Vasectomy is one of the safest and most effective permanent contraceptive methods available. Compared with tubal ligation, which is usually done under general anaesthesia and entails surgery within a woman's peritoneal cavity, vasectomy is safer and men recover more quickly from the procedure. Vasectomies are usually done under local anaesthesia in outpatient settings, and men usually go home within an hour of the surgery. None the less, for various reasons, vasectomy procedures are less common than tubal ligation procedures in most countries.
Surgical techniques used for vasectomy vary widely throughout the world. The two main components of vasectomy are isolation of the vas deferens from the scrotum and subsequent vas occlusion. However, more than 30 different combinations of vas occlusion techniques probably exist,1 and poor quality studies, heterogeneous study designs, and conflicting results have made it difficult to determine which are the most effective.2
The most common technique, especially in low resource settings, is suture ligation with excision of a small segment of the vas.3 Few data are available on exact rates of use, but recent observations and interviews with surgeons in Asia suggest that at least 95% of all vasectomies in India, Nepal, and Bangladesh are done using ligation and excision (Michel Labrecque, Laval University, written communication, 28 May 2004). In contrast, data from 1995 indicate that only about 18% of vasectomies in the United States are done using this technique.4 Although vasectomy has traditionally been thought to have overall failure rates of 1-3% or lower,5-7 recent research indicates higher failure rates for ligation and excision.8-10
Because of a concern that vasectomy failure rates with ligation and excision could be higher than generally acknowledged, Family Health International and EngenderHealth convened a meeting of vasectomy experts in April 2001 in Durham, North Carolina. Family Health International and EngenderHealth are non-profit, non-governmental organisations devoted to improving global reproductive health. As a result of the experts' recommendations in 2001, additional research was conducted, and new data are now available. To review the latest findings, a second meeting of vasectomy experts was convened in December 2003 in Washington, DC. We describe here the outcomes of discussions from that meeting.
Summary points
In fascial interposition, the sheath covering the vas is pulled over one severed end and the sheath is closed to create a natural tissue barrier
Ligation and excision of a small segment of the vas plus fascial interposition is more effective at occluding the vas than is ligation and excision alone
Thermal cautery or electrocautery of the vas lumen is also more effective than ligation and excision alone; inexpensive, battery powered thermal cautery devices are commercially available
Recent evidence suggests that cautery plus fascial interposition is more effective than ligation and excision plus fascial interposition, but fascial interposition is technically challenging; research is needed to determine where cautery alone fits into this hierarchy
Methods
Family Health International, EngenderHealth, and EngenderHealth's ACQUIRE Project organised an expert consultation on vasectomy to review the literature and share new research findings on vas occlusion techniques, discuss programmatic implications, prioritise future research, and develop guidelines for using vasectomy techniques in diverse healthcare settings. More than 50 representatives from 24 universities and reproductive health research, service delivery, training, advocacy, and donor organisations attended the consultation. We focus here on the new clinical findings and evidence based “points of consensus” on the effectiveness of techniques agreed on at the meeting. These points of consensus were based on recent research results, described below; input from independent experts; and results of a formal, systematic literature review that was presented at the meeting and has since been published.2
Recent research results
Because pregnancy after vasectomy is relatively rare and difficult to study, the findings given below are based on results of semen analysis rather than pregnancy outcomes.
Fascial interposition
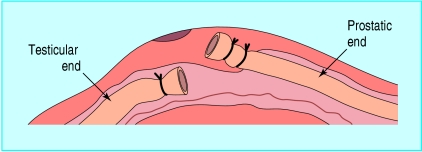
Fascial interposition is a technique in which the sheath covering the vas is pulled over one severed end and the sheath is closed to create a natural tissue barrier. Figure 1 shows the testicular end of the vas within the sheath and the prostatic end outside, but many practitioners prefer the reverse—that is, keeping the prostatic end inside the sheath and the testicular end outside.
Fig 1.
Fascial interposition. Adapted from EngenderHealth20
Recent results from a large randomised controlled trial conducted in eight outpatient clinics in Brazil, El Salvador, Mexico, Nepal, Panama, Sri Lanka, and the United States (see figures A and B on bmj.com) showed that ligation and excision plus fascial interposition is significantly more effective than ligation and excision alone.11 An interim analysis of 552 men suggested that fascial interposition significantly reduced vasectomy failure rates, leading to early termination of the study.12 Final results, which included data from 841 men receiving vasectomies between December 1999 and June 2002, confirmed these findings. The study included frequent semen analyses, at two weeks after vasectomy and every four weeks until either vasectomy success (defined as the complete absence of sperm—azoospermia—in two consecutive semen samples) or vasectomy failure (defined as more than five million motile sperm/ml at 14 weeks or later, or more than 100 000 sperm/ml with any motility at 26 weeks or later). Fascial interposition reduced failure rates by approximately 50%, from 12.7% to 5.9%.
This trial supported the results of several smaller studies suggesting the superiority of fascial interposition and helped to resolve conflicting results from previous studies.2 Although ligation and excision alone is considered safe and effective, the experts agreed that these findings had important implications for improving vasectomy services. Efforts are now under way to train vasectomy providers on fascial interposition, especially in low resource settings.13
Cautery
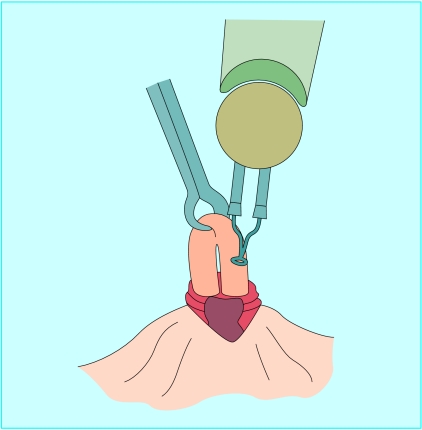
Another technique to improve the effectiveness of vasectomy is cautery, in which heat or an electric current is used to cauterise the lumen of the vas (fig 2). Cautery is the most common vas occlusion technique in the United States; it was used in 71% of vasectomies done in 1995,4 up from 50% in 1991.14 Data reviewed from several large case series and comparative studies suggest that failure rates are lower with cautery than with simple ligation and excision, with consistent failure rates of less than 1% when cautery is used in combination with fascial interposition.2 Although most surgeons cauterise both ends of the vas, some prefer to cauterise only the prostatic end. This is called an open ended vasectomy, and some researchers have suggested that leaving the testicular end open reduces side effects from the procedure.
Fig 2.
Thermal cautery. Adapted from EngenderHealth20
Recent results from a six month prospective non-comparative study of 400 men having vasectomies in Brazil, Canada, the United Kingdom, and the United States seem to confirm the low failure rate when cautery is used.15 In this multicentre study, the rate of failure (defined as more than 10 million sperm/ml at 12 weeks or later, without subsequent success) among 364 participants who completed follow up was 0.8%. This study also included frequent semen analyses, beginning at two weeks and continuing through 24 weeks.
The experts concluded that the results of this study should be interpreted with caution, because it was not a randomised trial and because different methods of cautery were used at each of the four centres. Providers at two centres used thermal cautery, and those at the remaining two used electrocautery. Other technical variations also occurred between sites, in particular the use of fascial interposition at only two of the sites. However, the experts did agree that, on the basis of these results and those of other published studies, cautery is more effective than ligation and excision alone, but not enough data exist to determine whether thermal cautery or electrocautery is more effective. Some surgeons prefer thermal cautery over electrocautery, because it may produce fewer granulomas and less nodular thickening of the vas.16 Furthermore, thermal cautery can be done using potentially reusable, cheap, battery powered, handheld devices practical for use in remote locations or where electricity is unreliable.17 See bmj.com for photographs of such a device.
Fascial interposition versus cautery
To compare cautery with fascial interposition, experts compared failure rates from the multicentre randomised controlled trial with those from the observational cautery study described above. Overall, cautery was associated with significantly fewer early vasectomy failures than was ligation and excision plus fascial interposition, when failure was defined as more than 10 million sperm/ml at 12 weeks or later (1% v 5%).18 The experts concluded that it was reasonable for vasectomy providers to consider switching from ligation and excision to cautery if it was feasible and sustainable in their settings.
Points of consensus
Overall, the recent research suggests a hierarchy of increasing contraceptive effectiveness with the following techniques: ligation and excision alone, ligation and excision with fascial interposition, and cautery with fascial interposition. The position of cautery alone in this hierarchy is unclear. On this basis, the experts at the meeting developed points of consensus in the form of a brief document for vasectomy providers and programme managers, to inform them of the latest research and to provide practical recommendations for the use of various techniques (box).
These points of consensus are meant to provide guidance to vasectomy providers and programme managers but should not be considered a mandate for change, for several reasons. Firstly, data are still limited on the effectiveness of cautery alone compared with ligation and excision plus fascial interposition. Secondly, some vasectomy providers might be encouraged to abandon ligation and excision prematurely because of the notion that cautery is a superior technique. However, vasectomy with ligation and excision alone is still very effective compared with most other contraceptive options, and cautery may be difficult to implement and sustain in some settings. Thirdly, training is advisable before adopting any new surgical technique, as the details of a particular cautery technique are important in determining efficacy.
Future research priorities
The expert consultation identified several future research priorities. Of highest priority was a three armed randomised controlled trial to compare ligation and excision with fascial interposition versus cautery alone versus cautery with fascial interposition. The exact surgical techniques used in such a study need to be carefully defined and standardised, and postvasectomy pain should be monitored. A small percentage of patients (less than 10%) have chronic testicular pain after vasectomy, but this has been poorly defined and can cause diagnostic and therapeutic challenges for physicians.19 For these reasons, systematic assessment of such pain should be incorporated into future vasectomy studies. A related question that deserves further research is whether an open ended vasectomy technique would result in less postvasectomy pain than would a vasectomy technique in which both ends of the vas are cauterised, as some researchers have suggested.2 The participants at the meeting also agreed on the importance of determining the optimal methods of cautery for low resource settings, including further research on developing simple, acceptable, and low cost approaches for sterilisation and reuse of cautery tips.
Additional educational resources
Royal College of Obstetricians and Gynaecologists. National evidence-based clinical guidelines: male and female sterilisation. London: Royal College of Obstetricians and Gynaecologists, 2004. www.rcog.org.uk/guidelines.asp?PageID=108&GuidelineID=30
EngenderHealth. Contraceptive sterilization: global issues and trends. New York: EngenderHealth, 2002. www.engenderhealth.org/res/offc/steril/factbook/index.html
Sokal DC. Recent research on vasectomy techniques. Asian J Androl 2003;5: 227-30. www.asiaandro.com/1008-682X/5/227.htm
Cook LA, Van Vliet H, Pun A, Gallo MF. Vasectomy occlusion techniques for male sterilization. Cochrane Database Syst Rev 2004;(3):CD003991
Information for patients
Sterilisation for women and men: what you need to know (www.rcog.org.uk/mainpages.asp?PageID=1420)—Patient information document produced by the Royal College of Obstetric8ians and Gynaecologists
Vasectomy: questions and answers (www.engenderhealth.com/wh/fp/cvas2.html)—Vasectomy facts from the US based non-governmental organisation EngenderHealth, including links for accessing additional information
Vasectomy information (www.vasectomy-information.com/indexie.asp)—Personal experiences of men who have had vasectomies; frequently asked questions about the procedure; vasectomy news from around the world
Points of consensus on the effectiveness of different vas occlusion techniques
Vasectomy can be thought of as both an approach to the vas and a vas occlusion technique. With respect to approach, strong, high quality evidence shows that the no-scalpel vasectomy technique has significantly fewer side effects and complications than does the standard incisional approach. The no-scalpel vasectomy approach to the vas is therefore recommended. The remainder of this consensus document considers different techniques of vas occlusion, for which high quality data are limited. However, some recent evidence indicates that certain occlusion techniques can further increase the effectiveness of vasectomy.
Research findings
Because postvasectomy pregnancies are rare and difficult to study, the vasectomy research findings described below are based mainly on data from semen analysis.
Fascial interposition—Several observational studies and a recent randomised controlled trial indicate that fascial interposition, when used with ligation and excision, reduces the likelihood of vasectomy failure.
Cautery—Available data suggest that cautery is more effective than ligation and excision for vas occlusion. Furthermore, some data suggest that cautery is more effective than ligation and excision with fascial interposition. Data are insufficient to determine if either of the cautery techniques—thermal cautery or electrocautery—is more effective than the other. A preliminary evaluation of a battery powered, handheld cautery device indicates that the thermal cautery tips can be effectively resterilised and safely reused; they can be inexpensively manufactured.
Recommendations
Training of vasectomy providers should emphasise the potential increased effectiveness of adding fascial interposition to the standard technique of ligation and excision. Providers now using simple ligation and excision should consider adopting fascial interposition, with appropriate training as needed
Where resources, training, and logistical support are available, cautery is recommended as an effective and safe vas occlusion technique
Further research is needed on simple ways to learn how to do fascial interposition and on the feasibility of using cost effective cautery devices in low resource settings
The experts also discussed programmatic research, including prospective evaluations of different techniques, studies to determine the feasibility of implementing and training providers on various techniques, and research to identify practical differences between the techniques and perhaps to make recommendations for providers depending on the number of vasectomies done in a particular clinical setting. Future research should clarify the appropriate use of cautery and fascial interposition in low resource settings.
Supplementary Material
 Photographs of family planning clinics and a handheld cautery device are on bmj.com
Photographs of family planning clinics and a handheld cautery device are on bmj.com
We thank John M Pile of EngenderHealth, Tim Black of Marie Stopes International, and Michel Labrecque of Laval University for careful review of this document. We also thank the clinicians who participated in the vasectomy studies we cited and the participants in both expert consultations on vasectomy, whose leadership and vision were invaluable in developing the points of consensus shared here.
Contributors: KWA and KB wrote the text. DCS developed the concept of the article, provided editorial input, and is the guarantor.
Funding: Partial support for this work was provided by EngenderHealth with funds from the US Agency for International Development (USAID) Cooperative Agreements No HRN-A-00-98-00042-00 and No GPO-A-00-03-00006-00, and by Family Health International with funds from USAID Cooperative Agreement No CCP-A-00-95-00022-02. The views expressed in the article are those of the authors and do not necessarily reflect those of EngenderHealth, Family Health International, or USAID.
Competing interests: None declared.
References
- 1.Labrecque M. Review of other evidence (abstract). In: Expert consultation on vasectomy: an interagency workshop organized by Family Health International, EngenderHealth and the ACQUIRE Project, Washington DC, Dec 3-5, 2003. Durham, NC: Family Health International, 2004. www.fhi.org/en/RH/Pubs/booksReports/vasconrpt.htm (accessed 10 Dec 2004).
- 2.Labrecque M, Dufresne C, Barone MA, St-Hilaire K. Vasectomy surgical techniques: a systematic review. BMC Med 2004;2: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pollack A. Prevalence of occlusion techniques, vasectomy follow-up protocols and compliance with follow-up (abstract). In: Sokal DC, ed. Proceedings of an expert consultation on vasectomy effectiveness co-sponsored by Family Health International and EngenderHealth, Apr 18-19, 2001, Durham, NC. Durham, NC: Family Health International, 2001. www.fhi.org/en/RH/Pubs/booksReports/vasec_effective.htm (accessed 10 Dec 2004).
- 4.Haws JM, Morgan GT, Pollack AE, Koonin LM, Magnani RJ, Gargiullo PM. Clinical aspects of vasectomies performed in the United States in 1995. Urology 1998;52: 685-91. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt SS. Vasectomy. Urol Clin North Am 1987;14: 149-54. [PubMed] [Google Scholar]
- 6.Liskin L, Pile JM, Quillin WF. Vasectomy—safe and simple. Popul Rep D 1983;4: 61-100. [PubMed] [Google Scholar]
- 7.Trussell J, Kowal D. The essentials of contraception: efficacy, safety, and personal considerations. In: Hatcher RA, Trussel J, Stewart F, Cates W Jr, Stewart GK, Guest F, et al, eds. Contraceptive Technology. 17th ed. New York: Ardent Media, 1998: 211-47.
- 8.Barone M, Nazerali H, Cortes M, Chen-Mok M, Pollack A, Sokal D. A prospective study of time and number of ejaculations to azoospermia after vasectomy by ligation and excision. J Urol 2003;170: 892-6. [DOI] [PubMed] [Google Scholar]
- 9.Nazerali H, Thapa S, Hays M, Pathak LR, Pandey KR, Sokal DC. Vasectomy effectiveness in Nepal: a retrospective study. Contraception 2003;67: 397-401. [DOI] [PubMed] [Google Scholar]
- 10.Wang D. Contraceptive failure in China. Contraception 2002;66: 173-8. [DOI] [PubMed] [Google Scholar]
- 11.Sokal D, Irsula B, Hays M, Chen-Mok M, Barone MA, Investigator Study Group. Vasectomy by ligation and excision, with or without fascial interposition: a randomized controlled trial. BMC Med 2004;2: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen-Mok M, Bangdiwala SI, Dominik R, Hays M, Irsula B, Sokal DC. Termination of a randomized controlled trial of two vasectomy techniques. Control Clin Trials 2003;24: 78-84. [DOI] [PubMed] [Google Scholar]
- 13.EngenderHealth. No-scalpel vasectomy: an illustrated guide for surgeons. 3rd ed. New York: EngenderHealth, 2003.
- 14.Marquette CM, Koonin LM, Antarsh L, Gargiullo PM, Smith JC. Vasectomy in the United States, 1991. Am J Public Health 1995;85: 644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barone MA, Irsula B, Chen-Mok M, Sokal DC, Investigator Study Group. Effectiveness of vasectomy using cautery. BMC Urol 2004;4: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schmidt SS, Minckler TM. The vas after vasectomy: comparison of cauterization methods. Urology 1992;40: 468-70. [DOI] [PubMed] [Google Scholar]
- 17.Seamans Y. Recent research results (abstract). In: Expert consultation on vasectomy: an interagency workshop organized by Family Health International, EngenderHealth and the ACQUIRE Project, Washington DC, Dec 3-5, 2003. Durham, NC: Family Health International, 2004. www.fhi.org/en/RH/Pubs/booksReports/vasconrpt.htm (accessed 10 Dec 2004).
- 18.Sokal D, Irsula B, Chen-Mok M, Labrecque M, Barone MA. A comparison of vas occlusion techniques: cautery more effective than ligation and excision with fascial interposition. BMC Urol 2004;4: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Christiansen CG, Sandlow JI. Testicular pain following vasectomy: a review of postvasectomy pain syndrome. J Androl 2003;24: 293-8. [DOI] [PubMed] [Google Scholar]
- 20.EngenderHealth. No-scalpel vasectomy: an illustrated guide for surgeons. 3rd ed. New York: EngenderHealth, 2003.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.