Abstract
Background and Objective
Short nighttime sleep duration is a possible factor contributing to childhood obesity. Our objective was to evaluate associations between sleep timing (including bedtime and waketime) and its association with weight gain in 4-5 year-old children.
Methods
We used cross-sectional and longitudinal regression analyses of a large, nationally-representative sample of children from the Early Childhood Longitudinal Study–Birth Cohort. Data regarding the timing and duration of weekday sleep was assessed via parent questionnaire. Short sleep duration, late bedtime and early wake time were defined as those greater than one standard deviation from the mean for the group.
Results
Using linear regression adjusted for confounders, sleep duration at 4 and 5 years and bedtime at 5 years were linked to BMI-z-score (p<0.001). Odds of obesity were higher at 4 years for children sleeping <9.44 hours nightly (adjusted odds ratio 1.35, confidence interval 1.02-1.78, p<0.05) and at 5 years for children going to bed at 9:00 pm or later (1.49, 1.16-1.45, p<0.01) or waking before 6:30 (1.23, 1.01-15.51, p<0.05). Assessed longitudinally, both short sleep duration (p<0.05) and later bedtime at 4 years (p<0.01) were associated with increase in BMI-z-score between 4-5 years.
Conclusions
Children with shorter nighttime sleep durations and later bedtimes were more likely to be obese and to gain weight over time. Pediatricians should encourage families to place children to bed at earlier times to promote longer sleep duration as a potential means of controlling weight gain.
Keywords: Obesity, weight gain, sleep, bedtime, preschool
Introduction
Over the past thirty years in the US, obesity rates have tripled, and currently about 1 in 3 children are overweight or obese(1). Preschoolers who are overweight are twice as likely to be overweight adults(2). The trend of increasing obesity is associated with many adverse health outcomes including cardiovascular, endocrine and psychological morbidity(3). As the long term risks of obesity are discovered, there is increasing interest in prevention strategies for maintaining normal weight.
Duration of nighttime sleep is a modifiable risk factor(4) related to many health outcomes, including obesity. Multiple studies relate shorter sleep duration to a range of morbidities including obesity, diabetes, coronary heart disease, and depression, as well as mortality(5-7). “Short sleeping” is typically defined for adults as less than 7 hours per night, with variable definitions during childhood. The AAP currently recommends that children ages 3-10 years receive 10-12 hours of sleep nightly(8). Among children and adolescents, many(9-16) but not all(17,18) previous reports have suggested that nighttime sleep duration is related to childhood overweight and obesity. However, these studies have had limitations that affect their generalizability to US preschool and kindergarten children, including use of wide age ranges(9,11,12), use of data from other countries(9,10,15,17), limited sample size without adjustment for confounders(14), and lack of longitudinal assessment(10). These studies have failed to evaluate for potential relationships between low amounts of sleep and less statural growth, a potential cause of high body mass index (BMI). Additionally, none of these studies has evaluated the relationship between bedtime and waketime on weight gain in this age range Such information would be helpful in guiding recommendations to parents regarding sleep timing.
Our goal was to assess cross-sectional and prospective relationships between sleep duration, sleep timing and weight status in preschool and kindergarten children. Our hypothesis was that shorter nightly sleep, related to both later bedtime and earlier waketime, would correspond to higher weight status and prospective weight gain, even after adjustment of potential confounders. We used the Early Childhood Longitudinal Study–Birth Cohort (ECLS-B), a large, nationally-representative cohort of children followed prospectively until kindergarten, to clarify potential relationships between sleep duration and timing and body weight in early childhood.
Methods
Data Set
The ECLS-B is a large multi-source, multi-method study sponsored by the National Center for Education Statistics (NCES), United States Department of Education. The ethics review board at NCES approved the study. The ECLS-B includes a nationally-representative sample of children born in 2001 selected by random sampling of birth certificates and examined longitudinally at ages 9 months, 2 years, 4 years and 5 years (from 9/2001–8/2006). The researchers obtained a final sample of approximately 10,700 completed parent interviews. NCES obtained informed consent from all participants.
Measures
The current analysis includes data from the evaluations at ages 4 years and 5 years during which data on nighttime sleep was available(19). The primary care-giver (most often the mother) completed a computer-assisted interview at home by trained assessors. The main predictor variable for this analysis, nighttime sleep duration, was calculated from the parent responses to two questions: “about what time does your child usually go to sleep on a weeknight?” and “about what time does your child usually wake up on a weekday?” These questions were used to examine nighttime sleep duration as well as bed and waketimes. Previous studies found that parental reports for bed and waketimes correspond with sleep duration as measured by actigraphy(20). Nighttime sleep durationwas examined continuously by approximate quintiles. Bedtime and waketime were divided into tertiles because commonly-reported bedtimes and waketimes precluded even division into quintiles. For logistic regression we used a cut-off of one standard deviation below the mean to categorize short sleep duration, late bedtime and early waketime.
During the parent interview, parents identified their child's gender and race/ethnicity. The parents told how many hours their child watches television on a typical weekday. In the ECLS-B the variable for each family's socioeconomic status was created by the NCES using family income, maternal education, maternal occupation, paternal education and paternal occupation based on an aggregate of data compiled by 5 years of age. This measure was then broken into quintiles(19).
The children's height and weight were measured using a standardized protocol. The children were dressed in light clothing without shoes. A portable stadiometer was used to measure height and a digital scale was used for weight. BMI was calculated as weight in kilograms divided by height in meters squared. BMI categories for normal (<85th%), overweight (≥85th–95th%), and obese (≥95th%) were defined based on percentiles according to age and gender using the 2000 Centers for Disease Control and Prevention growth charts for the United States. BMI z-scores were created using CDC SAS code.
Data Analysis
We performed statistical analyses using SAS software, Version 9.2 (SAS Institute Inc., Cary, NC, USA). All unweighted sample sizes are rounded to the nearest 50 in compliance with the NCES rules. We conducted all tests using two-sided analyses with a significance level of alpha equal to 0.05. SAS survey procedures were used to account for the complex sampling design in the ECLS-B and appropriate weights provided by the NCES were used to give population estimates. These weights adjust for the complex sampling design and oversampling of specific groups that was done during the study and allows for the data to be representative of all children born in the US in 2001. We examined the variables for normality using univariate and histogram procedures and used frequency procedures to look at relationships between the variables, using ANOVA to assess for differences between groups. To examine the relationship between sleep duration, bedtime and waketime and overweight/obesity, we used linear and logistic regression. To evaluate longitudinal associations of sleep duration and sleep timing on weight gain over time, we used linear regression, assessing change in BMI z-score between 4–5 years among different groups: quintiles of sleep duration at 4 years and tertiles of bedtime and waketime at 4 years. In determining mean levels of sleep, bedtime and waketime we adjusted for commonly-used confounders of sex, race/ethnicity and SES quintile. In linear and logistic regression analysis we additionally included TV viewing to assess its potential role in the relationship between sleep and weight status. In assessing changes in BMI z-score, we additionally excluded underweight children (BMI z<-2) to assess whether this affected the magnitude of the findings. Beta coefficients, odds ratios (OR), and confidence intervals are reported in tables.
Results
Demographics
We analyzed data from 10,700 initial participants of ECLS-B, of whom 8950 and 7000 at the 4- and 5-year time points, respectively had remained in the study and had complete data regarding sleep parameters and BMI. At the 4 year time point, children who dropped out by 5 years (as compared to those who did not drop out) had similar sleep duration (10.45 vs. 10.42 hours, p=0.99) and a similar BMI z-score (0.569 vs. 0.536, p=0.98). Nighttime sleep duration, bedtime and waketime by sex, race/ethnicity and SES quintile are shown in Table 1. As expected, there were significant inverse correlations between shorter sleep and both later bedtime and earlier waketime (Pearson's r at 4 years -0.43 for bedtime, and 0.61 for waketime, both p<0.001). From a cross-sectional basis there was a decrease in sleep duration between age 4–5 years (10.47 hours vs. 10.37 hours), with kindergarteners exhibiting both earlier bed times (8:34 pm vs. 8:46 pm) and earlier waketimes (6:56 am vs. 7:14 am)(all p<0.0001)(Table 1). Within-child differences also revealed a decrease in sleep duration, with children sleeping 5.5 +/-1.0 minutes less at 5 years compared to 4 years, going to bed 11.4 +/-0.8 minutes earlier and waking 16.8 +/-1.0 minutes earlier. At 4 and 5 years, respectively, 21% and 23% of children slept less than the 10 hours of sleep that is the lower limit recommended by the American Academy of Pediatrics for these ages(8). There were significant differences in sleep duration, bedtimes and waketimes by race/ethnicity (chi-square p<0.0001), with African American children having the shortest sleep duration and latest bedtimes and white children having the longest duration. There were also progressively earlier bedtimes with increasing SES level. Children watching >2 hours of TV daily had later bedtimes and later waketimes at both 4 and 5 years, with shorter sleep duration at 5 years only (p<0.01; Table 1). At both 4 and 5 years, children in the lowest quintile for sleep (p<0.05) and the highest tertile for bedtime (p<0.001) were more likely to have watched >2 hours of TV (data not shown). This was also true for children with the earliest wake tertile at 4 years (p<0.05) but not 5 years (p=0.66; data not shown).
Table 1. Descriptive data: Mean sleep amount, bedtime and wake time of included participants from ECLS-B.
| 4 years | 5 years | |||||||
|---|---|---|---|---|---|---|---|---|
| Number (weighted percent) | Sleep amount, hours (std error) | Bed time (std error in minutes) | Wake time (std error) | Number (weighted percent) | Sleep amount, hours (std error) | Bed time (std error) | Wake time (std error) | |
| Total | 8950 | 10.47 (0.01) | 8:46 (0.6) | 7:14 (0.6) | 7000 | 10.37 (0.01) | 8:34 (0.06) | 6:56 (0.6) |
| Sex | ||||||||
| Male | 4550 (50.9) | 10.46 (0.02) | 8:46 (1.2) | 7:14 (1.5) | 3550 (50.6) | 10.35 (0.02) | 8:35 (1.2) | 6:56 (1.1) |
| Female | 4400 (49.1) | 10.48 (0.02) | 8:46 (1.3) | 7:15 (1.4) | 3450 (49.4) | 10.39 (0.02) | 8:34 (1.4) | 6:57 (1.3) |
| p value* | 0.438 | 0.777 | 0.339 | 0.175 | 0.355 | 0.626 | ||
| Race/ethnicity | ||||||||
| White | 3900 (43.8) | 10.54 (0.02) | 8:37 (1.4) | 7:09 (1.4) | 2850 (41.4) | 10.47 (0.02) | 8:26 (1.4) | 6:54 (1.2) |
| African American | 1350 (15.4) | 10.16 (0.04) | 8:57 (2.2) | 7:07 (2.8) | 1100 (15.8) | 9.99 (0.04) | 8:45 (1.8) | 6:44 (2.3) |
| Hispanic | 1750 (19.7) | 10.52 (0.03) | 8:55 (1.7) | 7:27 (2.4) | 1400 (20.0) | 10.39 (0.03) | 8:44 (1.9) | 7:07 (2.3) |
| Asian | 900 (10.1) | 10.21 (0.04) | 8:19 (2.3) | 7:32 (2.9) | 800 (10.8) | 10.17 (0.04) | 8:59 (2.4) | 7:10 (2.1) |
| Other | 1000 (11.1) | 10.44 (0.06) | 8:49 (3.0) | 7:15 (3.5) | 850 (12.0) | 10.35 (0.06) | 8:35 (3.2) | 6:56 (3.4) |
| p value* | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | ||
| SES quintile | ||||||||
| 1 | 1650 (18.1) | 10.54 (0.04) | 8:57 (1.9) | 7:30 (2.3) | 1250 (17.7) | 10.31 (0.04) | 8:44 (2.4) | 7:02 (2.5) |
| 2 | 1700 (19.0) | 10.38 (0.04) | 8:57 (2.2) | 7:19 (3.1) | 1300 (19.0) | 10.23 (0.04) | 8:39 (2.1) | 6:53 (2.2) |
| 3 | 1750 (19.9) | 10.39 (0.03) | 8:48 (1.6) | 7:11 (1.6) | 1350 (19.5) | 10.34 (0.03) | 8:34 (1.9) | 6:55 (1.8) |
| 4 | 1750 (19.8) | 10.50 (0.03) | 8:40 (1.8) | 7:10 (1.6) | 1400 (19.9) | 10.47 (0.03) | 8:30 (1.9) | 6:58 (1.9) |
| 5 | 2050 (23.2) | 10.54 (0.03) | 8:29 (1.6) | 7:01 (1.6) | 1650 (23.8) | 10.50 (0.03) | 8:24 (2.0) | 6:54 (1.6) |
| p value* | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.036 | ||
| TV viewing | ||||||||
| ≤2 hours | 5980 (71.3) | 10.46 (0.02) | 8:41 (1.3) | 7:09 (1.3) | 4900 (78.1) | 10.40 (0.02) | 8:30 (1.0) | 6:54 (1.0) |
| >2 hours | 2400 (28.7) | 10.50 (0.03) | 8:58 (1.5) | 7:28 (1.8) | 1400 (21.9) | 10.26 (0.04) | 8:49 (2.2) | 7:05 (2.6) |
| p value* | 0.278 | <0.001 | <0.001 | 0.005 | <0.001 | <0.001 | ||
ANOVA for difference between groups for each descriptive category.
Sleep characteristics by weight category
At both 4 and 5 years there was a high prevalence of children who were overweight (15.9%, 16.6%, respectively) and obese (15.6% and 15.2%; Supplementary Table 1). Sleep duration by weight category is further given in Supplementary Table 1. At both 4 and 5 years there was shorter sleep duration among children in the heavier weight category, with obese children sleeping less than normal-weight children at both 4 years (10.5 hours normal weight vs. 10.37 hours obese, p<0.01) and 5 years (10.4 hours normal weight vs. 10.27 hours obese, p<0.01). Similarly, bedtime was later among obese children as compared to normal weight children (p<0.05; Supplementary Table 1).
Cross-sectional evaluation of sleep parameters and BMI z-score
Figure 1 displays mean BMI z-scores by quintile of night time sleep, adjusted for sex, race/ethnicity, and SES. At both 4 and 5 years, BMI z-score was progressively higher with decreasing sleep duration. This inverse relationship between sleep duration and BMI z-score was evaluated further using linear regression as shown in Supplementary Table 2, with a significant inverse association between sleep duration and BMI z-score at 4 and 5 years that persisted following adjustment for potential confounders (sex, race/ethnicity, SES, TV viewing; p<0.001). At 4 and 5 years, each additional hour of sleep was associated with a lower BMI z-score of 0.06 and 0.09 units, respectively. At 4 and 5 years, later bedtime was associated with higher BMI z-score; this association was attenuated following adjustment for the confounders above at 4 (p=0.24) but not 5 years (p<0.05). Waketime was not associated with BMI z-score, though at 5 years there was a trend toward an association between earlier waketime and obesity following adjustment (p=0.051). We further evaluated for effects of sleep amount on height-for-age z-scores and did not find an association (data not shown). For all of these analyses, exclusion of underweight children from the sample did not alter the results.
Figure 1. BMI z-score by Categories of Sleep Duration, Bedtime and Wake Time.
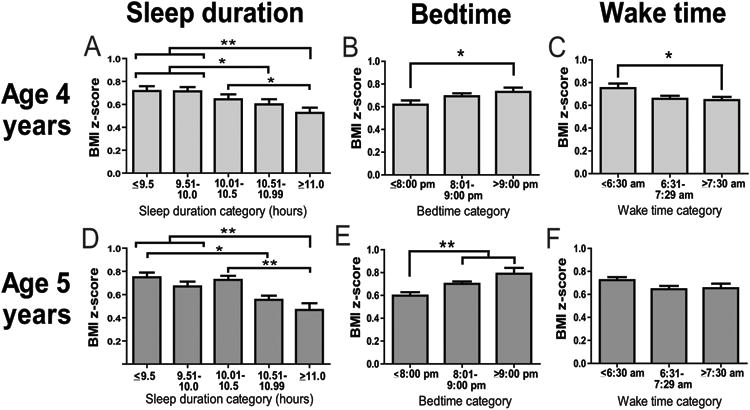
Mean BMI z-score (adjusted for sex, socioeconomic status and race/ethnicity) are shown at 4 and 5 years by approximate quintiles of sleep duration (A and D) and tertiles of bedtime (B and E) and wake time (C and F). Statistical significance: * p<0.05; * p<0.01.
We next divided children into those who had short sleep duration, late bedtime and early waketime based on those who were greater than one standard deviation from the mean. Those who had late bedtimes by this estimate also had early waketimes for 5.6% of preschoolers and 7.1% of kindergarteners. We then used logistic regression to compare children's odds of obesity based on sleep parameters (Table 2). Regarding sleep duration and risk of obesity, in fully-adjusted models at age 4 years children in the lowest quintile (sleep duration <9.44 hours) compared to all other children had an OR of 1.36 (1.03-1.80, p<0.05) for being obese (p<0.05). Regarding bedtime and risk of obesity, 5-year-old children with a bedtime at 9:00 pm or later had an OR of 1.49 (1.16-1.91) for being obese (p<0.01). Finally, regarding waketime, children at 5 years waking before 6:30 am had an OR of 1.23 (1.01-1.51) for being obese (p<0.05).
Table 2. Logistic regression of sleep amount on obesity status at 4 and 5 years old.
This analysis gives odds of overweight or obesity for children with low sleep duration, late bedtime and early wake time vs. all others in adjusted models.
| Age 4 years | Sleep duration <1 standard deviation below mean vs. others (<9.44 hours vs. ≥9.44 hrs) | Bedtime >1 st deviation above mean vs. others (after 9:30 pm vs. at or before 9:30 pm) | Wake time <1 standard deviation below mean vs. others (before 6:30 am vs. at or after 6:30 am) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overweight OR, CI | p-value | Obesity OR, CI | p-value | Overweight OR, CI | p-value | Obesity OR, CI | p-value | Overweight OR, CI | p-value | Obesity OR, CI | p-value | |
| Model 0 (no adjustments) | 1.15 (0.93-1.42) | 0.196 | 1.48 (1.13-1.93) | 0.004 | 1.20 (1.04-1.39) | 0.015 | 1.26 (1.05-1.52) | 0.014 | 1.05 (0.86-1.28) | 0.620 | 1.20 (0.94-1.53) | 0.154 |
| Model 1 (adjusted for sex, race/ethnicity, SES, television viewing) | 1.08 (0.88-1.34) | 0.471 | 1.36 (1.03-1.80) | 0.030 | 1.11 (0.96-1.29) | 0.154 | 1.13 (0.93-1.34) | 0.218 | 1.04 (0.85-1.27) | 0.696 | 1.17 (0.91-1.50) | 0.220 |
| Age 5 years | Sleep duration <1 standard deviation below mean vs. others (<9.48 hours vs. ≥9.48 hrs) | Bedtime >1 st deviation above mean vs. others (at or after 9:00 pm vs. before 9:00 pm) | Wake time <1 standard deviation below mean vs. others (before 6:30 am vs. at or after 6:30 am) | |||||||||
| Overweight OR, CI | p-value | Obesity OR, CI | p-value | Overweight OR, CI | p-value | Obesity OR, CI | p-value | Overweight OR, CI | p-value | Obesity OR, CI | p-value | |
| Model 0 (no adjustments) | 1.20 (0.94-1.52) | 0.148 | 1.19 (0.85-1.67) | 0.305 | 1.27 (1.06-1.52) | 0.011 | 1.66 (1.30-2.12) | <0.0001 | 1.23 (1.02-1.47) | 0.029 | 1.25 (1.02-1.53) | 0.028 |
| Model 1 (adjusted for sex, race/ethnicity, SES, television viewing) | 1.13 (0.90-1.43) | 0.296 | 1.12 (0.79-1.58) | 0.530 | 1.21 (1.00-1.45) | 0.046 | 1.49 (1.16-1.91) | 0.002 | 1.21 (1.00-1.46) | 0.051 | 1.23 (1.01-1.51) | 0.040 |
Longitudinal evaluation of sleep and weight status
We next hypothesized that lower sleep duration, later bedtime and earlier waketime would contribute to increased weight gain over time. Children in the lowest quintile for sleep at age 4 years exhibited an increase in BMI z-score while children in the highest sleep quintile overall exhibited a decrease in BMI z-score (Figure 2). Using linear regression to assess the relationship between sleep characteristics at age 4 years and change in BMI z-score between 4–5 years of age, sleep duration was inversely associated with BMI z-score over time (p<0.05), while later bedtime was associated with a higher BMI z-score (p<0.01; Supplementary Table 3).
Figure 2. Longitudinal Changes in BMI z-Score by Categories of Sleep Duration, Bedtime and Wake Time.
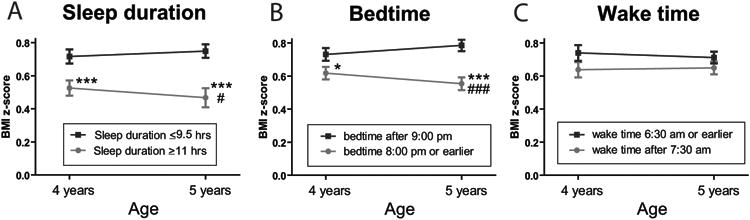
Mean BMI z-score (adjusted for sex, socioeconomic status and race/ethnicity) at 4 and 5 years based on baseline (4-year-old) sleep duration (A), bedtime (B) and wake time (C).
Comparison of BMI z-score to alternate group: *** p<0.001; * p<0.05.
Comparison of change in BMI z-score (4 to 5 years) between groups: ### p<0.001; #p<0.05.
Discussion
Evidence that temporal changes in sleep duration(21) may have contributed to the current obesity epidemic continues to accumulate, with multiple studies in adults(5) and children(9-16) linking shorter sleep time with higher weight status. The current study expands on previous reports by demonstrating 1) the association between short-sleep and higher BMI z-score following adjustment for multiple confounders is present already by preschool among a large, nationally-representative sample, 2) preschoolers with short-sleep are more likely to exhibit increased BMI z-score over a year's time and 3) later bedtime in particular was associated with higher weight status and increased weight gain over time. These findings suggest the potential that setting earlier bedtime for preschool children represents a modifiable lifestyle practice(4) that may help restrain unhealthy weight gain. In this way, this study supports recent calls by national organizations(22,23) and researchers(12,13) for more sleep in childhood.
In this national sample, preschool and kindergarten children slept an average of 10.47 hours per night at 4 years and 10.37 hours at 5 years, which appears to reflect a decrease in nighttime sleep duration from previous estimates of 11.5 hours nightly for 4 year-olds in the 1970's-1980's(24). The Zurich Longitudinal Studies followed sleep patterns among almost 500 children from the 1970's–1990's and reported nighttime sleep mean +/- standard deviation of 11.2 +/-0.8 hours at 4 years and 11.1 +/-0.7 hours at 5 years(21). Thus, ECLS-B mean sleep duration is equivalent to one standard deviation below the mean from the Zurich Study, suggesting the potential for overall sleep deprivation nationally in this age range. AAP recommendations regarding sleep are that children ages 3-10 years receive 10-12 hours of sleep nightly(8). In our study 21%-23% of children received less than the recommended lower range of sleep recommended.
Childhood sleep patterns in preschool and kindergarten are influenced by child temperament (potentially affecting compliance with bedtime routines) and parental limit setting(25). While total nighttime sleep duration is related to both bedtime and waketime, prior studies have implicated later bedtimes and not early waking as the major contributor to the current shift toward less sleep(26). We found that childhood weight status was more tightly linked to later bedtime than earlier waketime. Late bedtimes are related to factors such as TV viewing in school-aged children and adolescents(27). We found associations between increased daily TV viewing and later bedtime at 4 and 5 years, though we lacked data regarding whether this viewing occurred close to bedtime.
Even though we noted that heavier weight status was more consistently related to later bedtime than to earlier rising, we also noted associations of weight status and early rising, with an OR of obesity of 1.23 at 5 years for children waking before 6:30 am. While the reason for this association is unknown, previous studies have linked early school start times to less sleep among school-aged children(22,28). Studies regarding later school start times among middle school children reveal an increase in sleep time, with similar bedtimes but later waketimes among children in late-starting schools(28), though the effect of later start times on weight status has not been studied.
While this study was observational in nature, other studies on this topic have investigated for possible mechanistic links between sleep amount and obesity. Potential causative factors suggested have included the following: 1) increased caloric intake due to factors such as later bedtime and therefore more time available for eating(16,26,29), 2) short-sleep-induced or sleep timing induced dysregulation of appetite-related hormones such as ghrelin, leptin and cortisol(16,30), 3) a decrease in growth hormone, with related decrease in lipolysis and increase in fat mass accumulation(31), and 4) a decrease in exercise due to short-sleep-related fatigue(27, 31). More specific to children and adolescents, other studies have noted higher duration of TV viewing among short sleepers(9,15,27). Other studies have noted an increase in fat mass among short-sleeping children(10) and impaired cellular signaling in adipocytes of adults who were short-sleepers(32). These potential mechanisms have not been demonstrated in preschool children but involve elements of physiology that may also be relevant in this age range. We were unable to test the majority of these hypotheses relating short-sleep to obesity, though we noted higher TV viewing among short-sleepers. We also evaluated for cross-sectional associations between sleep amount and height and did not find any such association, suggesting that the association between shorter sleep and high BMI was not due to poor linear growth as a mechanism.
This study has several strengths, including its use of nationally representative data, adjustment for multiple potential confounders and assessment of longitudinal data to clarify these relationships over time. However, this study also had multiple limitations. Parental report of the time of sleep was used instead of measured sleep time, though prior studies have shown parental report to be within 20 minutes of actual sleep time(20). Napping was not recorded and may play a role in catching up on total sleep debt. A previous paper demonstrated that while nighttime sleep was associated with obesity, daytime sleep had no association with subsequent obesity at any age(13). Differences in BMI z-score between quintiles of sleep were modest (e.g., z-score difference of 0.28 between highest and lowest sleep quintile at age 5 years, corresponding to at 0.45 kg difference in weight on average); however, on a population basis relatively small differences in weight can have large public health implications(33).
Finally, it is important to note that this was an observational study that thus lacks the ability to conclude any true causality. Randomized trials of short vs. long duration of sleep have been performed in adults(29) and more recently in children(16), demonstrating an increase in food intake during the period of time that children were assigned to shorter sleep duration, providing plausibility regarding the possible causal nature behind these associations in childhood. Nevertheless, in our study, it remains possible that these associations are related to confounding variables for which we have failed to account. Overall, the continued association of these findings in childhood(9-14), including in longitudinal studies(11), supports the potential that earlier bedtimes and increased sleep may restrain childhood weight gain over time.
In conclusion, we found multiple cross-sectional and longitudinal links between short-sleep duration and later bedtime with weight status in a large cohort of American preschool and kindergarten children. These data confirm findings from other international studies and smaller cohorts and suggest the potential that increased sleep duration may constitute a modifiable means of restraining weight gain in early life. While interventional trials are needed to solidify these associations, it seems reasonable for pediatricians to recommend earlier bedtimes to promote longer sleep duration for children at risk for obesity.
Supplementary Material
What is known about this subject.
Short sleep duration in school-age children and adolescents has been linked to heavier weight status.
Over the past 20 years sleep amount has decreased among children, coincident with increased rates of obesity.
What this study adds.
The association between short sleep duration and increased BMI z-score following adjustment for multiple confounders is present already by preschool in a large, nationally-representative sample.
Later bedtime in particular was associated with heavier weight status and increased weight gain over time.
Acknowledgments
Funding source: 5K08HD060739-03 (MDD).
Footnotes
Conflict of interest statement: The authors have no conflicts of interest
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of Obesity and Trends in Body Mass Index Among US Children and Adolescents, 1999-2010. Jama-Journal of the American Medical Association. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garn SM, Lavelle M. 2-Decade Follow-Up of Fatness in Early-Childhood. American Journal of Diseases of Children. 1985;139(2):181–185. doi: 10.1001/archpedi.1985.02140040083033. [DOI] [PubMed] [Google Scholar]
- 3.Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss - An update of the 1997 American Heart Association Scientific Statement on obesity and heart disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113(6):898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 4.Wiggs L. Behavioural aspects of children's sleep. Archives of Disease in Childhood. 2009;94(1):59–62. doi: 10.1136/adc.2007.125278. [DOI] [PubMed] [Google Scholar]
- 5.Patel SR, Hu FB. Short sleep duration and weight gain: A systematic review. Obesity. 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cappuccio FP, Cooper D, D'Elia L, et al. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European heart journal. 2011;32(12):1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 7.Chen XL, Beydoun MA, Wang YF. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis Obesity. 2008;16(2):265–274. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 8.Cohen GJ. American Academy of Pediatrics Guide to Your Child's Sleep. New York: Villard; 1999. [Google Scholar]
- 9.Padez C, Mourao I, Moreira P, et al. Long Sleep Duration and Childhood Overweight/Obesity and Body Fat. American Journal of Human Biology. 2009;21(3):371–376. doi: 10.1002/ajhb.20884. [DOI] [PubMed] [Google Scholar]
- 10.von Kries R, Toschke AM, Wurmser H, et al. Reduced risk for overweight and obesity 5-and 6-y-old children by duration of sleep - a cross-sectional study. International Journal of Obesity. 2002;26(5):710–716. doi: 10.1038/sj.ijo.0801980. [DOI] [PubMed] [Google Scholar]
- 11.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Development. 2007;78(1):309–323. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell JA, Rodriguez D, Schmitz KH, et al. Sleep Duration and Adolescent Obesity. Pediatrics. 2013;131(5):E1428–E1434. doi: 10.1542/peds.2012-2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell JF, Zimmerman FJ. Shortened Nighttime Sleep Duration in Early Life and Subsequent Childhood Obesity. Archives of Pediatrics & Adolescent Medicine. 2010;164(9):840–845. doi: 10.1001/archpediatrics.2010.143. [DOI] [PubMed] [Google Scholar]
- 14.Agras WS, Hammer LD, McNicholas F, et al. Risk factors for childhood overweight: A prospective study from birth to 9.5 years. Journal of Pediatrics. 2004;145(1):20–25. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 15.Magee C, Caputi P, Iverson D. Lack of sleep could increase obesity in children and too much television could be partly to blame. Acta Paediatrica. 2014;103(1):E27–E31. doi: 10.1111/apa.12447. [DOI] [PubMed] [Google Scholar]
- 16.Hart CN, Carskadon MA, Considine RV, et al. Changes in Children's Sleep Duration on Food Intake, Weight, and Leptin. Pediatrics. 2013;132(6):E1473–E1480. doi: 10.1542/peds.2013-1274. [DOI] [PubMed] [Google Scholar]
- 17.Hiscock H, Scalzo K, Canterford L, et al. Sleep duration and body mass index in 0-7-year olds. Archives of Disease in Childhood. 2011;96(8):735–739. doi: 10.1136/adc.2010.204925. [DOI] [PubMed] [Google Scholar]
- 18.Knutson KL, Lauderdale DS. Sleep duration and overweight in adolescents: Self-reported sleep hours versus time diaries. Pediatrics. 2007;119(5):E1056–E1062. doi: 10.1542/peds.2006-2597. [DOI] [PubMed] [Google Scholar]
- 19.Snow K, Derecho A, Wheeless S, et al. Early Childhood Longitudinal Study-Birth Cohort (ECLS-B): Preschool year data file user's manual (2005-2006) (NCES2008-024) Washington, DC: U.S. Department of Education, Institute of Education Sciences, National Center for Education Statistics; 2007. [Google Scholar]
- 20.Werner H, Molinari L, Guyer C, et al. Agreement rates between actigraphy, diary, and questionnaire for children's sleep patterns: recommendations for clinical and research practice. Journal of Sleep Research. 2008;17:127–128. doi: 10.1001/archpedi.162.4.350. [DOI] [PubMed] [Google Scholar]
- 21.Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics. 2003;111(2):302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 22.Mindell JA, Owens J, Alves R, et al. Give children and adolescents the gift of a good night's sleep: A call to action. Sleep Medicine. 2011;12(3):203–204. doi: 10.1016/j.sleep.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Matricciani LA, Olds TS, Blunden S, et al. Never Enough Sleep: A Brief History of Sleep Recommendations for Children. Pediatrics. 2012;129(3):548–556. doi: 10.1542/peds.2011-2039. [DOI] [PubMed] [Google Scholar]
- 24.Adair RH, Bauchner H. Sleep problems in childhood. Curr Probl Pediatr. 1993;23(4):147–170. doi: 10.1016/0045-9380(93)90011-z. discussion 142. [DOI] [PubMed] [Google Scholar]
- 25.Morgenthaler TI, Owens J, Alessi C, et al. Practice parameters for behavioral treatment of bedtime problems and night wakings in infants and young children - An American Academy of Sleep Medicine report. Sleep. 2006;29(10):1277–1281. [PubMed] [Google Scholar]
- 26.Golley RK, Maher CA, Matricciani L, et al. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. International Journal of Obesity. 2013;37(4):546–551. doi: 10.1038/ijo.2012.212. [DOI] [PubMed] [Google Scholar]
- 27.Olds TS, Maher CA, Matricciani L. Sleep Duration or Bedtime? Exploring the Relationship between Sleep Habits and Weight Status and Activity Patterns. Sleep. 2011;34(10):1299–1307. doi: 10.5665/SLEEP.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wolfson AR, Spaulding NL, Dandrow C, et al. Middle school start times: the importance of a good night's sleep for young adolescents. Behavioral sleep medicine. 2007;5(3):194–209. doi: 10.1080/15402000701263809. [DOI] [PubMed] [Google Scholar]
- 29.Markwald RR, Melanson EL, Smith MR, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(14):5695–5700. doi: 10.1073/pnas.1216951110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spiegel K, Tasali E, Penev P, et al. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 31.Knutson KL, Spiegel K, Penev P, et al. The metabolic consequences of sleep deprivation. Sleep Medicine Reviews. 2007;11(3):163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Broussard JL, Ehrmann DA, Van Cauter E, et al. Impaired Insulin Signaling in Human Adipocytes After Experimental Sleep Restriction A Randomized, Crossover Study. Annals of Internal Medicine. 2012;157(8):549–558. doi: 10.7326/0003-4819-157-8-201210160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ludwig DS. Childhood obesity - The shape of things to come. New England Journal of Medicine. 2007;357(23):2325–2327. doi: 10.1056/NEJMp0706538. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


