Abstract
Background
Oesophageal cancer is one of the most common malignancies worldwide,and oesophageal squamous cell carcinoma (ESCC) is the predominant histological type both globally and in China. Collagen triple helix repeat containing 1 (CTHRC1) has been found to be upregulated in ESCC. However, its role in tumourigenesis and progression of ESCC remains unclear.
Methods
Using our previous ESCC mRNA profiling data, we screened upregulated genes to identify those required for proliferation. Immunohistochemistry was performed to determine the level of CTHRC1 protein expression in 204 ESCC patients. Correlations between CTHRC1 expression and clinicopathological characteristics were assessed. In addition, pyrosequencing and 5-aza-dC treatment were performed to evaluate methylation status of CTHRC1 promoter. In vitro and in vivo analyses were also conducted to determine the role of CTHRC1 in ESCC cell proliferation, migration and invasion, and RNA sequencing and molecular experiments were performed to study the underlying mechanisms.
Results
Based on mRNA profiling data, CTHRC1 was identified as one of the most significantly upregulated genes in ESCC tissues (n = 119, fold change = 20.5, P = 2.12E-66). RNA interference screening also showed that CTHRC1 was required for cell proliferation. Immunohistochemistry confirmed markedly high CTHRC1 protein expression in tumour tissues, and high CTHRC1 expression was positively correlated with advanced T stage (P = 0.043), lymph node metastasis (P = 0.023), TNM stage (P = 0.024) and poor overall survival (P = 0.020). Promoter hypomethylation at cg07757887 may contribute to increased CTHRC1 expression in ESCC cells and tumours. Forced overexpression of CTHRC1 significantly enhanced cell proliferation, migration and invasion, whereas depletion of CTHRC1 suppressed these cellular functions in three ESCC cell lines and xenografts. CTHRC1 was found to activate FRA-1 (Fos-related antigen 1, also known as FOSL1) through the MAPK/MEK/ERK cascade, which led to upregulation of cyclin D1 and thus promoted cell proliferation. FRA-1 also induced snail1-mediated MMP14 (matrix metallopeptidase 14, also known as MT1-MMP) expression to facilitate ESCC cell invasion, migration, and metastasis.
Conclusions
Our data suggest that CTHRC1 may act as an oncogenic driver in progression and metastasis of ESCC, and may serve as a potential biomarker for prognosis and personalized therapy.
Electronic supplementary material
The online version of this article (doi:10.1186/s13046-017-0555-8) contains supplementary material, which is available to authorized users.
Keywords: Oesophageal squamous cell carcinoma (ESCC), Collagen triple helix repeat containing 1 (CTHRC1), Prognosis, Progression, ERK pathway, FRA-1, MMP14
Background
With an estimated 455,800 new cases and 400,200 deaths each year, oesophageal cancer is the sixth leading cause of cancer death and the eighth most common cancer worldwide [1]. Oesophageal squamous cell carcinoma (ESCC) is the predominant histological type both in China and around the world. Despite advancements in population screening and standardized multidisciplinary treatment over the last four decades [2], our previous report showed that ESCC remains the fourth leading cause of cancer-related death in China [3], with a dismal 5-year survival rate of only 20.9% [4]. The poor outcome of patients is primarily attributed to the high rate of ESCC metastasis, including both regional lymph node and further distant metastases [5]. Therefore, it’s vital to identify the underlying molecular mechanisms that drive progression, especially metastasis, of ESCC for predicting patients’ prognosis and improving rational design of personalized medicine.
Collagen triple helix repeat containing 1 (CTHRC1) is a secreted glycoprotein that can reduce collagen matrix deposition and promote the mobility of fibroblasts and smooth muscle cells [6–8]. Indeed, overexpression of CTHRC1, which has been reported in various malignancies, is suggested to serve as an independent prognostic factor [9–12]. Recently, a germline mutation in CTHRC1 gene was identified to be associated with Barrett’s oesophagus and oesophageal adenocarcinoma [13], and high CTHRC1 expression in ESCC was revealed by expression profiling studies involving a small number of cases [14, 15]. However, these findings should be confirmed in studies including larger groups and the cellular function and clinical implications of CTHRC1 in ESCC need to be resolved.
In this study, we sought to confirm in a much larger cohort aberrant elevated expression of CTHRC1 and to investigate its association with clinicopathological characteristics in ESCC. To assess the effect of CTHRC1 on malignant phenotypes of ESCC cells in vitro and in vivo, we then established multiple cell lines with stable depletion or overexpression of CTHRC1. Furthermore, we defined the underlying signalling pathways and transcription factors that depend on CTHRC1 activation and are responsible for ESCC progression.
Methods
Patients and tissue specimens
The study design and use of clinical samples were approved by the Ethics Committee of Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College. A total of 204 formalin-fixed and paraffin-embedded (FFPE) ESCC tissue samples were obtained with informed consent and agreement from the biobank of Cancer Hospital of Chinese Academy of Medical Sciences. From 2000 to 2008, specimens were surgically resected from patients with stage I-III ESCC and who did not receive preoperative treatment. The clinicopathological characteristics of these patients are summarized in Table 1. Five tissue microarrays (TMAs) were constructed by incorporating one representative core of each tissue. The microarrays contained 204 primary ESCC tumour tissues, 169 of which were accompanied by adjacent non-tumour epithelial tissues.
Table 1.
Correlations between CTHRC1 levels in ESCC tissues and clinicopathological characteristics of patients with ESCC
| Characteristic | CTHRC1 expression | P | ||
|---|---|---|---|---|
| Low | High | |||
| Age | ≤60 | 49 | 67 | 0.128 |
| >60 | 28 | 60 | ||
| Gender | Male | 62 | 106 | 0.593 |
| Female | 15 | 21 | ||
| Tobacco use | No | 27 | 45 | 0.957 |
| Yes | 50 | 82 | ||
| Alcohol use | No | 30 | 46 | 0.695 |
| Yes | 47 | 81 | ||
| Family history | No | 65 | 106 | 0.858 |
| Yes | 12 | 21 | ||
| Location | Upper/Middle | 39 | 60 | 0.637 |
| Lower | 38 | 67 | ||
| Histology grade | G1/G2 | 59 | 94 | 0.677 |
| G3 | 18 | 33 | ||
| T stage | T1/T2/T3 | 44 | 54 | 0.043 |
| T4 | 33 | 73 | ||
| Lymph node metastasis | No | 49 | 60 | 0.023 |
| Yes | 28 | 67 | ||
| TNM stage | I/II | 39 | 44 | 0.024 |
| III | 38 | 83 | ||
| FRA-1 | Low | 22 | 28 | 0.116 |
| High | 45 | 97 | ||
| Snail1 | Low | 39 | 53 | 0.100 |
| High | 33 | 73 | ||
| MMP14 | Low | 45 | 58 | 0.022 |
| High | 26 | 67 | ||
| Cyclin D1 | Low | 53 | 66 | 0.018 |
| High | 24 | 61 | ||
χ 2test was used. P value was italicized when P < 0.05
CTHRC1 Collagen triple helix repeat containing-1 (CTHRC1); FRA-1 Fos-related antigen 1
Immunohistochemistry and scoring
Immunohistochemistry (IHC) was performed as previously described [16], using anti-CTHRC1 (ab192778, Abcam, USA), anti-FRA-1 (TA500624S, Origene, USA), anti-cyclin D1 (2978, CST, USA), anti-snail1 (TA500316S, Origene, USA) and anti-MMP14 (ab51047, Abcam, USA) antibodies. Slides were evaluated independently by two pathologists (S.S. & X.F.). The staining intensity was graded as 0 (negative), 1 (low), 2 (moderate) or 3 (high), and the proportion of staining was evaluated as 0 (negative), 1 (<10%), 2 (10–50%), 3 (51–80%), or 4 (>80%). The intensity and proportion scores were multiplied to generate the IHC index. The expression level was considered as low (IHC index < 6), and as high (IHC index ≥ 6).
Cell culture
All cell lines used in this study were regularly authenticated by short tandem repeat (STR) profiling. KYSE510, KYSE30, KYSE450, KYSE180 and KYSE70 cells were cultured in RPMI 1640 medium supplemented with 10% foetal bovine serum, 100 UI/ml penicillin and 100 UI/ml streptomycin (Gibco, USA). Het1a, a non-malignant immortalized human oesophageal squamous cell line, was cultured in BEGM (Bronchial Epithelial Cell Growth) medium (Lonza, USA). All cell lines were maintained in a humidified incubator at 37 °C and 5%CO2.
Transfection and stable cell line establishment
Small interfering RNA (SiRNA; Dharmacon, USA) and plasmid transfections were performed using Lipofectamine RNAiMAX Transfection Reagent and Lipofectamine 3000 (Invitrogen, USA), respectively. For silencing of CTHRC1, two short hairpin RNA (shRNA) oligonucleotides (5’-GCTATCTGGGTTGGTACTTGTTTCAAGAGAACAAGTACCAACCCAGATAGCTT-3’ and 5’-GCTTCTACTGGATGGAATTCATTCAAGAGATGAATTCCATCCAGTAGAAGCTT-3’) were cloned into the pLKD-CMV-R&PR-U6-shRNA vector (Heyuan, China). The negative control (NC) sequence was 5’-TGTTCTCCGAACGTGTCACGTTTCAAGAGAACGTGACACGTTCGGAGAACTT-3’. For overexpression, the coding DNA sequence (CDS) of CTHRC1 was cloned into the pLenti-EF1a-EGFP-P2A-Puro-CMV-MCS vector (Heyuan, China); the empty vector was used as the negative control. Lentivirus packaging and purification and cell infection were carried out with ViraPowerTM Lentiviral Expression Systems (Invitrogen, USA) according to the manufacturer’s instructions. Cells were selected using medium containing 1.5 μg/ml puromycin (Sigma-Aldrich, USA). The efficiency of knockdown and overexpression were confirmed by real-time polymerase chain reaction (PCR) and western blot.
RNA interference (RNAi) screening
KYSE30, KYSE510 and KYSE70 cells were plated in 96-well plates and transfected in triplicate with on-target plus smartpool siRNA (Dharmacon, USA). After 72 h, the cells were stained with 4’,6-diamidino-2-phenylindole (DAPI) (Sigma-Aldrich, Germany). Then the samples were imaged using a high content screening system (Operetta) and analysed using Harmony 3.1 software.
Real-time PCR (RT-PCR)
RT-PCR was performed as previously described [17]. The primers used are listed in Additional file 1: Table S1.
Western blot
Whole cell lysates were prepared using RIPA buffer supplemented with protease and phosphatase inhibitor cocktail (Thermo, USA) and culture supernatants were concentrated using Microcon centrifugal filters (Millipore, USA). Western blot was performed as previously described [17]. Primary antibodies against the following proteins were used: CTHRC1 (ab192778, Abcam, USA), p-c-Raf (9427, CST, USA), p-MEK1/2 (9154, CST, USA), p-ERK1/2 (4370, CST, USA), ERK1/2 (4695, CST, USA), p-FRA-1 (5841, CST, USA), FRA-1 (5281, CST, USA), cyclinD1 (2978, CST, USA), snail1 (3879, CST, USA), and MMP14 (13130, CST, USA). α − Tubulin (T9026, Sigma-Aldrich, USA) was used as a loading control.
Cell proliferation and colony formation assays
Cell proliferation and colony formation assays were performed as previously described [18]. Cell proliferation was assessed using Cell Counting Kit-8 (CCK8). Images of the colony formation assay results were scanned and the clone number was determined using GeneSys software (Genecompany, China).
Boyden chamber Transwell assay
For invasion and migration assays, we used 24-well Boyden chambers precoated with or without Matrigel matrix (Corning, USA), respectively. The experiments were performed as previously described [19].
Xenograft model and lung metastasis model
All mice used in this study received humane care, and all animal experiments were performed in accordance with the guidelines approved by the Institutional Animal Care and Use Committee of Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College. BALB/c-nu mice and non-obese diabetic (NOD)-SCID mice (female, 4–5 weeks old) were purchased from Huafukang (Beijing, China). For the xenograft model, shRNA- or vector-transfected KYSE510 cells and CTHRC1- or vector-transfected KYSE450 cells were injected into the right dorsal flanks of BALB/c-nu mice (5 × 106 cells per animal, 8 mice per group). Tumour formation was monitored every 5 days by measuring tumour size with a calliper. The tumour volume was calculated using the formula: V = (L × W2)/2. After 4 weeks, all mice were sacrificed, and the tumours were excised and weighed. For the lung metastasis model, shRNA- or vector-transfected KYSE510 cells and CTHRC1- or vector-transfected KYSE450 cells were injected into NOD-SCID mice through the tail vein (1 × 106 cells per animal, 8 mice per group). Ten weeks later, the mice were sacrificed, and the lungs were excised and fixed with Bouin’s solution followed by embedding in paraffin for haematoxylin and eosin (H&E) staining. The number of lung surface metastatic nodules was evaluated by gross and microscopic examination.
RNA sequencing
RNA sequencing was performed using KYSE510-shCTHRC1 and KYSE510-vector cells. Total RNA extraction, quality analysis, cDNA library preparation and sequencing were performed at Novogene (Beijing, China). Raw RNA sequences were mapped to the GRCh37.hg19 genome based on TopHat and assembled using Cufflinks. Relative transcript levels are expressed as “fragments per kilobase of transcript per million mapped” (FPKM). Differentially expressed genes (DEGs) were identified using Cuffdiff. To verify the RNA sequencing data, we assessed the transcriptional level of twenty genes using RT-PCR (Additional file 2: Table S2).
Pyrosequencing assay
The pyrosequencing assay was conducted by QIAGEN Translational Medicine Co., Ltd. (Suzhou, China). The primers used were as follows: F-5’-AGGATAGAGGGGGTTATAAAAAGA-3’ and R-5’- ACTCTAACACATTACAAAACCTTACA-3’.
Statistical analysis
Statistical analyses were performed using Prism GraphPad version 6.0 (GraphPad Software Inc., San Diego, USA). Correlations between mRNA expression levels were analysed using Pearson’s correlation coefficient. A chi square test was performed to determine the association between clinicopathological variables and CTHRC1 expression. Survival analysis was carried out using a log-rank test. A Cox proportional hazards model was used to identify independent prognostic factors. The significance of differences between groups was analysed using two-tailed Student’s t-test and the results are expressed as the mean ± SD. Differences were considered significant when P < 0.05. *P < 0.05 and **P < 0.01.
Results
CTHRC1 is significantly overexpressed in ESCC cells and required for their proliferation
We previously conducted transcriptome-wide microarray profiling of 119 pairs of tumour and pair-matched non-tumour oesophageal mucosa samples [20]. Among the top 500 upregulated genes in tumor tissues, we selected CTHRC1, neural EGFL like 2 (NELL2), DLG associated protein 5 (DLGAP5), DEP domain containing 1 (DEPDC1), Zic family member 2 (ZIC2) and centrosomal protein 55 (CEP55) for this study (Additional file 3: Figure S1); these genes were also significantly upregulated in an independent gene expression profiling dataset [15]. The highest fold increase was found for CTHRC1 (n = 119, fold change = 20.5, P = 2.12E-66, Wilcoxon test; false discovery rate (FDR) = 2.93E-64, Benjamin Hochberg procedure). RNAi screening targeting these genes in three ESCC cell lines was performed, and CTHRC1 knockdown dramatically inhibited proliferation in all three cell lines (Fig. 1a).
Fig. 1.
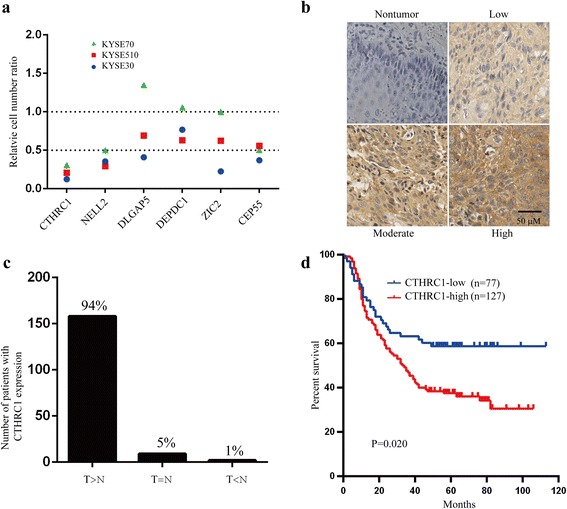
CTHRC1 is commonly upregulated in ESCC tissues and overexpression of CTHRC1 predicts poor prognosis. a Small RNA interference (RNAi) screening targeting Collagen triple helix repeat containing-1 (CTHRC1), Neural EGFL like 2 (NELL2), DLG associated protein 5 (DLGAP5), DEP domain containing 1 (DEPDC1), Zic family member 2 (ZIC2) and Centrosomal protein 55 (CEP55) in KYSE70, KYSE510 and KYSE30 cells. b Representative immunohistochemical (IHC) images of CTHRC1 staining in ESCC tumour tissues and non-tumour tissues. c The number and percent of patients with higher, equal or lower CTHRC1 staining in ESCC tumour tissues compared with non-tumour tissues. T: tumour tissue; N: non-tumour tissue. d Overall survival analysis based on the expression level of CTHRC1 measured by IHC in 204 ESCC patients. Survival rates were determined by the Kaplan-Meier survival analysis. P = 0.020, log-rank test
Endogenous expression levels of CTHRC1 in the ESCC cell lines were higher than in an immortalized oesophageal epithelium cell line (Additional file 4: Figure S2). IHC showed slight cytoplasmic staining of CTHRC1 protein in normal oesophageal epithelial cells, whereas moderate to strong staining in the cytoplasm and extracellular space was observed in most ESCC tumour tissues (Fig. 1b). Compared to matched non-tumor tissues, 94% (158/169) of tumour tissues exhibited stronger staining of CTHRC1 (Fig. 1c). Therefore, we focused on the role and mechanism of CTHRC1 in ESCC progression in this study.
High expression of CTHRC1 in ESCC tumour tissue predicts poor prognosis
As CTHRC1 is almost universally overexpressed in tumour tissue compared to normal oesophageal epithelial tissue, we divided the sample set into two groups based on the CTHRC1 expression level (low or high) in tumour tissues and examined significant differences in clinicopathological characteristics between these two groups (Table 1). Notably, higher expression of CTHRC1 was significantly associated with advanced T stage (P = 0.043, chi square test), lymph node metastasis (P = 0.023, chi square test) and TNM stage (P = 0.024, chi square test). Patients exhibiting a high level of CTHRC1 expression had shorter overall survival than those with low CTHRC1 expression according to both Kaplan-Meier analysis (P = 0.020, log-rank test; Fig. 1d) and univariate Cox regression analysis (Table 2). However, CTHRC1 expression was not independently associated with overall survival by multivariate Cox regression analysis in this cohort after adjustment for age, histology grade, lymph node metastasis and TNM stage (Table 2).
Table 2.
Univariate and multivariate analyses of overall survival among patients with ESCC
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| HR(95% CI) | P | HR(95% CI) | P | |
| Age (≥60 vs <60) |
1.958 (1.354–2.832) | 0.000 | 1.676 (1.149–2.443) | 0.007 |
| Gender (Male vs Female) |
1.178 (0.74–1.876) | 0.490 | ||
| Tobacco use (Yes vs No) |
0.869 (0.594–1.271) | 0.470 | ||
| Alcohol use (Yes vs No) |
0.890 (0.61–1.297) | 0.544 | ||
| Family history (Yes vs No) |
0.646 (0.369–1.130) | 0.125 | ||
| Location (upper/middle vs lower) |
0.782 (0.542–1.130) | 0.191 | ||
| Histology grade (3 vs 1/2) |
2.056 (1.39–3.041) | 0.000 | 1.381 (0.919–2.076) | 0.121 |
| T stage (4 vs 1/2/3) |
3.103 (2.085–4.620) | 0.000 | 1.335 (0.766–2.326) | 0.308 |
| Lymph node metastasis (Yes vs No) |
3.032 (2.055–4.474) | 0.000 | 1.637 (1.043–2.570) | 0.032 |
| TNM stage (III vs I/II) |
4.209 (2.672–6.632) | 0.000 | 2.239 (1.119–4.482) | 0.023 |
| CTHRC1 (high vs low) |
1.605 (1.074–2.399) | 0.021 | 1.157 (0.768–1.743) | 0.486 |
P value was italicized when P < 0.05
Promoter hypomethylation may participate in upregulation of CTHRC1
Previous genomic studies of ESCC didn’t show significant evidence of CTHRC1 gene amplification [21]. We assessed whether promoter hypomethylation contributes to the elevated expression of CTHRC1 in ESCC. Methylation array profiling of paired ESCC tissues revealed significantly lower methylation of cg07757887 (−1220 bp in the CTHRC1 genomic region) in ESCC tumour tissues compared with non-tumour tissues (n = 67, ∆ß =−0.19; FDR = 1.34E-23, unpublished data). Pyrosequencing was performed for further validation, and as expected, cg07757887 methylation was significantly lower in ESCC tumour tissues compared with corresponding non-tumour tissues (n = 50, P < 0.0001, t-test, Fig. 2a), with 92% (46/50) of tumour tissues showing CTHRC1 hypomethylation (Fig. 2b). With the exception of KYSE510 cells, treatment with the DNA methyltransferase inhibitor 5-aza-dC resulted in dramatically increased CTHRC1 mRNA expression and protein production in five ESCC cell lines (Fig. 2c, d). Moreover, pyrosequencing confirmed distinctly increased methylation of cg07757887 in these cell lines except for KYSE510 cells (Fig. 2e), supporting the notion that CTHRC1 expression may be closely associated with promoter methylation in ESCC.
Fig. 2.
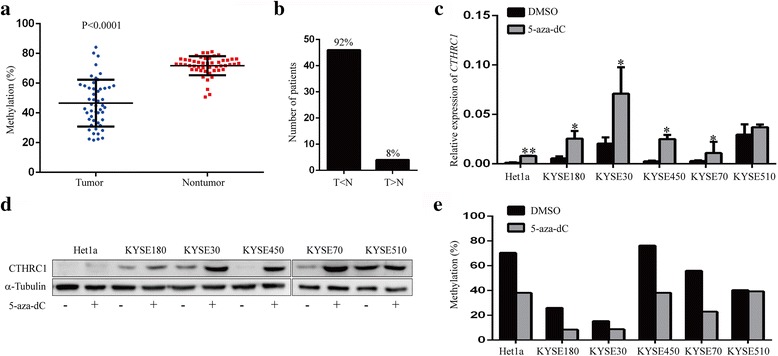
Promoter methylation is involved in regulating CTHRC1 expression in ESCC. a Promoter methylation of CTHRC1 in paired tissue specimens from 50 ESCC patients was detected by pyrosequencing assay. P < 0.0001, paired two-tailed Student’s t-test. b The number and percent of patients with higher or lower promoter methylation of CTHRC1 in ESCC tumour tissues compared with non-tumour tissues. T: tumour tissue; N: non-tumour tissue. c RT-PCR was performed to analyse the mRNA level of CTHRC1 in ESCC cells treated or not with the demethylating agent 5-aza-dC (10 μM) for 72 h. The significance of difference between groups was analysed using two-tailed Student’s t-test. Data are presented as the mean (n = 3) ± SD. *P < 0.05 and **P < 0.01. d Western blot was performed to detect the protein level of CTHRC1 in culture supernatants of cells with or without 5-aza-dC treatment. e Promoter methylation of CTHRC1 in ESCC cells with and without 5-aza-dC treatment was detected using a pyrosequencing assay
CTHRC1 promotes ESCC cell proliferation and tumour growth in vitro and in vivo
To investigate the effect of CTHRC1 on the malignant phenotypes of ESCC cells, we established cell models with CTHRC1 depletion or overexpression using three ESCC cell lines, and verified changes in expression by RT-PCR and western blot analyses (Fig. 3a, b). CTHRC1 depletion significantly attenuated cell proliferation and colony formation in KYSE510 and KYSE30 cells. Consistently, KYSE450 cells overexpressing CTHRC1 exhibited a significantly higher proliferation rate and colony formation capacity compared with KYSE450 cells transfected with the empty vector (Fig. 3c-e).
Fig. 3.
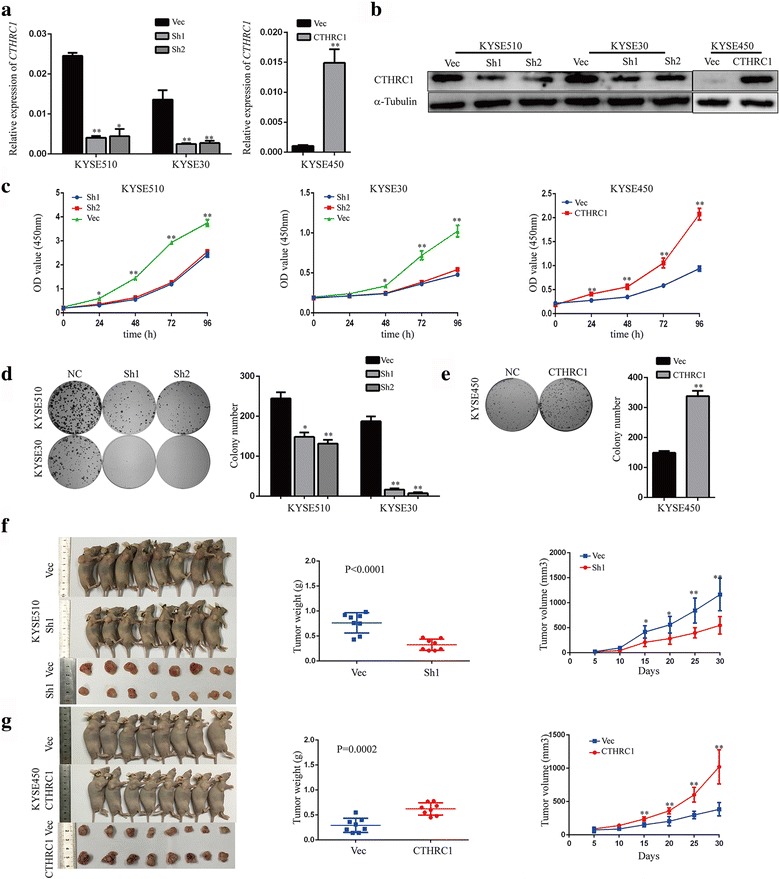
CTHRC1 is critical for ESCC cell proliferation and tumour growth. a, b Knockdown or overexpression efficiency of CTHRC1 in ESCC cells was verified by RT-PCR and western blot. c The proliferation capacity of KYSE510 and KYSE30 cells with depleted CTHRC1 expression and KYSE450 cells with enhanced CTHRC1 expression, as well as vector control cells was measured by CCK8 assay. d, e Representative images of colony formation assays using KYSE510, KYSE30 and KYSE450 cells (left). Columns show the mean number of clones formed in three independent experiments (right). f, g Representative images of tumour formation in nude mice subcutaneously inoculated with shCTHRC1- or vector-KYSE510 cells and CTHRC1- or vector-KYSE450 cells (left), and tumour weights and volumes for the two groups (right). The results are shown as the mean ± SD. The significance of the difference between groups was analysed using two-tailed Student’s t-test. *P < 0.05 and **P < 0.01
In agreement with the in vitro data, tumour size and weight were markedly reduced in the KYSE510-ShCTHRC1 group compared with the vector group (P < 0.0001, t-test, Fig. 3f), and KYSE450 cells with enhanced CTHRC1 expression formed significantly larger and heavier tumour xenografts compared to vector cells (P = 0.0002, t-test, Fig. 3g). Taken together, these results support the notion that CTHRC1 expression is critical for cell proliferation and tumour growth both in vitro and in vivo.
CTHRC1 promotes migration and invasion of ESCC cells in vitro and in vivo
To investigate the effect of CTHRC1 on the migration and invasion of ESCC cells, we conducted Boyden chamber Transwell assays. Overall, compared to cells transfected with the empty vector, migratory and invasive capacities were significantly suppressed in KYSE510 and KYSE30 cells with CTHRC1 knockdown (Fig. 4a, b) and remarkably enhanced in KYSE450 cells with CTHRC1 overexpression (Fig. 4c).
Fig. 4.
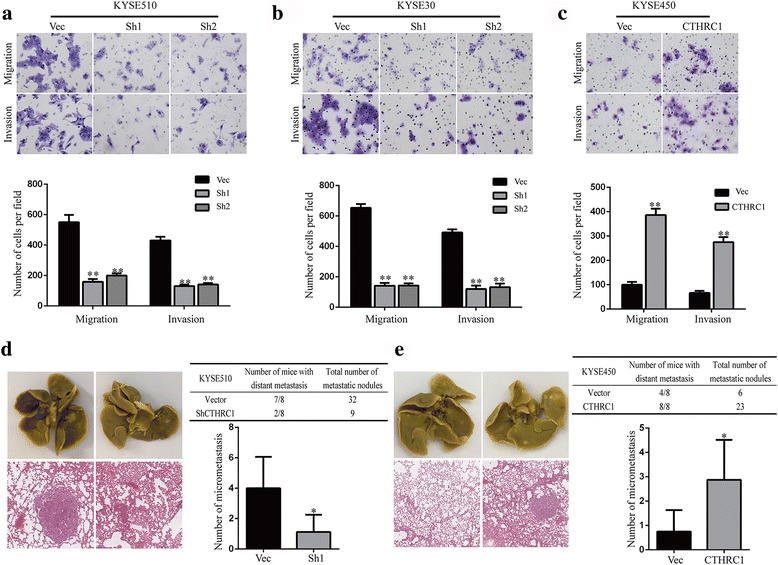
CTHRC1 facilitates migration and invasion of ESCC cells. Transwell assays were used to investigate migration and invasion of KYSE510 (a), KYSE30 (b) and KYSE450 (c) cells with altered CTHRC1 expression. d, e Representative images of isolated lungs (upper) and H&E-stained lung sections (lower) from each group. The number of mice with micrometastases and the total number of metastatic nodules of each group were also determined. Columns represent the mean number of metastatic nodules of each mouse. The results are shown as the mean ± SD. The P value was generated using two-tailed Student’s t-test. *P < 0.05 and **P < 0.01
A lung metastasis model in NOD-SCID mice constructed via tail vein injection of cells showed a significantly lower incidence of and fewer pulmonary metastasis nodules in mice with KYSE510-ShCTHRC1 cell injection than in the control group (Fig. 4d). On the other hand, the incidence and number of pulmonary metastatic nodules in mice with KYSE450-CTHRC1 cell injection were higher than in the control group (Fig. 4e).
CTHRC1 facilitates ESCC cells aggressiveness primarily via activation of the MAPK/MEK/ERK pathway
We next explored the downstream signalling pathways responsible for CTHRC1-mediated ESCC cell aggressiveness using RNA sequencing with KYSE510 cells carrying ShCTHRC1 or the empty vector. A total of 3430 significantly upregulated (more than 2-fold) and 4377 downregulated (less than 50%) genes were selected for Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis [22]. The results indicated the PI3K-Akt and MAPK pathways as the top two pathways most significantly affected by CTHRC1 knockdown (Fig. 5a).
Fig. 5.
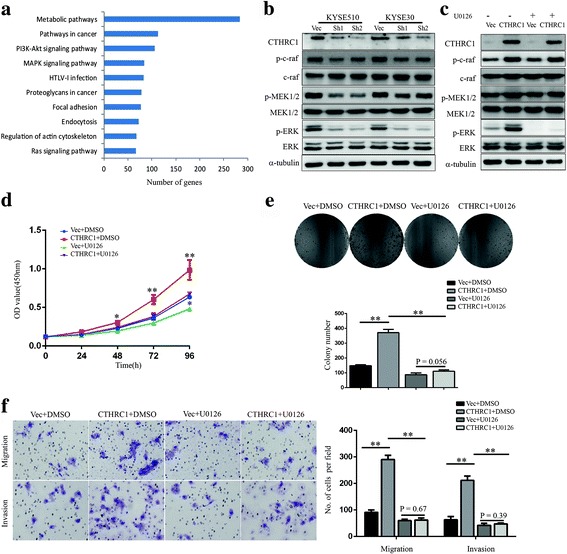
CTHRC1 exerts oncogenic functions by activating the MAPK/MEK/ERK pathway in ESCC cells. a Top-ranked KEGG pathway terms using DAVID. b Western blot was conducted to detect the protein levels of CTHRC1, c-raf, MEK1/2, ERK1/2 and phosphorylation of c-raf, MEK1/2, ERK1/2 in CTHRC1-knockdown KYSE510 and KYSE30 cells and corresponding vector control cells. c Western blot was conducted to detect the protein levels of CTHRC1, c-raf, MEK1/2, ERK1/2 and phosphorylation of c-raf, MEK1/2, ERK1/2 in CTHRC1-overexpressing KYSE450 cells and vector control cells. d-f KYSE450 with enhanced CTHRC1 expression and vector control cells were treated with the MEK inhibitor U0126 (10 μM) or dimethyl sulfoxide (DMSO). d Cell viability was measured using the CCK8 assay. e Colony formation assays were performed to measure the clonogenic capacity of cells. f Migration and invasion of cells were investigated using transwell assays. The results are shown as the mean ± SD. The difference between groups was analysed using two-tailed Student’s t-test. *P < 0.05 and **P < 0.01
Western blot verified that Akt phosphorylation was decreased in CTHRC1-depleted KYSE510 and KYSE30 cells, and increased in CTHRC1-overexpressing KYSE450 cells, but the changes were relatively minor (Additional file 5: Figure S3). We observed phosphorylation of core members of the classical MAPK pathway, c-raf, MEK1/2 and ERK1/2, to be strongly decreased in KYSE510-ShCTHRC1 cells and KYSE30-ShCTHRC1 cells, and increased in KYSE450-CTHRC1-overexpressed cells compared with their control cells (Fig. 5b, c). Furthermore, treatment with a MEK1/2 inhibitor (U0126 at 10 μM) significantly reversed CTHRC1-induced proliferation, migration and invasion of KYSE450 cells (Fig. 5d-f), indicating that MAPK/MEK/ERK activation may underlie the phenotypes induced by CTHRC1 in ESCC cells.
FRA-1 is the principle effector mediating activation of MAPK/MEK/ERK by CTHRC1 and upregulation of cyclin D1 and snail1/MMP14 expression
RNA sequencing analysis revealed FOSL1 (Fos-related antigen 1, also known as FRA-1), an extensively studied MAP Kinase target [23–25], to be among the most significantly downregulated genes (80% off); CCND1 (cyclin D1) (90% off), SNAI1 (snail1) (60% off) and a known target of snail1, MMP14 (matrix metallopeptidase 14, also known as MT1-MMP) (90% off) [26–28], were also significantly downregulated. Their dependency on CTHRC1 was repeatedly confirmed by RT-PCR and western blot in KYSE510 and KYSE30 cells with depleted CTHRC1 expression and in KYSE450 cells with CTHRC1 overexpression (Fig. 6a-c). Furthermore, administration of the MEK1/2 inhibitor U0126 abolished the increased phosphorylation of FRA-1 and increased protein levels of FRA-1, cyclin D1, snail1, and MMP14 induced by enhanced expression of CTHRC1 in KYSE450 cells (Fig. 6c).
Fig. 6.
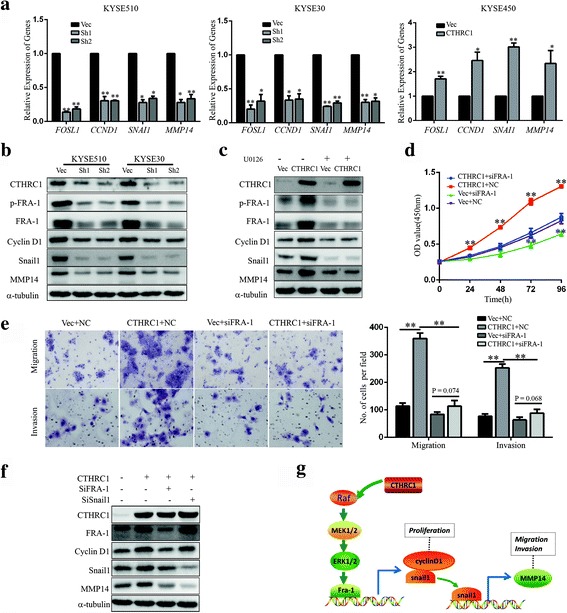
CTHRC1 upregulates cyclin D1 and snail1/MMP14 by activating the MAPK/MEK/ERK/FRA-1 cascade. a The relative mRNA levels of FOSL1, CCND1, SNAI1 and MMP14 in CTHRC1-knockdown cells or CTHRC1-overexpressing cells and control cells were detected by RT-PCR. b Western blot was conducted to detect the protein levels of CTHRC1, p-FRA-1, FRA-1, cyclin D1, snail1 and MMP14 in CTHRC1-knockdown KYSE510 and KYSE30 cells and corresponding vector control cells. c CTHRC1-overexpressing KYSE450 cells and control cells were treated with U0126 (10 μM) or DMSO. The protein levels of CTHRC1, p-FRA-1, FRA-1, cyclin D1, snail1 and MMP14 were detected by western blot. d, e CTHRC1-overexpressing KYSE450 cells and control cells were transfected with FRA-1 siRNA or negative control (NC) siRNA. d Cell viability was measured using the CCK8 assay. e Migration and invasion of cells were investigated using transwell assays. The results are shown as the mean ± SD. The difference between groups was analysed using two-tailed Student’s t-test. *P < 0.05 and **P < 0.01. f CTHRC1-overexpressing KYSE450 cells were transfected with FRA-1 siRNA or snail1 siRNA. The protein levels of CTHRC1, FRA-1, cyclin D1, snail1 and MMP14 in KYSE450 cells with different treatment were detected. g Schematic diagram illustrating the proposed CTHRC1-mediated activation of ERK1/2 signalling pathway and its role in ESCC cells
Moreover, knockdown of FRA-1 using siRNA reversed the promotion of proliferation, migration and invasion by CTHRC1 (Fig. 6d, e), and western blot showed that knockdown of FRA-1 attenuated the upregulation of cyclin D1, snail1, and MMP14 in KYSE450 cells induced by CTHRC1 overexpression. Additionally, knockdown of snail1 reversed the increased expression of MMP14 induced by CTHRC1 (Fig. 6f), indicating that cyclin D1 and snail1 were downstream effectors of FRA-1; in turn, snail1 induced high expression of MMP14 in CTHRC1-overexpressing ESCC cells (Fig. 6g).
Consistent with the above in vitro studies, the level of CTHRC1 mRNA was significantly positively correlated with those of CCND1 and SNAI1 in ESCC tumour tissues (n = 119, r = 0.227, P = 0.013; r = 0.550, P < 0.0001, Pearson’s correlation coefficient; Fig. 7a,b). Significant positive correlation between SNAI1 and MMP14 mRNA levels was also found (r = 0.318, P = 0.0004, Pearson’s correlation coefficient; Fig. 7c). Moreover, expression of CTHRC1 was positively associated with that of cyclin D1, as well as MMP14, at the protein level (n = 204, P = 0.018, chi square test; P = 0.022, chi square test; Table 1). In addition, Kaplan-Meier analysis revealed a significant association between shorter overall survival in ESCC patients and high expression of cyclin D1 (n = 204, P = 0.049, log-rank test, Fig. 7d), or MMP14 (n = 196, P = 0.0062, log-rank test; Fig. 7e).
Fig. 7.
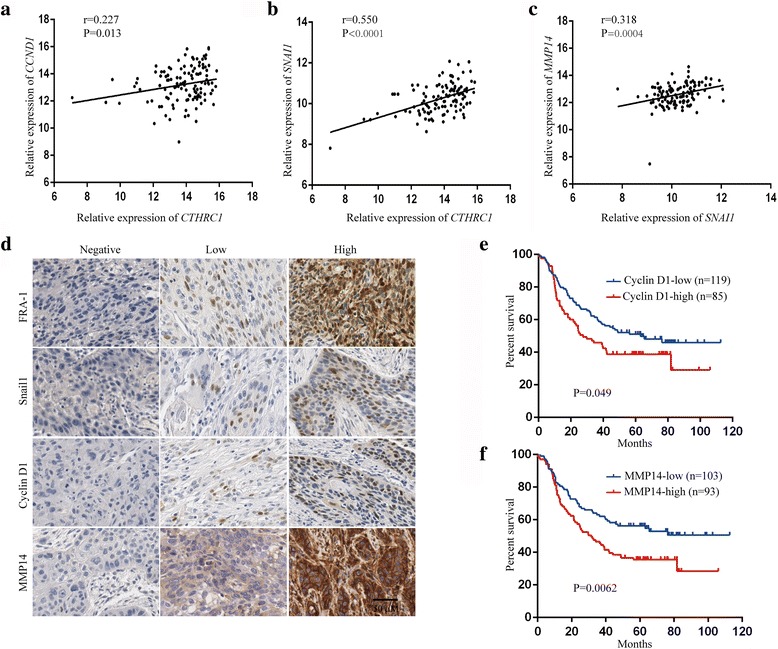
mRNA and protein level of CTHRC1, FRA-1, cyclin D1, snail1 and MMP14 in ESCC tissues. a Correlation between CTHRC1 and CCND1 according to transcriptome-wide microarray profiling data (n = 119). Pearson’s correlation coefficient. b Correlation between CTHRC1 and SNAI1 according to transcriptome-wide microarray profiling data (n = 119). Pearson’s correlation coefficient. c Correlation between SNAI1 and MMP14 according to transcriptome-wide microarray profiling data (n = 119). Pearson’s correlation coefficient. d Representative IHC images of FRA-1, snail1, cyclin D1 and MMP14 staining in ESCC tumour tissues. e, f Overall survival analysis based on the level of cyclin D1 and MMP14 expression, as measured by IHC, in ESCC patients. Survival rates were determined using Kaplan-Meier survival analysis
Discussion
This is the first study to present a comprehensive set of clinical and experimental evidence establishing CTHRC1 as an oncogenic factor that facilitates ESCC tumour progression and metastasis, resulting in poor prognosis. These data indicate that CTHRC1 may serve as a potential prognostic biomarker and treatment target in ESCC.
We also investigated the possible regulation mechanism of CTHRC1 in ESCC. Treatment with a demethylation agent (5-aza-dC) markedly elevated CTHRC1 expression in most ESCC cell lines, which was in agreement with previous reports [16, 29, 30]. A pyrosequencing assay revealed a CpG site (cg07757887, -1220 bp in the CTHRC1 genomic region) hypomethylated in ESCC tumour tissues, which has not been previously reported as being related to cancer. Although demethylation of the CTHRC1 genomic region (-391 to +4 bp) in gastric cancer cells [30], in the first exon in colon cancer [16], and at -628 to -269 of the promoter region in hepatocellular carcinoma [29] has been reported, we did not find significant demethylation at those CpG sites in ESCC tumour tissues. Therefore, methylation of the CpG site involved in regulating CTHRC1 may vary in different types of cancer.
Previous reports have suggested that other mechanisms may be involved in regulation of CTHRC1, such as TGF-β and Wnt3a pathway activation in gastric and oral squamous cell carcinoma, respectively [30, 31]. In addition, CTHRC1 was reported to be regulated by microRNA and long noncoding RNAs, such as let-7b and MALAT-1 [32, 33], which might explain the oncogenic role of MALAT-1 in ESCC [34]. Evidence to date supports the hypothesis that CTHRC1 integrates multiple pro-aggressiveness signalling pathways.
We also reveal for the first time that CTHRC1 exerts its effect on ESCC progression mainly through the Raf/MEK/ERK pathway, with dependence on the induction and activation of FRA-1, a FOS family transcription factor that binds to JUN-family proteins to form the AP-1 complex [35]. Transcriptional induction and post-translational stabilization of FRA-1 via MEK/ERK signalling increases the abundance of FRA-1, which has been causally linked to more aggressive behaviours of multiple cancer cell types [36–40], but not through a CTHRC1-dependent pathway.
There has been accumulating evidence for the significant role of MEK/ERK pathway in cancer development [41–44]. In accordance with the results of our study, the MEK/ERK pathway has been related to CTHRC1 in pancreatic cancer, without identification of any downstream effectors [45]. Another study suggested that CTHRC1 upregulated MMP9 via ERK activation in colorectal cancer [16]; however, alteration in MMP9 expression was not indicated in our RNA sequencing data. Through transcriptome sequencing and extensive step-by-step in vitro analyses, we identified Cyclin D1 and snail1 as major downstream effectors of FRA-1, accounting for the CTHRC1-mediated regulation of proliferation and motility in ESCC cells. The most prominent function of snail1 in cancer cells is to induce the epithelial-mesenchymal transition (EMT) [46, 47], and it was recently reported that CTHRC1 upregulated snail1 to induce EMT by activating the Wnt/β-catenin signalling pathway in epithelial ovarian cancer [48]. Interestingly, we did not observe any meaningful alteration in β-catenin expression or in hallmarks of EMT [49], namely, E-Cadherin and vimentin, after CTHRC1 knockdown in ESCC cell lines (Additional file 5: Figure S3), suggesting that an alternative hypothesis is needed to explain findings for ESCC. Indeed, a few recent studies invoked other possible mechanisms by which snail1 could regulate cell migration and invasion, such as MMP14-mediated pro-invasive and metastatic activities [26–28]. However, the respective upstream mechanisms were not elucidated. Here, we not only show that MMP14 can be upregulated by snail1 activation, but also demonstrate it under regulation of CTHRC1/MAPK/MEK/ERK/FRA-1 signalling in ESCC.
It should be acknowledged that there was one limitation related to this study: we did not clarify how CTHRC1 activates the MAPK/MEK/ERK pathway. It was recently demonstrated that EGFR inhibitors attenuated the promoting effect of CTHRC1 on epithelial ovarian cancer invasion and that phosphorylation of EGFR and ERK1/2 was reduced in CTHRC1-silenced ovarian cancer cells [50]. Since CTHRC1 is a secreted protein, it is worth investigating in future studies whether CTHRC1 acts as a ligand of EGFR to activate the MAPK/MEK/ERK pathway in ESCC.
Conclusions
In summary, our findings reveal that CTHRC1 plays a pivotal oncogenic role in ESCC proliferation, invasion, and metastasis by upregulating cyclin D1, snail1 and MMP14 through the Raf/MEK/ERK/FRA-1 pathway. Patients with high expression of CTHRC1 are possible candidates for biologic agents that affect the oncogenic circuit we found in ESCC, such as MEK1/2 inhibitors and CDK inhibitors. Additionally, the newly elucidated clinical implications of CTHRC1 in our cohort support its use as a potential prognostic marker for ESCC patients.
Additional files
Oligonucleotide primers used for RT-PCR. (DOCX 16 kb)
Verification of RNA-Seq data by RT-PCR. (DOCX 16 kb)
Analysis of Collagen triple helix repeat containing-1 (CTHRC1), Neural EGFL like 2 (NELL2), DLG associated protein 5 (DLGAP5), DEP domain containing 1 (DEPDC1), Zic family member 2 (ZIC2) and Centrosomal protein 55 (CEP55) mRNA levels according to previous transcriptome-wide microarray profiling data (n = 119). The P value was generated by Wilcoxon test. FC: Fold change. (TIF 554 kb)
Expression of CTHRC1 in ESCC cell lines was analysed by RT-PCR (a) and western blot analysis (b). (TIF 488 kb)
The levels of p-Akt, Akt, β-catenin, E-cadherin and vimentin proteins were determined by western blot in KYSE510 and KYSE30 cells depleted for CTHRC1 expression and KYSE450 cells overexpressing CTHRC1 as well as corresponding control cells. (TIF 670 kb)
Acknowledgements
We thank Ms. Meihua Xiong, Ms. Fang Zhou, and Ms. Jing Zhang of the Lab of the Department of Thoracic Surgery for administrative and technical help.
Funding
This work was supported by the National Natural Science Foundation of China [81502060] and the National Key Research and Development Program of China [2016YFC1303200, 2016YFC0901400].
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
JH, YG and CW contributed to study conception and design. CW performed molecular and cellular biology experiments, statistical analysis and interpretation. ZL, FS and XY were involved in sample collection, processing, and experiment operation. XF and SS performed pathological review and evaluated the data of immunohistochemistry. CW and YG wrote and revised the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The human tissue study protocol was approved by the Ethics Committee of Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (Beijing, China). All formalin-fixed and paraffin-embedded (FFPE) ESCC tissue samples were obtained with informed consent and agreement.
All animal experiments were performed in accordance with the guidelines approved by the Institutional Animal Care and Use Committee of Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (Beijing, China).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- BEGM
Bronchial epithelial cell growth
- CDS
Coding DNA sequence
- CEP55
Centrosomal protein 55
- CTHRC1
Collagen triple helix repeat containing-1
- DAPI
4’,6-diamidino-2-phenylindole
- DEG
Differentially expressed gene
- DEPDC1
DEP domain containing 1
- DLGAP5
DLG associated protein 5
- ESCC
Oesophageal squamous cell carcinoma
- FFPE
Formalin-fixed and paraffin-embedded
- FPKM
Fragments per kilobase of transcript per million mapped
- FRA-1
Fos-related antigen 1
- H&E
Haematoxylin and eosin staining
- IHC
Immunohistochemistry
- MMP14
Matrix metallopeptidase 14
- NC
Negative control
- NELL2
Neural EGFL like 2
- RNAi
RNA interference
- RT-PCR
Real-time polymerase chain reaction
- STR
Short tandem repeat
- TMA
Tissue microarray
- ZIC2
Zic family member 2
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s13046-017-0555-8) contains supplementary material, which is available to authorized users.
Contributor Information
Chunni Wang, Email: wangchunni@cicams.ac.cn.
Zitong Li, Email: lizitong@cicams.ac.cn.
Fei Shao, Email: shmf2009@live.cn.
Xueying Yang, Email: yangxueying@cicams.ac.cn.
Xiaoli Feng, Email: fengxiaoli@cicams.ac.cn.
Susheng Shi, Email: shisusheng@cicams.ac.cn.
Yibo Gao, Phone: 86-10-87788798, Email: gaoyibo@cicams.ac.cn.
Jie He, Phone: 86-10-87788207, Email: prof.jiehe@gmail.com.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381:400–12. [DOI] [PubMed]
- 3.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 4.Zhang SW, Zheng RS, Zuo TT, Zeng HM, Chen WQ, He J. Mortality and survival analysis of esophageal cancer in China. Zhonghua Zhong Liu Za Zhi. 2016;38:709–715. doi: 10.3760/cma.j.issn.0253-3766.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 5.Hosch SB, Stoecklein NH, Pichlmeier U, Rehders A, Scheunemann P, Niendorf A, et al. Esophageal cancer: the mode of lymphatic tumor cell spread and its prognostic significance. J Clin Oncol. 2001;19:1970–1975. doi: 10.1200/JCO.2001.19.7.1970. [DOI] [PubMed] [Google Scholar]
- 6.Pyagay P, Heroult M, Wang Q, Lehnert W, Belden J, Liaw L, et al. Collagen triple helix repeat containing 1, a novel secreted protein in injured and diseased arteries, inhibits collagen expression and promotes cell migration. Circ Res. 2005;96:261–268. doi: 10.1161/01.RES.0000154262.07264.12. [DOI] [PubMed] [Google Scholar]
- 7.Durmus T, LeClair RJ, Park KS, Terzic A, Yoon JK, Lindner V. Expression analysis of the novel gene collagen triple helix repeat containing-1 (Cthrc1) Gene Expr Patterns. 2006;6:935–940. doi: 10.1016/j.modgep.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 8.LeClair RJ, Durmus T, Wang Q, Pyagay P, Terzic A, Lindner V. Cthrc1 is a novel inhibitor of transforming growth factor-beta signaling and neointimal lesion formation. Circ Res. 2007;100:826–833. doi: 10.1161/01.RES.0000260806.99307.72. [DOI] [PubMed] [Google Scholar]
- 9.Tang L, Dai DL, Su M, Martinka M, Li G, Zhou Y. Aberrant expression of collagen triple helix repeat containing 1 in human solid cancers. Clin Cancer Res. 2006;12:3716–3722. doi: 10.1158/1078-0432.CCR-06-0030. [DOI] [PubMed] [Google Scholar]
- 10.Ke Z, He W, Lai Y, Guo X, Chen S, Li S, et al. Overexpression of collagen triple helix repeat containing 1 (CTHRC1) is associated with tumour aggressiveness and poor prognosis in human non-small cell lung cancer. Oncotarget. 2014;5:9410–9424. doi: 10.18632/oncotarget.2421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gu L, Liu L, Zhong L, Bai Y, Sui H, Wei X, et al. Cthrc1 overexpression is an independent prognostic marker in gastric cancer. Hum Pathol. 2014;45:1031–1038. doi: 10.1016/j.humpath.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 12.Wang SF, Yin Z, Yin JJ, Zhang W, Dong CG. Clinical significance of CTHRC1 protein expression in human cancers: a meta-analysis. Genet Mol Res. 2016;15. doi:10.4238/gmr.15027855. [DOI] [PubMed]
- 13.Orloff M, Peterson C, He X, Ganapathi S, Heald B, Yang YR, et al. Germline mutations in MSR1, ASCC1, and CTHRC1 in patients with Barrett esophagus and esophageal adenocarcinoma. JAMA. 2011;306:410–419. doi: 10.1001/jama.2011.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warnecke-Eberz U, Metzger R, Holscher AH, Drebber U, Bollschweiler E. Diagnostic marker signature for esophageal cancer from transcriptome analysis. Tumour Biol. 2016;37:6349–6358. doi: 10.1007/s13277-015-4400-4. [DOI] [PubMed] [Google Scholar]
- 15.Su H, Hu N, Yang HH, Wang C, Takikita M, Wang QH, et al. Global gene expression profiling and validation in esophageal squamous cell carcinoma and its association with clinical phenotypes. Clin Cancer Res. 2011;17:2955–2966. doi: 10.1158/1078-0432.CCR-10-2724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim HC, Kim YS, Oh HW, Kim K, Oh SS, Kim JT, et al. Collagen triple helix repeat containing 1 (CTHRC1) acts via ERK-dependent induction of MMP9 to promote invasion of colorectal cancer cells. Oncotarget. 2014;5:519–529. doi: 10.18632/oncotarget.1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shi X, Chen Z, Hu X, Luo M, Sun Z, Li J, et al. AJUBA promotes the migration and invasion of esophageal squamous cell carcinoma cells through upregulation of MMP10 and MMP13 expression. Oncotarget. 2016;7:36407–36418. doi: 10.18632/oncotarget.9239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang W, Zhou C, Luo M, Shi X, Li Y, Sun Z, et al. MiR-652-3p is upregulated in non-small cell lung cancer and promotes proliferation and metastasis by directly targeting Lgl1. Oncotarget. 2016;7:16703–16715. doi: 10.18632/oncotarget.7697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang C, Wang L, Su B, Lu N, Song J, Yang X, et al. Serine protease inhibitor Kazal type 1 promotes epithelial-mesenchymal transition through EGFR signaling pathway in prostate cancer. Prostate. 2014;74:689–701. doi: 10.1002/pros.22787. [DOI] [PubMed] [Google Scholar]
- 20.Li J, Chen Z, Tian L, Zhou C, He MY, Gao Y, et al. LncRNA profile study reveals a three-lncRNA signature associated with the survival of patients with oesophageal squamous cell carcinoma. Gut. 2014;63:1700–1710. doi: 10.1136/gutjnl-2013-305806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gao YB, Chen ZL, Li JG, Hu XD, Shi XJ, Sun ZM, et al. Genetic landscape of esophageal squamous cell carcinoma. Nat Genet. 2014;46:1097–1102. doi: 10.1038/ng.3076. [DOI] [PubMed] [Google Scholar]
- 22.Kanehisa M, Goto S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lau EY, Lo J, Cheng BY, Ma MK, Lee JM, Ng JK, et al. Cancer-Associated Fibroblasts Regulate Tumor-Initiating Cell Plasticity in Hepatocellular Carcinoma through c-Met/FRA1/HEY1 Signaling. Cell Rep. 2016;15:1175–1189. doi: 10.1016/j.celrep.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 24.Doehn U, Hauge C, Frank SR, Jensen CJ, Duda K, Nielsen JV, et al. RSK is a principal effector of the RAS-ERK pathway for eliciting a coordinate promotile/invasive gene program and phenotype in epithelial cells. Mol Cell. 2009;35:511–522. doi: 10.1016/j.molcel.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Basbous J, Chalbos D, Hipskind R, Jariel-Encontre I, Piechaczyk M. Ubiquitin-independent proteasomal degradation of Fra-1 is antagonized by Erk1/2 pathway-mediated phosphorylation of a unique C-terminal destabilizer. Mol Cell Biol. 2007;27:3936–3950. doi: 10.1128/MCB.01776-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ota I, Li XY, Hu Y, Weiss SJ. Induction of a MT1-MMP and MT2-MMP-dependent basement membrane transmigration program in cancer cells by Snail1. Proc Natl Acad Sci U S A. 2009;106:20318–20323. doi: 10.1073/pnas.0910962106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miyoshi A, Kitajima Y, Sumi K, Sato K, Hagiwara A, Koga Y, et al. Snail and SIP1 increase cancer invasion by upregulating MMP family in hepatocellular carcinoma cells. Br J Cancer. 2004;90:1265–1273. doi: 10.1038/sj.bjc.6601685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jiang W, Zhang Y, Kane KT, Collins MA, Simeone DM, di Magliano MP, et al. CD44 regulates pancreatic cancer invasion through MT1-MMP. Mol Cancer Res. 2015;13:9–15. doi: 10.1158/1541-7786.MCR-14-0076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bai L, Zhang W, Tan L, Yang H, Ge M, Zhu C, et al. Hepatitis B virus hijacks CTHRC1 to evade host immunity and maintain replication. J Mol Cell Biol. 2015;7:543–556. doi: 10.1093/jmcb/mjv048. [DOI] [PubMed] [Google Scholar]
- 30.Wang P, Wang YC, Chen XY, Shen ZY, Cao H, Zhang YJ, et al. CTHRC1 is upregulated by promoter demethylation and transforming growth factor-beta1 and may be associated with metastasis in human gastric cancer. Cancer Sci. 2012;103:1327–1333. doi: 10.1111/j.1349-7006.2012.02292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu G, Sengupta PK, Jamal B, Yang HY, Bouchie MP, Lindner V, et al. N-glycosylation induces the CTHRC1 protein and drives oral cancer cell migration. J Biol Chem. 2013;288:20217–20227. doi: 10.1074/jbc.M113.473785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yu J, Feng J, Zhi X, Tang J, Li Z, Xu Y, et al. Let-7b inhibits cell proliferation, migration, and invasion through targeting Cthrc1 in gastric cancer. Tumour Biol. 2015;36:3221–3229. doi: 10.1007/s13277-014-2950-5. [DOI] [PubMed] [Google Scholar]
- 33.Tano K, Mizuno R, Okada T, Rakwal R, Shibato J, Masuo Y, et al. MALAT-1 enhances cell motility of lung adenocarcinoma cells by influencing the expression of motility-related genes. FEBS Lett. 2010;584:4575–4580. doi: 10.1016/j.febslet.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 34.Hu L, Wu Y, Tan D, Meng H, Wang K, Bai Y, et al. Up-regulation of long noncoding RNA MALAT1 contributes to proliferation and metastasis in esophageal squamous cell carcinoma. J Exp Clin Cancer Res. 2015;34:7. doi: 10.1186/s13046-015-0123-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ransone LJ, Verma IM. Nuclear proto-oncogenes fos and jun. Annu Rev Cell Biol. 1990;6:539–557. doi: 10.1146/annurev.cb.06.110190.002543. [DOI] [PubMed] [Google Scholar]
- 36.Pollock CB, Shirasawa S, Sasazuki T, Kolch W, Dhillon AS. Oncogenic K-RAS is required to maintain changes in cytoskeletal organization, adhesion, and motility in colon cancer cells. Cancer Res. 2005;65:1244–1250. doi: 10.1158/0008-5472.CAN-04-1911. [DOI] [PubMed] [Google Scholar]
- 37.Adiseshaiah P, Lindner DJ, Kalvakolanu DV, Reddy SP. FRA-1 proto-oncogene induces lung epithelial cell invasion and anchorage-independent growth in vitro, but is insufficient to promote tumor growth in vivo. Cancer Res. 2007;67:6204–6211. doi: 10.1158/0008-5472.CAN-06-4687. [DOI] [PubMed] [Google Scholar]
- 38.Belguise K, Kersual N, Galtier F, Chalbos D. FRA-1 expression level regulates proliferation and invasiveness of breast cancer cells. Oncogene. 2005;24:1434–1444. doi: 10.1038/sj.onc.1208312. [DOI] [PubMed] [Google Scholar]
- 39.Debinski W, Gibo DM. Fos-related antigen 1 modulates malignant features of glioma cells. Mol Cancer Res. 2005;3:237–249. doi: 10.1158/1541-7786.MCR-05-0004. [DOI] [PubMed] [Google Scholar]
- 40.Vial E, Sahai E, Marshall CJ. ERK-MAPK signaling coordinately regulates activity of Rac1 and RhoA for tumor cell motility. Cancer Cell. 2003;4:67–79. [DOI] [PubMed]
- 41.Ding C, Luo J, Li L, Li S, Yang L, Pan H, et al. Gab2 facilitates epithelial-to-mesenchymal transition via the MEK/ERK/MMP signaling in colorectal cancer. J Exp Clin Cancer Res. 2016;35:5. doi: 10.1186/s13046-015-0280-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao L, Wang Y, Jiang L, He M, Bai X, Yu L, et al. MiR-302a/b/c/d cooperatively sensitizes breast cancer cells to adriamycin via suppressing P-glycoprotein(P-gp) by targeting MAP/ERK kinase kinase 1 (MEKK1) J Exp Clin Cancer Res. 2016;35:25. doi: 10.1186/s13046-016-0300-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoon S, Seger R. The extracellular signal-regulated kinase: multiple substrates regulate diverse cellular functions. Growth Factors. 2006;24:21–44. [DOI] [PubMed]
- 44.Dhillon AS, Hagan S, Rath O, Kolch W. MAP kinase signalling pathways in cancer. Oncogene. 2007;26:3279–3290. doi: 10.1038/sj.onc.1210421. [DOI] [PubMed] [Google Scholar]
- 45.Park EH, Kim S, Jo JY, Kim SJ, Hwang Y, Kim JM, et al. Collagen triple helix repeat containing-1 promotes pancreatic cancer progression by regulating migration and adhesion of tumor cells. Carcinogenesis. 2013;34:694–702. doi: 10.1093/carcin/bgs378. [DOI] [PubMed] [Google Scholar]
- 46.Peinado H, Olmeda D, Cano A. Snail, Zeb and bHLH factors in tumour progression: an alliance against the epithelial phenotype? Nat Rev Cancer. 2007;7:415–428. doi: 10.1038/nrc2131. [DOI] [PubMed] [Google Scholar]
- 47.Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009;9:265–273. doi: 10.1038/nrc2620. [DOI] [PubMed] [Google Scholar]
- 48.Hou M, Cheng Z, Shen H, He S, Li Y, Pan Y, et al. High expression of CTHRC1 promotes EMT of epithelial ovarian cancer (EOC) and is associated with poor prognosis. Oncotarget. 2015;6:35813–35829. doi: 10.18632/oncotarget.3436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2:442–454. doi: 10.1038/nrc822. [DOI] [PubMed] [Google Scholar]
- 50.Ye J, Chen W, Wu ZY, Zhang JH, Fei H, Zhang LW, et al. Upregulated CTHRC1 promotes human epithelial ovarian cancer invasion through activating EGFR signaling. Oncol Rep. 2016;36:3588–3596. doi: 10.3892/or.2016.5198. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Oligonucleotide primers used for RT-PCR. (DOCX 16 kb)
Verification of RNA-Seq data by RT-PCR. (DOCX 16 kb)
Analysis of Collagen triple helix repeat containing-1 (CTHRC1), Neural EGFL like 2 (NELL2), DLG associated protein 5 (DLGAP5), DEP domain containing 1 (DEPDC1), Zic family member 2 (ZIC2) and Centrosomal protein 55 (CEP55) mRNA levels according to previous transcriptome-wide microarray profiling data (n = 119). The P value was generated by Wilcoxon test. FC: Fold change. (TIF 554 kb)
Expression of CTHRC1 in ESCC cell lines was analysed by RT-PCR (a) and western blot analysis (b). (TIF 488 kb)
The levels of p-Akt, Akt, β-catenin, E-cadherin and vimentin proteins were determined by western blot in KYSE510 and KYSE30 cells depleted for CTHRC1 expression and KYSE450 cells overexpressing CTHRC1 as well as corresponding control cells. (TIF 670 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


