Abstract
A male newborn presented with hypospadias and differential testicular volumes. Short femur length was detected four times during pregnancy, at 23, 31, 32 and 33 weeks, by ultrasonographic examination. Chromosome analysis was performed on peripheral lymphocytes obtained from the infant and his parents. Fluorescent in situ hybridization (FISH), using sex determining region Y (SRY)/DXZ1 and DYZ3 probes, was performed to verify the deletion of the SRY gene (located on Yp11.3 region) and the activation of Y chromosomal centromeres. Single nucleotide polymorphism (SNP)-array comparative genomic hybridization (CGH) was used to detect copy number variations in the infant. The results revealed a ~2.2 Mb mircodeletion on Yp11.32 containing the short stature homeobox (SHOX) gene. According to the above examinations, the abnormal Y chromosome of the patient was identified as a dicentric derivate of the Y chromosome with pseudoinactivation of one of the two centromeres. The karyotype is therefore: 45,X[20]/46,X,idic(Y)(p11.3).ish psu idic(Y)(p11.3) (SRY++, DYZ3++). array Yp11.32 (118,551–2,393,500)x0[26]/46,X,ishY(SRY+, DYZ3+)[4]. The combination of cytogenetic, FISH and SNP-array CGH technologies was beneficial for diagnosing the karyotype accurately, predicting the prognosis, and preparing an effective treatment plan for the patient.
Keywords: haploinsufficiency of short stature homeobox, dicentric Y hypospadias, mosaicism, short stature
Introduction
A dicentric Y chromosome has 2 centromeres and is a common abnormal structural rearrangement of the Y chromosome that is unstable during cell division. It is likely to generate various cell lines and most affected patients that have been reported are chromosomal mosaics, typically including the 45,X cell line (1). If there are completely symmetrical arms on the dicentric chromosome, it is considered an isodicentric chromosome. Regardless of the proportion of the two cell lines in peripheral blood, the phenotypic spectrum of chromosomal mosaics of all ages may vary widely and includes healthy infertile males, females with or without Turner syndrome, individuals with ambiguous genitalia and mixed gonadal dysgenesis (2–6). However, there are few reports regarding patients with three different cell lines, particularly the 46,XY normal karyotype.
Hypospadias is a common abnormality of the external genitalia in males, and patients with hypospadias may exhibit chromosomal abnormalities. Kojima et al (7) assessed 400 patients who underwent surgery to repair hypospadias and identified chromosomal anomalies in 22 (6%).
The present case report is of a hypospadiac male infant with a 45,X/46,X,psu idic(Y)(p11.32)/46,XY karyotype. The patient carried a pseudodicentric Y chromosome with the break point located at pseudoautosomal region 1 (PAR1). To the best of our knowledge, this is the first description of a mosaic karyotype containing three cell lines. The proband manifested short stature due to haploinsufficiency of short stature homeobox (SHOX), confirmed through single nucleotide polymorphism (SNP)-array comparative genomic hybridization (CGH) detection. The combination of cytogenetic, fluorescence in situ hybridization (FISH) and SNP-array CGH technologies was beneficial for diagnosing the karyotype accurately, predicting the prognosis and preparing an effective treatment plan.
Case report
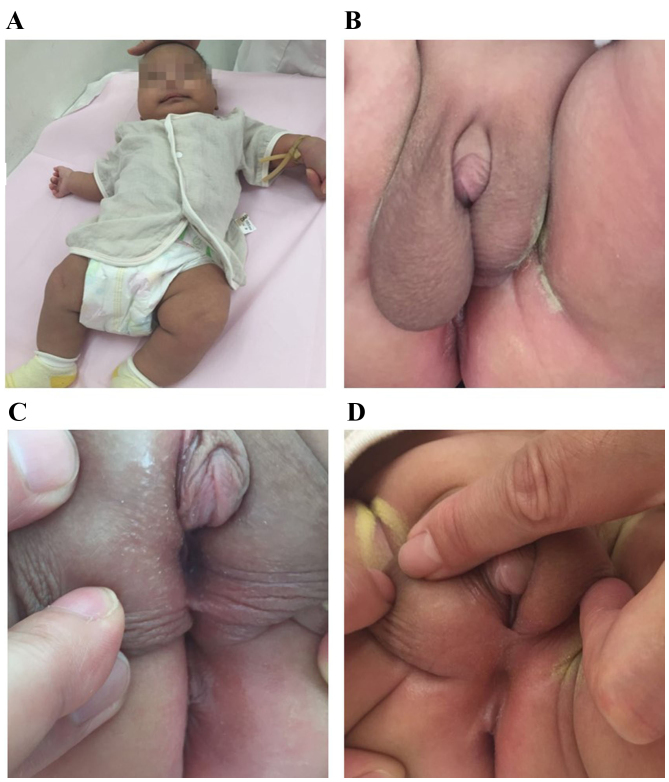
A newborn infant was investigated due to hypospadias and differential testicular volumes (Fig. 1). Written informed consent was obtained from the parents. The parents of the infant had not had contact with hazardous substances and were healthy 28-year-olds. The karyotypes of the parents were normal male (46, XY) and normal female (46, XX). There was no known parental consanguinity and family history was negative for hypospadias and short adult stature. During the pregnancy, there was no evidence of intrauterine growth retardation except for short femur length at 23, 31, 32 and 33 weeks. Due to the low risk of Down's syndrome, karyotype analysis of amniotic cells was not performed. At 6 weeks pregnant, the infant's mother (gravida 1 para 1) had taken progesterone for approximately one month due to low progesterone levels. Due to hypothyroidism at 36 weeks pregnancy, levothyroxine sodium tablets had been taken.
Figure 1.
(A) The male infant. (B) Different sizes of bilateral testes. (C and D) Hypospadias of the patient.
Cesarean delivery occurred at 38 weeks of gestation. The birth weight of the infant was 3,150 g (−0.5 standard deviation; 3,300 g being the average weight of a healthy male Chinese newborn) and a length of 47 cm (−1.5 standard deviation; 49.9 cm being the average length of a healthy male Chinese newborn). The Apgar score was 9/10/10. The infant was examined at a pediatric day-surgery center (Department of Pediatric Surgery, Beijing Children's Hospital, Capital Medical University, Beijing, China) at 29 days. Inguinal ultrasonography revealed no uterus or ovaries. Bilateral testes were both located in the scrotum, with a left testicular size of 0.8×0.4 cm and a right testicular size of 1.2×0.7 cm. There was a liquid dark space of ~2.5×0.8 cm on the testicular sheath membrane cavity. No abnormalities were detected regarding bilateral testicular parenchyma, blood supply and bilateral spermatic cords. An intra-abdominal investigation of laparoscopy was not performed. At 56 days old, the weight of the infant was 6,100 g (0.5 standard deviation; 5,600 g being the average) and length was 56 cm (−1.5 standard deviation; 58.4 cm being the average). Averages provided are according to the World Health Organization standards of child growth.
The serum reproductive hormone levels of the patient were detected at 56 days (Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing, China) by immunoassay, using a UniCel® DxI 800 Immunoassay system (Beckman Coulter, Inc., Brea, CA, USA), and were normal for luteinizing hormone (7.22 IU/l; normal range, 1.24–8.62 IU/l), follicle-stimulating hormone (4.02 IU/l; normal range, 1.27–19.26 IU/l), estradiol (12.37 pg/ml; normal range, <47 pg/ml), progesterone (0.70 ng/ml; normal range, 0.10–0.84 ng/ml) and testosterone (1.13 ng/ml; normal range, 1.75–7.81 ng/ml). However, prolactin levels were elevated (37.49 ng/ml; normal range, 2.64–13.13 ng/ml).
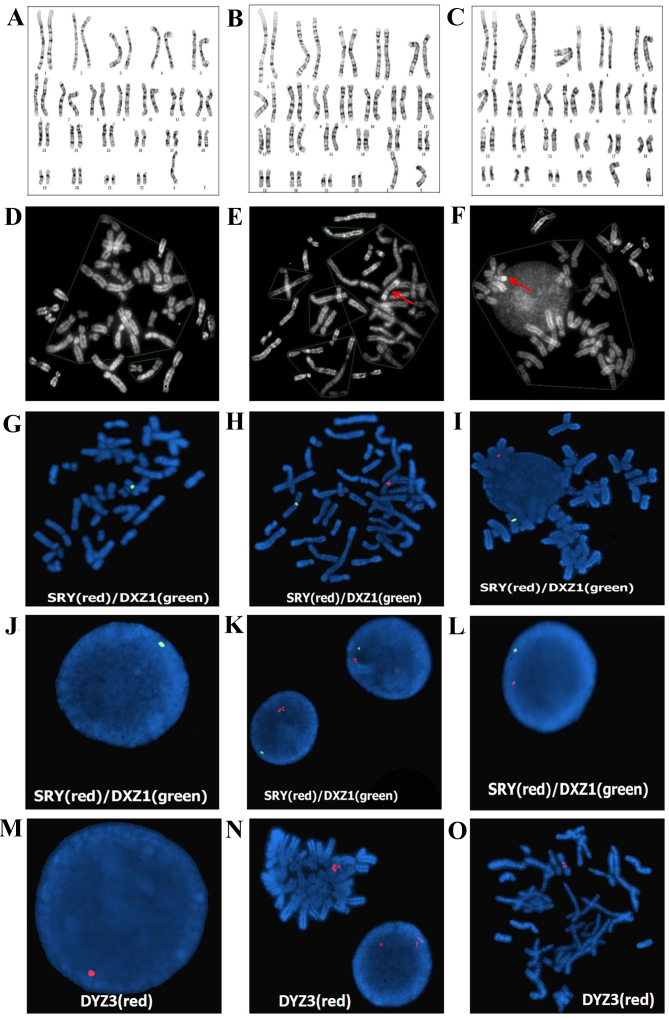
Chromosomal karyotype and FISH analysis
Lymphocytes were obtained at 5 days after birth; 2 ml of peripheral blood was collected, and then 0.5 ml of peripheral blood lymphocytes were cultured in lymphocyte culture medium (Yishengjun; BaiDi Bio-Technology, Guangzhou, China) at 37°C for 72 h, followed by 50 µg/ml colchicine treatment (Yishengjun; BaiDi Bio-Technology) 1 h before culture termination to arrest mitoses. The lymphocytes were hypotonically treated in 0.075 M KCl and fixed in methanol:acetic acid (3:1); then G-banding was performed. Immunoassay was performed to detect the infant's serum reproductive hormone levels. Chromosomal analysis of peripheral lymphocytes revealed the presence of 3 cell lines. In 23 of 50 (46%) analyzed metaphases, a numerically abnormal karyotype was detected: 45,X (Fig. 2A). In 24 of 50 (48%) metaphases, a suspected isodicentric Y chromosome was detected: 46,X,?idic (Y)(p11.3) (Fig. 2B). In 3 of 50 (6%) metaphases, a normal karyotype was detected: 46,XY (Fig. 2C). Additional QFQ-banding techniques revealed that the heterochromatic region of the long arm of the Y chromosome was none, two copies and one copy in the above three cell lines, respectively (Fig. 2D-F). The karyotype was designated as 45,X/46,X,?idic(Y)(p11.3)/46,XY.
Figure 2.
(A-C) Giemsa banding and (D-F) QFQ banding, of (E) Dic(Y) and (F) normal Y. SRY/DXZ1 probe detection in (G-I) metaphase cells and (J-L) interphase cell nuclei. DYZ3 probe detection in (M) interphase nuclei cell (46,XY) and (N and O) metaphase cells [46,X,psu idic (Y)(p11.3)]. SRY, sex determining region Y.
FISH was performed using a sex-determining region Y (SRY)/Vysis CEP X (DXZ1) probe and a Vysis CEP Y (DYZ3) probe on the SRY region of Yq11.3, the centromeric region of the X chromosome and Y chromosome (Vysis; Abbott Molecular, Inc., Des Plaines, IL, USA). The probes were denatured for 2 min at 73°C. The hybridization mixture (1 µl of each probe, 1 µl H2O and 7 µl of hybridization solution) was applied to each slide and covered with a coverslip 20×20 mm. The hybridization mixture was a 70% solution of dextran sulphate and formamide in saline-sodium citrate (SSC) buffer (pH 7). Each slide was then sealed with rubber cement before hybridization was carried out overnight in a moist chamber at 37°C. After hybirdization, the slides were washed for 3 min in a solution of X0.4 SSC at 73°C and a second time for 30 sec in a solution of X2 SSC/0.1% Nonidet P40. Following the final wash, slides were air dried in the dark. The slides were counterstained with a solution of 4′, 6-Diamidine-2′-phenylindole dihydrochloride (DAPI II; Vysis Inc., Downers Grove, IL, USA) diluted in an antifade mounting medium. The SRY/DXZ1 probe was successfully hybridized to metaphase cells (Fig. 2G-I) and interphase cell nuclei (Fig. 2J-L). Fig. 2J-L demonstrates that there was no SRY signal in Fig. 2J, but there were two signals and one signal on the SRY region of Yq11.3 in (Fig. 2K and L, respectively). In addition, there was one signal in the centromeric regions of the X chromosome on metaphase cells (Fig. 2G-I) and one signal in interphase cell nuclei, respectively (Fig. 2J-L). One red signal revealed the active Y centromere on interphase cell nuclei (46,XY; Fig. 2M). Two red signals revealed the inactive Y centromere and one red signal revealed the active Y centromere on a metaphase cell [46,X,psu idic (Y)(p11.3); Fig. 2N-O]. According to these results, the abnormal Y chromosome was identified as a dicentric derivate of the Y chromosome with psuedoinactivation of one of the two centromeres (Fig. 3). The karyotype of the infant was designated as 45,X[20]/46,X,?idic (Y)(p11.3).ish psu idic(Y)(p11.3) (SRY++, DYZ3++)[26]/46, X,.ish Y (SRY+, DYZ3+)[4].
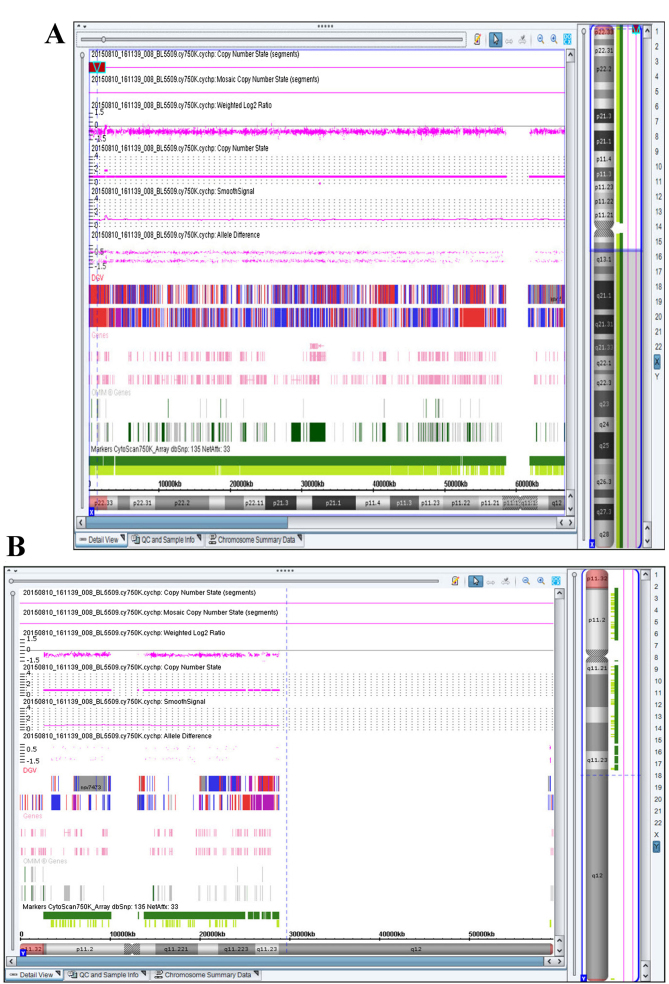
Figure 3.
Diagrams of (A) a normal Y chromosome and (B) a 46,X,psu idic (Y)(p11.32).
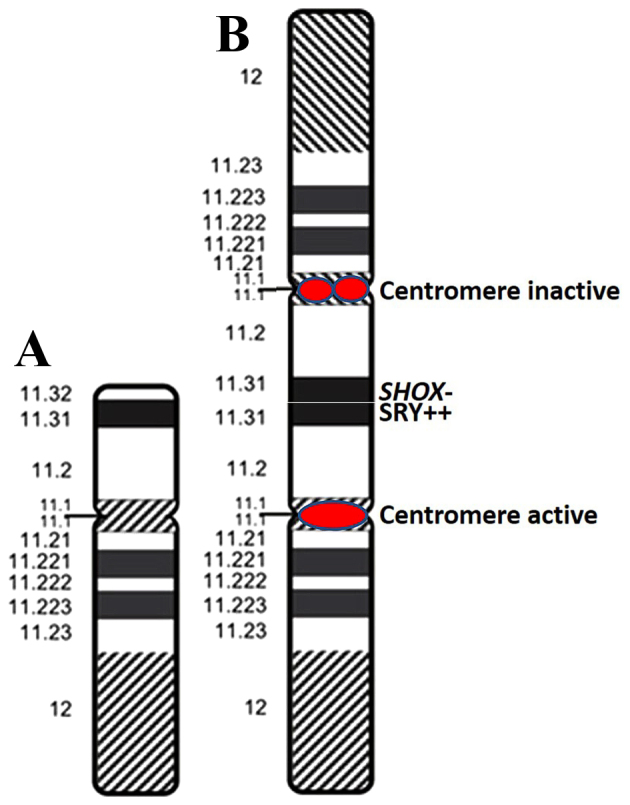
SNP-array CGH analysis
Peripheral blood (1 ml) containing 2.25 mg/ml EDTA was sent to Be Creative Lab Co. Ltd (Beijing, China) for processing and an Affymetrix CytoScan® 750K (Affymetrix, Inc., Santa Clara, CA, USA) gene chip was used to determine the SNPs and copy number variations (CNVs). SNP-array CGH detected a deletion on the pseudoautosomal region of the Y chromosome (Yp11.32) that encompassed ~2.2 Mb (Fig. 4). Thus, the SNP-array CGH results of the patient were arr[hg19] Yp11.32(118,551–2,393,500)x0. When the results of chromosome karyotype analysis, FISH and SNP-array CGH were combined, it was possible to identify the precise breakage of the abnormal Y chromosome on Yp11.32. The results were analyzed using the Online Mendelian Inheritance in Man (OMIM) database (omim.org/), Gene Review (Reviews of genetic disorders/syndromes and lab testing; www.ncbi.nlm.nih.gov/gtr/#genereviews), the International Standards for Cytogenomic Arrays (ISCA) and the Consortium Clinical CNV Database (www.ncbi.nlm.nih.gov/dbvar). Data analysis revealed that the 2.2 Mb deletion encompassed ~20 OMIM genes, including SHOX. No clinically significant microdeletions or microduplications on other chromosomes were observed.
Figure 4.
Single nucleotide polymorphism-array profiles of (A) an X chromosome with one copy of SHOX on Xp22.33 and (B) a Y chromosome with no copy of SHOX on Yp11. SHOX, short stature homeobox.
Discussion
The phenotypic spectrum of 45, X/46, XY, dic(Y) mosaicism is broad and variable. Table I presents previous studies regarding patients with differing sex, age, proportions of cell lines and break points. It has been suggested that the diverse clinical phenotypes are dependent on the proportions of the different cell lines, and the variable sites of breakage and fusion on Y chromosomes.
Table I.
Genotype-phenotype correlations in reported patients with dic(Y) chromosomes.
| Author, year | Peripheral karyotype | Sex | Age, years | Phenotype | Sex Determining Region Y, copies | (Refs.) |
|---|---|---|---|---|---|---|
| Cui et al, 2015 | 46,X,idic(Y) (p11.32) | Male | 32 | Short stature, severe oligozoospermia | 2 | (13) |
| Yoshida et al, 1997 | 45,X[7]/46,X,psu dic(q11.2)[33] | Male | 28 | Azoospermia | (14) | |
| Hes et al, 2009 | 45,X[22]/46,X,psu dic(Y)(pter→q11.21:: p11.31→p11.2::q11.21→pter)[12] | Male | 50 | Mental retardation and hypogonadism | 3 | (17) |
| Batstone et al, 1991 | 45,X/46,X dic (Y) | Male | 14 | Noonan's syndrome | / | (18) |
| Fernandez et al, 2002; Yoshida et al, 1997 | 45,X/46,X,dic(Y)(pter→q11::q11→pter) | Female | 24 | Widely spaced nipples, Pterygium colli, coarctation of aorta, a small uterus, rudimentary gonads, deficient intrauterine growth, low weight at birth, psychomotor and mental delay, lumbar scoliosis, strabismus | 2 different | (3,14) |
| Gole et al, 2008 | 45,X[10]/46,X,idic(Y)(q11.2)[90] | Female | 2.7 | Clitoromegaly, short stature | 2 | (19) |
| Smith et al, 1996 | 45,X[70%]/46,X,dic(q11.2)[30%] | Female | 66 | Clitoromegaly, primary amenorrhea, no breast development, a large right inguinal hernia | / | (6) |
| Shimoda et al, 1998 | 45,X[13]/46,X,dic(q11.2)[17] | Female | 29 | Ambiguous genitalia with clitoromegaly | / | (20) |
| Kaprova-Pleskacova et al, 2013 | 45,X[92.2%]/46,X,psu dic(Y)(p12)[7.8%] | / | Infant | Congenital ambiguous genitalia | 2 | (4) |
| Reddy et al, 1996 | 45,X[92%]/46,X,psu dic(q11.2)[8%] | / | Infant | Mixed gonadal dysgenesis | / | (5) |
| Bittmann et al, 2005 | 45,X(13)/46,X,dic (Y) (del(Y) (q?-qter) | Male | Infant | Right-sided inguinal hernia, ambiguously differentiated gonad | / | (21) |
| The present study | 45,X[23]/46,X,psu dic(Y)(p11.3)[24]/46,XY[3] | Male | Infant | Hypospadias, short stature | 2 | – |
The present study reported a patient with hypospadias and a mosaicism karyotype of 3 cell lines 45,X[23]/46,X,?idic(Y)(p11.32)[24]/46,XY[3]. The dic(Y) chromosome of the male infant was a result of meiosis I exchange between sister chromatids at the pseudoautosomal region, followed by centromere misdivision at meiosis II during spermatogenesis in the father. Another cause probably occurred during the first division following fertilization (8). The most important reason for chromosomal breakage and reunion is exposure to hazardous substances including radiation, medication, chemical and biological factors. Although the parents of the present infant denied contact with the above factors, the presence or absence of hazardous material tends to be unpredictable in daily life.
The SRY gene, located at the tip of the Y short arm (Yp11.3), is a critical switch that results in testis development (9). To confirm whether the break point on the Y chromosome involved SRY and sex differentiation, FISH was performed on metaphase cells and interphase cell nuclei using a SRY/DXZ1 probe. The results revealed that there were two signals on dic(Y), which suggested that the breakage was on Yp11.3. A DYZ3 probe was additionally used to verify the activity of the two Y chromosomal centromeres on dic(Y). The rearranged Y chromosome was of dicentric structure in which only one centromere was active, meaning that the aberrant Y chromosome was stable in mitotic cell division.
SHOX, located in the PAR1 on the tip of the short arms of the X and Y sex chromosomes (Xp22.33 and Yp11.32), is comprised of ~2.6 Mb (10). To evaluate the development of the patient and to confirm the deficiency of SHOX gene on the terminal of the short arm of the Y chromosome, SNP-array CGH was used for genome-wide sequencing and to identify CNVs. Only one copy of SHOX was detected on Xp22.33. However, the copy on Yp11.32 was deletion. This revealed that the break point on dic(Y) chromosome was Yp11.23, and it had lost the pseudoautosomal region. The deficiency of SHOX causes Leri-Weill Syndrome, which is characterized by short stature and abnormal limbs (11). This indicates that the short femur length during pregnancy and short stature following birth in the infant described in the present study were due to the deletion of the short arm end of the Y chromosome and the haploinsufficiency of the SHOX gene. Previous evidence regarding the use of recombinant growth hormone in patients with SHOX deficiency has indicated the beneficial effect of this treatment, which improved growth speed and final height (12).
It is likely that this infant will suffer infertility upon maturation. Multiple previous reports have observed that male patients with 45,X/46,X,dic(Y) exhibit azoospermia or oligozoospermia (2,13–15). The cause of spermatogenic failure may be explained by the presence of an abnormal Y chromosome that may not form a sex vesicle, which appears to be necessary for the completion of the meiosis process and the formation of sperm, or the presence of the 45,X cell line (16).
In conclusion, the present study reports the case of an 8-week-old hypospadiac male infant with 45,X/46,X,psu idic(Y)(p11.32)/46,XY mosaicism and haploinsufficiency of SHOX. Doctors and genetic consultants must pay greater attention to pregnant women with low risk of prenatal screening and ultrasonic structural abnormalities. The combination of cytogenetic, FISH and SNP-array CGH technologies was beneficial for diagnosing the karyotype accurately, predicting the prognosis, and preparing an effective treatment plan for the patient.
Acknowledgements
The authors thank the patient and his family for participating in the present study, and all staff of the Be Creative Lab Co., Ltd. (Beijing, China). The present study was supported by the Basic-Clinical Scientific Research Cooperation Fund, Capital Medical University (grant no. 15JL76) and the Beijing Obstetrics and Gynecology Hospital, Capital Medical University (grant no. fcyy201534).
References
- 1.Hsu LY. Prenatal diagnosis of 45,X/46,XY mosaicism-a review and update. Prenat Diagn. 1989;9:31–48. doi: 10.1002/pd.1970090106. [DOI] [PubMed] [Google Scholar]
- 2.Codina-Pascual M, Oliver-Bonet M, Navarro J, Starke H, Liehr T, Gutierrez-Mateo C, Sánchez-García JF, Arango O, Egozcue J, Benet J. FISH characterization of a dicentric Yq (p11.32) isochromosome in an azoospermic male. Am J Med Genet A. 2004;127A:302–306. doi: 10.1002/ajmg.a.30027. [DOI] [PubMed] [Google Scholar]
- 3.Fernandez R, Marchal JA, Sanchez A, Pasaro E. A point mutation, R59G, within the HMG-SRY box in a female 45,X/46,X, psu dic(Y) (pter->q11::q11->pter) Hum Genet. 2002;111:242–246. doi: 10.1007/s00439-002-0767-6. [DOI] [PubMed] [Google Scholar]
- 4.Kaprova-Pleskacova J, Snajderova M, Stoop J, Koudova M, Kocarek E, Novotna D, Drop SL, Obermannova B, Lebl J, Oosterhuis JW, Looijenga LH. 45,X/46,X,psu dic(Y) gonadal dysgenesis: Influence of the two cell lines on the clinical phenotype, including gonadal histology. Sex Dev. 2013;7:282–288. doi: 10.1159/000356173. [DOI] [PubMed] [Google Scholar]
- 5.Reddy KS, Sulcova V, Ho CK, Conner ED, Khurana A. An infant with a mosaic 45,X/46,X,psu dic(Y) (pter-> q11.2::q11.2->pter) karyotype and mixed gonadal dysgenesis studied for extent of mosaicism in the gonads. Am J Med Genet. 1996;66:441–444. doi: 10.1002/(SICI)1096-8628(19961230)66:4<441::AID-AJMG11>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 6.Smith YR, Stetten G, Charity L, Isacson C, Gearhart JP, Namnoum AB. Ambiguous genitalia in an elderly woman with a mosaic 45,X/46,X,dic(Y)(Q11.2) karyotype. Urology. 1996;47:259–262. doi: 10.1016/S0090-4295(99)80431-2. [DOI] [PubMed] [Google Scholar]
- 7.Kojima Y, Hayashi Y, Yanai Y, Tozawa K, Sasaki S, Kohri K. Molecular analysis of hypospadias in a boy with dicentric Y chromosome. J Urol. 2001;165:1244–1245. doi: 10.1097/00005392-200104000-00060. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez R, Pasaro E. Molecular analysis of an idic(Y)(qter ->p11.32::p11.32->qter) chromosome from a female patient with a complex karyotype. Genet Mol Res. 2006;5:399–406. [PubMed] [Google Scholar]
- 9.Sinclair AH, Berta P, Palmer MS, Hawkins JR, Griffiths BL, Smith MJ, Foster JW, Frischauf AM, Lovell-Badge R, Goodfellow PN. A gene from the human sex-determining region encodes a protein with homology to a conserved DNA-binding motif. Nature. 1990;346:240–244. doi: 10.1038/346240a0. [DOI] [PubMed] [Google Scholar]
- 10.Binder G. Short stature due to SHOX deficiency: Genotype, phenotype, and therapy. Horm Res Paediatr. 2011;75:81–89. doi: 10.1159/000324105. [DOI] [PubMed] [Google Scholar]
- 11.Shears DJ, Vassal HJ, Goodman FR, Palmer RW, Reardon W, Superti-Furga A, Scambler PJ, Winter RM. Mutation and deletion of the pseudoautosomal gene SHOX cause Leri-Weill dyschondrosteosis. Nat Genet. 1998;19:70–73. doi: 10.1038/ng0198-70. [DOI] [PubMed] [Google Scholar]
- 12.Blum WF, Ross JL, Zimmermann AG, Quigley CA, Child CJ, Kalifa G, Deal C, Drop SL, Rappold G, Cutler GB., Jr GH treatment to final height produces similar height gains in patients with SHOX deficiency and Turner syndrome: Results of a multicenter trial. J Clin Endocrinol Metab. 2013;98:E1383–E1392. doi: 10.1210/jc.2013-1222. [DOI] [PubMed] [Google Scholar]
- 13.Cui YX, Wang WP, Li TF, Li WW, Wu QY, Li N, Zhang C, Yao Q, Hu YA, Xia XY. Clinical and cytogenomic studies in a case of infertility associated with a nonmosaic dicentric Y chromosome. Andrologia. 2015;47:477–481. doi: 10.1111/and.12278. [DOI] [PubMed] [Google Scholar]
- 14.Yoshida A, Nakahori Y, Kuroki Y, Motoyama M, Araki Y, Miura K, Shirai M. Dicentric Y chromosome in an azoospermic male. Mol Hum Reprod. 1997;3:709–712. doi: 10.1093/molehr/3.8.709. [DOI] [PubMed] [Google Scholar]
- 15.Sasagawa I, Ishigooka M, Kato T, Hayami S, Hashimoto T, Nakada T. Dicentric Y chromosome without evidence of mosaicism in an azoospermic male. Scand J Urol Nephrol. 1996;30:75–76. doi: 10.3109/00365599609182354. [DOI] [PubMed] [Google Scholar]
- 16.Hamerton JL, Canning N, Ray M, Smith S. A cytogenetic survey of 14,069 newborn infants. I. Incidence of chromosome abnormalities. Clin Genet. 1975;8:223–243. doi: 10.1111/j.1399-0004.1975.tb01498.x. [DOI] [PubMed] [Google Scholar]
- 17.Hes FJ, Madan K, Rombout-Liem IS, Szuhai K, Sørensen H, van Amstel HK, Bakker E, Visser TJ, Smit JW, Hansson K. Multiple genomic aberrations in a patient with mental retardation and hypogonadism: 45,X/46,X,psu dic(Y) karyotype, thyroid hormone receptor beta (THRB) mutation and heterozygosity for Wilson disease. Am J Med Genet A. 2009;149A:2231–2235. doi: 10.1002/ajmg.a.33004. [DOI] [PubMed] [Google Scholar]
- 18.Batstone PJ, Faed MJ, Jung RT, Gosden J. 45,X/46,X dic (Y) mosaicism in a phenotypic male. Arch Dis Child. 1991;66:252–253. doi: 10.1136/adc.66.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gole LA, Lim J, Crolla JA, Loke KY. Gonadal mosaicism 45,X/46,X,psu dic(Y)(q11.2) resulting in a turner phenotype with mixed gonadal dysgenesis. Singapore Med J. 2008;49:349–351. [PubMed] [Google Scholar]
- 20.Shimoda N, Sato K, Satoh S, Ogawa O, Ito S, Kato T. Atypical true hermaphroditism with a mosaic 45,X/46,X,dic(Y)(q11.2) karyotype. J Urol. 1998;160:1434–1435. doi: 10.1097/00005392-199810000-00067. [DOI] [PubMed] [Google Scholar]
- 21.Bittmann S, Wieczorek D, Stallmach T, Ulus H. 45,X/46,X,dic(Y)-Mosaicism in the newborn. Klin Padiatr. 2005;217:300–303. doi: 10.1055/s-2004-832335. [DOI] [PubMed] [Google Scholar]