Abstract
Systemic hyperaminoacidemia, induced by either intravenous amino acid infusion or protein ingestion, reduces insulin-stimulated glucose disposal. Studies of mice suggest that the valine metabolite 3-hydroxyisobutyrate (3-HIB), fibroblast growth factor 21 (FGF21), adiponectin, and nonesterified fatty acids (NEFAs) may be involved in amino acid–mediated insulin resistance. We therefore measured in 30 women the rate of glucose disposal, and plasma 3-HIB, FGF21, adiponectin, and NEFA concentrations, under basal conditions and during a hyperinsulinemic-euglycemic clamp procedure (HECP), with and without concomitant ingestion of protein (n = 15) or an amount of leucine that matched the amount of protein (n = 15). We found that during the HECP without protein or leucine ingestion, the grand mean ± SEM plasma 3-HIB concentration decreased (from 35 ± 2 to 14 ± 1 µmol/L) and the grand median [quartiles] FGF21 concentration increased (from 178 [116, 217] to 509 [340, 648] pg/mL). Ingestion of protein, but not leucine, decreased insulin-stimulated glucose disposal (P < 0.05) and prevented both the HECP-mediated decrease in 3-HIB and increase in FGF21 concentration in plasma. Neither protein nor leucine ingestion altered plasma adiponectin or NEFA concentrations. These findings suggest that 3-HIB and FGF21 might be involved in protein-mediated insulin resistance in humans.
Introduction
Systemic hyperaminoacidemia, induced by either intravenous amino acid infusion or protein ingestion, acutely reduces insulin-stimulated glucose disposal (1–3), and chronic high protein intake is associated with an increased risk of type 2 diabetes (4–7). The mechanism(s) responsible for the adverse effects of dietary protein intake and the concomitant increase in circulating amino acids on insulin sensitivity is not clear. Leucine-mediated mammalian target of rapamycin (mTOR) signaling in muscle, which can inhibit phosphoinositide 3-kinase/protein kinase B (also known as AKT) signaling, has been considered a major cause of amino acid–induced insulin resistance (8,9). However, we recently demonstrated a dissociation between increased mTOR signaling in muscle, induced by protein or leucine ingestion, and insulin resistance in humans (3). Despite the same increase in mTOR signaling in muscle after ingestion of either protein or leucine (matching the amount of leucine present in the ingested protein), ingestion of protein, but not leucine, inhibited insulin-stimulated glucose disposal (3).
Data from a series of studies conducted in mice suggest two new potential mechanisms for amino acid–induced insulin resistance that involve alterations in 3-hydoxyisobutyrate (3-HIB) and fibroblast growth factor 21 (FGF21) metabolism. 3-HIB, a metabolite of the branched-chain amino acid valine, induced insulin resistance presumably by increasing fatty acid uptake in muscle (10), and FGF21, which is predominantly secreted by the liver (11), increased secretion by adipose tissue of the insulin-sensitizing hormone adiponectin, but may also have direct endocrine and/or autocrine insulin-sensitizing effects in skeletal muscle (11–15). Restriction of dietary protein, or branched-chain amino acids (combined leucine, isoleucine, and valine, or leucine alone), or methionine was found to increase basal plasma FGF21 concentration in animals and humans (16–22). However, the interpretation of these results is confounded by a decrease in body weight associated with protein/amino acid restriction in these studies. Peroxisome proliferator–activated receptor γ coactivator 1-α (PPARGC1A) could provide a potential cellular mechanism that links protein ingestion, 3-HIB, FGF21, and insulin resistance. PPARGC1A suppresses FGF21 expression in the liver (23,24) and increases the gene expression of key enzymes involved in branched-chain amino acid catabolism in muscle (10). In mice, a high-protein diet stimulates PPARGC1A expression (25).
The goal of this study was to determine whether the difference we observed between the effects of protein and matched leucine ingestion on insulin sensitivity is related to differences in PPARGC1A expression in muscle and plasma 3-HIB and FGF21 concentrations. We hypothesized that ingestion of protein, but not leucine, would increase PPARGC1A gene expression in muscle, increase plasma 3-HIB concentration, and decrease plasma FGF21 concentration and that these alterations would be associated with increased gene expression of key enzymes involved in branched-chain amino acid and FGF21 metabolism in muscle and plasma adiponectin concentration. Accordingly, we measured the gene expression of PPARGC1A, branched-chain amino transferase 2 (BCAT2), branched-chain α-keto acid dehydrogenase (BCKDHA), and FGF21 in muscle and plasma 3-HIB, FGF21, and adiponectin concentrations during both basal conditions and a hyperinsulinemic-euglycemic clamp procedure (HECP) with and without concomitant ingestion of protein or leucine (which matched the amount of leucine provided in the protein load).
Research Design and Methods
Subjects
Thirty sedentary, 50- to 65-year-old women with a stable weight (weight change <2 kg for 3 months) (Table 1) participated in this study, which was approved by the Institutional Review Board of Washington University School of Medicine in St. Louis, St. Louis, MO. Written informed consent was obtained from all subjects before participation. All subjects were evaluated through a history and physical examination, a resting 12-lead electrocardiogram, standard blood tests, an oral glucose tolerance test, and the Michigan Alcohol Screening Test. None of the subjects had evidence of chronic illness or significant organ dysfunction (e.g., diabetes, liver cirrhosis), or were taking medications (including hormone replacement therapy) that could affect insulin or glucose metabolism, and none consumed tobacco products, reported regular consumption of >115 g alcohol/week, or scored >2 points on the Michigan Alcohol Screening Test. Glucose kinetics in 22 of the 30 subjects were previously reported in a study that evaluated the effects of protein and leucine ingestion on muscle mTOR and AKT phosphorylation and insulin-mediated glucose disposal (3).
Table 1.
Subjects’ body composition and metabolic characteristics at screening
| Protein group (n = 15) | Leucine group (n = 15) | |
|---|---|---|
| Age (years) | 57.0 ± 0.9 | 59.6 ± 1 |
| BMI (kg/m2) | 34.2 ± 0.9 | 36.4 ± 1.2 |
| Body mass (kg) | 92.0 ± 2.4 | 97.6 ± 3.5 |
| Fat-free mass (kg) | 47.3 ± 1.2 | 47.9 ± 1.1 |
| Body fat (%) | 48.5 ± 0.8 | 50.5 ± 1.1 |
| Subcutaneous abdominal adipose tissue volume (cm3) | 2,980 ± 104 | 3,370 ± 225 |
| Intra-abdominal adipose tissue volume (cm3) | 1,463 ± 126 | 1,342 ± 181 |
| Intrahepatic triglyceride content (%) | 8.4 ± 1.9 | 7.4 ± 1.6 |
| Plasma concentrations | ||
| Glucose (mmol/L) | ||
| Basal | 5.1 ± 0.1 | 5.5 ± 0.1 |
| 2 h after OGTT | 7.2 ± 0.5 | 7.7 ± 0.4 |
| Triglycerides (mmol/L) | 1.7 ± 0.2 | 1.2 ± 0.2 |
| Total cholesterol (mmol/L) | 5.7 ± 0.3 | 5.2 ± 0.2 |
| HDL cholesterol (mmol/L) | 1.5 ± 0.1 | 1.6 ± 0.1 |
| LDL cholesterol (mmol/L) | 3.5 ± 0.2 | 3.1 ± 0.2 |
Values are mean ± SEM. OGTT, oral glucose tolerance test.
Experimental Design
Subjects’ body fat mass and fat-free mass were determined using DEXA (Lunar iDXA; GE Healthcare). Intra-abdominal adipose tissue and subcutaneous abdominal adipose tissue volumes and intrahepatic triglyceride content were quantified using MRI/MRS (1.5-T superconducting magnet; Siemens, Iselin, NJ). Each subject was then randomized to ingest either protein (n = 15) or leucine (n = 15) and completed two HECPs: one with and one without simultaneous protein ingestion during the HECP, or one with and one without simultaneous leucine ingestion during the HECP. On each occasion, subjects were admitted to the Clinical Research Unit, where they consumed a standard 800-kcal dinner (50% carbohydrate, 30% fat, 20% protein) between 1800 and 1900 h. Subjects then fasted, except for water, until the next morning. At 0600 h, catheters were inserted into an arm vein for the infusion of stable isotopically labeled glucose, insulin, and dextrose, and into a radial artery and a femoral vein for blood sampling. At ∼0645 h, a primed, constant intravenous infusion of [6,6-2H2] glucose was started, and a 4-h HECP (insulin infusion rate 50 mU · m−2 body surface area · min−1) was initiated 4 h later. Euglycemia (plasma glucose concentration ∼5.6 mmol/L) was maintained during the HECP by variable-rate infusion of 20% dextrose (Baxter, Deerfield, IL) enriched to 2.5% with [6,6-2H2] glucose. Subjects in the protein group consumed a total of 0.6 g protein/kg fat-free mass (containing 0.0684 g leucine/kg fat-free mass) and subjects in the leucine group consumed a total of 0.0684 g leucine/kg fat-free mass in small aliquots every 20 min during one of the two HECPs. Blood samples were obtained immediately before starting the glucose tracer infusion; every 10 min during the last 30 min of the basal period; and 60, 120, 180, 220, 230, and 240 min after starting the HECP in order to determine plasma metabolite and hormone concentrations and glucose kinetics. Muscle tissue from the quadriceps femoris was obtained 60 min after starting the glucose tracer infusion (basal period) and 180 min after starting the insulin infusion to determine PPARGC1A, BCAT2, BCKDHA, and FGF21 gene expression.
Sample Analyses
Blood samples were collected in chilled tubes containing heparin (to determine glucose and insulin concentrations) or EDTA (to determine 3-HIB, FGF21, adiponectin, nonesterified fatty acid [NEFA], and amino acid concentrations and glucose enrichment). Samples were placed in ice, and plasma was separated by centrifugation within 30 min of collection and then stored at −80°C until final analyses. Muscle samples were rinsed in ice-cold saline immediately after collection, cleared of visible fat and connective tissue, frozen in liquid nitrogen, and stored at −80°C until final analysis.
Plasma glucose concentration was determined using an automated glucose analyzer (Yellow Spring Instruments Co, Yellow Springs, OH). ELISAs were used to determine plasma insulin (EMD Millipore, St. Charles, MO), FGF21, and high–molecular weight adiponectin (both R&D Systems, Minneapolis, MN) concentrations. The coefficient of variation for FGF21 was 2.1% at 250 pg/mL and 1.3% at 500 pg/mL. Plasma leucine and 3-HIB concentrations were determined using gas chromatography–mass spectrometry (GC-MS; MSD 5973 System; Hewlett-Packard) as their t-butyldimethylsilyl derivative after adding a known amount of nor-leucine and β-hydroxybutyrate to aliquots of each plasma sample. The coefficient of variation for 3-HIB was 2.1% at 13.7 μmol/L and 2.2% at 25.2 μmol/L. Total plasma amino acid concentration was determined by using the EZ:faast Physiological (Free) Amino Acid Kit (Phenomenex, Torrence, CA) and GC-MS analysis per the manufacturer’s instructions. Total plasma NEFA concentration was determined using an enzymatic colorimetric assay (Sigma-Aldrich, St. Louis, MO). The glucose tracer-to-tracee ratio in plasma was determined using GC-MS (Hewlett-Packard MSD 5973 system with a capillary column) after derivatizing glucose with acetic anhydride.
Gene expression in muscle was assessed using the RT-PCR technique and normalizing the cycle threshold value of each sample to the housekeeping control gene, ribosomal protein (RPLP0), as previously described (26). Total RNA was isolated from frozen muscle samples using Trizol reagent (Invitrogen, Carlsbad, CA), quantified spectrophotometrically (NanoDrop 1000 spectrophotometer; Thermo Fisher Scientific, Waltham, MA), and reverse transcribed (High-Capacity cDNA Reverse Transcription Kit; Invitrogen). Gene expression was determined using an ABI 7500 real-time PCR system (Invitrogen) and SYBR Green Master Mix (Invitrogen), with the following primers: PPARGC1A (accession no. NM_013261), 5′-TCTGAGTCTGTATGGAGTGACAT-3′ (forward), and 5′-CCAAGTCGTTCACATCTAGTTCA-3′ (reverse); BCAT2 (accession no. NM_001190), 5′-GCTCAACATGGACCGGATG-3′ (forward), and 5′-CCGCACATAGAGGCTGGTG-3′ (reverse); BCKDHA (accession no. NM_001164783), 5′-CTACAAGAGCATGACACTGCTT-3′ (forward), and 5′-CCCTCCTCACCATAGTTGGTC-3′ (reverse); FGF21 (accession no. NM_019113), 5′-GCCTTGAAGCCGGGAGTTATT-3′ (forward), and 5′-GTGGAGCGATCCATACAGGG-3′ (reverse); RPLP0 (accession no. NM_053275), 5′-GTGATGTGCAGCTGATCAAGACT-3′ (forward), and 5′-GATGACCAGCCCAAAGGAGA-3′ (reverse).
Calculations
Glucose rate of disappearance (Rd) in plasma in the basal state and during the HECP was calculated by dividing the glucose tracer infusion rate by the average plasma glucose tracer-to-tracee ratio during the last 20 min of the basal period and HECP, when metabolic and isotopic steady states were achieved, and adding the glucose tracer infusion rate to this value.
Statistical Analyses
Statistical analyses were carried out with SPSS version 22 for Windows (IBM, Armonk, NY). All data sets were tested for normality using the Kolmogorov-Smirnov test, and skewed data sets were log-transformed for further analysis. Repeated measures ANOVA and the Tukey post hoc procedure were used to evaluate the effects of protein and leucine ingestion on outcome measures. A P value ≤0.05 was considered statistically significant. Data are presented as mean ± SEM or median (quartiles) for normally distributed and skewed data sets, respectively.
Results
Plasma Glucose, Insulin, NEFA, and Amino Acid Concentrations
Basal plasma glucose, insulin, NEFA, and amino acid concentrations were not different between the protein and leucine ingestion groups. Plasma glucose concentration during the HECP was not different among the different studies, but plasma insulin concentration during the HECP was ∼12% higher with concomitant protein ingestion than the respective control and the leucine ingestion and control studies. Plasma NEFA concentration decreased by ∼90% during the HECP in all studies. Total amino acid, total branched-chain amino acid, leucine, valine, total essential amino acid, and nonessential amino acid concentrations decreased by ∼20–45% during the HECP compared with basal conditions in the control studies. Both protein and leucine ingestion during the HECP approximately doubled plasma leucine concentration compared with the basal condition, whereas ingestion of only protein, not of leucine, increased plasma valine concentration by ∼25% compared with basal conditions. Total amino acid and total branched-chain, total essential, and nonessential amino acid concentrations increased (compared with basal conditions) only after ingestion of protein, not leucine, during the HECP (Table 2 and Supplementary Fig. 1).
Table 2.
Effects of protein and leucine ingestion on arterial plasma glucose, insulin, NEFA, and amino acid concentrations
| Protein group |
Leucine group |
|||
|---|---|---|---|---|
| Control | Protein | Control | Leucine | |
| Glucose (mmol/L) | ||||
| Basal | 5.13 ± 0.05 | 5.15 ± 0.06 | 5.34 ± 0.13 | 5.27 ± 0.09 |
| Clamp | 5.65 ± 0.05* | 5.65 ± 0.06* | 5.57 ± 0.05* | 5.56 ± 0.04* |
| Insulin (pmol/L) | ||||
| Basal | 48 ± 8 | 44 ± 6 | 40 ± 5 | 40 ± 5 |
| Clamp | 404 ± 28* | 459 ± 33*† | 380 ± 31* | 386 ± 23*‡ |
| NEFAs (μmol/L) | ||||
| Basal | 667 ± 55 | 758 ± 56 | 742 ± 35 | 684 ± 30 |
| Clamp | 63 ± 8* | 73 ± 11* | 68 ± 12* | 63 ± 15* |
| Leucine (µmol/L) | ||||
| Basal | 113 ± 4 | 120 ± 3 | 116 ± 5 | 114 ± 5 |
| Clamp | 63 ± 5* | 222 ± 13*† | 62 ± 4* | 236 ± 16*† |
| Valine (µmol/L) | ||||
| Basal | 210 ± 8 | 223 ± 5 | 206 ± 7 | 204 ± 8 |
| Clamp | 151 ± 9* | 297 ± 10*† | 148 ± 7* | 104 ± 7*†‡ |
| Total branched-chain amino acids (µmol/L) | ||||
| Basal | 373 ± 13 | 396 ± 9 | 367 ± 11 | 362 ± 14 |
| Clamp | 239 ± 15* | 647 ± 27*† | 231 ± 11* | 351 ± 21†‡ |
| Essential amino acids (µmol/L) | ||||
| Basal | 836 ± 31 | 868 ± 26 | 799 ± 28 | 795 ± 30 |
| Clamp | 593 ± 32* | 1,403 ± 56*† | 575 ± 24* | 684 ± 28*†‡ |
| Nonessential amino acids (µmol/L) | ||||
| Basal | 933 ± 33 | 940 ± 35 | 902 ± 29 | 938 ± 24 |
| Clamp | 737 ± 28* | 1,037 ± 31*† | 762 ± 25* | 764 ± 45*‡ |
| Total amino acids (µmol/L) | ||||
| Basal | 1,770 ± 62 | 1,808 ± 56 | 1,700 ± 48 | 1,733 ± 47 |
| Clamp | 1,330 ± 58* | 2,440 ± 82*† | 1,337 ± 42* | 1,448 ± 63*†‡ |
Values are mean ± SEM.
*Value is significantly different from the corresponding basal value (P < 0.01).
†Value is significantly different from the corresponding control values (P < 0.01).
‡Value is significantly different from the corresponding value in the protein group (P < 0.01).
Muscle Insulin Sensitivity and Plasma 3-HIB, FGF21, and Adiponectin Concentrations
Basal glucose Rd was not different in the control and protein ingestion studies (846 ± 33 and 825 ± 30 μmol · min−1) or in the control and leucine ingestion studies (788 ± 29 and 809 ± 27 μmol · min−1). Protein ingestion during the HECP decreased the glucose infusion rate required to maintain euglycemia within 1–2 h and decreased the glucose Rd–to–plasma insulin concentration ratio by 17 ± 4% (P < 0.01), whereas leucine ingestion had no effect on it (−1 ± 5% difference from control study; P < 0.05 vs. the protein group) (Figs. 1 and 2 and Supplementary Fig. 1).
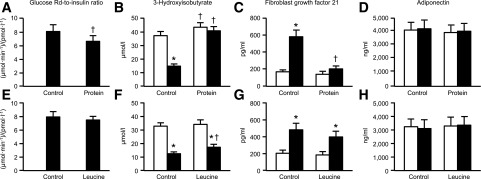
Figure 1.
Insulin-stimulated Rd–to–plasma insulin ratio (A and E) and plasma 3-HIB (B and F), FGF21 (C and G), and adiponectin (D and H) concentrations during basal conditions (white bars) and during the last 20 min of the HECP (black bars), with and without (control) concomitant protein (A–D) or leucine (E–H) ingestion. Data are presented as mean ± SEM. *Significant difference from the corresponding basal value (P < 0.01). †Significant difference from the corresponding control value (P < 0.05).
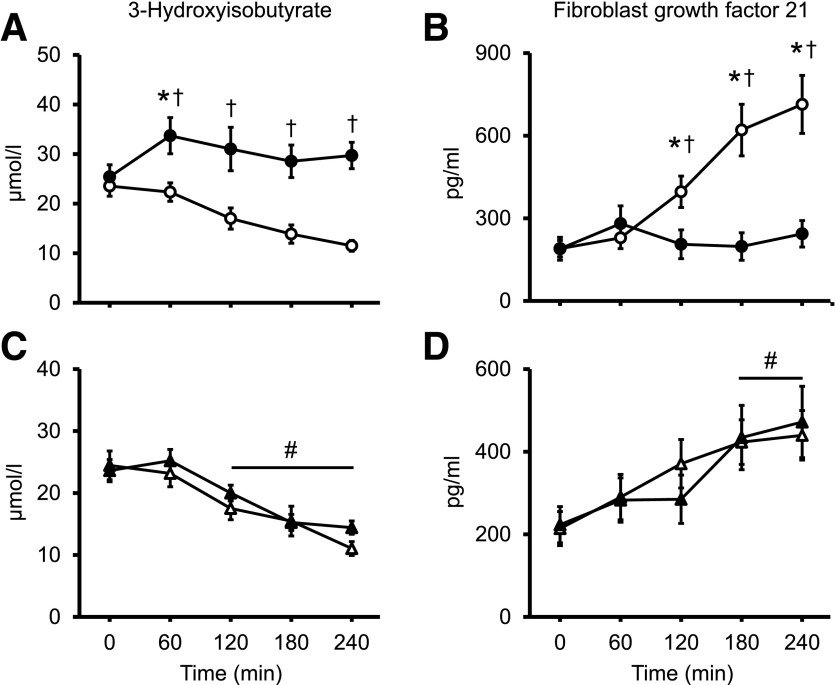
Figure 2.
Plasma 3-HIB (A and C) and FGF21 (B and D) concentrations during basal conditions (time 0) and hourly during the HECP, with (black symbols) and without (white symbols) concomitant protein (A and B) or leucine (C and D) ingestion, in a subset of 10 subjects/group. Data are mean ± SEM. In panels A and B, ANOVA revealed a significant time × drink interaction (P < 0.001); in panels C and D, ANOVA revealed a main effect of time (P < 0.001). *Significant difference from the corresponding basal value (P < 0.01). †Significant difference from the corresponding control value (P < 0.05). #Significant main effect of time.
Plasma 3-HIB concentration gradually decreased to ∼60% of basal values during the HECP without protein or leucine ingestion, and ingestion of protein, but not leucine, prevented the HECP-mediated decrease in plasma 3-HIB concentration. Plasma FGF21 concentration gradually increased to more than double the basal values during the HECP without protein or leucine ingestion, and ingestion of protein, not leucine, prevented the HECP-mediated increase in plasma FGF21 concentration. A small net amount of FGF21 was released from the leg, which was suppressed by ingestion of protein, but not leucine. Plasma adiponectin concentration did not change during the HECP and was not affected by either protein or leucine ingestion (Figs. 1 and 2 and Supplementary Fig. 2).
Muscle PPARGC1A, BCAT2, BCKDHA, and FGF21 Gene Expression
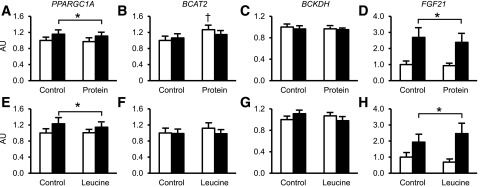
During the HECP, PPARGC1A expression increased by ∼15% and FGF21 expression approximately doubled in all studies; the increases were not different among the control, protein ingestion, and leucine ingestion studies. BCAT2 and BCKDHA gene expression were not affected by the HECP or protein or leucine ingestion (Fig. 3).
Figure 3.
Gene expression in muscle of PPARGC1A (A and E), BCAT2 (B and F), BCKDH (C and G), and FGF21 (D and H) during basal conditions (white bars) and during the HECP (black bars), with and without (control) concomitant protein (A–D) or leucine (E–H) ingestion. Data are mean ± SEM. *Significant difference from the corresponding basal value (P < 0.01). †Significant difference from the corresponding control value (P < 0.05).
Discussion
The adverse effect of systemic hyperaminoacidemia, caused by either intravenous amino acid infusion or protein ingestion, on insulin-mediated glucose disposal is well established (1–3), but the mechanism(s) responsible for it are not known. We found that leucine-mediated inhibition of AKT via mTOR signaling, which occurs in animal and cell culture models (8,9), was not involved in insulin resistance induced by protein ingestion in humans (3). In this study, we evaluated whether the adverse effect of protein ingestion on glucose uptake is related to alterations in valine and FGF21 metabolism. We measured the plasma concentrations of 3-HIB, a valine metabolite that decreases insulin sensitivity in mice when added to drinking water (10), and FGF21, which increases insulin sensitivity directly in isolated skeletal muscles or increases adiponectin secretion by adipose tissue in mice (11–14), during basal conditions and during an HECP with and without concomitant ingestion of protein or an amount of leucine that matched the amount in the protein drink. We found that the increase in glucose and insulin availability during the HECP caused a rapid decrease in plasma 3-HIB and an increase in plasma FGF21 concentrations. Ingestion of protein, but not leucine, prevented the HECP-induced decrease in 3-HIB and increase in FGF21 concentrations and blunted the insulin-mediated increase in glucose disposal. These results suggest that the adverse effect of protein ingestion on insulin-mediated glucose disposal is related to increased valine catabolism, which results in 3-HIB accumulation and its suppressive effect on plasma FGF21 concentration. Increased release of adiponectin by adipose tissue and a PPARGC1A-mediated increase in branched-chain amino acid catabolism genes in muscle, however, were most likely not involved in mediating the relationship between protein ingestion, 3-HIB, FGF21, and insulin resistance, because plasma adiponectin concentration and PPARGC1A, BCAT2, and BCKDH expression in muscle were not affected by protein ingestion.
The decrease in 3-HIB during the HECP without protein ingestion or with only leucine ingestion was likely a result of the antiproteolytic effect of insulin (27), which reduces the release of valine from protein stores. Our results suggest that the antiproteolytic effect of insulin may be necessary to promote insulin-mediated glucose disposal. Protein ingestion prevented the decrease in plasma 3-HIB concentration, most likely by the presence in the circulation of increased valine from the ingested protein, thereby negating the insulin-mediated suppression of 3-HIB production. 3-HIB has been proposed to inhibit insulin action by stimulating fatty acid uptake and lipid accumulation in muscle (10). Our data suggest it is unlikely that 3-HIB–mediated fatty acid uptake in muscle is involved in the pathogenesis of insulin resistance after protein ingestion because insulin infusion is a potent inhibitor of adipose tissue lipolysis and fatty acid release into the blood stream (28), and effectively suppressed plasma NEFA concentration in our subjects during the HECP in all studies. Moreover, lipid-induced insulin resistance typically develops after several hours of increased fatty acid concentrations in plasma and involves impaired AKT signaling (29–32), whereas the impairment in glucose disposal after protein ingestion or intravenous amino acid infusion occurs without changes in muscle AKT signaling (3,33).
Our data suggest that an increase in circulating FGF21 is also involved in insulin-stimulated glucose disposal. The exact mechanism responsible for this metabolic effect is unclear. It has been demonstrated that FGF21 enhances the classic phosphoinositide 3-kinase–AKT insulin signaling pathway in target tissues either directly or through increased secretion of adiponectin by adipose tissue into the systemic circulation (12,34–36). However, the results from studies conducted in isolated rat muscle (13) and the data from our previous study (3) suggest that the increase in plasma FGF21 during insulin infusion potentiates the effect of insulin on glucose disposal through a mechanism that is independent of adiponectin and canonical insulin signaling.
The source of the increased circulating FGF21 during the HECP is uncertain. It has been proposed that the increase in plasma FGF21 during a HECP is due to an increase in muscle FGF21 production, because insulin stimulates FGF21 gene expression and FGF21 release in cultured myocytes (37), and combined insulin and glucose infusion during an HECP has been found to increase FGF21 gene expression in muscle and plasma concentration in young healthy men (38). We also found that the HECP increased muscle FGF21 gene expression and plasma FGF21 concentration but did not increase the net release of FGF21 from the leg. Protein ingestion did not affect FGF21 gene expression in muscle but completely blocked the net release of FGF21 from the leg and prevented an increase in plasma FGF21. These findings suggest that muscle-derived FGF21 is not a major source of circulating FGF21, and the increase in plasma FGF21 concentration during the HECP is a result of the hyperinsulinemia-induced reduction in plasma amino acid concentrations, which is prevented by protein ingestion. This notion is supported by data from studies of mice that found that both deprivation of protein and select amino acids increased hepatic, but not muscle, FGF21 gene expression and plasma FGF21 concentration (16,20–22).
Although our data suggest that a decrease in plasma FGF21 contributes to the adverse effect of protein ingestion on insulin action, basal plasma FGF21 concentrations are actually higher, not lower, in people who are insulin resistant than those who are insulin sensitive (39). This apparent contradiction is likely due to FGF21 resistance (40) and an adaptive increase in plasma FGF21. The mechanism responsible for increased plasma FGF21 concentrations in people with insulin resistance is unclear. It is possible that chronic hyperinsulinemia increases plasma FGF21 by stimulating hepatic FGF21 production, but this seems unlikely. Although, insulin acutely stimulates FGF21 production in hepatocytes (41) and increases plasma FGF21 concentration in humans (as seen in this study and in ref. 38), plasma FGF21 concentration is normal in liver-specific insulin-receptor knockout mice (42).
Our study has some limitations. First, our entire study population comprised postmenopausal women with obesity, so our findings might not extrapolate to premenopausal women, lean women, or men. However, previous studies have shown that acute amino acid infusion or protein ingestion causes insulin resistance in lean and obese men and women, which suggests that our finding are likely relevant in these other cohorts (1–3,43,44). Second, we did not study the effect of valine ingestion alone, which would have provided insights as to whether valine is an important mediator of dietary protein–induced insulin resistance. Our observation that ingestion of protein, but not leucine, increased plasma 3-HIB concentration supports the possibility that valine is involved in the pathogenesis of protein ingestion–induced insulin resistance, which will need to be confirmed by other studies. Third, it is possible that intestinal hormones that were not evaluated in this study, namely, incretin hormones, and glucagon are involved in the pathogenesis of dietary protein–induced insulin resistance. Protein ingestion stimulates the release of incretin hormones (45,46) and glucagon (47,48), which can affect plasma insulin concentration and insulin sensitivity, and increase FGF21 concentration (49,50). In our study, even though plasma insulin concentration was higher during the HECP when protein was ingested than during the corresponding control HECP or the HECP with leucine ingestion, the glucose disposal rate during the HECP was lower when subjects ingested protein than the control or leucine conditions, and protein ingestion suppressed plasma FGF21 concentration. Therefore, it seems unlikely that a difference in intestinal hormone and/or glucagon response to protein ingestion can explain the adverse effect of dietary protein on FGF21 metabolism and insulin sensitivity.
In summary, the results from our study demonstrate that 1) the decrease in plasma 3-HIB concentration and increase in plasma FGF21 concentration induced by insulin and glucose infusion during an HECP is blocked by protein ingestion and 2) the protein-induced increase in circulating 3-HIB and decrease in circulating FGF21 were associated with a marked impairment in insulin-stimulated glucose disposal. These results suggest that alterations in valine and FGF21 metabolism are involved in the pathogenesis of insulin resistance in skeletal muscle induced by protein ingestion in humans.
Supplementary Material
Article Information
Acknowledgments. The authors thank Emily Lake and Janet Winkelmann for help with subject recruitment and scheduling and Kathryn Gratza, Jennifer Shew, and Freida Custodio for technical assistance (all from the Washington University School of Medicine in St. Louis, St. Louis, MO). The authors also thank the staff of the Clinical Research Unit at Washington University School of Medicine in St. Louis for help in performing the studies and the study subjects for participating.
Funding. This publication was made possible by National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases grants DK-094483, DK-101578, and DK-056341 (to the Washington University School of Medicine Nutrition Obesity Research Center) and DK-020579 (to the Washington University School of Medicine Diabetes Research Center); the National Center for Advancing Translational Sciences (grant UL1-TR-000448 [a Washington University School of Medicine Clinical and Translational Science Award], including KL2 subaward TR-000450); and a grant from the Longer Life Foundation.
Duality of Interest. No conflicts of interest relevant to this article were reported.
Author Contributions. L.-A.L.S.H. processed samples, analyzed data, and prepared the manuscript. G.I.S. conducted the studies, processed samples, analyzed data, and edited the manuscript. B.W.P., A.L.O., and J.Y. processed samples, analyzed data, and edited the manuscript. R.S.R. conducted the studies and edited the manuscript. S.C.K. and L.C.P. processed samples and edited the manuscript. S.K. obtained funding for the studies, conducted the studies, and edited the manuscript. B.M. designed the studies, obtained funding for the studies, supervised the performance of the study and sample processing and data analysis, and edited the manuscript. B.M. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical trial reg. nos. NCT01538836 and NCT01757340, clinicaltrials.gov.
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-1475/-/DC1.
L.-A.L.S.H. and G.I.S. contributed equally to this work.
References
- 1.Robinson MM, Soop M, Sohn TS, et al. High insulin combined with essential amino acids stimulates skeletal muscle mitochondrial protein synthesis while decreasing insulin sensitivity in healthy humans. J Clin Endocrinol Metab 2014;99:E2574–E2583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krebs M, Krssak M, Bernroider E, et al. Mechanism of amino acid-induced skeletal muscle insulin resistance in humans. Diabetes 2002;51:599–605 [DOI] [PubMed] [Google Scholar]
- 3.Smith GI, Yoshino J, Stromsdorfer KL, et al. Protein ingestion induces muscle insulin resistance independent of leucine-mediated mTOR activation. Diabetes 2015;64:1555–1563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Nielen M, Feskens EJ, Mensink M, et al.; InterAct Consortium . Dietary protein intake and incidence of type 2 diabetes in Europe: the EPIC-InterAct Case-Cohort Study. Diabetes Care 2014;37:1854–1862 [DOI] [PubMed] [Google Scholar]
- 5.Shang X, Scott D, Hodge AM, et al. Dietary protein intake and risk of type 2 diabetes: results from the Melbourne Collaborative Cohort Study and a meta-analysis of prospective studies. Am J Clin Nutr 2016;104:1352–1365 [DOI] [PubMed] [Google Scholar]
- 6.Sluijs I, Beulens JW, van der A DL, Spijkerman AM, Grobbee DE, van der Schouw YT. Dietary intake of total, animal, and vegetable protein and risk of type 2 diabetes in the European Prospective Investigation into Cancer and Nutrition (EPIC)-NL study. Diabetes Care 2010;33:43–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tinker LF, Sarto GE, Howard BV, et al. Biomarker-calibrated dietary energy and protein intake associations with diabetes risk among postmenopausal women from the Women’s Health Initiative. Am J Clin Nutr 2011;94:1600–1606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tremblay F, Lavigne C, Jacques H, Marette A. Role of dietary proteins and amino acids in the pathogenesis of insulin resistance. Annu Rev Nutr 2007;27:293–310 [DOI] [PubMed] [Google Scholar]
- 9.Lynch CJ, Adams SH. Branched-chain amino acids in metabolic signalling and insulin resistance. Nat Rev Endocrinol 2014;10:723–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jang C, Oh SF, Wada S, et al. A branched-chain amino acid metabolite drives vascular fatty acid transport and causes insulin resistance. Nat Med 2016;22:421–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Markan KR, Naber MC, Ameka MK, et al. Circulating FGF21 is liver derived and enhances glucose uptake during refeeding and overfeeding. Diabetes 2014;63:4057–4063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holland WL, Adams AC, Brozinick JT, et al. An FGF21-adiponectin-ceramide axis controls energy expenditure and insulin action in mice. Cell Metab 2013;17:790–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mashili FL, Austin RL, Deshmukh AS, et al. Direct effects of FGF21 on glucose uptake in human skeletal muscle: implications for type 2 diabetes and obesity. Diabetes Metab Res Rev 2011;27:286–297 [DOI] [PubMed] [Google Scholar]
- 14.Kharitonenkov A, Shiyanova TL, Koester A, et al. FGF-21 as a novel metabolic regulator. J Clin Invest 2005;115:1627–1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Itoh N. FGF21 as a hepatokine, adipokine, and myokine in metabolism and diseases. Front Endocrinol (Lausanne) 2014;5:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laeger T, Henagan TM, Albarado DC, et al. FGF21 is an endocrine signal of protein restriction. J Clin Invest 2014;124:3913–3922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Sousa-Coelho AL, Relat J, Hondares E, et al. FGF21 mediates the lipid metabolism response to amino acid starvation. J Lipid Res 2013;54:1786–1797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wanders D, Stone KP, Dille K, Simon J, Pierse A, Gettys TW. Metabolic responses to dietary leucine restriction involve remodeling of adipose tissue and enhanced hepatic insulin signaling. Biofactors 2015;41:391–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fontana L, Cummings NE, Arriola Apelo SI, et al. Decreased consumption of branched-chain amino acids improves metabolic health. Cell Reports 2016;16:520–530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stone KP, Wanders D, Orgeron M, Cortez CC, Gettys TW. Mechanisms of increased in vivo insulin sensitivity by dietary methionine restriction in mice. Diabetes 2014;63:3721–3733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Solon-Biet SM, Cogger VC, Pulpitel T, et al. Defining the nutritional and metabolic context of FGF21 using the geometric framework. Cell Metab 2016;24:555–565 [DOI] [PubMed] [Google Scholar]
- 22.Fisher FM, Chui PC, Nasser IA, et al. Fibroblast growth factor 21 limits lipotoxicity by promoting hepatic fatty acid activation in mice on methionine and choline-deficient diets. Gastroenterology 2014;147:1073–1083.e6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Estall JL, Ruas JL, Choi CS, et al. PGC-1alpha negatively regulates hepatic FGF21 expression by modulating the heme/Rev-Erb(alpha) axis. Proc Natl Acad Sci U S A 2009;106:22510–22515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cornu M, Oppliger W, Albert V, et al. Hepatic mTORC1 controls locomotor activity, body temperature, and lipid metabolism through FGF21. Proc Natl Acad Sci U S A 2014;111:11592–11599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garcia-Caraballo SC, Comhair TM, Verheyen F, et al. Prevention and reversal of hepatic steatosis with a high-protein diet in mice. Biochim Biophys Acta 2013;1832:685–695 [DOI] [PubMed] [Google Scholar]
- 26.Fabbrini E, Yoshino J, Yoshino M, et al. Metabolically normal obese people are protected from adverse effects following weight gain. J Clin Invest 2015;125:787–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdulla H, Smith K, Atherton PJ, Idris I. Role of insulin in the regulation of human skeletal muscle protein synthesis and breakdown: a systematic review and meta-analysis. Diabetologia 2016;59:44–55 [DOI] [PubMed] [Google Scholar]
- 28.Conte C, Fabbrini E, Kars M, Mittendorfer B, Patterson BW, Klein S. Multiorgan insulin sensitivity in lean and obese subjects. Diabetes Care 2012;35:1316–1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boden G, Chen X. Effects of fat on glucose uptake and utilization in patients with non-insulin-dependent diabetes. J Clin Invest 1995;96:1261–1268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gormsen LC, Jessen N, Gjedsted J, et al. Dose-response effects of free fatty acids on glucose and lipid metabolism during somatostatin blockade of growth hormone and insulin in humans. J Clin Endocrinol Metab 2007;92:1834–1842 [DOI] [PubMed] [Google Scholar]
- 31.Roden M, Price TB, Perseghin G, et al. Mechanism of free fatty acid-induced insulin resistance in humans. J Clin Invest 1996;97:2859–2865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Belfort R, Mandarino L, Kashyap S, et al. Dose-response effect of elevated plasma free fatty acid on insulin signaling. Diabetes 2005;54:1640–1648 [DOI] [PubMed] [Google Scholar]
- 33.Tremblay F, Krebs M, Dombrowski L, et al. Overactivation of S6 kinase 1 as a cause of human insulin resistance during increased amino acid availability. Diabetes 2005;54:2674–2684 [DOI] [PubMed] [Google Scholar]
- 34.Kong LJ, Feng W, Wright M, et al. FGF21 suppresses hepatic glucose production through the activation of atypical protein kinase Cι/λ. Eur J Pharmacol 2013;702:302–308 [DOI] [PubMed] [Google Scholar]
- 35.Wente W, Efanov AM, Brenner M, et al. Fibroblast growth factor-21 improves pancreatic beta-cell function and survival by activation of extracellular signal-regulated kinase 1/2 and Akt signaling pathways. Diabetes 2006;55:2470–2478 [DOI] [PubMed] [Google Scholar]
- 36.Lee MS, Choi SE, Ha ES, et al. Fibroblast growth factor-21 protects human skeletal muscle myotubes from palmitate-induced insulin resistance by inhibiting stress kinase and NF-κB. Metabolism 2012;61:1142–1151 [DOI] [PubMed] [Google Scholar]
- 37.Izumiya Y, Bina HA, Ouchi N, Akasaki Y, Kharitonenkov A, Walsh K. FGF21 is an Akt-regulated myokine. FEBS Lett 2008;582:3805–3810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hojman P, Pedersen M, Nielsen AR, et al. Fibroblast growth factor-21 is induced in human skeletal muscles by hyperinsulinemia. Diabetes 2009;58:2797–2801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chavez AO, Molina-Carrion M, Abdul-Ghani MA, Folli F, Defronzo RA, Tripathy D. Circulating fibroblast growth factor-21 is elevated in impaired glucose tolerance and type 2 diabetes and correlates with muscle and hepatic insulin resistance. Diabetes Care 2009;32:1542–1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fisher FM, Chui PC, Antonellis PJ, et al. Obesity is a fibroblast growth factor 21 (FGF21)-resistant state. Diabetes 2010;59:2781–2789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alonge KM, Meares GP, Hillgartner FB. Glucagon and insulin cooperatively stimulate fibroblast growth factor 21 gene transcription by increasing the expression of activating transcription factor 4. J Biol Chem 2017;292:5239–5252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Emanuelli B, Vienberg SG, Smyth G, et al. Interplay between FGF21 and insulin action in the liver regulates metabolism. J Clin Invest 2014;124:515–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ang M, Müller AS, Wagenlehner F, Pilatz A, Linn T. Combining protein and carbohydrate increases postprandial insulin levels but does not improve glucose response in patients with type 2 diabetes. Metabolism 2012;61:1696–1702 [DOI] [PubMed] [Google Scholar]
- 44.Flakoll PJ, Wentzel LS, Rice DE, Hill JO, Abumrad NN. Short-term regulation of insulin-mediated glucose utilization in four-day fasted human volunteers: role of amino acid availability. Diabetologia 1992;35:357–366 [DOI] [PubMed] [Google Scholar]
- 45.Adams RL, Broughton KS. Insulinotropic effects of whey: mechanisms of action, recent clinical trials, and clinical applications. Ann Nutr Metab 2016;69:56–63 [DOI] [PubMed] [Google Scholar]
- 46.Nair KS, Short KR. Hormonal and signaling role of branched-chain amino acids. J Nutr 2005;135(Suppl.):1547S–1552S [DOI] [PubMed] [Google Scholar]
- 47.Carr RD, Larsen MO, Winzell MS, et al. Incretin and islet hormonal responses to fat and protein ingestion in healthy men. Am J Physiol Endocrinol Metab 2008;295:E779–E784 [DOI] [PubMed] [Google Scholar]
- 48.Westphal SA, Gannon MC, Nuttall FQ. Metabolic response to glucose ingested with various amounts of protein. Am J Clin Nutr 1990;52:267–272 [DOI] [PubMed] [Google Scholar]
- 49.Arafat AM, Kaczmarek P, Skrzypski M, et al. Glucagon increases circulating fibroblast growth factor 21 independently of endogenous insulin levels: a novel mechanism of glucagon-stimulated lipolysis? Diabetologia 2013;56:588–597 [DOI] [PubMed] [Google Scholar]
- 50.Hansen JS, Clemmesen JO, Secher NH, et al. Glucagon-to-insulin ratio is pivotal for splanchnic regulation of FGF-21 in humans. Mol Metab 2015;4:551–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.