2000.15 In 2002, Chuna was approved as a nonpayment item10 by the National Health Insurance, and in 2005, it was approved for coverage by automobile insurance.16
Table 1.
History and insurance coverage of Chuna.
| Era | Years | History | Insurance coverage or historical characteristic | Remark | |
|---|---|---|---|---|---|
| Traditional Chuna era | In 1445, during the Joseon dynasty | Eui-Bang-Yoo-Chui addressed Tao Yin *, Anma † | No Anma or Chuna-related specialty publication existed. Regarding Chuna-related subjects, the term Tao Yin appeared in a health preservation-related book. |
Chuna was passed down by individuals or specific practitioner groups. | The terms Anma and Angyo ‡ were coused before the Ming dynasty. The terms Chuna and Anma were coused during the Ming dynasty. Since the Qing dynasty, the term Chuna has been used to describe the integrated practice of these and other related terms. |
| Approximately 1550 | Hwal-In-Sim-Bang described Tao Yin | ||||
| In 1610 | Dong-Eui-Bo-Gam addressed Tao Yin, Anma, Angyo The evolution of manipulation therapy was hampered by a conservative social atmosphere. |
||||
| During Japanese colonial era (1910–1945) |
Chuna was regarded as a set of folk remedies rather than a manipulation therapy. | Anma was taught to the blind as a form of vocational education | |||
| Suppressed Chuna era | From 1945 to the 1980s | The evolution of Chuna training courses was hampered. | Anma was permitted only for blind practitioners. | ||
| Modern Chuna era | 1991 | The Korean Society of Chuna Manual Medicine for Spine and Nerves was established. | Chuna practices that were traditionally passed down by individuals or groups were formally integrated. | Chuna continues to develop by integrating aspects of Chinese Tuina, American chiropractic and osteopathy, and Japanese-style manual manipulation. | |
| 1992 | The Korean Society of Chuna Manual Medicine for Spine and Nerves was officially approved as a subsociety of Korean Medicine. | ||||
| 1994 | The Ministry of Health and Society viewed Chuna favorably | Official definition of Chuna by the Ministry of Health and Society was provided in 1994 | |||
| 1995 | Chuna was accepted as part of the curriculum of the Korean Medicine college of Kyung Hee University. | - - |
|||
| 1996 | The first training course of Chuna was launched. | ||||
| 2000 | The journal of the Korean Society of Chuna Manual Medicine for Spine and Nerves was published for the first time. | - | |||
| 2002–2011 | Chuna was accepted as part of the curricula in most Korean medical colleges except the Dongguk Korean Medical College. Chuna educational textbooks were published for the first time in 2002, then in 2006 and 2011. | Chuna was approved as a nonpayment item by National Health Insurance in 2002 | |||
| Chuna was approved for covered by automobile insurance carriers in 2005. | |||||
| Chuna was included as a subdirectory of KM physical therapy, and again approved as a nonpayment item by National Health Insurance in 2011. | |||||
| 2013 | The first Chuna training course extended to the 19th. | - |
* Tao Yin is a series of exercises practiced by Taoists to cultivate chi, the internal energy of the body according to the TKM theory.
† Anma is thought to be of Chinese origin, developing from Tuina. Henceforward, Anma was introduced into Korea and Japan from China. Anma practitioners use common massage techniques such as kneading, rubbing, tapping, and shaking. These methods are directed to specific vital points and meridians on the body.
‡ Angyo is another name of Anma in Korea.
KM, Korean medicine.
Traditional Chuna therapy resulted from various clinical experiences, but modern Chuna, which basically is based on traditional Chuna, represents the combination of traditional practice and modern scientific knowledge in fields such as anatomy, physiology, and pathology.11, 12, 13 Chuna has evolved by integrating aspects of Chinese Tuina, American chiropractic and osteopathy, and Japanese manipulation techniques.14
3.2. Education of CRSs in Korea
All of the KM colleges in Korea (11 private colleges and 1 national college) were found to include CRSs in their curricula. Generally, CRS included Chuna, oriental rehabilitation medicine (ORM), and musculoskeletal oriental medicine (MOM). A detailed CRS curriculum for each KM college is presented in Table 2. Of the 12 colleges, eight belonged to Classification I, which meant that the curriculum contained an independent Chuna lecture that was not merged with ORM or MOM. The remaining colleges belonged to Classification II, which meant that the Chuna lecture was merged with ORM or MOM. It is very important for KM colleges to be equipped with CRS courses pertaining to its practice and theory as opposed to general clinical practice (GCP). The CRS practice should not be included as a part of GCP training because manual therapies such as Chuna require specific training. The CRS in three of the KM colleges was offered as an elective, but in the remaining nine schools, CRS was a mandatory subject. The total number of lecture units allocated to CRS (A) ranged from four to eight, whereas the total number of lecture units (B) ranged from 172 to 273 units in the entire 6-year curriculum. The ratio of A to B (less than 3.33 over the entire curriculum) is too small; at least 30 subjects are included in the curricula of KM colleges. This deficiency is striking, especially when compared with the World Health Organization (WHO) manipulation guidelines,17 which require a total of 4465 hours over 4 years of full-time study. To compensate for the shortage of CRS lessons in the KM curriculum, the KSCMM annually offers a Chuna training course (approximately 126 hours for 1 year15) for KM doctors. In the near future, a specialized curriculum that has a sufficient number of lesson hours devoted to Chuna must be established.
Table 2.
Education on Chuna-related subjects for all 12 colleges in Korea.
| College | Subject | Establishment of Chuna lectures | Chuna lectures merged with ORM or MOM | Existence of CRS practice lectures | MS/SS | Total lecture units of CRS (A) | Total lecture units of other subjects for 6 years of KM education (B) | A/B (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Classification | KHC | Chuna Chuna and practice ORM ORM and practice |
Y | N | Y | MS | 7 | 242.5 | 2.88 |
| GCC | Chuna 1,2 ORM 1,2,3,4 GCP 2,3 |
Y | N | N | MS | 6 (16) | 238 | 2.52 | |
| DEC | Chuna 1,2 ORM ORM and practice |
Y | N | Y | MS | 6 | 240 | 2.5 | |
| DSC | Chuna and practice ORM GCP |
Y | N | Y | MS | 7 (11) | 240 | 2.91 | |
| DHC | ORM and practice 1,2,3,4 Chuna and practice |
Y | N | Y | MS | 5 | 240 | 2.08 | |
| DJC | Chuna ORM 1,2,3,4 GCP 1,2,3,4 |
Y | N | N | SS | 6 (16) | 240 | 2.5 | |
| WSC | Chuna and practice 1,2 ORM GCP 2,3 |
Y | N | Y | SS MS MS |
8 (18) | 240 | 3.33 | |
| WKC | Chuna ORM 1,2 ORM and practice 1,2 |
Y | N | Y | SS MS MS |
6.5 | 240 | 2.70 | |
| Classification | PNU | MOM 1,2 MOM and practice 1,2 |
N | Y | N | MS | 4 (25) | 172 | 2.32 |
| DGC | ORM 1,2 ORM practice 1,2 |
N | Y | Y | MS | 4 | 240 | 1.66 | |
| SJC | ORM 1 ORM 2 ORM practice 1,2 |
N | Y | N | MS | 4 (19) | 273 | 1.46 | |
| SMC | ORM ORM practice |
N | Y | Y | MS | 6 | 240 | 2.5 |
The numbers enclosed in parenthesis appearing in the A column (Total lecture units of CRS) refer to the total lecture units of CRS including GCP lecture units. Classification I includes an independent Chuna lecture that is not combined with ORM or MOM. However, in Classification II, there is no independent Chuna lecture.
CRS, Chuna-related subjects-CRS included Chuna, ORM, and MOM; DEC, Dong-Eui Korean Medical College; DGC, Dongguk Korean Medical College; DHC, Daegu Haany Korean Medical College; DJC, Daejeon Korean Medical College; DSC, Dong-Shin Korean medical college; GCC, Gachon Korean Medical College; GCP, general clinical practice-GCP includes Chuna practice as part of general clinical practice; KHC, Kyung Hee Korean Medical College; KM, Korean medicine; MOM, musculoskeletal oriental medicine-MOM has includes portions of a Chuna lecture; MS, mandatory subject; N, No; ORM, oriental rehabilitation medicine; PNU, Pusan National University of school of Korean Medicine; SJC, Sangji Korean Medical College; SMC, Se-Myeong Korean Medical College; SS, Selective subject; WKC, Wonkwang Korean Medical College; WSC, Woo-suk Korean Medical College; Y, Yes.
3.3. Clinical studies of Chuna
3.3.1. Study description
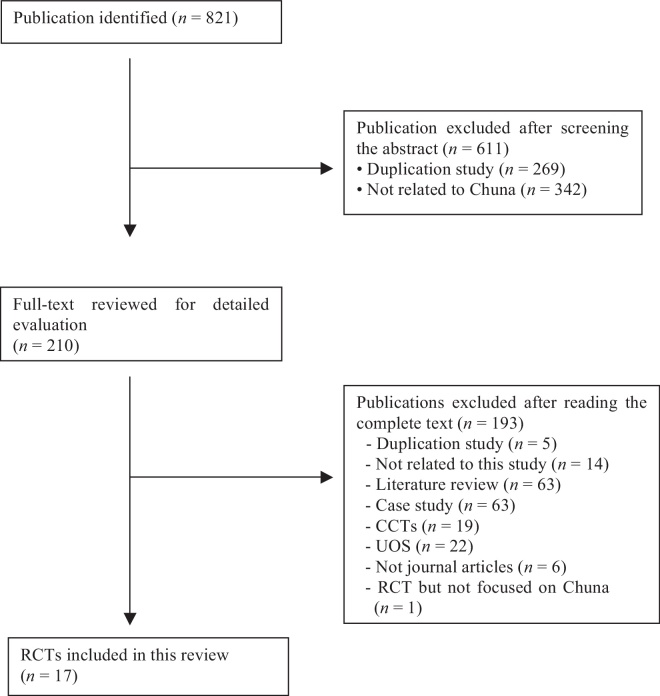
The literature search identified 821 potentially relevant studies. Of these studies, 804 were excluded. The exclusion criteria are described in Figure 1. Finally, 17 RCTs18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 met our inclusion criteria. Fourteen18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 of these RCTs were related to musculoskeletal diseases, and three RCTs32, 33, 34 were of neurological diseases. The key data are summarized in Table 3.
Fig. 1.
Flow chart of the literature search. CCT, controlled clinical trial; RCT, randomized controlled trial; UCT, uncontrolled clinical trial; UOS, uncontrolled observational study.
Table 3.
Key data from RCTs of Chuna in musculoskeletal and neurological diseases in the Korean literature.
| Disease classification | First author (Year) | Sample size/conditions | Interventions (regimen) | Main outcomes (intergroup difference) | Author's conclusion | Risk of bias * |
|---|---|---|---|---|---|---|
| Musculoskeletal disease | Lee (2012)18 | 82 patients with neck pain caused by TA | (A) Chuna (2 times weekly for 4 wks, total 8 sessions, n = 45) plus usual care [AT (15 min, 2 times weekly for 4 wks) and herbal medicine (Dangkwisoo-san for 2 wks and Ojucksan for 2 wks)] (B) PA (Hwangryunhaedock-tang herbal injection, 2 times weekly for 4 wks, total 8 sessions, n = 37) plus usual care |
(1) NDI (NS) (2) VAS (NS) |
Both (A) and (B) were considered to be effective and useful for low back pain caused by TA. No significant difference was found between (A) and (B) after 4 wks. However, (A) was more effective than (B) from weeks 2 to 4. | U, U, H, U, U, U |
| Lee (2012)19 | 87 patients with neck pain caused by TA | (A) PA (2 times a week for 4 wks, total 8 sessions, n = 24) plus usual care [AT (15 min, daily for 4 wks), herbal medicine (Dangkwisoo-san for 2 wks and Ojucksan for 2 wks)] (B) Chuna (2 times a week for 4 wks, total 8 sessions, n = 29) plus usual care (C) PA (once a week for 4 wks, total 4 sessions, n = 34), Chuna (once a week for 4 wks, total 4 sessions, n = 34) plus usual care |
(1) VAS (n.r.) (2) NDI (n.r.) |
(A), (B), and (C) were effective after 4 wks for neck pain caused by TA. After 4 wks of treatment, (C) was more effective than (A) and (B) individually for neck pain caused by TA. No statistical significance was found regarding whether (A) or (B) was superior, but (B) tended to be more effective than (A) |
L, U, H, U, U, U | |
| Kim (2011)20 | 20 patients with cervical sprain caused by TA | (A) Chuna (2 times weekly for 4 wks, total 8 sessions, n = 10) plus (B) (B) Usual care [AT (15 min, 2 times weekly for 4 wks, total 8 sessions), herbal medicine (n.r.), PA (Jungsongouhyul herbal injection 2 times weekly for 4 wks, total 8 injections), n = 10] |
(1) VAS (p < 0.05) | (A) was considered to be effective and useful on cervical sprains caused by TA. | U, U, H, U, U, U | |
| Woo (2011)21 | 60 patients with cervical pain caused by TA | (A) Chuna (2 times a week for 2 wks, total 4 sessions, n = 30) plus AT (15 min, 4 sessions, 2 times a week for 2 wks) (B) PA (ouhyul herbal injection, 2 times a week for 2 wks, total 4 injections, n = 30) plus AT (15 min, 2 times a week for 2 wks, total 4 sessions) |
(1) VAS (NS) (2) NDI (NS) |
(A) and (B) were effective in reducing cervical pain caused by traffic accidents. No significant difference was found between (A) and (B). | L, U, H, U, U, U | |
| Park (2007)22 | 10 patients with acute neck pain caused by TA | (A) Chuna (2 times weekly for 2 wks, total 4 sessions, n = 5) plus (B) (B) Usual care [AT (n.r., 4 times weekly, n = 5) plus cupping and physical therapy] |
(1) VAS (NS) (2) PDI (NS) (3) Pressure pain thresholds (NS) |
(A) may have been effective and useful for neck pain caused by TA, but no statistically significant difference was found between (A) and (B). | U, U, H, U, U, U | |
| Ryu (2006)23 | 20 chronic neck pain patients with a hypolordotic cervical spine | (A) Chuna (5 sessions, n = 10) plus (B) (B) AT (5 sessions, n = 10) |
(1) VAS (p < 0.05) | (A) was more effective than (B) in reducing neck pain. | U, U, H, U, U, U | |
| Yun (2012)24 | 38 patients with cervicogenic headache caused by TA | (A) Chuna (20 min, 3 times for 1 wk, n = 20) plus (B) (B) Usual care [AT (20 min, daily for 1 wk), herbal medicine (Kami-hwal-hyeol-tang, 2 times daily for 1 wk), PA (2 sessions for 1 wk), ICT (15 min, 3 sessions for 1 wk), cupping (3 sessions for 1 wk), n = 18] |
(1) VAS (p < 0.05) (2) NDI (p < 0.05) |
(A) had a significant effect on the cervicogenic headache caused by TA, which was more effective than (B). | L, U, H, U, U, U | |
| Jin (2011)25 | 52 patients with TMD | (A) Chuna (2 times weekly for 4 wks, n = 26) plus (B) (B) AT (2 times weekly for 4 wks, n = 26) plus PA |
(1) VAS (NS) (2) FPSC (NS) |
(A) and (B) were considered to be effective and useful in TMD, but additional comparative studies are needed to assess intergroup differences. | U, U, H, U, U, U | |
| Kim (2006)26 | 31 patients with TMD | (A) Chuna (3 trials of distraction per round, translation selectively, total 6 sessions, n = 15) plus muscle release technique (B) AT (20 min, total 6 sessions, n = 16) plus muscle release technique |
(1) MM (p < 0.05) (2) TN (p < 0.05) |
- | L, U, H, U, U, U | |
| Park (2009)27 | 74 patients with LBP | (A) Chuna (5 times, finger pressing technique on 6 AT points, n = 37) (B) TENS (20 min, 100 Hz, 10–30 mA, unilateral placement, n = 37) |
(1) VAS (p < 0.05) | (A) was a practical therapy for patients with LBP. | H, U, H, U, U, U | |
| Kim (2011)28 | 81 patients with LBP caused by TA | (A) Chuna (2 times weekly for 4 wks, total 8 sessions, n = 46) plus usual care [AT (15 min 2 times weekly for 4 wks) and herbal medicine (Dangkwisoo-san for 2 wks and Ojucksan for 2 wks)] (B) PA (Hwangryunhaedock-tang herbal injection, twice weekly for 4 wks, total 8 injections, n = 35) plus Usual care |
(1) ODI (NS) (2) VAS (NS) |
Both (A) and (B) were considered to be effective and useful for LBP caused by TA. No significant difference was found between (A) and (B). However, from weeks 2 to 4, (A) was more effective than (B). | U, U, H, U, H, U | |
| Yoon (2010)29 | 20 patients with acute LBP caused by TA | (A) Chuna (3 times in 1 wk, n.r., n = 10) plus (B) (B) Usual care [AT (15 min, 2 times daily, n.r.), herbal medicine (n.r.), physical therapy (n.r.), n = 10] |
(1) VAS (p < 0.05) | (A) was considered to be effective and useful in lumbar sprains caused by TA. | U, U, H, U, U, U | |
| Lee (2009)30 | 20 patients with LBP caused by TA | (A) Chuna (2 times at second and fourth day after admission, n = 10) plus (B) (B) Usual care [AT (2 times for one day), herbal medicine (n.r.), physical therapy (n.r.), n = 10] |
(1) HRV (NS) (2) VAS (NS) |
(A) appeared to help TA patients in the early stages to reduce pain. (A) appeared to have a positive effect. Further long-term, large-scale studies are necessary. | U, U, H, U, U, U | |
| Kim (2007)31 | 50 hemiplegic patients with shoulder pain | (A) Chuna (5 times weekly for 2 wks, total 10 sessions, n = 26) plus (B) (B) Usual care [AT (n.r.), herbal medicine (n.r.), physical therapy (n.r.), n = 24] |
(1) VAS (p < 0.01) (2) Passive ROM (p < 0.05) (3) Motor grade, difference in meridian electromyography, subluxation grade (NS) |
(A) may have been an efficacious method of improving shoulder pain and passive ROM in stroke patients. | U, U, H, U, U, U | |
| Neurological Diseases | Park (2011)32 | 36 patients with acute peripheral facial palsy | (A) Chuna (n.r., Danmuji Anchu traction technique, n = 18) plus (B) (B) Usual care [(AT (n.r., 2 times for 1 day), herbal medicine (n.r.), PA (once a day, Hominis placenta herbal injection), n = 18] |
(1) Yanagihara's score (p < 0.05) (2) Improvement index (p < 0.05) |
The Danmuji Anchu traction technique was effective for acute peripheral facial paralysis. | U, U, H, U, U, U |
| Bae (2010)33 | 39 patients with stroke-induced hemiplegia | (A) Chuna (daily for 3 wks, n = 20) plus (B) (B) Usual care [AT (30 min, 2 times for 1 day), herbal medicine, physical therapy (ICT, TENS, US, tilting table, Bobath approach), moxibustion, cupping, n = 19] |
(1) MBI (p < 0.05) (2) TCD (p < 0.05) |
Adjusting LLI by Chuna manual treatment was efficacious for the rehabilitation of stroke-induced hemiplegia in terms of ADL and cerebral blood flow. | U, U, H, U, U, U | |
| Kwon (2009)34 | 39 patients with stroke-induced hemiplegia | (A) Chuna (daily for 3 wks, n = 20) plus (B) (B) Usual care [AT (30 min, 2 times for 1 day), herbal medicine, physical therapy (ICT, TENS, US, tilting table, Bobath approach), moxibustion, cupping, n = 19] |
(1) MBI (p < 0.05) (2) BBS (p < 0.05) (3) FMA (p < 0.05) |
Adjusting LLI by Chuna manual treatment was efficacious for the rehabilitation of stroke-induced hemiplegia in terms of ADL balance and lower extremity function. | L, U, H, U, U, U |
* Domains of quality were assessed based on the Cochrane tools for assessing risk of bias, including random sequence generation, allocation concealment, patient blinding, assessor blinding, reporting dropout or withdrawal, selective outcome reporting. “L” indicates a low risk of bias; “U” indicates that the risk of bias is uncertain; “H” indicates a high risk of bias.
ADL, activity of daily living; AT, acupuncture; BBS, Berg Balance Scale; FMA, Fugl-Meyer Assessment; FPSC, Facial Pain Score Scale; HRV, heart-rate variability; ICT, interferential current therapy; LBP, low back pain; LLI, leg length inequality; MBI, Modified Barthel Index; min, minute; MM, mandibular movement; NDI, Neck Disability Index; n.r.; not reported; NS, not significant; ODI, Oswestry Disability Index; PA, pharmacoacupuncture; PDI, Pain Disability Index; RCT, randomized controlled trial; ROM, range of motion; TA, traffic accident; TCD, transcranial Doppler ultrasonography; TENS, transcutaneous electrical nerve stimulator; TMD, temporomandibular joint disorder; TN, temporomandibular joint noise; US, ultrasound; VAS, Visual Analog Scale; wks, weeks.
A total of 645 patients with musculoskeletal diseases were involved in the included studies, and a total of 114 patients were involved in the studies of neurological diseases. In the studies of musculoskeletal diseases, the medical conditions that were treated included neck pain with cervical sprain and cervical pain caused by traffic accidents (TAs) (five trials),18, 19, 20, 21, 22 neck pain with a hypolordotic cervical spine (one trial),23 cervicogenic headache caused by TA (one trial),24 temporomandibular joint disorder (TMD, two trials),25, 26 lower back pain (four trials; one trial was of nonspecific lower back pain, and three trials of lower back pain caused by TA),27, 28, 29, 30 and shoulder pain caused by stroke (one trial).31 In the studies of neurological diseases, the conditions that were treated were peripheral facial palsy (one trial)32 and stroke (two trials).33, 34
All of the included articles involved Chuna techniques. The number of times a patient was treated ranged from two to approximately 21 across all studies. The subjective outcome measures that were used in the studies of musculoskeletal diseases included the Neck Disability Index, the Visual Analog Scale, the Pain Disability Index, the Facial Pain Score Scale, the temporomandibular joint noise, and the Oswestry Disability Index. The objective outcome measures used in these studies were mandibular movement, pressure pain thresholds, heart-rate variability, and passive range of motion (ROM).
The subjective outcome measures that were used in the studies of neurological diseases were Yanagihara's score, the improvement index obtained using Yanagihara's score, the Modified Barthel Index, the Berg Balance Scale, and the Fugl-Meyer Assessment. The objective outcome measure used in these studies was transcranial Doppler ultrasonography.
3.3.2. Assessment of the risk of bias
Among the 17 included RCTs, only five19, 21, 24, 26, 34 described an appropriate method of sequence generation. One RCT27 had a high risk of bias due to random sequence generation. The remaining 11 articles did not clearly report the methods used to generate sequences. Allocation concealment was not conducted in any of the 17 RCTs. In terms of patient blinding, all of the included RCTs had a high risk of bias. The risk of assessor blinding was unclear in all of the studies. With regard to reporting participant dropout or withdrawal, one study28 had a high risk of bias, whereas the remaining 16 articles did not clearly report these data. All of the studies had an unclear risk of bias in selective outcome reporting. A quality assessment of the included RCTs is summarized in Table 3.
3.3.3. Outcomes
Five RCTs18, 19, 20, 21, 22 were of neck pain with cervical sprain and cervical pain caused by TAs. There were three RCTs18, 21, 22 that reported a neutral effect, one RCT20 that reported a positive effect, and one RCT19 in which Chuna could not be compared with the control condition to evaluate whether it was statistically more effective because the results of the study were not reported. Two RCTs18, 21 were designed to compare the effectiveness of Chuna plus standard care versus pharmacoacupuncture (PA) plus standard care. Another two RCTs20, 22 were designed to compare the effectiveness of Chuna plus standard care versus standard care alone. Lastly, only one RCT19 was designed as a three-armed controlled trial to compare PA plus standard care versus Chuna plus standard care versus PA plus Chuna plus standard care.
Both cervicogenic headache caused by TA and chronic neck pain with hypolordotic cervical spine were investigated by single respective RCTs. Both the RCT23 of chronic neck pain with hypolordotic cervical spine and the RCT24 of cervicogenic headache caused by TA reported positive effects after using Chuna compared with a control condition. Both of the two RCTs were designed in the form of Chuna plus standard care versus standard care.
TMD was studied in two RCTs.25, 26 Of the two RCTs for TMD, Chuna was reported to have a neutral effect in one RCT,25 and the other RCT26 reported that Chuna had a negative effect on TMD when compared with acupuncture. One RCT was designed to compare Chuna plus standard care versus standard care alone, whereas the other RCT was designed to compare Chuna plus an adjunctive therapy versus standard care plus an adjunctive therapy.
Four RCTs27, 28, 29, 30 examined lower back pain caused by TA or nonspecific lower back pain. Of the four RCTs of lower back pain, two RCTs27, 29 reported a positive effect of applying Chuna techniques, and the remaining two RCTs28, 30 reported a neutral effect. Two RCTs29, 30 were designed to compare Chuna plus standard care versus standard care alone, and another RCT28 was designed to compare Chuna plus standard care versus PA plus standard care. Only one RCT27 of the 17 included RCTs was designed to compare Chuna alone versus standard care.
Only one RCT31 of Chuna in hemiplegic stroke patients with shoulder pain drew a conclusion that it was effective in improving shoulder pain and passive ROM. This RCT was designed to compare Chuna plus standard care versus standard care alone.
All of the three RCTs32, 33, 34 reported that Chuna had a positive effect in neurological diseases; one RCT32 dealt with an acute peripheral facial palsy, and the remaining two RCTs33, 34 examined stroke-induced hemiplegia. All of these studies were designed to compare Chuna plus standard care versus standard care alone. A detailed explanation of each RCT is shown in Table 3.
In addition to the study design and results of each trial, it is important to note that a high risk of bias or uncertainty in assessing bias was evident in the overwhelming majority of these RCTs. None of the RCTs used allocation concealment or assessor blinding; in addition, neither participant dropout or withdrawal rates nor specific outcomes were fully described. Considering the fact that low-quality trials tend to overestimate effect sizes,35 we could not unequivocally say that Chuna is more effective than control treatment conditions, even in specific trials suggesting this.
Fundamentally, we must admit that we were at a disadvantage to assess the effectiveness of Chuna using Korean trials; Korea is one of the East Asian countries that has been shown to reject negative results for publication.36 This implies that there may have been a number of unreported RCTs of Chuna with negative results.
4. Conclusions
Although all the KM colleges in Korea have established a curriculum that includes Chuna education, the total number of hours dedicated to CRS was less than those dedicated to the WHO guidelines. In the modern Chuna era, Chuna has developed substantially as the result of a more solid Korean academic system, partial coverage of services by insurance carriers, and after the formation of a formal Chuna association. By analyzing the available RCTs of Chuna, we concluded that evidence regarding the effectiveness of Chuna in musculoskeletal and neurological diseases is insufficient. The methodological quality of the included RCTs was also typically too low to draw firm conclusions.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- 1.World Health Organization Media centre. Traditional medicine. Geneva, Switzerland: World Health Organization; 2008. Available from: http://www.who.int/mediacentre/factsheets/fs134/en/. Accessed April 1, 2013.
- 2.Cheung F. TCM: made in China. Nature. 2011;480:S82–S83. doi: 10.1038/480S82a. [DOI] [PubMed] [Google Scholar]
- 3.Moon TW, Choi TY, Park TY, Lee MS. Chuna therapy for musculoskeletal pain: a systematic review of randomized clinical trials in Korean literature. Chin J Integr Med. 2013;19:228–232. doi: 10.1007/s11655-012-1238-0. [DOI] [PubMed] [Google Scholar]
- 4.Shin B, Shin J, Lee J, Lim H. Chuna coordinative and orthopedic manual medicine. Seoul, Korea: Korean Society of Chuna Manual Medicine for Spine and Nerves; 2006:5–6. [Google Scholar]
- 5.Park J, Shin S, Park J. A comparative study on the concepts of the Chuna. J Korean Soc Orient Med Class. 2008;21:173–191. [Google Scholar]
- 6.Park T, Shin B. Curriculum analysis of Chuna manual medicine in Korea. J Korean Chuna Man Med Spine Nerves 2010; 5:157-68.[In Korean, English abstract].
- 7.Korean Society of Chuna Manual Medicine for Spine and Nerves. Introduction. Seoul, Korea: Korean Society of Chuna Manual Medicine for Spine and Nerves; 2011. Available from: http://www.chuna.or.kr/v2/include/english.php. Accessed March 25, 2013.
- 8.Shin BC, Kim SD, Lee MS. Comparison between the effects of Chuna manipulation therapy and cervical traction treatment on pain in patients with herniated cervical disc: a randomized clinical pilot trial. Am J Chin Med. 2006;34:923–925. doi: 10.1142/S0192415X06004399. [DOI] [PubMed] [Google Scholar]
- 9.Park JJ, Shin J, Choi Y, Youn Y, Lee S, Kwon SR. Integrative package for low back pain with leg pain in Korea: a prospective cohort study. Complement Ther Med. 2010;18:78–86. doi: 10.1016/j.ctim.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 10.Health Insurance Review and Assessment Service. Healthcare system. Seoul, Korea: Health Insurance Review and Assessment Service; 2011. Available from: http://www.hira.or.kr/dummy.do?pgmid=HIRAA030063010000&cmsurl=/cms/law/02/01/01/1210317_13412.html. Accessed April 30, 2013.
- 11.Shin BC, Yoon SH, Lee JS. Review on the history of Chuna manual medicine. J Korean Man Med. 2000;1:9–43. [Google Scholar]
- 12.Han YS, Heo DS, Oh MS. A medico-historical consideration of documents on Chuna. J Res Cent Orient Med in Daejeon Univ. 2007;16:167–180. [Google Scholar]
- 13.Park JM, Shin SW, Park JH. A comparative study on the concepts of the Chuna. Korean Soc Orient Med Class. 2008;21:173–191. [Google Scholar]
- 14.Shin JS. 1st ed. Seoul, Korea; Korea KCA: 1995. Chuna manual therapy in Korea. [Google Scholar]
- 15.Korean Society of Chuna Manual Medicine for Spine and Nerves. Chuna Academy. Seoul, Korea: Korean Society of Chuna Manual Medicine for Spine and Nerves; 2011. Available from: http://www.chuna.or.kr/board_v2/bbs/board.php?bo_table=03_03_03&wr_id=705. Accessed from: March 28, 2013.
- 16.Auto Insurance Medical Fee Review Council. Announcement list. Available from: http://www.aimfrc.or.kr/public/notice_view.asp?num=338&page=1&kind=1.
- 17.World Health Organization. WHO guidelines on basic training and safety in chiropractic. Geneva, Switzerland: World Health Organization; 2005.
- 18.Lee J, Kim J, Yang K, Han S, Lee C, Shin H. The comparative study on the effect of pharmacopuncture treatment and Chuna treatment for neck pain caused by traffic accidents. J Orient Rehab Med. 2012;22:75–83. [In Korean, English abstract] [Google Scholar]
- 19.Lee J, Lee S, Nam J, Kim K, Lee M, Lim S. The comparative study on the effect of pharmacopuncture treatment. Chuna treatment, pharmacopuncture-Chuna cooperative treatment for neck pain caused by traffic accidents. J Korean Acupunct Moxibustion Soc. 2012;29:87–95. [In Korean, English abstract] [Google Scholar]
- 20.Kim E, Kim T, Lee S, Bae S, Woo J, Han K. Effect of Chuna manipulation on cervical sprain caused by traffic accident. J Orient Sports Med. 2011;11:49–56. [In Korean, English abstract] [Google Scholar]
- 21.Woo J, Han K, Kim E, Lee S, Lee J, Nam J. A clinical study comparing the effects of Chuna treatment and Ouhyul herbal acupuncture on the patients with cervical pain caused by traffic accidents. J Korean Acupunct Moxibustion Soc. 2011;28:9–18. [In Korean, English abstract] [Google Scholar]
- 22.Park S, Kim J, Ko K, Choi S, Lee Y, Lee Y. The clinical studies for Chuna treatment on patients of neck pain caused by traffic accidents. J Korean Acupunct Moxibustion Soc. 2007;24:55–64. [In Korean, English abstract] [Google Scholar]
- 23.Ryu H, Jeon S, Park D, Lee S. Clinical study for Chuna treatment on neck pain patients with hypolordotic cervical spine. J Korean Chuna Man Med Spine Nerves. 2006;1:11–20. [In Korean, English abstract] [Google Scholar]
- 24.Yun S, Jung W, Cho S, Cho H. The clinical study for Chuna treatment on patients with cervicogenic headache caused by traffic accident. J Orient Rehab Med. 2012;22:165–175. [In Korean, English abstract] [Google Scholar]
- 25.Jin E, Lee J, Kim H, Yeom S, Jeong H, Lim C. The clinical study for the effects of Chuna treatment on patients with temporomandibular disorder. J Orient Rehab Med. 2011;21:125–135. [In Korean, English abstract] [Google Scholar]
- 26.Kim T, Kim C, Lee K, Um T, Jung Y, Kho Y. Comparative clinical study between the acupuncture treatment and the Chuna treatment on temporomandibular disorder. J Korean Chuna Man Med Spine Nerves. 2006;1:55–64. [In Korean, English abstract] [Google Scholar]
- 27.Park H. Effects of Chuna therapy on the low back pain; focusing on the finger pressure therapy of acupuncture point. J Korean Contents Assoc. 2009;9:243–248. [In Korean, English abstract] [Google Scholar]
- 28.Kim J, Lee J, Yang K, Kim J, No H, Jeong Y. The comparative study on the effect of pharmacopuncture treatment and Chuna treatment for low back pain caused by traffic accidents. J Korean Chuna Man Med Spine Nerves. 2011;6:155–164. [In Korean, English abstract] [Google Scholar]
- 29.Yoon D, Son J, Choi J, Jung S, Kim S. Effect of Chuna treatment on lumbar sprain caused by traffic accident. J Korean Chuna Man Med Spine Nerves. 2010;5:23–30. [In Korean, English abstract] [Google Scholar]
- 30.Lee J, Park J, Lee E, Jeon T, Hong S. Effect of Chuna treatment on lumbar sprain caused by traffic accident in early stage. J Korean Chuna Man Med Spine Nerves. 2009;4:61–74. [In Korean, English abstract] [Google Scholar]
- 31.Kim M, Chung S, Kim S. The influences of Chuna therapy for shoulder pain and range of movement in hemiplegic patients after stroke. J Orient Rehab Med. 2007;17:185–198. [In Korean, English abstract] [Google Scholar]
- 32.Park J, Lee C, Lee Y, Kwon K, Yoon H, Jeon D. The clinical research of the effectiveness of “DanmujiAnchu traction technique” on acute peripheral facial paralysis. J Korean Chuna Man Med Spine Nerves. 2011;6:43–52. [In Korean, English abstract] [Google Scholar]
- 33.Bae B, Kwon O. The effect of adjusting leg length inequality by Chuna manual treatment on the cerebral blood flow in post-stroke hemiplegia. J East-West Med. 2010;35:75–84. [In Korean, English abstract] [Google Scholar]
- 34.Kwon O, Jang W, Woo C, An H. The efficacy of adjusting leg length inequality by Chuna manual treatment for post-stroke hemiplegia. J Orient Rehab Med. 2009;19:187–202. [In Korean, English abstract] [Google Scholar]
- 35.Moore A, McQuay H. Oxford University Press; Oxford: 2006. Bandolier's little book of making sense of the medical evidence. [Google Scholar]
- 36.Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results?. A systematic review of controlled trials. Control Clin Trials. 1998;19:159–166. doi: 10.1016/s0197-2456(97)00150-5. [DOI] [PubMed] [Google Scholar]