Abstract
Objective To determine the subsequent pattern of emergency admissions in older people with a history of frequent emergency admissions.
Design Analysis of routine admissions data from NHS hospitals using hospital episode statistics (HES) in England.
Subjects Individual patients aged ≥ 65, ≥ 75, and ≥ 85 who had at least two emergency admissions in 1997-8.
Main outcome measures Emergency admissions and bed use in this “high risk” cohort of patients were counted for the next five years and compared with the general population of the same age. No account was taken of mortality as the analysis was designed to estimate the future use of beds in this high risk cohort.
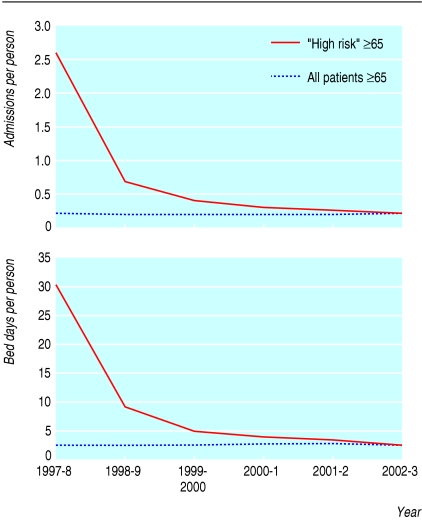
Results Over four to five years, admission rates and bed use in the high risk cohorts fell to the mean rate for older people. Although patients ≥ 65 with two or more such admissions were responsible for 38% of admissions in the index year, they were responsible for fewer than 10% of admissions in the following year and just over 3% five years later.
Conclusion Patients with multiple emergency admissions are often identified as a high risk group for subsequent admission and substantial claims are made for interventions designed to avoid emergency admission in such patients. Simply monitoring admission rates cannot assess interventions designed to reduce admission among frail older people as rates fall without any intervention. Comparison with a matched control group is necessary. Wider benefits than reduced admissions should be considered when introducing intensive case management of older people.
Introduction
Efforts to improve the effectiveness and efficiency of health services often focus on reducing inpatient stays, the most expensive element of health care. A systematic review found that integrated care experiments in elderly people could reduce rates of admission, though the effects are highly dependent on the system of care and the nature of the intervention.1 Case management of patients at risk of admission has also been proposed as a way of reducing the risk of readmission, but a recent review found only limited evidence that this approach reduces use of health services.2
One way of identifying patients at risk of admission is to select those with recent emergency or unscheduled admissions. Published risk assessment tools identify past admissions, especially unscheduled admissions, as important risk factors for subsequent admission.3-5 For example, a history of two or more emergency admissions in the previous year is the principle factor used to identify patients to enrol in an intensive case management programme for older people currently being introduced in the United Kingdom by Evercare,6 an arm of the US healthcare provider United Health Group. This initiative uses specially trained nurses to monitor vulnerable older people at home and is modelled on similar Evercare interventions in the United States7 that are associated with reduced risk of readmission to hospital.8
Evercare is not alone in using history of unplanned admissions as a means of identifying patients at risk of future admission. The same approach has been used as the entry criterion for several trials9-11 and as one of the criteria for case management in the new NHS policy on long term conditions.12
Sometimes, outcomes of interventions are assessed purely in terms of reduction in admissions among a cohort of older people without any reference to a control group, the assumption being that patients identified at high risk on the basis of their previous admissions would continue to be at high risk of admission in the absence of the intervention.
Since April 1997, administrative data have been available in England that make it possible to track emergency admission patterns of individual patients. We used these data to establish the natural history of emergency admissions and bed use of older patients with a history of multiple unscheduled admissions.
Method
Hospital episode statistics (HES) contain records for all NHS patients admitted to English hospitals in each financial year (April 1 to March 31). Since 1997-8 HES has contained a field—derived from the patient's NHS number, postcode, date of birth, and sex—that enables separate spells by an individual patient to be tracked within any year and in subsequent years. From the full set of HES records for the index year 1997-8 (n = 11 544 551) we selected a cohort of “high risk” patients (n = 227 206) who had two or more emergency finished inpatient spells in the year, were discharged alive at the end of their last spell, and were aged ≥ 65 when admitted. We tracked this high risk cohort of patients through five years of HES data (1998-9 to 2002-3) and identified subsequent emergency admissions and the length of stay for these admissions.
We wanted to compare the admissions and bed days of the 1997-8 high risk cohort with the admissions and bed days of the general population of those aged ≥ 65 in 1997-8. To do this we needed to allow for the different numbers at risk in the two cohorts. One method would have been to calculate admission rates in a particular year for the two groups with the denominator equal to the number alive in that year. This was not possible with our data, however, as we did not know how many of those in the 1997-8 high risk cohort were still alive in 1998-9 etc. We therefore compared admission rates (and bed day rates) using the initial sizes of the high risk and general population cohorts in 1997-8 as the denominator in all years. Thus, for example, the emergency admission rate for the 1997-8 high risk cohort in 1999-2000 (0.387 admissions per patient) was the total number of finished emergency spells in 1999-2000 (87 834) for the 1997-8 cohort divided by 227 206. We calculated analogous rates for members of the high risk group aged ≥ 75 and ≥ 85.
We deliberately made no attempt to take account of deaths of patients in the high risk groups studied as our intention was to estimate the future emergency use of beds by the 1997-8 high risk cohort, rather than to estimate the admission rate for members of the cohort alive in any given year. By modelling the impact of including mortality in the calculations, we have previously shown that it makes only a small impact on the overall conclusions.13
In each year of HES data (1997-8 to 2002-3) we counted the number of emergency admissions and emergency bed days for all patients aged ≥ 65 in 1997-8, patients aged ≥ 66 in 1998-9, and so on. To ensure that the denominator for the calculation of admission rates for this population was as far as possible on the same basis as for the 1997-8 high risk cohort, we used the Office for National Statistics' population estimates based on the 2001 census to estimate the English population aged ≥ 65 in mid-1997.14 Thus, for example, the admission rate in 1999-2000 for the general population aged ≥ 65 in 1997-8 was the total number of emergency admissions for those aged ≥ 67 in 1999-2000 divided by the English population aged ≥ 65 in mid-1997. We performed analogous calculations for those aged ≥ 75 and those aged ≥ 85 in 1997.
To illustrate the sensitivity of being ≥ 65 and having two or more emergency admissions in an index year (1997-8) as a means of detecting those at high risk of admission in the following year, we also used the HES records to count patients who were ≥ 66 in 1998/9 and had at least two admissions in that year and the previous year. We were unable to calculate specificities because we did know how many patients who had two or more admissions in 1997-8 had died before 1998-9.
Results
The table and figure show that the total admissions and bed days for older people with a history of two or more unscheduled admissions in an index year decreased sharply in subsequent years (table). Members of the high risk cohort aged 65-74 had an admission rate in the index year 1997-8 that was 20 times greater than the rate in the general population of the same age. The ratio fell to 5.2 in 1998-9 and 1.7 in 2002-3. For the oldest members of the high risk cohort (aged ≥ 85 in 1997-8) the ratio of their admission rate to that of the general population of the same age fell from 5.9 in the index year to 1.6 in the following year and to 0.53 in 2002-3.
Table 1.
Emergency admissions and bed days per head for patients aged ≥65, 65-74, 75-84, and ≥85 in 1997-8: comparison of those with two or more emergency admissions in 1997-8 with general population (England)
| 1997-8 | 1998-9 | 1999-2000 | 2000-1 | 2001-2 | 2002-3 | |
|---|---|---|---|---|---|---|
| Admissions per person per year | ||||||
| Patients ≥65 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 (n=227 206) | 2.568 | 0.641 | 0.387 | 0.294 | 0.232 | 0.194 |
| All patients (n=7 724 200) | 0.198 | 0.191 | 0.187 | 0.181 | 0.177 | 0.177 |
| Patients 65-74 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 (n=83 820) | 2.626 | 0.697 | 0.443 | 0.356 | 0.301 | 0.260 |
| All patients (n=4 166 000) | 0.129 | 0.134 | 0.139 | 0.142 | 0.146 | 0.153 |
| Patients 75-84 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 (n=94 730) | 2.563 | 0.640 | 0.384 | 0.292 | 0.223 | 0.186 |
| All patients (n=2 670 600) | 0.230 | 0.232 | 0.228 | 0.221 | 0.216 | 0.215 |
| Patients ≥85 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 (n=48 656) | 2.477 | 0.550 | 0.294 | 0.195 | 0.130 | 0.094 |
| All patients (n=887 600) | 0.421 | 0.339 | 0.287 | 0.247 | 0.204 | 0.176 |
| Bed days per person per year | ||||||
| Patients ≥65 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 | 29.6 | 9.0 | 5.0 | 3.9 | 3.2 | 2.6 |
| All patients | 2.5 | 2.5 | 2.5 | 2.6 | 2.6 | 2.6 |
| Patients 65-74 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 | 25.6 | 8.2 | 4.9 | 4.0 | 3.6 | 3.0 |
| All patients | 1.3 | 1.5 | 1.5 | 1.7 | 1.8 | 1.9 |
| Patients 75-84 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 | 30.6 | 9.4 | 5.2 | 4.1 | 3.3 | 2.8 |
| All patients | 3.1 | 3.3 | 3.3 | 3.4 | 3.5 | 3.5 |
| Patients ≥85 in 1997-8: | ||||||
| With ≥2 emergency admissions in 1997-8 | 34.5 | 9.6 | 4.6 | 3.3 | 2.3 | 1.6 |
| All patients | 6.4 | 5.6 | 4.8 | 4.3 | 3.7 | 3.2 |
Figure 1.
Emergency admissions and emergency bed days per person for patients ≥65 in 1997-8: comparison of those with two or more emergency admissions in 1997-8 (“high risk”) with general population (England)
The 1997-8 high risk cohort was 2.9% of the total English population aged ≥ 65 in mid-1997. The share of emergency admissions of those aged ≥ 65 in 1997-8 accounted for by the 1997-8 high risk cohort fell from 38.2% in 1997-8 to 9.9% in the following year and to 3.2% by 2002-3.
Of the 223 993 patients aged ≥ 66 who had two or more emergency admissions in 1998-9, 30 020 had had two or more emergency admissions in the previous year (1997-8). Thus the sensitivity of the criteria of being ≥ 65 and having at least two admissions in 1997-8 in detecting patients age ≥ 66 who would have two or more admissions in the following year (1998-9) was 13.4%.
Discussion
The analyses reported here form part of a wider evaluation of case management initiatives in the United Kingdom.13 They show the caution that is needed when attributing reductions in admission rates in high risk groups to a particular intervention. A history of two or more emergency admissions in a year is indeed a risk factor for future admission in elderly patients: in the first year after the index year such patients aged ≥ 65 still have admission rates that are 3.4 times higher than those in the general population of the same age. But these rates are still much lower than in the index year. In the year after two emergency admissions, the overall emergency admission rate was reduced by 75% in patients ≥ 65, without any intervention. Moreover, using the criteria of being ≥ 65 and having two or more admissions in the index year has low sensitivity in detecting older patients who will have high admissions in the following year.
The progressive reduction in admissions and bed days in the “high risk” cohort is probably due both to mortality in the cohort and to regression toward the mean in surviving patients. These factors vary by age. The admission rate for “high risk” patients aged 65-74 remains above that in the general population of the same age, whereas the admission rates for the cohorts aged 75-84 and ≥ 85 eventually fall below those for the general population. This suggests that a larger proportion of the 65-74 “high risk” group remain at increased risk of future admission. Further research to refine the definition of “high risk” groups for interventions to reduce admissions may therefore be warranted.
There has been considerable debate about the merits of changes in admission rates as a measure of quality of care.15,16 Within the United States, “ambulatory sensitive admissions” seem to be influenced by quality of care. However, this may be because quality of care is influenced by whether people have access to primary care when they are unwell.17,18 This is less of an issue in the United Kingdom, with its universal health coverage. Furthermore, within the United Kingdom, ambulatory admission rates may be substantially affected by factors such as sociodemographic population characteristics19 and casemix.20 Nevertheless, there is evidence within the United Kingdom that improved primary care could result in fewer admissions for some conditions,21 and it is therefore reasonable to expect to see a reduction in admissions after a targeted intervention if high risk groups are followed on a longitudinal basis. The question that we have examined is the baseline against which any apparent reduction should be judged.
Our findings might be regarded as counterintuitive, as many would expect the admission rates of frail older people to rise progressively as more complications ensue. If this assumption were made, interventions such as the recently announced policy of case management for frail elderly people12 might be monitored simply by following trends in admission rates for a target group. Our data show that this approach could be seriously misleading and could result in the misattribution of falling admission rates to an intervention because the admissions would probably decline anyway. To attribute reduced admission rates to a healthcare intervention it is essential to compare the intervention group with a carefully selected control population. If a randomised trial design is not feasible then, at the very least, admissions after the intervention should be compared with a control group who satisfy the “high risk” criteria used to select the intervention group.
We did not look at the wider potential impact of schemes for avoidance of admission on quality of life for older people. These could have an impact on a range of outcomes, including better health or more effective terminal care at home, either of which could result in a reduction in admissions compared with a control population. We recommend that when avoidance schemes are introduced, wider benefits than those that narrowly affect admission rates should be considered, and that changes in admission rates themselves should be treated with great caution unless there are adequate control data for comparison.
What is already known on this topic
People aged ≥ 65 with two of more emergency admissions are responsible for 38% of emergency hospital admissions in their age group
To reduce future hospital admissions, these patients have been targeted by interventions such as Evercare
The 2005 NHS policy on long term conditions also identifies these people as a group for intervention by “community matrons”
What this paper adds
Admissions in people age ≥ 65 with two of more emergency admissions fall in subsequent years without any intervention and account for fewer than 10% of admissions in the following year
The effectiveness of admission avoidance schemes cannot be judged by tracking admission rates without careful comparison with a control group
Editorial by Morrison and also p 293
Contributors: All authors contributed to the design of the study and to the authorship of the paper. HG and MD conducted the analyses. MR and HG are guarantors.
Funding: The National Primary Care Research and Development Centre receives funding from the Department of Health.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1.Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. Int J Geriatr Psychiatry 2003;18: 222-35. [DOI] [PubMed] [Google Scholar]
- 2.Hutt R, Rosen R, McCauley J. Case managing long term conditions. London: King's Fund, 2004.
- 3.Pacala JT, Boult C, Boult L. Predictive validity of a questionnaire that identifies older persons at risk of hospital admission. J Am Geriatr Soc 1995;43: 374-7. [DOI] [PubMed] [Google Scholar]
- 4.Brody KK, Johnson RE, Ried LD, Carder PC, Perrin N. A comparison of two methods for identifying frail Medicare aged persons. J Am Geriatr Soc 2002;50: 562-9. [DOI] [PubMed] [Google Scholar]
- 5.Meldon SW, Mion LC, Palmer RM, Drew BL, Connor JT, Lewiwicki LJ, et al. A brief risk stratification tool to predict repeat emergency department visits and hospitalisations in older patients discharged from the emergency room. Acad Emerg Med 2003;10: 224-32. [DOI] [PubMed] [Google Scholar]
- 6.Implementing the Evercare Programme. Interim report. February 2004. www.natpact.nhs.uk/cms/186.php (accessed 14 Jan 2005).
- 7.www.evercareonline.com/products/products.html (accessed 14 Jan 2005).
- 8.Kane R, Keckhafer G, Flood S, Bershadsky B, Siadaty M. The effect of Evercare on hospital use. J Am Geriatr Soc 2003;51: 1427-34. [DOI] [PubMed] [Google Scholar]
- 9.Brook GM, Reuben D, Zendle LJ, Ershoff DH, Wolde-Tsadik G, Rubenstein LZ, et al. Rationale and design of a multi-centre randomized trial of comprehensive geriatric assessment consultation for hosptializes patients in an HMO. J Am Geriatr Soc 1994;42: 536-44. [DOI] [PubMed] [Google Scholar]
- 10.Stewart S, Pearson S, Horowitz JD. Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care. Arch Intern Med 1998;158: 1067-72. [DOI] [PubMed] [Google Scholar]
- 11.Rich MW, Vinson JM, Sperry JC, Shah AS, Spinner LR, Chung MK, et al. Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study. J Gen Intern Med 1993;8: 585-90. [DOI] [PubMed] [Google Scholar]
- 12.Department of Health. Supporting people with long term conditions. London: Department of Health, 2005. www.dh.gov.uk/PublicationsAndStatistics/Pub lications/PublicationsPolicyAndGuidance/Publications PolicyAndGuidanceArticle/fs/en (accessed 14 Jan 2005).
- 13.Boaden R, Dusheiko M, Gravelle H, Parker S, Pickard S, Roland M, et al. Evercare evaluation interim report: implications for supporting people with long term conditions. Manchester: National Primary Care Research and Development Centre, University of Manchester. www.npcrdc.man.ac.uk/ResearchDetail.cfm?ID=131&status=In%20Progress&theme=3
- 14.Office for National Statistics. Mid-1997 population estimates: England; single year of age and sex; estimated resident population, revised (03/06/04) in light of the results of the 2001 Census. London: Office for National Statistics. www.statistics.gov.uk/ (accessed 14 Jan 2005).
- 15.Ashton C, Wray NP. A conceptual framework for the study of early readmission as an indicator of quality of care. Soc Sci Med 1996;43: 1533-41. [DOI] [PubMed] [Google Scholar]
- 16.Clarke A. Readmission to hospital: a measure of quality or outcome? Qual Saf Health Care 2004;13: 10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basu J, Friedman B, Burstin H. Primary care, HMO enrolment, and hospitalization for ambulatory sensitive conditions. Med Care 2002;40: 1260-9. [DOI] [PubMed] [Google Scholar]
- 18.Ricketts TC, Randolph R, Howard HA, Pathman D, Carey T. Hospitalisation rates as indicators of access to primary care. Health Place 2001;7: 27-38. [DOI] [PubMed] [Google Scholar]
- 19.Giuffrida A, Gravelle H, Roland M. Measuring quality with routine data: avoiding confusion between performance indicators and health outcomes. BMJ 1999;319: 94-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leng GC, Walsh D, Fowkes FGR, Swainson CP. Is the emergency readmission rate a valid outcome indicator? Qual Health Care 1999;8: 234-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sanderson C, Dixon J. Conditions for which onset or hospital admission is potentially preventable by timely and effective ambulatory care. J Health Serv Res Policy 2000;5: 222-30. [DOI] [PubMed] [Google Scholar]