Abstract
Objective
Dysregulation across multiple physiological systems, referred to as allostatic load, has pervasive consequences for an individual’s health. The present study examined whether allostatic load is associated with personality and personality changes during a 4-year follow-up.
Method
A total of 5200 participants aged from 50 to 99 years old (59.5% women, mean age= 66.91 years, SD= 8.88) from the Health and Retirement Study provided data on cardiovascular, metabolic, and immune markers at baseline and personality both at baseline and four years later.
Results
Higher allostatic load was related to higher neuroticism (β = .03, p =.042), lower extraversion (β = −.06, p < .001) and lower conscientiousness (β = −.06, p < .001) at baseline, and to declines in extraversion (β = −.03, p = .007), conscientiousness (β = −.04, p < .001), and agreeableness (β = −.02, p = .020) over the 4-year period, controlling for demographic covariates. A significant quadratic relation between allostatic load and changes in openness (β = −.03, p =.002) suggested that openness declines when individuals exceed a high level of cumulative physiological dysregulation. No association was found with changes in neuroticism.
Conclusion
Allostatic load is associated with personality change across adulthood and old age. The findings indicate that physiological dysregulation across multiple systems challenges personality stability and is associated with accelerated personality traits change.
Keywords: allostatic load, personality development, psychological aging
Allostatic load is a measure of physiological dysregulation across multiple systems that accumulates over the lifespan as a result of repeated cycles of physiological responses to environmental and psychosocial stressors (1). This cumulative biological dysregulation has pervasive consequences for physical and mental health. Individuals with higher allostatic load, for example, have more disability and functional limitations (2–4), lower bone strength (5), more cognitive impairment (6), and greater risk of major depression (7). Higher allostatic load also predicts a range of adverse health outcomes, including cardiovascular disease (8) and all-cause mortality (9). This multi-system physiological dysregulation tends to be stronger than any single biological system indicator in predicting health outcomes (6, 10). In this study, we examine whether allostatic load is associated with changes in personality —i.e. individuals’ characteristic way of feeling, thinking and behaving (11) —across adulthood and old age.
Personality traits play an important role for the health and well-being of older adults (12–14). Traits such as conscientiousness and neuroticism are associated consistently with a range of biomarkers, including metabolic (14), immune (15–17), and cardiovascular (18). It is likely, however, that this relation is reciprocal, and that physiological functioning may contribute to how individuals feel, behave, and think across adulthood and old age. From a theoretical standpoint, this assumption is consistent with the tenets of the Five Factor Theory of Personality, which argues that stability and change in personality are biologically driven (19). In addition, a growing body of research suggested that health patterns are predictive of personality development. For example, individuals with more chronic conditions tend to decline in extraversion, conscientiousness, openness to experiences, and emotional stability (12, 20). In addition, personality changes, such as decreased conscientiousness and increased neuroticism, have been observed in neurodegenerative diseases (21). These studies, however, have used self-reported measures of disease burden or have tracked personality changes using retrospective methods. To our knowledge, there has yet to be an empirical test of the direct relation between a multi-system index of biological alterations, as reflected by allostatic load, and personality development.
There are reasons to expect that the deviation of different regulatory systems from their normal operating range may be associated with changes in personality traits. Allostatic load, for example, has been associated with physical limitations and disease burden (2, 22), lower cardiorespiratory fitness (23–25), sleep disturbances (26), chronic fatigue symptoms (27), depressive symptoms (7), and lower cognitive functioning (6). In turn, these alterations in physical, emotional, and cognitive functioning have been found to shape personality over time, by reducing the tendency to be enthusiastic, self-disciplined and organized, emotionally stable, agreeable, or open to new experiences (12, 20, 21, 28). Allostatic load is also associated with lifestyle changes that may alter personality traits. For example, the decline in energy combined with the physical and functional impairment that result from allostatic load place limits on individuals’ lifestyles and daily activities, including restrictions in the ability to be physically active (29–31). In turn, a sedentary lifestyle has been associated with greater declines in extraversion, conscientiousness, openness, and agreeableness across adulthood and old age (32).
Using data from a large national sample of adults, the present study examined the association between allostatic load and patterns of personality development across adulthood and old age. Given that biological dysfunction across multiple systems alters physical, emotional, and cognitive resources, we expected individuals with greater allostatic load to have lower scores and steeper decline over time in emotional stability, extraversion, openness, agreeableness and conscientiousness.
Methods
Participants
Participants were drawn from the Health and Retirement Study (HRS), a nationally representative longitudinal study sponsored by the National Institute of Aging (Grant No. NIA U01AG009740) and conducted by the University of Michigan. Participants in HRS were Americans aged 50 and older and their spouses. Participants signed a consent form approved by the Institutional Review Board at the University of Michigan. HRS data is publically available for download at http://hrsonline.isr.umich.edu/. A random one-half of the HRS sample was pre-selected for an enhanced face-to-face interview in 2006. The interview included the collection of biomarker measurements and a psychosocial questionnaire, which had a personality assessment that participants completed at home and returned by mail. The participants in this half of the sample completed the personality assessment again in 2010. The other half of the sample was interviewed in 2008 for the first personality measure and biomarker measurements and provided the second personality assessment in 2012. Biomarker data are currently available only for the 2006 and the 2008 waves.
Data from the 2006–2010 and 2008–2012 samples were pooled. Only participants with complete demographic information (e.g., age, sex, race, ethnicity, and education), biomarker measurements, and personality data at baseline and follow-up were included in the analyses. Complete data at both baseline and follow-up were available from 5200 participants (59.5% women). Participants were, on average, 66.91 (SD=8.88) years old, had an average of 13.19 (SD=2.72) years of education, were 89.6% white, 8% African-American, and 2.4% other race, and 6.6% were Hispanic across all races (see supplemental material for attrition analysis).
Measures
Personality
Personality was assessed using the Midlife Development Inventory (33). Participants were asked how much 26 adjectives that assess neuroticism, conscientiousness, extraversion, openness, and agreeableness described themselves on a scale ranging from 1 “not at all” to 4 “a lot” (34). The adjectives were moody, worrying, nervous, and calm (neuroticism); outgoing, friendly, lively, active, and talkative (extraversion); creative, imaginative, intelligent, curious, broad minded, sophisticated, and adventurous (openness); organized, responsible, hardworking, careless, and thorough (conscientiousness); and helpful, warm, caring, softhearted, and sympathetic (agreeableness). Cronbach alphas for each trait at Wave 1 and Wave 2 respectively were as follows: .72 and .71 for neuroticism, .75 and .76 for extraversion, .79 and .79 for openness, .67 and .69 for conscientiousness, and .79 and .80 for agreeableness. Stability correlations between the baseline and follow-up personality scores were as follows: .64 (agreeableness), .65 (neuroticism), .67 (conscientiousness), .70 (openness) to .71 (extraversion).
Allostatic load
The biomarkers assessed in the HRS were used to compute the allostatic load index. Markers of cardiovascular functioning were systolic and diastolic blood pressure. Metabolic indicators included hemoglobin A1C (HbA1C), high density lipoprotein cholesterol (HDL), total cholesterol (TC), waist circumference, and cystatin C. The inflammation marker was C-reactive protein (CRP). Dried blood spots were used to assay for HbA1C, HDL, TC, cystatin C, and CRP. The participant’s finger was cleansed with an alcohol swab, pricked with a sterile lancet, and the blood droplets were placed on specially treated filter paper. Blood samples were assayed using a standard ELISA assay (35). Due to the skewed distribution for each blood biomarker, we took the natural log to normalize the distribution. From a sitting position, three blood pressure readings, 45 seconds apart, were taken using an Omron HEM-780 Intellisense Automated Blood Pressure Monitor on the participant’s left arm. Systolic and diastolic blood pressure were recorded and averaged across the three measurements (mmHg). Participants with at least one valid measure were included in the present sample. To measure waist circumference, participants were asked to stand up, remove any bulky clothing, point to their navel, and place a tape measure around their waist at the level of their navel. The interviewer checked to be sure that the tape measure was horizontal around the waist and snug but not tight. Waist circumference in inches was recorded. The allostatic load index was computed using the eight biomarkers. Z scores were computed for each biomarker and then averaged. Higher values indicate higher multi-system physiological dysregulation.
Covariates
Age (in years), sex (coded as 1 for men and 0 for women), race (coded as 1 for white and 0 for other), ethnicity (coded as 1 for Hispanic and 0 for not Hispanic) and educational level (in years) were included as covariates given their relation with personality change (36, 37). Age squared was also included given the non-linear changes in personality across adulthood (38).
Data Analysis
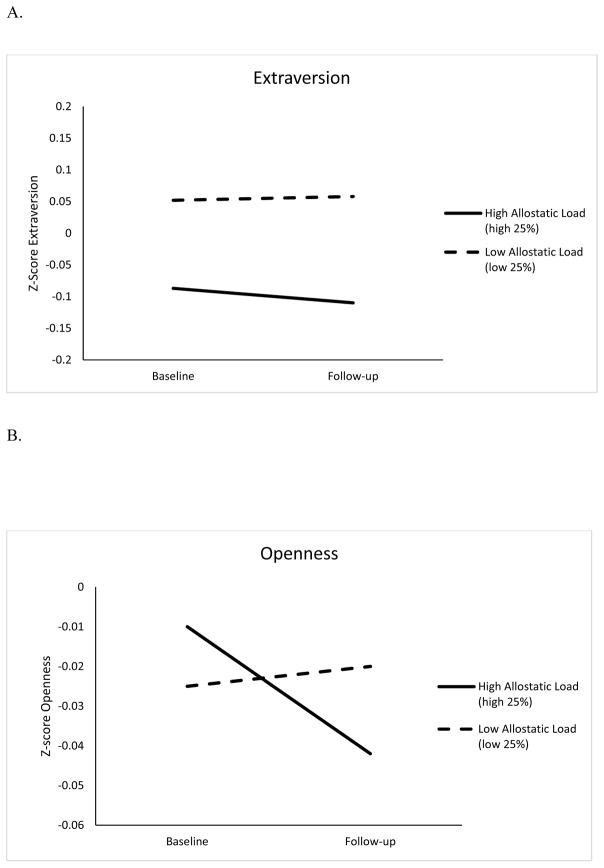
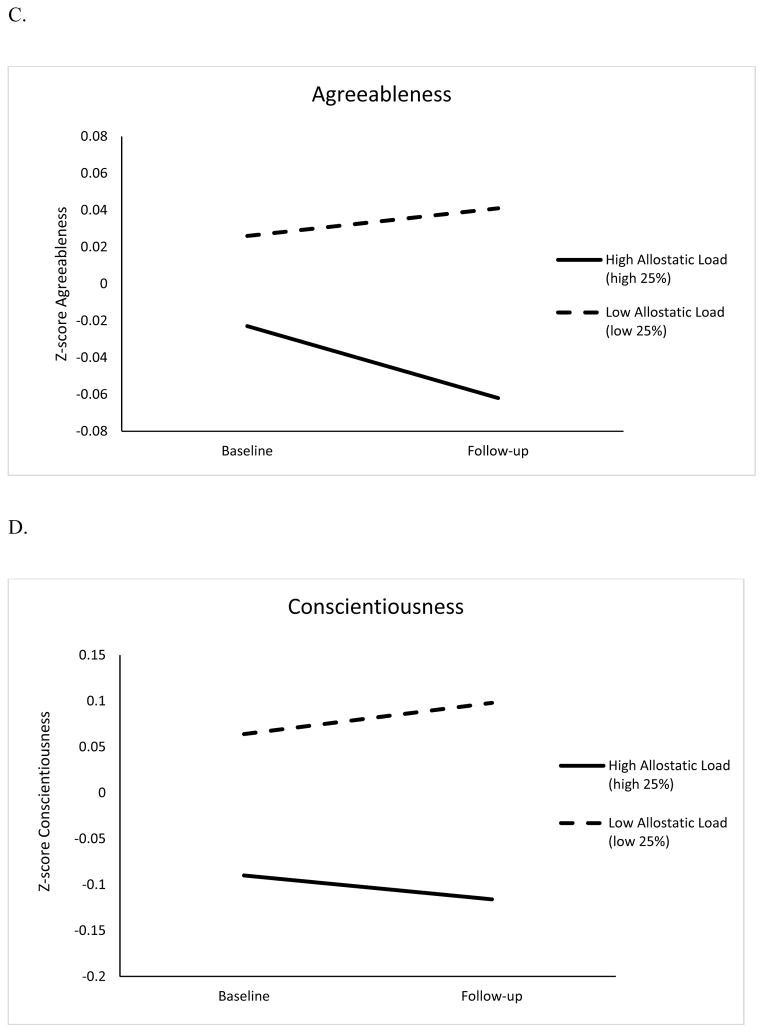
Regression analyses were first conducted to identify baseline associations between allostatic load and personality, controlling for demographic factors (age, age squared, sex, race, ethnicity, and education). Drawing upon existing research on factors associated with personality change (20, 28), to test whether physiological dysregulation was associated with change in personality traits, we regressed personality at follow-up on baseline personality, age, age squared, sex, race, ethnicity, education, and the allostatic load index. We further examined potential non-linear relations between physiological dysregulation and change in personality traits by including the squared term for allostatic load in additional regression analyses. Collinearity diagnostics revealed no problems with multicollinearity (i.e., all variance inflation factors were inferior to 2). Based on strategies used in previous research (39, 40), we estimated the contribution of allostatic load in terms of years of aging on personality changes. Specifically, the unstandardized coefficient for allostatic load was multiplied by its standard deviation and divided by the unstandardized coefficient for chronological age (39, 40). To provide a graphical representation of the results, we plotted changes in z-scores for each personality trait separately for those at the top and bottom quartiles of allostatic load. We also tested whether age, sex, race, ethnicity, and education moderated the association between allostatic load and personality change. To test for interactions, all continuous predictors were first mean centered. The same regression analysis as described above was conducted for each trait, with the demographic covariates, baseline personality, allostatic load, and an allostatic load by moderator (e.g., age, sex, education, race or ethnicity) interaction as predictors, and personality at follow-up as the outcome. Finally, as supplemental analysis, we examined the association between the individual markers of allostatic load and change in personality using the same procedure.
Results
Table 1 shows the descriptive statistics for all study variables. At baseline, a higher allostatic load was associated with higher neuroticism, lower extraversion, and lower conscientiousness (Table 2). Partially consistent with our hypothesis, the regression analysis indicated that allostatic load was related to changes in extraversion, agreeableness, and conscientiousness controlling for the demographic variables and baseline personality (Table 3). A significant quadratic relation was found between allostatic load and openness. Allostatic load was unrelated to changes in neuroticism (Table 3).
Table 1.
Means and Standard Deviations for the Variables Under Study at Time 1 and Time 2 (N= 5200)
| Variables | Time 1 | Time 2 |
|---|---|---|
| Sex, female, n (%) | 3092 (59.5%) | - |
| Race, white, n (%) | 4657 (89.6%) | - |
| Ethnicity, Hispanic, n (%) | 341 (6.6%) | - |
| Education, y | 13.19 (2.72) | - |
| Age, y | 66.91 (8.88) | - |
| Allostatic Load | 0.00 (0.44) | - |
| Neuroticism | 2.02 (0.59) | 1.97 (0.59)a |
| Extraversion | 3.22 (0.55) | 3.17 (0.56)a |
| Openness | 2.96 (0.54) | 2.91 (0.55)a |
| Agreeableness | 3.55 (0.46) | 3.52 (0.48)a |
| Conscientiousness | 3.40 (0.45) | 3.38 (0.48)a |
Note.
Significantly lower than the baseline value
Table 2.
Summary of Regression Analysis Predicting Baseline Personality Traits from Baseline Allostatic Load (N= 5200)
| Variables | Neuroticism | Extraversion | Openness | Agreeableness | Conscientiousness | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | |
| Sex | −0.11(.02) | −0.09*** | −0.11(.01) | −0.10*** | −0.03(.01) | −0.02 | −0.26(.01) | −0.28*** | −0.11(.01) | −0.12*** |
| Age | −0.01(.00) | −0.16*** | 0.00(.00) | 0.05*** | −0.00(.00) | −0.04** | 0.00(.00) | 0.04** | −0.00(.00) | −0.03 |
| Age Squared | 0.00(.00) | 0.05*** | −0.00(.00) | −0.07*** | −0.00(.00) | −0.03* | −0.00(.00) | −0.03* | −0.00(.00) | −0.04** |
| Educational level | −0.02(.00) | −0.11*** | 0.01(.00) | 0.06*** | 0.06(.00) | 0.29*** | 0.00(.00) | 0.02 | 0.02(.00) | 0.15*** |
| Race | 0.11(.03) | 0.05*** | −0.03(.02) | −0.02 | −0.04(.02) | −0.02 | 0.01(.02) | 0.00 | 0.05(.02) | 0.03* |
| Ethnicity | 0.12(.03) | 0.05*** | 0.06(.03) | 0.03* | 0.06(.03) | 0.03 | 0.00(.02) | 0.00 | 0.03(.02) | 0.02 |
| Baseline Allostatic Load | 0.04(.02) | 0.03* | −0.07(.02) | −0.06*** | 0.01(.02) | 0.00 | −0.02(.01) | −0.01 | −0.06(.01) | −0.06*** |
| Adjusted R2 | .05 | .02 | .08 | .08 | .04 | |||||
Note. B= Unstandardized Coefficients; SE= Standard Error; β = Standardized Coefficient
p < .05,
p < .01,
p <.001
Table 3.
Summary of Regression Analysis Predicting Follow-up Personality Traits from Baseline Allostatic Load (N= 5200)
| Variables | Neuroticism | Extraversion | Openness | Agreeableness | Conscientiousness | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | |
| Sex | −0.04(.01) | −0.04*** | −0.04(.01) | −0.03*** | −0.01(.01) | −0.01 | −0.10(.01) | −0.10*** | −0.04(.01) | −0.04*** |
| Age | −0.00(.00) | −0.00 | −0.001(.00) | −0.02* | −0.004(.00) | −0.06*** | −0.001(.00) | −0.03** | −0.003(.00) | −0.05*** |
| Age Squared | 0.00(.00) | 0.00 | −0.00(.00) | −0.03*** | −0.00(.00) | −0.00 | −0.00(.00) | −0.03* | −0.00(.00) | −0.00 |
| Educational level | −0.01(.00) | −0.05*** | 0.01(.00) | 0.03*** | 0.02(.00) | 0.08*** | 0.01(.00) | 0.04*** | 0.01(.00) | 0.07*** |
| Race | 0.04(.02) | 0.02 | −0.00(.02) | −0.00 | −0.03(.02) | −0.02 | 0.03(.02) | 0.02 | −0.01(.02) | −0.01 |
| Ethnicity | 0.01(.03) | 0.00 | 0.04(.02) | 0.02 | 0.00(.02) | 0.00 | −0.03(.02) | −0.02 | 0.01(.02) | 0.00 |
| Baseline Personality Trait | 0.63(.01) | 0.64*** | 0.72(.01) | 0.71*** | 0.69(.01) | 0.67*** | 0.65(.01) | 0.61*** | 0.69(.01) | 0.64*** |
| Baseline Allostatic Load | −0.01(.01) | −0.00 | −0.03(.01) | −0.03** | −0.01(.01) | −0.01 | −0.03(.01) | −0.02* | −0.05(.01) | −0.04*** |
| Adjusted R2 | .42 | .51 | .50 | .42 | .45 | |||||
| With Allostatic Load | ||||||||||
| Squared Tem Included | ||||||||||
| Sex | −0.04(.01) | −0.03** | −0.04(.01) | −0.03*** | −0.01(.01) | −0.01 | −0.10(.01) | −0.10*** | −0.04(.01) | −0.04*** |
| Age | −0.00(.00) | −0.00 | −0.001(.00) | −0.02* | −0.004(.00) | −0.06*** | −0.002(.00) | −0.03** | −0.003(.00) | −0.05*** |
| Age Squared | 0.00(.00) | 0.00 | −0.00(.00) | −0.03** | −0.00(.00) | −0.00 | −0.00(.00) | −0.03* | −0.00(.00) | −0.00 |
| Educational level | −0.01(.00) | −0.05*** | 0.01(.00) | 0.04*** | 0.02(.00) | 0.08*** | 0.01(.00) | 0.04*** | 0.01(.00) | 0.07*** |
| Race | 0.04(.02) | 0.02* | −0.00(.02) | −0.00 | −0.03(.02) | −0.02 | 0.03(.02) | 0.02 | −0.01(.02) | −0.01 |
| Ethnicity | 0.01(.03) | 0.00 | 0.04(.02) | 0.02 | 0.00(.02) | 0.00 | −0.03(.02) | −0.02 | 0.01(.02) | 0.00 |
| Baseline Personality Trait | 0.63(.01) | 0.64*** | 0.72(.01) | 0.71*** | 0.69(.01) | 0.67*** | 0.65(.01) | 0.61*** | 0.69(.01) | 0.64*** |
| Baseline Allostatic Load | −0.01(.01) | −0.00 | −0.03(.01) | −0.02* | −0.01(.01) | −0.00 | −0.02(.01) | −0.02* | −0.05(.01) | −0.04*** |
| Squared Allostatic Load | 0.04(.02) | 0.02 | −0.02(.02) | −0.01 | −0.06(.02) | −0.03** | −0.02(.02) | −0.01 | −0.01(.02) | −0.01 |
| Adjusted R2 | .42 | .51 | .50 | .42 | .45 | |||||
Note. B= Unstandardized Coefficients; SE= Standard Error; β = Standardized Coefficient.
p < .05,
p < .01,
p <.001
In the HRS sample, the average mean level of extraversion, openness, agreeableness, and conscientiousness declined over the 4-year period. Our results thus indicated that greater physiological dysregulation at baseline was associated with an even steeper decline in extraversion, openness, agreeableness, and conscientiousness than was found with normal aging. Specifically, the findings suggested that every one standard deviation increase in allostatic load was associated with roughly 0.02 to 0.04 SD decrease in these traits. In addition, we estimated that one-SD higher allostatic load was associated with 6.6 accelerated years of aging in openness, 7.3 more years of aging in conscientiousness, and 13.2 more years of aging in both extraversion and agreeableness. The size of the associations between the allostatic load and personality changes was comparable or stronger than the association of most demographic factors with personality (see Table 3). Furthermore, these associations were also observed without demographic covariates included in the model and when controlling for baseline and follow-up level of the other traits. The one exception was the association between allostatic load and change in agreeableness, which was reduced to non significance with the inclusion of the other traits (β= .00, p = .762). Figure 1 presents changes in the z-scores of extraversion, openness, agreeableness, and conscientiousness for individuals in the top and bottom 25% of the distribution of the allostatic load index, adjusted for the covariates.
Figure 1.
Changes in Extraversion (Panel A), Openness (Panel B), Agreeableness (Panel C), and Conscientiousness (Panel D) for Low (Bottom 25%) and High (High 25%) Allostatic Load, adjusted for baseline sociodemographic factors.
We next examined whether the association between allostatic load and personality change was moderated by demographic factors. Allostatic load was associated with a steeper decline in conscientiousness among women (βinteraction= .03, p = .014) and individuals of non-Hispanic origin (βinteraction= .02, p = .042). A more pronounced decline in extraversion was also found for individuals with higher education (βinteraction= −.02, p = .031) and individuals of non-Hispanic origin (βinteraction= .04, p < .001). Age and race did not moderate any of the associations.
Finally, partial correlations between each biomarker and each trait at baseline and follow-up, controlling for demographic factors are presented in Table 4. Of the individual biomarkers, regression analysis indicated that cystatin C was associated with a decrease in extraversion (β= −.02, p = .043) and HbA1C was associated with declines in agreeableness (β= −.03, p = .020) and conscientiousness (β= −.03, p = .003).
Table 4.
Partial Correlations between the Individual Biomarkers and Personality Traits at Baseline and Follow-Up, Controlling for Demographic Factors (N= 5200)
| Variables | Neuroticism | Extraversion | Openness | Agreeableness | Conscientiousness |
|---|---|---|---|---|---|
| HbA1C | .02 (.02) | −.03* (−.04**) | −.01 (−.02) | −.00 (−.03) | −.05*** (−.07***) |
| HDL | −.00 (−.01) | .03* (.03*) | .03 (.03*) | −.00 (−.01) | .05*** (.04**) |
| TC | .00 (−.01) | .02 (.02) | .04** (.03*) | −.00 (−.01) | .02 (.02) |
| WC | −.01 (.00) | −.07*** (−.06***) | −.01 (−.01) | −.00 (−.00) | −.10*** (−.10***) |
| CC | .03* (.03) | −.06*** (−.07***) | −.05*** (−.03*) | −.01 (−.02) | −.09*** (−.07***) |
| CRP | .03 (.02) | −.06*** (−.06***) | −.01 (−.01) | .01 (−.01) | −.05*** (−.06***) |
| SBP | .01 (−.01) | −.02 (−.03*) | .01 (−.01) | −.02 (−.02) | .01 (−.02) |
| DBP | .01 (.00) | −.02 (−.03*) | .02 (−.00) | −.02 (−.02) | −.01 (−.03*) |
Note. Partial Correlations controlling for age, age squared, sex, education, race and ethnicity. Values under brackets are partial correlations between biomarkers and follow-up personality traits.
p < .05,
p < .01,
p <.001
HbA1C: Hemoglobin A1C; HDL: High Density Lipoprotein; TC: Total Cholesterol; WC: Waist Circumference; CC: Cystatin C; CRP: C-Reactive Protein; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure.
Discussion
The purpose of this prospective study was to examine the relation between allostatic load, a measure of multi-system physiological dysregulation, and personality development over a four-year period in a large sample of Americans. At baseline, we found that individuals with higher allostatic load scored higher on neuroticism and lower on extraversion and conscientiousness. Over the 4-year follow-up, individuals with more dysregulation at baseline had a steeper decline in conscientiousness, extraversion, agreeableness, and openness. Surprisingly, allostatic load was unrelated to changes in neuroticism. Overall, the results suggest that individuals with physiological dysregulation have accelerated aging on most dimensions of personality. Furthermore, the strength of these associations was similar or stronger than those of the demographic factors. These findings provide support for physiologically-driven personality changes across adulthood and old age.
In our sample, allostatic load had the strongest association with declines in extraversion and conscientiousness. The cumulative dysregulation may result in a significant loss of energy (23–27). Individuals who are extraverted and conscientious have higher energy expenditures (41); the energy costs associated with higher physiological dysregulation may reduce the ability to sustain extraverted and conscientious behaviors. In addition, higher allostatic load is related to physical limitations (22), depressive symptoms (7), and cognitive declines (6), which have been associated with a reduced tendency to experience positive emotions and to be enthusiastic (extraversion) and a decline in the propensity to be self-disciplined, planful, and organized (conscientiousness) over time (28, 42). Individuals with higher physiological burden also have a restricted ability to be physically active (30), which is associated with steeper declines in extraversion and conscientiousness (32).
Allostatic load had a more modest association with declines in agreeableness. This finding adds to empirical evidence for disease-related changes in this trait (20). Allostatic load is related to an increased risk of depressive symptoms (7), which have been recently found to lead to a decline in agreeableness (28). In addition, a physically active lifestyle has been found to mitigate declines in agreeableness (32). The lifestyle limitations associated with higher allostatic load may thus restrict individuals’ prosocial orientations and abilities to be socially engaged. The loss of resources resulting from multi-system physiological dysregulation may also generate negative interpersonal reactions, such as irritability or anger, reflected in lower agreeableness over time.
The decline in openness to experience occurred only when individuals exceeded a higher multi-system physiological dysregulation at baseline. This result suggests that the propensity to seek novelty and variety may be relatively unaffected by allostatic load up to a point that past which individuals may not be able to compensate for the accumulated physiological burden. In this case, compounded depletion of energy and physical, emotional, and cognitive resources may challenge people’s ability to maintain an open mind and the desire to engage in a variety of activities. In addition, individuals who exceed a given threshold of allostatic load are exposed to an increased risk of disease (4), which may lead them to be less exploratory and to prefer familiar activities and close relationships (12).
Our hypothesis for an association between allostatic load and increases in neuroticism over time was not confirmed. Our results indicate that individuals who experience multi-system physiological dysregulation present a higher propensity to experience distress and negative emotions at baseline but not over time. This finding is consistent with reports of a cross-sectional relationship between higher allostatic load and acute depressive symptoms (7, 43), which fades over time (43). Therefore, cumulative physiological dysregulation may have acute emotional and affective manifestations that are expressed temporarily in higher emotional instability but may not be sufficiently persistent over time to translate in changes in neuroticism.
These findings indicate that physiological dysregulation is associated with a deviation of personality traits from their normative pattern of development. More specifically, allostatic load may be a risk factor for maladaptive personality trajectories that have been associated with a range of negative psychological, cognitive, and health-related outcomes (14, 44, 45). In addition, allostatic load could be a potential explanatory factor for the association between major life events and personality changes (37, 46). The experience of adverse life events, or chronic exposure to threatening situations, may generate stress-related physiological dysregulation across multiple systems, leading to maladaptive personality trajectories.
The present study adds to existing knowledge on the factors associated with personality development. Previous research has focused primarily on the effect of demographic factors, such as ethnicity and education (36), and of contextual/environmental factors, such as life experiences and normative life events (37, 46–48). Although health-related personality changes have been identified, previous studies have almost exclusively focused on self-reported measures of health and disease (20, 49) or have retrospectively tracked personality changes among clinical samples, such as Alzheimer’s disease patients (42). Although self-report measures have good validity, they are potentially subject to bias due to the self-report method. Therefore, this study extends previous research by providing evidence of a link between a cluster of laboratory-based biomarker measures and personality development. The use of such a cluster of mainly non-symptomatic biomarkers extends existing knowledge toward a more distal health factor represented by the physiological dysregulation, and reduces potential bias due to shared methods of previous studies. Nevertheless, it is reassuring that previous research based mostly on self-report measures generated results that are mostly consistent with the findings of this study that relied on physical and laboratory-based assessments. In addition, the findings from this study are consistent with the Five Factor Theory, which postulates that personality stability and change are mainly biologically driven (19). Importantly, this study demonstrates that beyond genetics, physiological factors are associated with patterns of personality development.
The current study has limitations that should be considered when interpreting the results. It is possible that attrition may have influenced the findings and that additional statistical modeling thereof would yield different results. The generalizability of our findings is limited to some extent by the positive selection of the longitudinal participants. The effects observed in the study may underestimate the true association of allostatic load with personality development given that participants without complete data had higher physiological dysregulation across systems, and thus could have experienced more change in their personality. In addition, given that biomarkers were available at only one wave in the HRS, the present study focused only on the predictive value of the level of physiological dysregulation on personality development. As such, it is possible that the observed associations might be the results of changes in personality that started to occur before the assessment of allostatic load. Specifically, such changes may have caused the higher allostatic load observed among those individuals who declined more in extraversion, openness, agreeableness, and conscientiousness. Future research is needed to test whether accumulated physiological burden over time is associated with personality changes, and vice-versa. In addition, both higher allostatic load and changes in personality may be attributable to a third variable, such as shared genetic factors. This study also relied on a brief measure of personality; detailed measures of personality facets would have provided a more in-depth understanding of the association between allostatic load and personality change. Finally, the allostatic load index only includes markers of metabolic, cardiovascular, and immune functions, considered as secondary mediators in the process leading to allostatic load (10). Future research could expand this measure to include markers of hypothalamic–pituitary–adrenal axis, or other markers of sympathetic and parasympathetic nervous system functioning, such as cortisol or brain-derived neurotrophic factors (50).
Despite these limitations, the study indicates that allostatic load is associated with patterns of personality development across adulthood and old age. Specifically, cumulative physiological dysregulation across multiple systems challenges individuals’ characteristic ways of feeling, thinking, and behaving, and is associated with a pattern of maladaptive changes in personality. This study is a step toward a better understanding of the biological underpinning of personality development.
Supplementary Material
Abbreviations
- HRS
Health and Retirement study
Footnotes
In additional analyses, we used a different method for computing allostatic load. Drawing upon McEwen (2000), allostatic load was measured by summing the number of parameters for which the subject fell into the top quartile (except HDL cholesterol for which membership in the lowest quartile corresponds to highest risk). Using this method, the pattern of results was identical for extraversion and conscientiousness. Although the results for agreeableness and openness were not significant, the direction of the relations was unchanged.
Conflicts of Interest and Source of Funding: None
References
- 1.McEwen BS. Allostasis and allostatic load: Implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22:108–24. doi: 10.1016/S0893-133X(99)00129-3. [DOI] [PubMed] [Google Scholar]
- 2.Karlamangla AS, Singer BH, McEwen BS, Rowe JW, Seeman TE. Allostatic load as a predictor of functional decline. MacArthur studies of successful aging. J Clin Epidemiol. 2002;55:696–710. doi: 10.1016/s0895-4356(02)00399-2. [DOI] [PubMed] [Google Scholar]
- 3.Read S, Grundy E. Allostatic load and health in the older population of England: a crossed-lagged analysis. Psychosom Med. 2014;76:490–6. doi: 10.1097/PSY.0000000000000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35:2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Mori T, Karlamangla AS, Merkin SS, Crandall CJ, Binkley N, Greendale GA, Seeman TE. Multi-system dysregulation and bone strength: Finding from the Study of Midlife in the United States. J Clin Endocrinol Metab. 2014;99:1843–51. doi: 10.1210/jc.2013-3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karlamangla AS, Miller-Martinez D, Lachman ME, Tun PA, Koretz A, Seeman TM. Biological correlates of adult cognition: Midlife in the United States (MIDUS) Neurobiol Aging. 2014;35:387–94. doi: 10.1016/j.neurobiolaging.2013.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kobrosly RW, Seplaki CL, Cory-Slechta DA, Moynihan J, van Wijngaarden E. Multi-system physiological dysfunction is associated with depressive symptoms in a population-based sample of older adults. Int J Geriatr Psychiatry. 2013;28:718–27. doi: 10.1002/gps.3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation–allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997;157:2259–68. [PubMed] [Google Scholar]
- 9.Karlamangla AS, Singer BH, Seeman TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosom Med. 2006;68:500–7. doi: 10.1097/01.psy.0000221270.93985.82. [DOI] [PubMed] [Google Scholar]
- 10.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA. 2001;98:4770–5. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Digman JM. Personality structure: Emergence of the five-factor model. Annu Rev Psychol. 1990;41:417–40. [Google Scholar]
- 12.Sutin AR, Zonderman AB, Ferrucci L, Terracciano A. Personality traits and chronic disease: Implications for adult personality development. J Gerontol B Psychol Sci Soc Sci. 2013;68:912–20. doi: 10.1093/geronb/gbt036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sutin AR, Costa PT, Jr, Uda M, Ferrucci L, Schlessinger D, Terracciano A. Personality and metabolic syndrome. Age (Dordr) 2010;32:513–9. doi: 10.1007/s11357-010-9153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Human LJ, Biesanz JC, Miller GE, Chen E, Lachman ME, Seeman TE. Is change bad? Personality change is associated with poorer psychological health and greater metabolic syndrome in midlife. J Pers. 2013;81:249–60. doi: 10.1111/jopy.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luchetti M, Barkley JM, Stephan Y, Terracciano A, Sutin AR. Five-Factor Model Personality Traits and inflammatory markers: New data and a meta-analysis. Psychoneuroendocrinology. 2014;50:181–93. doi: 10.1016/j.psyneuen.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sutin AR, Terracciano A, Deiana B, Naitza S, Ferrucci L, Uda M, Schlessinger D, Costa PT., Jr High neuroticism and low conscientiousness are associated with interleukin-6. Psychol Med. 2010;40:1485–93. doi: 10.1017/S0033291709992029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turiano NA, Mroczek DK, Moynihan J, Chapman BP. Big 5 personality traits and interleukin-6: Evidence for “healthy neuroticism” in a U.S. Population sample. Brain Behav Immun. 2013;28:83–9. doi: 10.1016/j.bbi.2012.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Terracciano A, Strait J, Scuteri A, Meirelles O, Sutin AR, Tarasov K, Ding J, Marongiu M, Orru M, Pilia MG, Cucca F, Lakatta E, Schlessinger D. Personality traits and circadian blood pressure patterns: A seven year prospective study. Psychosom Med. 2014;76:237–43. doi: 10.1097/PSY.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCrae RR, Costa PT, Jr, Ostendorf F, Angleitner A, Hrebícková M, Avia MD, Sanz J, Sánchez-Bernardos ML, Kusdil ME, Woodfield R, Saunders PR, Smith PB. Nature over nurture: temperament, personality, and life span development. J Pers Soc Psychol. 2000;78:173–86. doi: 10.1037//0022-3514.78.1.173. [DOI] [PubMed] [Google Scholar]
- 20.Jokela M, Hakulinen C, Singh-Manoux A, Kivimäki M. Personality change associated with chronic diseases: Pooled analysis of four prospective cohort studies. Psychol Med. 2014;44:2629–40. doi: 10.1017/S0033291714000257. [DOI] [PubMed] [Google Scholar]
- 21.Robins-Wahlin TB, Byrne GJ. Personality changes in Alzheimer’s disease: A systematic review. Int J Geriatr Psychiatry. 2011;26:1019–29. doi: 10.1002/gps.2655. [DOI] [PubMed] [Google Scholar]
- 22.Gruenewald TL, Seeman TE, Karlamangla AS, Sarkisian CA. Allostatic load and frailty in older adults. J Am Geriatr Soc. 2009;57:1525–31. doi: 10.1111/j.1532-5415.2009.02389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barlow CE, LaMonte MJ, Fitzgerald SJ, Kampert JB, Perrin JL, Blair SN. Cardiorespiratory fitness is an independent predictor of hypertension incidence among initially normotensive healthy women. Am J Epidemiol. 2006;163:142–50. doi: 10.1093/aje/kwj019. [DOI] [PubMed] [Google Scholar]
- 24.Hassinen M, Lakka TA, Savonen K, Litmanen H, Kiviaho L, Laaksonen DE, Komulainen P, Rauramaa R. Cardiorespiratory fitness as a feature of metabolic syndrome in older men and women: The Dose–Responses to Exercise Training study (DR’s EXTRA) Diabetes Care. 2008;31:1242–7. doi: 10.2337/dc07-2298. [DOI] [PubMed] [Google Scholar]
- 25.Kullo IJ, Khaleghi M, Hensrud DD. Markers of inflammation are inversely associated with VO2 max in asymptomatic men. J Appl Physiol. 2007;102:1374–9. doi: 10.1152/japplphysiol.01028.2006. [DOI] [PubMed] [Google Scholar]
- 26.Chen X, Redline S, Shields AE, Williams DR, Williams MA. Associations of allostatic load with sleep apnea, insomnia, short sleep duration, and other sleep disturbances: Findings from the National Health and Nutrition Examination Survey 2005 to 2008. Ann Epidemiol. 2014;24:612–9. doi: 10.1016/j.annepidem.2014.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goertzel BN, Pennachin C, de Souza Coelho L, Maloney EM, Jones JF, Gurbaxani B. Allostatic load is associated with symptoms in chronic fatigue syndrome patients. Pharmacogenomics. 2006;7:485. doi: 10.2217/14622416.7.3.485. [DOI] [PubMed] [Google Scholar]
- 28.Hakulinen C, Elovainio M, Pulkki-Raback L, Virtanen M, Kivimäki M, Jokela M. Personality and depressive symptoms: Individual participant meta-analysis of 10 cohort studies. Depress Anxiety. 2015 doi: 10.1002/da.22376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carriere I, Pérès K, Ancelin ML, Gourlet V, Berr C, Barberger-Gateau P, Bouillon K, Kivimaki M, Ritchie K, Akbaraly T. Metabolic syndrome and disability: Findings from the prospective three-city study. J Gerontol A Biol Sci Med Sci. 2014;69:79–86. doi: 10.1093/gerona/glt101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuo HK, Bean JF, Yen CJ, Leveille SG. Linking C-reactive protein to late-life disability in the National Health and Nutrition Examination Survey (NHANES) 1999–2002. J Gerontol A Biol Sci Med Sci. 2006;61:380–7. doi: 10.1093/gerona/61.4.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu P, Wagle N, Goldman N, Weinstein M, Seeman TE. The associations between socioeconomic status, allostatic load and measures of health in older Taiwanese persons: Taiwan Social Environment and Biomarkers of Aging Study. J Biosoc Sci. 2007;39:545–56. doi: 10.1017/S0021932006001556. [DOI] [PubMed] [Google Scholar]
- 32.Stephan Y, Sutin AR, Terracciano A. Physical activity and personality development across adulthood and old age: Evidence from two longitudinal studies. J Res Pers. 2014;49:1–7. doi: 10.1016/j.jrp.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lachman ME, Weaver SL. Unpublished Technical Report. Brandeis University; 1997. Midlife Development Inventory (MIDI) personality scales: Scale construction and scoring. [Google Scholar]
- 34.Graham EK, Lachman ME. Personality stability is associated with better cognitive performance in adulthood: Are the stable more able? J Gerontol B Psychol Sci Soc Sci. 2012;67:545–54. doi: 10.1093/geronb/gbr149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Crimmins E, Faul J, Kim JK, Guyer H, Langa K, Ofstedal MB, Sonnega A, Wallace R, Weir D. Documentation of biomarkers in the 2006 and 2008 Health and Retirement. Ann Arbor, MI: Survey Research Center University of Michigan; 2013. [Google Scholar]
- 36.Löckenhoff CE, Terracciano A, Bienvenu OJ, Patriciu NS, Nestadt G, McCrae RR, Eaton WW, Costa PT., Jr Ethnicity, education, and the temporal stability of personality traits in the East Baltimore Epidemiologic Catchment Area Study. J Res Pers. 2008;42:577–98. doi: 10.1016/j.jrp.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Specht J, Egloff B, Schmukle SC. Stability and change of personality across the life course: The impact of age and major life events on mean-level and rank-order stability of the Big Five. J Pers Soc Psychol. 2011;101:862–82. doi: 10.1037/a0024950. [DOI] [PubMed] [Google Scholar]
- 38.Lucas RE, Donnellan MB. Personality development across the life span: Longitudinal analyses with a national sample from Germany. J Pers Soc Psychol. 2011;101:847–61. doi: 10.1037/a0024298. [DOI] [PubMed] [Google Scholar]
- 39.Infurna FJ, Gerstorf D. Linking perceived control, physical activity, and biological health to memory change. Psychol Aging. 2013;28:386–401. doi: 10.1037/a0033327. [DOI] [PubMed] [Google Scholar]
- 40.Infurna FJ, Gerstorf D. Perceived control relates to better functional health and lower cardio-metabolic risk: The mediating role of physical activity. Health Psychol. 2014;33:85–94. doi: 10.1037/a0030208. [DOI] [PubMed] [Google Scholar]
- 41.Terracciano A, Schrack JA, Sutin AR, Chan W, Simonsick EM, Ferrucci L. Personality, metabolic rate and aerobic capacity. PLoS One. 2013;8:e54746. doi: 10.1371/journal.pone.0054746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pocnet C, Rossier J, Antonietti JP, Von Gunten A. Personality features and cognitive level in patients at an early stage of Alzheimer’s disease. Pers Individ Dif. 2013;54:174–9. [Google Scholar]
- 43.Juster RP, Marin MF, Sindi S, Nair NP, Ng YK, Pruessner JC, Lupien SJ. Allostatic load associations to acute, 3-year and 6-year prospective depressive symptoms in healthy older adults. Physiol Behav. 2011;104:360–4. doi: 10.1016/j.physbeh.2011.02.027. [DOI] [PubMed] [Google Scholar]
- 44.Mroczek DK, Spiro A. Personality change influences mortality in older men. Psychol Sci. 2007;18:371–6. doi: 10.1111/j.1467-9280.2007.01907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Turiano NA, Pitzer L, Armour C, Karlamangla A, Ryff CD, Mroczek DK. Personality trait level and change as predictors of health outcomes: Findings from a national study of Americans (MIDUS) J Gerontol B Psychol Sci Soc Sci. 2012;67:4–12. doi: 10.1093/geronb/gbr072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Löckenhoff CE, Terracciano A, Patriciu NS, Eaton WW, Costa PT., Jr Self-reported extremely adverse life events and longitudinal changes in five-factor model personality traits in an urban sample. J Trauma Stress. 2009;22:53–9. doi: 10.1002/jts.20385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ogle CM, Rubin DC, Siegler IC. Changes in neuroticism following trauma exposure. J Pers. 2014;82:93–102. doi: 10.1111/jopy.12037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jeronimus BF, Ormel J, Aleman A, Penninx BW, Riese H. Negative and positive life events are associated with small but lasting change in neuroticism. Psychol Med. 2013;43:2403–15. doi: 10.1017/S0033291713000159. [DOI] [PubMed] [Google Scholar]
- 49.Takahashi Y, Edmonds GE, Jackson JJ, Roberts BW. Longitudinal correlated changes in conscientiousness, preventative health-related behaviors, and self-perceived physical health. J Pers. 2013;81:417–27. doi: 10.1111/jopy.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Terracciano A, Lobina M, Piras MG, Mulas A, Cannas A, Meirelles O, Sutin AR, Zonderman AB, Uda M, Crisponi L, Schlessinger D. Neuroticism, depressive symptoms, and serum BDNF. Psychosom Med. 2011;73:638–42. doi: 10.1097/PSY.0b013e3182306a4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.