Abstract
Objectives
Very few studies have evaluated perceptions of electronic nicotine delivery systems (ENDS) among smokers with mental illness. This study assessed expectancies about the effects of smoking combustible cigarettes or using ENDS among current smokers with and without severe psychological distress (SPD).
Methods
We used a crowdsourcing system to survey 268 smokers on their expectancies for the effects of combustible cigarettes and ENDS. Positive expectancies assessed included negative affect reduction, stimulation, positive social effects and weight control, and negative expectancies included negative physical effects, negative psychosocial effects and future health concerns.
Results
Smokers with SPD had higher positive expectancies for weight control and social effects of both products compared to those without such distress, and higher expectancies for stimulation from combustible cigarettes compared to ENDS. All participants had significantly lower negative expectancies for ENDS compared to combustible cigarettes, with no significant differences between the groups.
Conclusions
Smokers with SPD may be more vulnerable toward ENDS use, as they are for combustible cigarette use, due to greater positive expectancies of the products. Challenging positive expectancies may increase the efficacy of tobacco control efforts in this vulnerable population.
Keywords: electronic cigarette, expectancies, smoking, cigarette, mental illness
INTRODUCTION
Combustible cigarette smoking continues to decline in the U.S., however the use of electronic nicotine delivery systems (ENDS), is steadily increasing.1 While ENDS may expose users to lower levels of toxicants than combustible cigarettes, their long-term health effects remain unknown.2,3 The Food and Drug Administration (FDA) recently deemed ENDS subject to regulation under the Family Smoking Prevention and Tobacco Control Act.4 As such, assessment of factors affecting ENDS use, especially among vulnerable populations, will aid in future regulatory decisions. Individuals with severe psychological distress (SPD) may be particularly prone to ENDS use. People with SPD have higher rates of nicotine dependence and lower quit rates than those without SPD,6,7 resulting in significant smoking related morbidity and mortality. 8,9 Initial reports also indicate that ENDS use is disproportionately high among people with mental illness,10,11 but reasons for the high rates of ENDS use are unknown.
Smoking expectancies, or positive and negative beliefs about the anticipated effects of smoking, are associated with cigarette use among people with and without mental illness.12–17 Compared to smokers without mental illness, those with mental illness endorse greater positive smoking expectancies (ie, boredom reduction, stimulation, taste or sensory pleasure from handling cigarettes), and particularly the belief that smoking will reduce negative affect18–21 and help them to cope with social situations.16 Positive and negative expectancies for ENDS are lower than for combustible cigarettes in the general population. Specifically, ENDS are rated as less toxic and addictive, and more socially acceptable than combustible cigarettes, but also as less effective for negative affect reduction, weight control and stimulation.22–26 Similar to combustible cigarettes, greater positive expectancies for ENDS have been associated with an increased likelihood of future ENDS use, and greater negative expectancies with a decreased likelihood of future use.25 However, expectancies for ENDS among individuals with SPD are largely unknown.
Comparing expectancies for combustible cigarettes versus ENDS in smokers with and without SPD may illuminate reasons for differential rates of nicotine and tobacco use by these populations, and may inform cessation interventions or public health efforts. Therefore, we compared combustible and ENDs expectancies among smokers with SPD and controls without SPD. We hypothesized that smokers with SPD would rate negative affect reduction expectancies higher than controls for both combustible cigarettes and ENDS. We also hypothesized that both groups would have lower health concern expectancies for ENDS than for combustible cigarettes.
METHODS
Participants
Participants were recruited through Amazon.com’s Mechanical Turk (mTurk), a validated crowdsourcing system.27,28 Eligible participants were ≥ 18, resided in the United States, had smoked ≥ 5 cigarettes per day for ≥ one year, and had ≥ 80% approval rating on previously submitted mTurk tasks. SPD was prospectively determined with the Kessler 6 (K6) Questionnaire, a validated measure of non-specific, self-perceived psychological distress over the past 30 days. We used the standard cutoff score of ≥ 135 to indicate significant distress.
Procedures
Participants were recruited in March of 2015. After confirming informed consent, participants completed a brief eligibility screening, including the Kessler K6, to identify smokers with SPD and controls. The survey was designed to close once 300 participants were enrolled (150 SPD, 150 CON). However, due to a technical problem, enrollment was closed early; therefore the total sample size was 268 (135 with SPD, 133 controls). Participants were ineligible if they failed to meet one of the eligibility criteria listed above, when one of the groups filled, or if they chose to terminate participation during the screen.
Eligible participants completed a battery of questionnaires (below) and were compensated $2.00 through mTurk. To ensure participant attention, a simple mathematical question was embedded within the survey. Data from participants who failed the question were excluded.
Measures
Demographics and smoking history were assessed using clinic-derived measures. The Fagerström Test for Nicotine Dependence (FTND) 29 was administered to evaluate severity of nicotine dependence. To assess other tobacco product use, participants were asked “Have you ever used electronic cigarettes (e-cigarettes)?” Expectancies for combustible cigarettes and ENDS were measured using brief versions of the Smoking Effects Questionnaire (SEQ; ESEQ),30 which included the 7 items that loaded most highly on each of the subscales that comprise 2 higher-order factors (Positive and Negative Expectancies).30 The 4 Positive Expectancy items came from the Negative Affect Reduction Scale (“Smoking an [electronic] cigarette would help me when I am uptight, nervous or tense”), the Stimulation Scale (“Smoking an [electronic] cigarette would keep me from slowing down”), the Positive Social Effects Scale (“Smoking an [electronic] cigarette would give me something to do with my hands in a group”), and the Weight Control Scale (“Smoking an [electronic] cigarette would help me lose weight”). The 3 Negative Expectancy items came from the Negative Physical Effects Scale (“Smoking an [electronic] cigarette would make me feel weaker physically”), the Negative Psychosocial Effects Scale (“Smoking an [electronic] cigarette would make my family or friends respect me less”), and the Future Health Concerns Scale (“Smoking an [electronic] cigarette would make me worry about getting cancer”). Participants rated the importance of each expectancy item on 0–3 scales (0 = “False, the statement does not apply to me,” 1 = “True, the statement does apply to me, and it is hardly at all important,” 2 = “True, the statement does apply to me, and it is moderately important,” 3 = “True, the statement does apply to me, and it is very important”).
Data Analysis
Group comparisons on demographics and smoking history were conducted using t-tests and chi-square tests. Groups and products (cigarettes versus ENDS) were compared on the 2 higher-order factors (ie, positive vs. negative) using 2 × 2 Analysis of Covariance tests (ANCOVAs), with Group (control, SPD) as the between-groups factor and Product (combustible cigarette, ENDS) as the within-subjects factor. The same approach was used to compare ratings on each specific expectancy item. Number of cigarettes per day was covaried because the groups differed significantly on this variable and it is known to affect smoking expectancies.30 Prior ENDS use was also covaried as experience with the products may have influenced expectancy ratings. As exploratory analyses, we also compared groups for overall positive and negative expectancies based on whether or not they had any prior ENDS use. Differences were considered significant when p < .05. Analyses were conducted with SPSS version 22 (IBM).
RESULTS
Sample Characteristics
Participants were 31.7 ± 9.8 years old, 54.5% were male, 81.3% were white, and they smoked 11.8 ± 6.8 cigarettes per day (CPD). Participants with SPD were younger, more likely to be non-white, and smoked fewer CPD than the control group (see Table 1). Overall, 65.5% of participants reported prior ENDS use (NS). Internal consistency of the positive and negative SEQ-brief and ESEQ-brief scales ranged from Cronbach’s alphas of 0.53 – 0.60 and 0.57 – 0.68, respectively, which is acceptable given the broad range of effects that these combined scales measure.
Table 1.
Participant Characteristics
| Total (N = 268) | SPD (N = 133) | Control (N = 135) | p-valuea | |
|---|---|---|---|---|
| Demographic Characteristics | ||||
| Age, yrs | 31.7 ± 9.8 | 30.2 ± 8.4 | 33.2 ± 10.8 | .01 |
| Less than highschool education (%) | 1.5 | 1.5 | 1.5 | .99 |
| Male (%) | 54.5 | 50.4 | 58.5 | .18 |
| White (%) | 81.3 | 72.9 | 89.6 | <.01 |
| Psychiatric Characteristics | ||||
| K6 score | 10.9 ± 5.8 | 15.7 ± 2.6 | 6.1 ± 3.6 | <.01 |
| Smoking Characteristics | ||||
| Cigarettes per day | 11.8 ± 6.8 | 10.8 ± 5.3 | 12.8 ± 8.0 | .02 |
| FTND (0–10) | 4.2 ± 2.2 | 4.2 ± 2.1 | 4.2 ± 2.3 | .96 |
| Prior e-cigarette use (%) | 65.5 | 66.9 | 64.2 | .64 |
Values represent Mean ± SD unless otherwise indicated.
p-values based on independent sample t-tests for continuous variables and chi-square measures for categorical variables.
Positive and Negative Smoking Expectancies
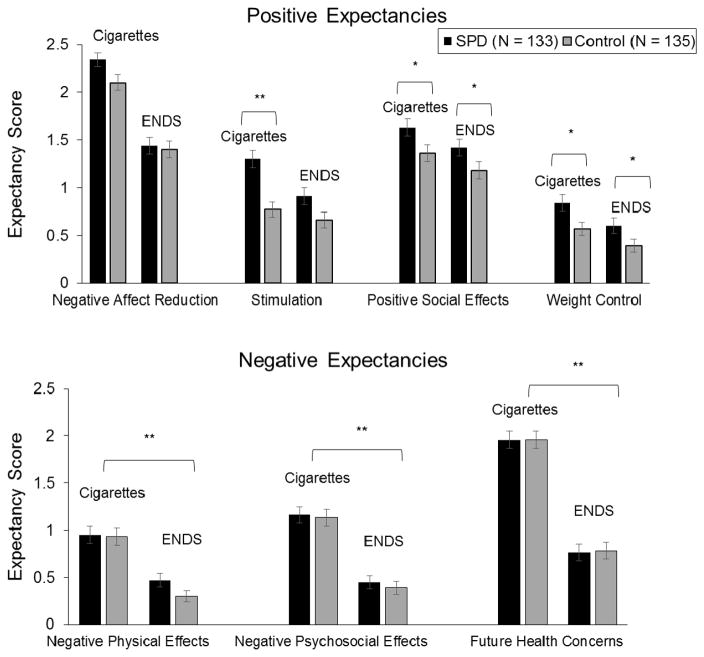
Overall, participants with SPD had higher positive expectancies for both combustible cigarettes and ENDS than the control group (p < .01). Specifically, the SPD group had higher expectancy ratings on the Positive Social Effects (p = .01) and Weight Control items (p = .01) for both cigarettes and ENDS compared to the control group (Figure 1, top). In addition, the SPD group had higher expectancy ratings than the control group on the Stimulation item for combustible cigarettes (p < .01), but the groups did not differ on Stimulation ratings for ENDS (Figure 1, top).
Figure 1.
Positive (top) and negative (bottom) smoking expectancy scores (scale range 0–3) in smokers with severe psychological distress (SPD) (solid bars) and controls (light bars) for combustible cigarettes and electronic nicotine delivery systems (ENDS). Bars represent individual item scores (M ± SEM) (* p < .05, **p < .01). For Stimulation (F (1, 255) = 5.35, p = .02), the SPD group endorsed higher expectancies than the Control group for combustible cigarettes but not ENDS (p < .01). For Positive Social Effects (F (1, 255) = 6.19, p = .01) and Weight Control (F (1, 255) = 6.53, p = .01), the SPD group endorsed higher expectancies for both products. For Negative Physical Effects (F (1, 255) = 12.01, p < .01), Negative Psychosocial Effects (F (1, 255) = 13.98, p < .01), and Future Health Concerns (F (1, 255) = 15.66, p < .01), both groups endorsed higher expectancies for combustible cigarettes compared to ENDS.
Overall, both groups had higher negative expectancies for combustible cigarettes than for ENDS (p < .01). Specifically, both groups reported higher expectancy ratings on the Physical Effects, Negative Psychosocial Effects and Future Health Concerns items for combustible cigarettes compared to ENDS (p’s < .01) (Figure 2, bottom).
Composite Smoking Expectancies as a Function of Prior ENDs Use
Among participants with prior ENDS experience, the SPD group had higher overall positive expectancies than the control group for both products (F (1, 172) = 3.29, p < .05), and both groups had higher overall negative expectancies for combustible cigarettes than for ENDS (F (1, 172) = 48.27, p < .01).
Likewise, among participants without prior ENDS experience, the SPD group had higher overall positive expectancies than the controls for both products (F (1, 89) = 13.98, p < .0). Both groups had higher overall positive expectancies for ENDS than for cigarettes (F (1, 89) = 16.98, p < .01), and higher negative expectancies for combustible cigarettes than ENDS (F (1, 89) = 9.48, p < .01).
DISCUSSION
Consistent with our hypothesis and studies in the general population, both individuals with and without SPD reported lower negative expectancies (specifically, were less concerned about Negative Physical Effects, Negative Psychosocial Effects, and Future Health Concerns) for ENDS compared to combustible cigarettes.23–25 These results were uninfluenced by whether or not they had prior ENDS use. The perception of reduced risks of ENDS may be a result of the aggressive advertising of these products.31,32 One study, for example, found that 95% of branded ENDS websites made health claims, and 64% had a smoking cessation related claim.33 Although research suggests that ENDS may be less harmful than combustible cigarettes, little is known about the health effects of extended use. 2,34
Individuals with SPD were as concerned as smokers without SPD about the negative effects of cigarettes and ENDS. Similarities between smokers with and without psychiatric disorders on negative expectancies for combustible cigarettes have been reported in the past, 16,18,20–21 and suggest that messages regarding the harms of tobacco products are wide reaching. However, the SPD group had greater expectancies that both cigarettes and ENDS would help with weight control and positive social interactions, and that combustible cigarettes would have stronger stimulating effects, than the control group. Individuals with mental illness generally have higher positive smoking expectancies than those without mental illness, and these expectancies have been associated with persistent smoking.17–18,21 Contrary to our hypothesis and previous research, the SPD group did not endorse higher Negative Affect Reduction expectancies than Controls for either product. Negative affect reduction was rated as the most important expectancy across groups and products, as has been shown in other clinical samples.16
We also looked at differences in expectancies as a function of prior ENDS use. There were no differences in positive expectancies of combustible cigarettes and ENDS among individuals with prior ENDS use, however individuals without prior ENDS use had higher positive expectancies for combustible cigarette than for ENDS. Whether positive expectancies promoted ENDS use or changed as a function of use remains an empirical question. However, there is some evidence that positive ENDS expectancies are associated with sustained ENDS use, and these individuals may be the subset who transition from combustible cigarettes to ENDS.35
Several study limitations should be noted. First, the use of mTurk resulted in a sample with low minority representation. Additionally, we limited the study to current smokers, as research shows that they are significantly more likely to use ENDS than nonsmokers.1 Several strengths should also be noted. We prospectively identified SPD and Control smokers using an established criterion during screening, ensuring comparable group sizes and limiting biases in group determination.5 In addition, the online crowdsourcing system increased geographic representation among our sample.
This study adds to the emerging evidence that smokers perceive ENDS to be of lower risk than combustible cigarettes, and those with mental illness have higher positive expectancies regarding nicotine and tobacco products than those without mental illness. Modifying positive smoking expectancies for both cigarettes and ENDS (eg, challenging overly positive beliefs of smoking) and assessing associations between ENDS expectancies and uptake may increase the efficacy of smoking cessation and public health interventions aimed at reducing product use.
IMPLICATIONS FOR TOBACCO REGULATION
As the FDA develops regulations related to sale and advertising of ENDS, it is important to consider the implications for vulnerable populations. Similar to combustible cigarettes, smokers with mental illness have higher positive expectancies for the effects of ENDS. Efforts are needed to ensure that accurate messaging regarding the effects of these products will reach those most burdened by nicotine addiction.
Acknowledgments
Funding: The research reported in this paper was supported by the National Institute on Drug Abuse and the Food and Drug Administration Center for Tobacco Products (P50DA036114). Additional author support was provided by U54DA031659 (JWT) and DA034628 (DJR). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Food and Drug Administration.
Footnotes
Human Subjects Statement
The Institutional Review Board at Brown University approved this study and declared it to be exempt from the regulations of 45 CRF 46 regarding the inclusion of human participants in research (#1411001167).
Conflict of Interest Statement
All authors of this article declare they have no conflicts of interest.
Contributor Information
Mollie E. Miller, Postdoctoral Research Associate, Center for Alcohol and Addiction Studies, Brown University, Providence, RI.
Jennifer W. Tidey, Professor, Center for Alcohol and Addiction Studies, Brown University, Providence, RI.
Damaris J. Rohsenow, Professor, Center for Alcohol and Addiction Studies, Brown University, Providence, RI.
Stephen T. Higgins, Professor, Vermont Center on Tobacco Regulatory Science, University of Vermont, Burlington, VT.
References
- 1.King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010–2013. Nicotine Tob Res. 2015;17(2):219–227. doi: 10.1093/ntr/ntu191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hecht SS, Carmella SG, Kotandeniya D, et al. Evaluation of toxicant and carcinogen metabolites in the urine of e-cigarette users versus cigarette smokers. Nicotine Tob Res. 2015;17(6):704–709. doi: 10.1093/ntr/ntu218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orr MS. Electronic cigarettes in the USA: a summary of available toxicology data and suggestions for the future. Tob control. 2014;23(Suppl 2):18–22. doi: 10.1136/tobaccocontrol-2013-051474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.FDA takes significant steps to protect Americans from dangers of tobacco through new regulation [press release] 2016 May 5; [Google Scholar]
- 5.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 6.Hagman BT, Delnevo CD, Hrywna M, Williams JM. Tobacco use among those with serious psychological distress: results from the national survey of drug use and health, 2002. Addict Behav. 2008;33(4):582–592. doi: 10.1016/j.addbeh.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sung HY, Prochaska JJ, Ong MK, et al. Cigarette smoking and serious psychological distress: a population-based study of California adults. Nicotine Tob Res. 2011;13(12):1183–1192. doi: 10.1093/ntr/ntr148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chwastiak LA, Rosenheck RA, Desai R, Kazis LE. Association of psychiatric illness and all-cause mortality in the National Department of Veterans Affairs Health Care System. Psychosom Med. 2010;72(8):817–822. doi: 10.1097/PSY.0b013e3181eb33e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suvisaari J, Partti K, Perala J, et al. Mortality and its determinants in people with psychotic disorder. Psychosom Med. 2013;75(1):60–67. doi: 10.1097/PSY.0b013e31827ad512. [DOI] [PubMed] [Google Scholar]
- 10.Cummins SE, Zhu SH, Tedeschi GJ, et al. Use of e-cigarettes by individuals with mental health conditions. Tob Control. 2014;23(Suppl 3):48–53. doi: 10.1136/tobaccocontrol-2013-051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prochaska JJ, Grana RA. E-cigarette use among smokers with serious mental illness. PloS One. 2014;9(11):e113013. doi: 10.1371/journal.pone.0113013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cano MA, Lam CY, Chen M, et al. Positive smoking outcome expectancies mediate the association between negative affect and smoking urge among women during a quit attempt. Exp Clin psychopharmacol. 2014;22(4):332–340. doi: 10.1037/a0036749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Copeland AL, Brandon TH. Testing the causal role of expectancies in smoking motivation and behavior. Addict Behav. 2000;25(3):445–449. doi: 10.1016/s0306-4603(99)00003-9. [DOI] [PubMed] [Google Scholar]
- 14.Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: prediction of smoking lapse and relapse. J Abnorm Psychol. 2005;114(4):661–675. doi: 10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
- 15.Wetter DW, Smith SS, Kenford SL, et al. Smoking outcome expectancies: factor structure, predictive validity, and discriminant validity. J Abnorm Psychol. 1994;103(4):801–811. doi: 10.1037//0021-843x.103.4.801. [DOI] [PubMed] [Google Scholar]
- 16.Tidey JW, Rohsenow DJ. Smoking expectancies and intention to quit in smokers with schizophrenia, schizoaffective disorder and non-psychiatric controls. Schizophr Res. 2009;115(2–3):310–316. doi: 10.1016/j.schres.2009.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hruska B, Bernier J, Kenner F, et al. Examining the relationships between posttraumatic stress disorder symptoms, positive smoking outcome expectancies, and cigarette smoking in people with substance use disorders: a multiple mediator model. Addict Behav. 2014;39(1):273–281. doi: 10.1016/j.addbeh.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Calhoun PS, Levin HF, Dedert EA, et al. The relationship between posttraumatic stress disorder and smoking outcome expectancies among U.S. military veterans who served since September 11, 2001. J Trauma Stress. 2011;24(3):303–308. doi: 10.1002/jts.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McClernon FJ, Calhoun PS, Hertzberg JS, et al. Associations between smoking and psychiatric comorbidity in U.S. Iraq- and Afghanistan-era veterans. Psychol Addict Behav. 2013;27(4):1182–1188. doi: 10.1037/a0032014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stewart DW, Vinci C, Adams CE, et al. Smoking topography and outcome expectancies among individuals with schizotypy. Psychiatry Res. 2013;205(3):205–212. doi: 10.1016/j.psychres.2012.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weinberger AH, George TP, McKee SA. Differences in smoking expectancies in smokers with and without a history of major depression. Addict Behav. 2011;36(4):434–437. doi: 10.1016/j.addbeh.2010.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Etter JF, Bullen C. Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction. 2011;106(11):2017–2028. doi: 10.1111/j.1360-0443.2011.03505.x. [DOI] [PubMed] [Google Scholar]
- 23.Goniewicz ML, Lingas EO, Hajek P. Patterns of electronic cigarette use and user beliefs about their safety and benefits: an internet survey. Drug Alcohol Rev. 2013;32(2):133–140. doi: 10.1111/j.1465-3362.2012.00512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harrell PT, Marquinez NS, Correa JB, et al. Expectancies for cigarettes, e-cigarettes, and nicotine replacement therapies among e-cigarette users (aka vapers) Nicotine Tob Res. 2015;17(2):193–200. doi: 10.1093/ntr/ntu149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hendricks PS, Cases MG, Thorne CB, et al. Hospitalized smokers’ expectancies for electronic cigarettes versus tobacco cigarettes. Addict Behav. 2015;41:106–111. doi: 10.1016/j.addbeh.2014.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pineiro B, Correa JB, Simmons VN, et al. Gender differences in use and expectancies of e-cigarettes: online survey results. Addict Behav. 2016;52:91–97. doi: 10.1016/j.addbeh.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk: A New Source of Inexpensive, Yet High-Quality, Data? Perspect Psychol Sci. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 28.Simons DJ, Chabris CF. Common (mis)beliefs about memory: a replication and comparison of telephone and Mechanical Turk survey methods. PloS One. 2012;7(12):e51876. doi: 10.1371/journal.pone.0051876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 30.Rohsenow DJ, Abrams DB, Monti PM, et al. The Smoking Effects Questionnaire for adult populations. Development and psychometric properties. Addict Behav. 2003;28(7):1257–1270. doi: 10.1016/s0306-4603(02)00254-x. [DOI] [PubMed] [Google Scholar]
- 31.Cantrell J, Emelle B, Ganz O, et al. Rapid increase in e-cigarette advertising spending as Altria’s MarkTen enters the marketplace. Tob Control. 2016;25(e1):e16–18. doi: 10.1136/tobaccocontrol-2015-052532. [DOI] [PubMed] [Google Scholar]
- 32.Kim AE, Arnold KY, Makarenko O. E-cigarette advertising expenditures in the U.S., 2011–2012. Am J Prev Med. 2014;46(4):409–412. doi: 10.1016/j.amepre.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Grana RA, Ling PM. “Smoking revolution”: a content analysis of electronic cigarette retail websites. Am J Prev Med. 2014;46(4):395–403. doi: 10.1016/j.amepre.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farsalinos KE, Polosa R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review. Ther Adv Drug Saf. 2014;5(2):67–86. doi: 10.1177/2042098614524430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harrell PT, Simmons VN, Pineiro B, et al. E-cigarettes and expectancies: why do some users keep smoking? Addiction. 2015;110(11):1833–1843. doi: 10.1111/add.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]