Abstract
IMPORTANCE
Fatal self-injury in the United States associated with deliberate behaviors is seriously underestimated owing to misclassification of poisoning suicides and mischaracterization of most drug poisoning deaths as “accidents” on death certificates.
OBJECTIVE
To compare national trends and patterns of self-injury mortality (SIM) with mortality from 3 proximally ranked top 10 causes of death: diabetes, influenza and pneumonia, and kidney disease.
DATA, SETTING, AND PARTICIPANTS
Underlying cause-of-death data from 1999 to 2014 were extracted for this observational study from death certificate data in the US Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research online databases. Linear time trends were compared by negative binomial regression with a log link function. Self-injury mortality was defined as a composite of suicides by any method and estimated deaths from drug self-intoxication whose manner was an “accident” or was undetermined.
MAIN OUTCOMES AND MEASURES
Mortality rates and ratios, cumulative mortality in individuals younger than 55 years, and years of life lost in 2014.
RESULTS
There were an estimated 40 289 self-injury deaths in 1999 and 76 227 in 2014. Females comprised 8923 (22.1%) of the deaths in 1999 and 21 950 (28.8%) of the 76 227 deaths in 2014. The estimated crude rate for SIM increased 65%between 1999 and 2014, from 14.4 to 23.9 deaths per 100 000 persons (rate ratio, 1.03; 95%CI, 1.03–1.04; P < .001). The SIM rate continuously exceeded the kidney disease mortality rate and surpassed the influenza and pneumonia mortality rate by 2006. By 2014, the SIM rate converged with the diabetes mortality rate. Additionally, the SIM rate was 1.8-fold higher than the suicide rate in 2014 vs 1.4-fold higher in 1999. The male-to-female ratio for SIM decreased from 3.7 in 1999 to 2.6 in 2014 (male by year: rate ratio, 0.98; 95%CI, 0.97–0.98; P < .001). By 2014, SIM accounted for 32.2 and 36.6 years of life lost for male and female decedents, respectively, compared with 15.8 and 17.3 years from diabetes, 15.0 and 16.6 years from influenza and pneumonia, and 14.5 and 16.2 years from kidney disease.
CONCLUSIONS AND RELEVANCE
The burgeoning SIM rate has converged with the mortality rate for diabetes, but there is a 6-fold differential in the proportion of SIM vs diabetes deaths involving people younger than 55 years and SIM is increasingly affecting women relative to men. Accurately characterizing, measuring, and monitoring this major clinical and public health challenge will be essential for developing a comprehensive etiologic understanding and evaluating preventive and therapeutic interventions
Substance use disorders are an omnipresent risk factor for suicide, with a meta-analysis1 attesting to a very strong association (odds ratio, 5.24; 95% CI, 3.30–8.31). Nonetheless, most pharmaceutical opioid and other drug intoxication deaths are reported as “accident”2 on the death certificate under the constraints of the prevailing medicolegal paradigm, which requires compelling evidence of intent to confirm suicide. “Accident” is an official manner-of-death classification used by medical examiners and coroners, although the US Centers for Disease Control and Prevention prefers the term “unintentional” to “accident” from a public health prevention perspective. Moreover, a history of repeated, deliberate drug use and associated life-threatening overdoses, indicative of intentional behaviors that fundamentally alter the probability of a fatal outcome, does not suffice to eliminate the use of “accident” by medical examiners and coroners, whose standard procedures typically depend on definitive evidence of intent on the day of death to establish suicide as the manner of death.
However, from the public health perspective of reducing injuries and preventing adverse fatal outcomes,3 factors leading to altered probabilities frequently arise long before fatal events, and suicides and lethal overdoses often share many antecedent characteristics in terms of emotional, behavioral, familial, and social disruptions. This contrasts with purely psychological or medicolegal perspectives, which have sought to distinguish the individual intent of a final suicidal act from the inferred, inadvertent nature of a lethal drug overdose. Suicidal motivations also elude investigators in many instances, in part reflecting forensic deficits4 emanating from poorly financed emergency health care5,6 and death investigation systems.7 Thus, the label of “accident” has served as the default determination when definitive proximal evidence remains uncertain.8
A consensus panel, whose participants included psychiatrists, medical examiners, toxicologists, epidemiologists, and emergency physicians, conceived of death from drug self intoxication (DDSI) as a working category that would cut across 3 manners of death—suicide, “accident,” and undetermined intent.8 Not contingent on modifying extant manner-of death categories, operationalization of DDSI would circumvent data formulation and acquisition problems for researchers and preventionists, which are inherent in the sometimes competing functions of the medicolegal and epidemiologic paradigms.
Mindful of public health priorities and allocation of associated resources, we adopted a burden of disease and injury approach to examine the need and usefulness of an expanded self-injury mortality (SIM) category.9,10 We operationalized SIM as a combination of known suicides by any method and estimated DDSIs that have been classified by medical examiners and coroners as “accident” or undetermined. By contextualizing SIM, we can compare its overall and sex-specific trends from 1999 to 2014 with trends of 3 proximally ranked top 10 causes of death, namely, diabetes, influenza and pneumonia, and kidney disease. We also examined the effect of the 4 conditions across age as well as sex and hypothesized that SIM would emerge as an outlier as a cause of premature mortality.11–13
Key Points.
Question
What are the differences in the patterns of US self-injury mortality compared with 3 proximally ranked top 10 causes of death?
Findings
In this study, the crude mortality rate of self-injury mortality increased rapidly from 1999 to 2014, ultimately converging with the diabetes rate and surpassing the influenza and pneumonia and kidney disease rates, and the proportion of women dying of self-injury mortality increased dramatically. Additionally, more than 70% of self-injury decedents were younger than 55 years vs less than 12%of counterparts dying of diabetes, influenza and pneumonia, or kidney disease.
Meaning
Accurate characterization, measurement, and monitoring of self-injury mortality will be essential for etiologic understanding and for evaluating preventive and therapeutic interventions.
Methods
Data Source and Cause Selection
Underlying cause-of-death data for this observational study were extracted from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research online databases. 14 Deaths, from medical certificates, had been precoded according to International Statistical Classification of Diseases and Related Health Problems, Tenth Revision15 coding. Selected causes were suicide (UO3, X60-X84, and Y87.0), diabetes (E10-E14), influenza and pneumonia, (J09-J18), kidney disease (N00-07, N17-19, and N25-27), and drug intoxication deaths that had first been coded by intent or manner as “accident” (X40-X44) or undetermined (Y10-14) and then, by corresponding drug groups, as nonopioid analgesics (X40, X60, and Y10), sedative hypnotics (X41, X61, and Y11), narcotics (X42, X62, and Y12), other autonomic nervous system drugs not stated (X43, X63, and Y13), and other unspecified drugs (X44, X64, and Y14).15 Self-injury mortality was estimated as a combination of suicides by any method and “accidents” or undetermined DDSIs, assuming that 80% of “accidental” drug intoxication deaths and 90% of undetermined drug intoxication deaths for decedents 15 years and older were DDSIs.10 Disease selection was based on national ranking proximal to suicide and our expanded self-injury category among the top10 causes of death in 2013. The observation period was1999 to2014. This study received a waiver from the West Virginia University Institutional Review Board because it used open and de-identified secondary mortality data.
Statistical Analysis and Measures
We first plotted the crude cause-specific death rates by sex across time and then used negative binomial regression with a log link function to compare linear trends. Time was modeled as a continuous variable. Female sex served as the referent when sex was included in the models. As appropriate, an interaction term between time and sex was incorporated. Negative binomial dispersion parameters are presented and were estimated by maximum likelihood. For model fit, Pearson χ2 P values (desired P > .05) and Akaike information criterion (smaller is better) are also presented, along with the maximum likelihood parameter estimates and rate ratios (RRs) for significant parameters (P < .05). Statistical analyses were performed using SAS version 9.4 (SAS Institute). Sensitivity analyses were conducted for the individual components of SIM(DDSI and suicide) to estimate model fit relative to SIM.
Age- and sex-specific death rates were computed for the periods of 1999 to 2001 and 2012 to 2014 to compare patterns and change across the selected causes. The rates were annualized for stabilization. We used 3 complementary measures to examine demographic variation in premature mortality by cause. The first was cumulative mortality, with the age of 55 years serving as a cutoff for separating younger and older middle-aged adults. The second measure was the respective mortality RR of self-injury to each of the comparative diseases. Finally, we computed years of life lost by cause in 2014 using a double decrement life table procedure.16,17
Results
Cause-Specific Mortality Trends
All models for the selected causes presented a good fit for our statistical analysis of time trends (Table 1). Specifically, self injury time (year) fit the model well (RR = 1.03). There were an estimated 40 289 self-injury decedents in 1999 and 76 227 in 2014 (data not shown).
Table 1.
Model Fit Parameter Estimates for Crude and Sex-Adjusted Negative Binomial Models of Cause-Specific Mortality Trends in the United States From 1999 to 2014
| Statistic | Self-Injury | Suicidea | Diabetes | Influenza and Pneumonia | Kidney Disease |
|---|---|---|---|---|---|
| Unadjusted model fit | |||||
| P valueb | .31 | .32 | .32 | .31 | .32 |
| AICc | 279.33 | 254.35 | 298.60 | 308.77 | 295.66 |
| Parameter estimates | |||||
| Year | 0.03 | 0.02 | −0.01 | −0.03 | 0.01 |
| SE | 0.001 | 0.001 | 0.002 | 0.003 | 0.003 |
| Wald 95% CI | 0.03 to 0.04 | 0.02 to 0.02 | −0.01 to −0.00 | −0.03 to −0.02 | 0 to 0.01 |
| P value | <.001 | <.001 | .002 | <.001 | <.001 |
| Rate ratio | 1.03 | 1.02 | 0.99 | 0.98 | 1.01 |
| Dispersion | 0.001 | 0 | 0.001 | 0.003 | 0.002 |
| Sex-adjusted model fit | |||||
| P value | .26 | .30 | .29 | .27 | .28 |
| AICc | 532.54 | 455.15 | 551.27 | 570.95 | 545.35 |
| Parameter estimates | |||||
| Year | 0.05 | 0.03 | −0.02 | −0.03 | 0.01 |
| SE | 0.002 | 0.001 | 0.002 | 0.003 | 0.003 |
| Wald 95% CI | 0.05 to 0.06 | 0.02 to 0.03 | −0.02 to −0.01 | −0.04 to −0.02 | 0.00 to 0.01 |
| P value | <.001 | <.001 | <.001 | <.001 | .02 |
| Rate ratio | 1.05 | 1.03 | 0.98 | 0.97 | 1.01 |
| Sex (male) | 50.42 | 25.45 | −43.12 | −23.96 | −13.17 |
| SE | 5.31 | 2.80 | 4.85 | 8.20 | 7.39 |
| Wald 95% CI | 40.02 to 60.82 | 19.96 to 30.95 | −52.63 to −33.61 | −40.02 to −7.90 | 27.65 to 1.32 |
| P value | <.001 | <.001 | <.001 | .003 | .07 |
| Rate ratio | 0 | 0 | 0 | 0 | 0 |
| Year × sex (male) | −0.03 | −0.01 | 0.02 | 0.01 | 0.01 |
| SE | 0.003 | 0.001 | 0.002 | 0.004 | 0.004 |
| Wald 95% CI | −0.03 to −0.02 | −0.02 to −0.01 | 0.02 to 0.03 | 0.01 to 0.02 | 0 to 0.01 |
| P value | <.001 | <.001 | <.001 | .004 | .07 |
| Rate ratio | 0.98 | 0.99 | 1.02 | 1.01 | 1.01 |
| Dispersion | 0.001 | 0 | 0.001 | 0.003 | 0.002 |
Abbreviation: AIC, Akaike information criterion.
Suicide is a component of self-injury, together with estimated deaths from drug self-intoxication. See results of the sensitivity analysis.
P values calculated with Pearson χ2 test.
The Akaike information criterion estimates the relative quality of statistical models for a given set of data. Lower values indicate better quality.
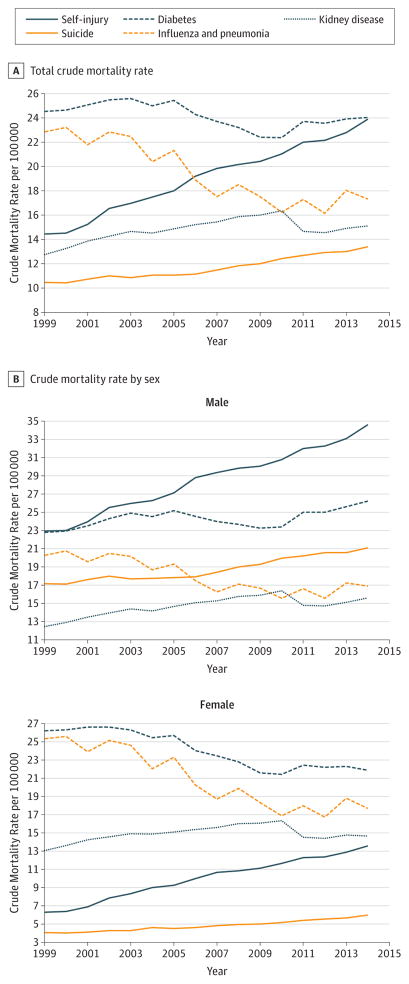
The crude rate for SIM rose from 14.4 per 100 000 persons in 1999 (estimated 40 289 deaths) to 23.9 in 2014 (estimated 76 227 deaths), which was a 65% increase (Figure 1A). This rate exceeded the kidney disease mortality rate throughout the observation period, surpassed the influenza and pneumonia rate by 2006, and converged with the diabetes rate in 2014 (23.9 vs 24.0 deaths per 100000). The crude mortality rate for influenza and pneumonia declined from 23.2 per 100 000 in 2000 to 17.3 in 2014, and the kidney disease mortality rate increased from 12.7 per 100000 to 15.1 per 100 000 by 2014. In 2014, the SIM rate was 1.8-fold higher than the suicide rate whereas it was 1.4-fold higher in 1999.
Figure 1.
Crude Mortality Rates for Self-injury and Other Selected Leading Causes by Sex in the United States From 1999 to 2014
The sensitivity analysis demonstrated similarities in model fit between SIM and its individual components of DDSI and suicide. Notably, the year parameter estimate for SIM (estimate, 0.033; 95% CI, 0.031–0.036) showed increases over time between the suicide parameter (estimate, 0.017; 95%CI, 0.015–0.019) and DDSI parameter (estimate, 0.063; 95% CI, 0.053–0.073).
With sex incorporated in the model, the model fit remained satisfactory (all P > .25) and year trends statistically significant (all P < .02). For self-injury, both sex (male estimate, 50.42; P < .001) and the interaction between sex and year (year × male estimate, −0.025; P < .001) were significant. Sex and the respective interaction term were also significant for diabetes (both P < .001) and influenza and pneumonia (main effect, P = .004; interaction, P = .004) but not for kidney disease.
Males exhibited far higher crude SIM rates than females between 1999 and 2014 (Figure 1B). However, the female rate over the period increased by 116%, while the male rate increased by 51%. Whereas the male/female RR was 3.7 in 1999, it contracted to 2.6 by 2014. Rate ratios of SIM to suicide for males and females were 1.6 and 2.3, respectively, in 2014 vs 1.3 and 1.5 in 1999. Large sex differences manifested between the SIM rate and the rates for the 3 comparison diseases. With the SIM mortality rate equivalent to the diabetes rate at the turn of the century, the self-injury rate for males thereafter diverged upwards from comparison rates. The SIM rate for females remained below comparison rates over the entire observation period but trended toward convergence after 2000.
Demographic Mortality Patterns, Change, and Lost Years
In the period from 1999 to 2001, 77.1%of self-injury deaths occurred among those younger than 55 years compared with 11.1% of diabetes deaths, 6.0%of influenza and pneumonia deaths, and 7.8%of kidney disease deaths (Table 2). Similar variation by cause was evident from 2012 to 2014. The large gaps in cumulative mortality in those younger than 55 years between self-injury and comparison diseases were mirrored by each sex (Table 3). Excepting those 75 years and older, the SIM rate was higher in all specified age groups in 2012 to 2014 than in 1999 to 2001. The RRs of SIM to the corresponding disease rates generally far exceeded unity in those aged 15 to 24 years through those aged 45 to 54 years and were also higher in the 2012 to 2014 than the 1999 to 2001 period. At ages 25 to 34 years, for example, SIM rates for males in the first period were 17-fold higher than the diabetes mortality rate and 25-fold higher in the second period. For females, corresponding differentials were 6-fold and 12-fold between the first and second periods. Self-injury mortality accounted for an estimated 32.2 and 36.6 years of life lost by male and female decedents, respectively, compared with 15.8 and 17.3 years from diabetes, 15.0 and 16.6 years from influenza and pneumonia, and 14.5 and 16.2 years from kidney disease (data not tabulated).
Table 2.
Mortality Patterns and Change for Self-injury and Other Selected Leading Causes by Age in the United States From 1999 to 2014
| Age, y | SI | D | I/P | KD | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||||||
| No. of Deaths | Suicide, % | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | SI:D Rate Ratio | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | SI:I/P Rate Ratio | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | SI:KD Rate Ratio | |
| 1999–2001 | |||||||||||||||||
|
| |||||||||||||||||
| ≤14 | 829 | 100 | 0.7 | 0.5 | NA | 0.1 | 0.1 | NA | 6.6 | 0.8 | 0.8 | NA | 0.5 | 0.5 | 0.3 | NA | 1.4 |
|
| |||||||||||||||||
| 15–24 | 14924 | 79.5 | 12.6 | 12.6 | NA | 0.3 | 0.4 | NA | 31.9 | 1.1 | 0.5 | NA | 27.2 | 0.7 | 0.2 | NA | 59.2 |
|
| |||||||||||||||||
| 25–34 | 21 805 | 68.6 | 30.1 | 18.2 | NA | 1.1 | 1.5 | NA | 12.1 | 1.6 | 0.9 | NA | 20.9 | 1.4 | 0.6 | NA | 30.2 |
|
| |||||||||||||||||
| 35–44 | 33 255 | 59.1 | 56.8 | 24.6 | NA | 3.9 | 4.3 | NA | 5.7 | 3.3 | 2.3 | NA | 10.7 | 3.4 | 1.6 | NA | 15.0 |
|
| |||||||||||||||||
| 45–54 | 25 255 | 65.2 | 77.1 | 22.2 | NA | 11.1 | 13.2 | NA | 1.7 | 6.0 | 4.6 | NA | 4.8 | 7.8 | 4.4 | NA | 5.1 |
|
| |||||||||||||||||
| 55–64 | 10 900 | 84.0 | 85.8 | 14.9 | NA | 24.4 | 38.1 | NA | 0.4 | 10.3 | 11.2 | NA | 1.3 | 16.0 | 12.6 | NA | 1.2 |
|
| |||||||||||||||||
| 65–74 | 7796 | 92.3 | 92.1 | 14.1 | NA | 48.5 | 91.2 | NA | 0.1 | 21.2 | 37.5 | NA | 0.4 | 34.9 | 38.4 | NA | 0.4 |
|
| |||||||||||||||||
| ≥75 | 9801 | 91.8 | 100 | 19.6 | NA | 100 | 215.8 | NA | 0.1 | 100 | 302.0 | NA | 0.1 | 100 | 146.5 | NA | 0.1 |
|
| |||||||||||||||||
| All | 124 605 | 71.6 | NA | 14.7 | NA | NA | 24.7 | NA | 0.6 | NA | 22.6 | NA | 0.6 | NA | 13.3 | NA | 1.1 |
|
| |||||||||||||||||
| 2012–2014 | |||||||||||||||||
|
| |||||||||||||||||
| ≤14 | 1133 | 100 | 0.5 | 0.6 | 36.7 | 0.1 | 0.1 | −14.9 | 10.5 | 0.7 | 0.6 | −26.4 | 1.0 | 0.2 | 0.2 | −46.0 | 3.6 |
|
| |||||||||||||||||
| 15–24 | 22 944 | 64.6 | 11.0 | 17.4 | 37.6 | 0.3 | 0.4 | 9.0 | 40.2 | 1.0 | 0.4 | −11.4 | 42.2 | 0.4 | 0.1 | −28.6 | 114.1 |
|
| |||||||||||||||||
| 25–34 | 39 731 | 48.2 | 29.3 | 30.8 | 69.3 | 1.2 | 1.6 | 5.2 | 19.5 | 1.9 | 1.1 | 20.7 | 29.3 | 0.9 | 0.6 | −5.4 | 54.1 |
|
| |||||||||||||||||
| 35–44 | 40 460 | 49.5 | 47.8 | 33.3 | 35.5 | 3.7 | 4.8 | 11.2 | 6.9 | 3.5 | 2.2 | −3.8 | 15.0 | 2.3 | 1.6 | −2.0 | 20.8 |
|
| |||||||||||||||||
| 45–54 | 51 757 | 50.7 | 71.6 | 39.4 | 77.1 | 11.6 | 13.5 | 1.8 | 2.9 | 7.7 | 5.2 | 11.3 | 7.6 | 6.6 | 4.6 | 6.8 | 8.5 |
|
| |||||||||||||||||
| 55–64 | 36 436 | 59.3 | 88.3 | 30.9 | 107.3 | 28.8 | 33.0 | −13.3 | 0.9 | 16.3 | 11.9 | −6.5 | 2.6 | 17.1 | 12.5 | −0.9 | 2.5 |
|
| |||||||||||||||||
| 65–74 | 14 025 | 80.4 | 94.8 | 18.5 | 31.3 | 51.9 | 69.0 | −24.3 | 0.3 | 29.6 | 28.5 | −23.9 | 0.6 | 35.3 | 33.8 | −11.8 | 0.5 |
|
| |||||||||||||||||
| ≥75 | 11 433 | 90.0 | 100 | 19.5 | −0.5 | 100 | 185.7 | −14.0 | 0.1 | 100 | 196.0 | −35.1 | 0.1 | 100 | 155.9 | 6.4 | 0.1 |
|
| |||||||||||||||||
| All | 217 933 | 57.1 | NA | 23.1 | 57.0 | NA | 23.8 | −3.7 | 1.0 | NA | 17.2 | −24.1 | 1.3 | NA | 14.8 | 11.8 | 1.6 |
Abbreviations: D, diabetes; I/P, influenza/pneumonia; KD, kidney disease; NA, not applicable; SI, self-injury.
Table 3.
Mortality Patterns and Change for Self-injury and Other Selected Leading Causes by Age and Sex in the United States From 1999 to 2014
| Age, y | SI | D | I/P | KD | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||||||
| No. of Deaths | Suicide, % | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | SI:D Rate Ratio | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | SI:I/P Rate Ratio | Cumulative Deaths, % | Rate per 100 000 | Period Change, % | SI: KD Rate Ratio | |
| Males, 1999–2001 | |||||||||||||||||
|
| |||||||||||||||||
| ≤14 | 651 | 100 | 0.7 | 0.7 | NA | 0.1 | 0.1 | NA | 10.0 | 1.0 | 0.9 | NA | 0.8 | 0.6 | 0.4 | NA | 1.9 |
|
| |||||||||||||||||
| 15–24 | 12 534 | 21.1 | 13.6 | 20.7 | NA | 0.3 | 0.4 | NA | 48.4 | 1.3 | 0.5 | NA | 42.1 | 0.9 | 0.2 | NA | 103.6 |
|
| |||||||||||||||||
| 25–34 | 17 419 | 70.8 | 31.7 | 28.9 | NA | 1.4 | 1.7 | NA | 16.8 | 2.1 | 1.0 | NA | 29.4 | 1.5 | 0.6 | NA | 47.6 |
|
| |||||||||||||||||
| 35–44 | 24 883 | 61.5 | 57.4 | 37.0 | NA | 5.1 | 5.2 | NA | 7.2 | 4.2 | 2.6 | NA | 14.0 | 3.8 | 1.9 | NA | 20.0 |
|
| |||||||||||||||||
| 45–54 | 18 726 | 36.8 | 76.8 | 33.6 | NA | 14.2 | 15.7 | NA | 2.1 | 8.0 | 5.8 | NA | 5.8 | 9.2 | 5.2 | NA | 6.5 |
|
| |||||||||||||||||
| 55–64 | 8132 | 77.1 | 85.2 | 23.2 | NA | 30.0 | 42.8 | NA | 0.5 | 13.7 | 13.5 | NA | 1.7 | 18.3 | 13.9 | NA | 1.7 |
|
| |||||||||||||||||
| 65–74 | 6297 | 95.0 | 91.7 | 25.2 | NA | 56.1 | 100 | NA | 0.2 | 27.6 | 46.7 | NA | 0.5 | 38.6 | 43.7 | NA | 0.6 |
|
| |||||||||||||||||
| ≥75 | 7978 | 96.3 | 100 | 43.4 | NA | 100 | 228.6 | NA | 0.2 | 100 | 329.9 | NA | 0.1 | 100 | 179.2 | NA | 0.2 |
|
| |||||||||||||||||
| All | 96 658 | 74.2 | NA | 23.3 | NA | NA | 23.0 | NA | 1.0 | NA | 20.2 | NA | 1.1 | NA | 12.9 | NA | 1.8 |
|
| |||||||||||||||||
| Females, 1999–2001 | |||||||||||||||||
|
| |||||||||||||||||
| ≤14 | 178 | 100 | 0.6 | 0.2 | NA | 0.1 | 0.1 | NA | 3.0 | 0.6 | 0.8 | NA | 0.3 | 0.4 | 0.3 | NA | 0.7 |
|
| |||||||||||||||||
| 15–24 | 2390 | 71.4 | 9.2 | 4.1 | NA | 0.2 | 0.4 | NA | 11.4 | 0.9 | 0.4 | NA | 9.5 | 0.7 | 0.2 | NA | 18.2 |
|
| |||||||||||||||||
| 25–34 | 4386 | 60.1 | 24.9 | 7.4 | NA | 0.9 | 1.3 | NA | 5.7 | 1.3 | 0.8 | NA | 9.7 | 1.2 | 0.6 | NA | 12.3 |
|
| |||||||||||||||||
| 35–44 | 8372 | 52.0 | 54.8 | 12.3 | NA | 3.0 | 3.5 | NA | 3.5 | 2.6 | 2.0 | NA | 6.3 | 2.9 | 1.4 | NA | 8.6 |
|
| |||||||||||||||||
| 45–54 | 6530 | 60.5 | 78.2 | 11.3 | NA | 8.5 | 10.8 | NA | 1.0 | 4.5 | 3.5 | NA | 3.2 | 6.4 | 3.6 | NA | 3.1 |
|
| |||||||||||||||||
| 55–64 | 2768 | 75.0 | 88.1 | 7.3 | NA | 19.8 | 33.7 | NA | 0.2 | 7.7 | 9.1 | NA | 0.8 | 13.9 | 11.4 | NA | 0.6 |
|
| |||||||||||||||||
| 65–74 | 1499 | 81.1 | 93.5 | 4.9 | NA | 42.2 | 83.9 | NA | 0.1 | 16.1 | 30.0 | NA | 0.2 | 31.4 | 34.0 | NA | 0.1 |
|
| |||||||||||||||||
| ≥75 | 1823 | 71.6 | 100 | 5.8 | NA | 100 | 208.3 | NA | 0.0 | 100 | 285.7 | NA | 0.0 | 100 | 127.4 | NA | 0.0 |
|
| |||||||||||||||||
| All | 27 947 | 62.3 | NA | 6.5 | NA | NA | 26.3 | NA | 0.2 | NA | 24.9 | NA | 0.3 | NA | 13.6 | NA | 0.5 |
|
| |||||||||||||||||
| Males, 2012–2014 | |||||||||||||||||
|
| |||||||||||||||||
| ≤14 | 755 | 100 | 0.5 | 0.8 | 14.6 | 0.1 | 0.1 | −7.3 | 12.4 | 0.8 | 0.7 | −25.7 | 1.2 | 0.3 | 0.2 | −46.9 | 4.2 |
|
| |||||||||||||||||
| 15–24 | 17 891 | 66.6 | 12.0 | 26.5 | 27.9 | 0.3 | 0.5 | 17.9 | 52.5 | 1.2 | 0.5 | −3.8 | 55.9 | 0.4 | 0.1 | −23.0 | 172.0 |
|
| |||||||||||||||||
| 25–34 | 29 702 | 51.4 | 30.6 | 45.7 | 58.2 | 1.3 | 1.8 | 6.9 | 24.9 | 2.0 | 1.1 | 16.9 | 39.8 | 1.0 | 0.6 | −0.9 | 76.0 |
|
| |||||||||||||||||
| 35–44 | 28 040 | 54.3 | 49.1 | 46.4 | 25.3 | 4.3 | 5.9 | 14.6 | 7.8 | 4.2 | 2.4 | 10.0 | 19.5 | 2.6 | 1.8 | −0.2 | 25.1 |
|
| |||||||||||||||||
| 45–54 | 34 185 | 66.7 | 71.0 | 52.7 | 57.1 | 13.6 | 17.0 | 8.3 | 3.1 | 8.0 | 5.8 | 1.1 | 9.0 | 7.7 | 5.6 | 8.2 | 9.4 |
|
| |||||||||||||||||
| 55–64 | 25 113 | 65.2 | 87.2 | 44.1 | 90.6 | 33.4 | 41.8 | −2.5 | 1.1 | 13.7 | 14.3 | 6.0 | 3.1 | 19.6 | 14.8 | 6.1 | 3.0 |
|
| |||||||||||||||||
| 65–74 | 10 522 | 86.0 | 93.9 | 29.8 | 17.9 | 58.5 | 84.7 | −15.3 | 0.3 | 27.6 | 34.0 | −27.2 | 0.9 | 38.3 | 38.5 | −11.9 | 0.8 |
|
| |||||||||||||||||
| ≥75 | 9437 | 94.8 | 100 | 40.3 | −7.2 | 100 | 211.9 | −7.3 | 0.2 | 100 | 215.1 | −34.8 | 0.2 | 100 | 184.5 | 3.0 | 0.2 |
|
| |||||||||||||||||
| All | 155 658 | 62.3 | NA | 33.6 | 44.1 | NA | 25.6 | 11.1 | 1.3 | NA | 16.6 | −17.9 | 2.0 | NA | 15.1 | 16.9 | 2.2 |
|
| |||||||||||||||||
| Females, 2012–2014 | |||||||||||||||||
|
| |||||||||||||||||
| ≤14 | 379 | 100 | 0.6 | 0.4 | 109.3 | 0.0 | 0.1 | −23.0 | 8.1 | 0.6 | 0.6 | −27.3 | 0.3 | 0.2 | 0.2 | −45.5 | 2.8 |
|
| |||||||||||||||||
| 15–24 | 5053 | 57.8 | 9.2 | 7.8 | 89.1 | 0.3 | 0.4 | −2.0 | 22.1 | 0.9 | 0.3 | −20.5 | 12.0 | 0.3 | 0.1 | −33.7 | 52.1 |
|
| |||||||||||||||||
| 25–34 | 10 029 | 38.5 | 24.9 | 15.7 | 112.7 | 1.1 | 1.3 | 2.9 | 11.9 | 1.6 | 0.9 | 25.7 | 7.7 | 0.8 | 0.5 | −10.1 | 29.2 |
|
| |||||||||||||||||
| 35–44 | 12 420 | 38.6 | 44.8 | 20.4 | 65.4 | 3.2 | 3.7 | 6.0 | 5.5 | 3.0 | 2.0 | 4.6 | 6.0 | 2.0 | 1.4 | −4.4 | 14.9 |
|
| |||||||||||||||||
| 45–54 | 17 572 | 39.0 | 73.0 | 26.3 | 133.5 | 9.4 | 10.0 | −7.6 | 2.6 | 6.6 | 4.5 | 27.2 | 2.5 | 5.7 | 3.8 | 4.6 | 7.0 |
|
| |||||||||||||||||
| 55–64 | 11 323 | 46.0 | 91.2 | 18.5 | 154.8 | 23.7 | 24.9 | −26.2 | 0.7 | 13.5 | 9.8 | 7.0 | 0.7 | 14.7 | 10.4 | −9.0 | 1.8 |
|
| |||||||||||||||||
| 65–74 | 3503 | 63.3 | 96.8 | 8.7 | 75.7 | 44.6 | 55.3 | −34.1 | 0.2 | 24.7 | 23.8 | −20.7 | 0.2 | 31.0 | 29.7 | −12.6 | 0.3 |
|
| |||||||||||||||||
| ≥75 | 1995 | 67.0 | 100 | 5.7 | 1.7 | 100 | 168.1 | −19.3 | 0.0 | 100 | 183.3 | −35.9 | 0.0 | 100 | 138.2 | 7.3 | 0.0 |
|
| |||||||||||||||||
| All | 62 276 | 44.3 | NA | 12.9 | 99.2 | NA | 22.1 | −16.1 | 0.6 | NA | 17.7 | −28.9 | 0.4 | NA | 14.5 | 7.1 | 0.9 |
Abbreviations: D, diabetes; I/P, influenza/pneumonia; KD, kidney disease; NA, not applicable; SI, self-injury.
Discussion
The escalation of official suicide18 and drug intoxication death rates during the first 14 years of the 21st century19,20 revealed a burgeoning crisis. We see significant inconsistencies that seriously compromise the study of fatal self-harm or self directed violence. Although researchers, clinicians, medical examiners, and coroners acknowledge that repeated opioid and other drug self-intoxication is a form of self-directed injury, death arising from such behavior continues to be labeled as an “accident” or unintentional, despite the presence of an individual’s clinical history of deliberate, repeated substance misuse, which fundamentally increases the probability of later death. Restricting determination of intentionality to the day of death in the context of a pattern of intentional self-harm precludes the types of investigations needed to better understand the biological, social, and psychological factors that contribute to these premature deaths. Our study underscores an urgent need to overcome such inconsistencies in classification in order to study the factors associated with fatal self injuries more inclusively. Future research on SIM trends will need to evaluate a wide array of potential individual-level and contextual determinants (eg, social, economic, political, health, and environmental), disaggregating SIM by such variables as race/ethnicity, military veteran status, state, and region. We can readily infer from 2 studies,21,22 which differentiated suicide and unintentional poisoning mortality, that the burden of SIM disproportionately affects white individuals relative to black and Hispanic individuals.
The comparisons between fatal self-injury, as we defined the combination of suicide and the majority of over dose deaths, and the 3 proximally ranked diseases highlight a gross deficiency in simply weighing all deaths equally when prioritizing prevention. Basing rankings on mortality numbers or accompanying summary rates obscures the harm of SIM on those during the prime of their lives. Crude mortality rates alone fail to capture the effect of years of life lost; comparisons for the 1999 to 2001 and 2012 to 2014 periods revealed that more than70% of self-injury decedents were younger than 55 years compared with less than 12% of this population dying of diabetes, influenza and pneumonia, or kidney disease, substantiating the large comparative excess of lost years from self-injury. Incorporating nonsuicide DDSIs in the SIM rate illuminated absolute and relative increasing trends among women, which are obscured when viewed solely through the suicide lens. Further, the reconstituted SIM rate is nearly double the suicide rate. The SIM rate for males was still 2.6-fold higher than the female rate in 2014, but the 30% reduction in this sex ratio since 1999 reveals disquieting trends that augur further mortality increases among women in the coming years unless effective means of prevention are developed and pervasively deployed.
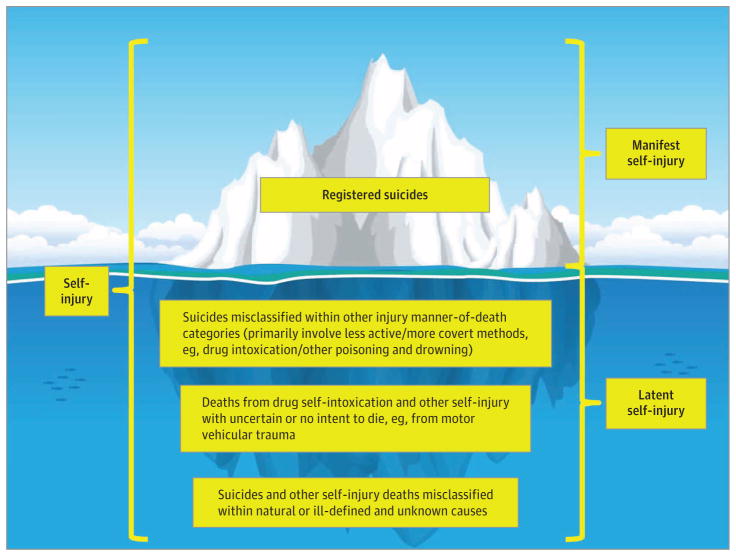
An iceberg illustrates the epidemiologic, clinical, and public health imperative to expand self-harm injury mortality beyond the confines of registered suicides (Figure 2). Although mortality from persisting self-harm serves as an etiology for certain diseases (eg, lung cancer caused by tobacco smoking and alcohol-related cirrhosis), suicide typically occurs as the result of multiple disorders (eg, schizophrenia, depressive disorders, bipolar disorder, and anxiety disorders as well as comorbid systemic diseases and acute alcohol intoxication), interpersonal stresses, and adverse life events. Stringent criteria that couple clearly defined intentions with actions to kill oneself assure that suicide determination is conservative in most countries.23
Figure 2.
Iceberg of Suicide and Latent Self-injury Mortality (Not to Scale)
Suicide under counting primarily involves less active or more am biguous methods, such as poisoning and drowning,24–26 and presumably includes opioid intoxication as a very lethal and increasingly accessible method.19 Moreover, documented multimorbidity mitigates against the conduct of autopsies and toxicological testing, especially in cases involving older middle-aged and elderly adults, the groups most prone to die from disease rather than injury.27 Consequently, this constellation of forces would predispose pharmaceutical opioid and other drug intoxication suicides to an excess likelihood of manner-of- death misclassification under natural causes (diseases). In addition, without an autopsy and toxicological testing, these suicides are also susceptible to misclassification under ill-defined and unknown causes.28,29
As a composite of registered suicides and estimated DDSIs that are not suicide, self-injury would have ranked as the eighth leading cause of death in the United States in 2013, ahead of influenza and pneumonia and kidney disease10 and behind diabetes.30 Suicide alone ranked as the tenth leading cause, and the estimated SIM rate has been rising much faster than the suicide rate since 2000. In this study, we compared mortality trends with patterns of self-injury and 3 proximally ranked diseases from 1999 to 2001 and 2012 to 2014 to contextualize the rankings and inform injury etiology, surveillance, prevention, treatment, and rehabilitation.
Without fundamental changes in public priorities and the allocation of health resources, we anticipate a continuing rise in the rate of SIM, with its heavy psychosocial, physical, and economic toll on individuals, families, and communities. This upward trajectory may continue despite general improvements in the national economy because there is a dearth of widely applied prevention programs and a paucity of treatment services for persons with mental and substance use disorders in the United States.31 Furthermore, unmet substance abuse treatment needs are associated with excess use and high costs of hospital emergency care,32 regardless of whether the “frequent flyers” are motivated solely to obtain opioids to alleviate cravings or actually to receive treatment for illnesses arising from intravenous use of drugs, suicide attempts, deliberate self-harm, or associated injuries (eg, falls and motor vehicular trauma). States are currently responding unevenly to the health care initiatives legislated in the Affordable Care Act and the Mental Health Parity and Addiction Equity Act,33 with vulnerable minorities being disproportionately and adversely affected.34
This study has a number of limitations. Our results could have been influenced by unexamined heterogeneity in death certification stemming from variable certifier training and practice, involvement of hospitals and death investigation systems and their types and professional accreditation status, autopsy and toxicological testing rates, diagnostic competence and coding, and/or relationships and coordination between state vital recording registrars and the National Center for Health Statistics.35–37
We acknowledge that our reconceptualization of SIM has not been validated,10 and its measurement is neither precise nor nuanced, with deficits that could be averted or ameliorated if there was uniform provision in death certificates for recording qualitative and quantitative information on alcohol and other substance use, misuse, and abuse. We recommend that the National Association of Medical Examiners, American College of Medical Toxicology, International Association of Coroners and Medical Examiners, Mortality Statistics Branch of the National Center for Health Statistics of the Centers for Disease Control and Prevention, and other stakeholders collaborate to attain this end within a standardized death certificate.
Another potential study limitation pertains to the number and relative ranking of comparison diseases. However, had the comparisons included the 5 major disease killers—heart disease, cancer, chronic obstructive pulmonary disease, stroke, and Alzheimerdisease29— this would not have tempered our potent finding that SIM disproportionately affects persons during their middle years, when costs to families, communities, and society are their highest. Like suicide, diabetes is underreported on death certificates,38 but correction also would be unlikely to diminish the salience of younger age selection in SIM. Additionally, although data on multiple causes of death revealed a greater role of diabetes in overall disease mortality than is evident from underlying cause-of-death data alone,39 it is likely these data seriously underestimate substance use and mental health disorders as powerful contributors to diabetes and other disease mortality. Our estimates of the SIM rate are conservative owing to the omission of self-injury deaths whose underlying cause is not drug intoxication, such as those from motor vehicular trauma and other forms of poisoning. Furthermore, persistent alcohol and other substance misuse contributed to many of these deaths.40
Conclusions
The burgeoning SIM rate has converged with the diabetes rate, but there is a 6-fold differential in the proportion of SIM vs diabetes deaths involving people younger than 55 years and SIM is increasingly affecting women relative to men. Accurately characterizing, measuring, and monitoring this major clinical and public health challenge will be essential for developing a comprehensive etiologic understanding and for evaluating preventive and therapeutic interventions.
Acknowledgments
Funding/Support: This research received partial support from grants R49CE002109 and R49CE002093 from the National Center for Injury Prevention and Control of the Centers for Disease Control and Prevention.
Footnotes
Conflict of Interest Disclosures: None reported.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the US Centers for Disease Control and Prevention or the US government.
Author Contributions: Dr Rockett had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Rockett, Larkin, Miller, Caine.
Acquisition, analysis, or interpretation of data: Rockett, Lilly, Jia, Nelson, Nolte, Putnam, Smith.
Drafting of the manuscript: Rockett, Lilly, Caine, Smith.
Critical revision of the manuscript for important intellectual content: Rockett, Jia, Larkin, Miller, Nelson, Nolte, Putnam, Smith.
Statistical analysis: Rockett, Lilly, Jia.
Obtaining funding: Caine.
Administrative, technical, or material support: Rockett.
Study supervision: Rockett.
References
- 1.Yoshimasu K, Kiyohara C, Miyashita K Stress Research Group of the Japanese Society for Hygiene. Suicidal risk factors and completed suicide: meta-analyses based on psychological autopsy studies. Environ Health Prev Med. 2008;13(5):243–256. doi: 10.1007/s12199-008-0037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warner M, Paulozzi LJ, Nolte KB, Davis GG, Nelson LS. State variation in certifying manner of death and drugs involved in drug intoxication deaths. Acad Forensic Pathol. 2013;3(2):231–237. [Google Scholar]
- 3.Haddon W., Jr The changing approach to the epidemiology, prevention, and amelioration of trauma: the transition to approaches etiologically rather than descriptively based. Am J Public Health Nations Health. 1968;58(8):1431–1438. doi: 10.2105/ajph.58.8.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rockett IRH, Hobbs GR, Wu D, et al. Variable classification of drug-intoxication suicides across US states: a partial artifact of forensics? PLoS One. 2015;10(8):e0135296. doi: 10.1371/journal.pone.0135296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Institute of Medicine. Emergency Medical Services at the Crossroads. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 6.Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 7.Committee on Identifying the Needs of the Forensic Sciences Community, National Research Council. Strengthening Forensic Science in the United States: A Path Forward. Washington, DC: National Academies Press; 2009. [Google Scholar]
- 8.Rockett IRH, Smith GS, Caine ED, et al. Confronting death from drug self-intoxication (DDSI): prevention through a better definition. Am J Public Health. 2014;104(12):e49–e55. doi: 10.2105/AJPH.2014.302244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rockett IRH, Kapusta ND, Coben JH. Beyond suicide: action needed to improve self-injury mortality accounting. JAMA Psychiatry. 2014;71(3):231–232. doi: 10.1001/jamapsychiatry.2013.3738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rockett IRH, Caine ED. Self-injury is the eighth leading cause of death in the United States: it is time to pay attention. JAMA Psychiatry. 2015;72(11):1069–1070. doi: 10.1001/jamapsychiatry.2015.1418. [DOI] [PubMed] [Google Scholar]
- 11.Knox KL, Caine ED. Establishing priorities for reducing suicide and its antecedents in the United States. Am J Public Health. 2005;95(11):1898–1903. doi: 10.2105/AJPH.2004.047217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bergen H, Hawton K, Waters K, et al. Premature death after self-harm: a multicentre cohort study. Lancet. 2012;380(9853):1568–1574. doi: 10.1016/S0140-6736(12)61141-6. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Suicide among adults aged 35–64 years: United States, 1999–2010. MMWR Morb Mortal Wkly Rep. 2013;62(17):321–325. [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. [Accessed December 9, 2015];Wide-ranging online data for epidemiologic research. http://wonder.cdc.gov/
- 15.World Health Organization. International Statistical Classification of Diseases, Tenth Revision (ICD-10) Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 16.Manton KG, Patrick CH, Stallard E. Population impact of mortality reduction: the effects of elimination of major causes of death on the ‘saved’ population. Int J Epidemiol. 1980;9(2):111–120. doi: 10.1093/ije/9.2.111. [DOI] [PubMed] [Google Scholar]
- 17.Rockett IRH. Injury elimination and survival: a cross-national study. Public Health. 1998;112(1):27–30. [PubMed] [Google Scholar]
- 18.Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014. NCHS Data Brief. 2016;(241):1–8. [PubMed] [Google Scholar]
- 19.Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374(2):154–163. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rossen LM, Bastian B, Warner M, Khan D, Chong Y. National Center for Health Statistics. [Accessed April 5, 2016];Drug poisoning mortality: United States. 1999–2014 http://blogs.cdc.gov/nchs-data-visualization/drug-poisoning-mortality/
- 21.Rockett IRH, Regier MD, Kapusta ND, et al. Leading causes of unintentional and intentional injury mortality: United States, 2000–2009. Am J Public Health. 2012;102(11):e84–e92. doi: 10.2105/AJPH.2012.300960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rockett IRH, Kapusta ND, Bhandari R. Suicide misclassification in an international context: revisitation and update. Suicidol Online. 2011;2:48–61. [Google Scholar]
- 24.Rockett IRH, Wang S, Stack S, et al. Race/ethnicity and potential suicide misclassification: window on a minority suicide paradox? BMC Psychiatry. 2010;10:35. doi: 10.1186/1471-244X-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huguet N, Kaplan MS, McFarland BH. Rates and correlates of undetermined deaths among African Americans: results from the National Violent Death Reporting System. Suicide Life Threat Behav. 2012;42(2):185–196. doi: 10.1111/j.1943-278X.2012.00081.x. [DOI] [PubMed] [Google Scholar]
- 26.Haw C, Hawton K. Suicide and self-harm by drowning: a review of the literature. Arch Suicide Res. 2016;20(2):95–112. doi: 10.1080/13811118.2015.1025120. [DOI] [PubMed] [Google Scholar]
- 27.Hoyert DL. The changing profile of autopsied deaths in the United States, 1972–2007. NCHS Data Brief. 2011;(67):1–8. [PubMed] [Google Scholar]
- 28.Phillips DP, Ruth TE. Adequacy of official suicide statistics for scientific research and public policy. Suicide Life Threat Behav. 1993;23(4):307–319. [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Toxicology testing and results for suicide victims: 13 states, 2004. MMWR Morb Mortal Wkly Rep. 2006;55(46):1245–1248. [PubMed] [Google Scholar]
- 30.Kochanek KD, Murphy SL, Xu J, Arias E. Mortality in the United States, 2013. NCHS Data Brief. 2014;(178):1–8. [PubMed] [Google Scholar]
- 31.Hoge MA, Stuart GW, Morris J, Flaherty MT, Paris M, Jr, Goplerud E. Mental health and addiction workforce development: federal leadership is needed to address the growing crisis. Health Aff (Millwood) 2013;32(11):2005–2012. doi: 10.1377/hlthaff.2013.0541. [DOI] [PubMed] [Google Scholar]
- 32.Rockett IRH, Putnam SL, Jia H, Chang CF, Smith GS. Unmet substance abuse treatment need, health services utilization, and cost: a population-based emergency department study. Ann Emerg Med. 2005;45(2):118–127. doi: 10.1016/j.annemergmed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 33.Wen H, Cummings JR, Hockenberry JM, Gaydos LM, Druss BG. State parity laws and access to treatment for substance use disorder in the United States: implications for federal parity legislation. JAMA Psychiatry. 2013;70(12):1355–1362. doi: 10.1001/jamapsychiatry.2013.2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andrews CM, Guerrero EG, Wooten NR, Lengnick-Hall R. The Medicaid expansion gap and racial and ethnic minorities with substance use disorders. Am J Public Health. 2015;105(suppl 3):S452–S454. doi: 10.2105/AJPH.2015.302560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hanzlick R. The relevance of queries and coding procedures to the writing of cause-of-death statements. Am J Forensic Med Pathol. 1996;17(4):319–323. doi: 10.1097/00000433-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Smith Sehdev AE, Hutchins GM. Problems with proper completion and accuracy of the cause-of-death statement. Arch Intern Med. 2001;161(2):277–284. doi: 10.1001/archinte.161.2.277. [DOI] [PubMed] [Google Scholar]
- 37.Davis GG National Association of Medical Examiners and American College of Medical Toxicology Expert Panel on Evaluating and Reporting Opioid Deaths. Complete republication: National Association of Medical Examiners position paper: recommendations for the investigation, diagnosis, and certification of deaths related to opioid drugs. J Med Toxicol. 2014;10(1):100–106. doi: 10.1007/s13181-013-0323-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McEwen LN, Karter AJ, Curb JD, Marrero DG, Crosson JC, Herman WH. Temporal trends in recording of diabetes on death certificates: results from Translating Research Into Action for Diabetes (TRIAD) Diabetes Care. 2011;34(7):1529–1533. doi: 10.2337/dc10-2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lin YP, Lu TH. Trends in death rate from diabetes according to multiple-cause-of-death differed from that according to underlying-cause-of- death in Taiwan but not in the United States, 1987–2007. J Clin Epidemiol. 2012;65(5):572–576. doi: 10.1016/j.jclinepi.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 40.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]