The necessity of the times, more than ever, calls for our utmost circumspection, …
— Samuel Adams, 1771
When computed tomography (CT) became available in the 1970s, it enabled us to establish diagnoses with unprecedented speed and accuracy. But it also affected the way we practice and teach medicine, shifting our focus from the bedside to the laboratory and giving rise to a malady that has slowly pervaded our profession. I call this malady “technologic tenesmus”—the uncontrollable urge to rely on sophisticated medical gadgetry for diagnoses.1
Technologic tenesmus is particularly noticeable with regard to CT. Indeed, from my observations as a fulltime medical educator in city-county hospitals, private community hospitals, and university clinical settings, indiscriminate use of this test is almost routine.
To encourage circumspection before ordering CT, I emphasize here the drawbacks of this test—its expense, the high dose of radiation it delivers, the laziness it promotes, and the havoc it can wreak when misinterpreted. I also highlight certain limitations of CT and suggest ways to reduce its radiation dose and curtail its ever-increasing misuse.
Drawbacks
Exorbitantly Expensive
How Much Does a CT Examination Cost?
I often ask that question of medical students, house officers, faculty members, and practicing subspecialists, but few of them ever answer correctly. In fact, most are surprised—and a few shocked—to learn how expensive CT really is.
In a survey of 4 major hospitals in Houston, I found that the charge for CT of the head, chest, or abdomen—including contrast, but excluding the radiologist's fee—ranges from $1,400 to $2,500. The same studies without contrast average $100 to $200 less. Scans of the head are slightly cheaper than those of the chest or abdomen. One of the hospitals automatically includes the pelvis in abdominal CTs, which raises the cost to $4,079 (abdomen, $2,112; pelvis, $1,967).
Comment
These prices can create a significant financial burden for patients, especially those who undergo multiple CT examinations. And for those without medical insurance, the burden can be devastating. Yet, the medical literature and teachers in medical schools remain silent when it comes to the monetary specifics of CT. No wonder physicians know so little about the expense of this test.
Delivers High Dose of Radiation
How Much Radiation Does a Patient Receive from a CT Examination?
Even the few who know how much CT costs almost invariably are ignorant of how much radiation it delivers. They are not alone.
Using a self-administered mail questionnaire, Renston and colleagues2 surveyed 1,000 board-certified physicians nationwide regarding the risks and benefits of chest CT. More than 90% of the 313 respondents—comprising internists, pulmonologists, thoracic surgeons, and family practitioners—either “did not know” or significantly underestimated the degree of radiation exposure associated with chest CT. In a similar questionnaire administered in England to 130 doctors, including 10 consultant radiologists, 97% of the answers were underestimates of the actual doses of radiation that patients receive during various radiologic investigations.3
Several factors determine the radiation dose a patient receives from CT. These include the design of the scanner, size of the patient, anatomic volume scanned, scanning protocol, technique used, and quality of the x-ray beam.4
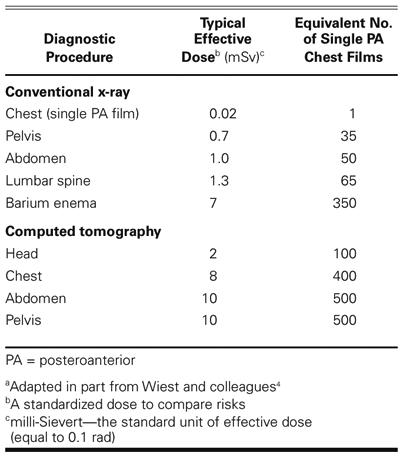
As shown in Table I, typical effective radiation doses in adults range from about 2 mSv (0.2 rad) for head CTs to about 8 to 10 mSv for CTs of the chest, abdomen, or pelvis.4 These latter doses are high compared to those of natural background radiation, which is about 3 mSv/year.5 Thus, it would take a person 3.3 years to get the same amount of background radiation that an abdominal CT delivers in less than a minute. Even more striking, one chest CT gives an effective dose of radiation equivalent to that of about 400 posteroanterior chest films.
TABLE I. Effective Radiation Doses from Conventional X-Ray Examinations and Computed Tomographya
Comment
Although CT has been with us for more than 3 decades, only in recent years have radiologists and allied radiology personnel focused attention on the amount and potential risks of radiation that CT delivers. Clearly, CT is a costly and relatively high-dose procedure, with levels of radiation often approaching and sometimes exceeding those known to increase the probability of cancer.4 Furthermore, the radiation dose per procedure has not diminished with the advent of helical, fluoroscopic, and multi-slice techniques.4
Yet the use of CT continues to spiral upwards.6 Many patients undergo 2 or 3 CT examinations in the same day and then have serial scans during follow-up. In that regard, Wiest and colleagues reported that 7% of a large group of patients had more than 5 CT scans, and 4% had 9 or more.4 Disturbingly, I recently saw a patient who had undergone 12 CT examinations during the previous 3 months and was in the hospital to have another one. While evidence linking CT with cancer has not been established, the carcinogenic potential of this test is real.7,8
About 40% of the collective dose of radiation in diagnostic radiology results from CT procedures,4,9 4% of which involve children 0 to 15 years old.8 Moreover, the radiation dose in children often exceeds the level necessary for diagnostic information,10 and the proportion of CT examinations in children is increasing rapidly.8 Even worse, a panel of expert pediatric radiologists concluded that up to 30% of CTs in children are unnecessary.11 Given the fact that children are more sensitive to radiation than are middle-aged adults by a factor of 10,12 pediatric radiologists wisely are leading the crusade against the unnecessary or indiscriminate use of CT.
Promotes Laziness
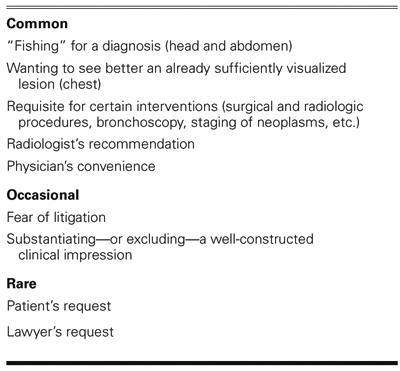
Physicians order CTs for a variety of reasons (Table II). From my vantage point, the most common reason is “fishing”—scanning the body part thought to be the source of the patient's complaint or problem, in the hope that a diagnosis will somehow be reeled in. In such cases, the physician takes a brief medical history, may or may not examine the patient, and, guided by the chief complaint, proceeds directly to CT scanning.
TABLE II. Observed Reasons for Ordering Computed Tomography
This approach has many attractive features. It takes little of the physician's time, requires no special expertise, demands no discriminate thought, and serves as an easy, convenient way to obtain a lot of information quickly. In fact, the physician need not even see the patient before ordering the test.
Comment
There appear to be two basic reasons why physicians use CT to fish for diagnoses—convenience and necessity. With regard to convenience, we have a large group of well-trained doctors who once were capable of using their minds and sensory faculties to make correct diagnoses. Through CT, however, they have found an easy way to reduce their busy workloads. And by using CT over and over again in this manner, they gradually, but unwittingly, become victims of technologic tenesmus.
The other reason—necessity—stems from our current medical education system. We are producing laboratory-oriented physicians who are deficient in clinical skills, especially history-taking and physical examination. They also are poorly informed about the natural history of disease. As a consequence, they turn to CT and other forms of advanced technology to formulate rather than substantiate their clinical impressions. Inevitably, they end up prisoners of the laboratory.
That said, fishing with CT frequently does provide a correct diagnosis, which reinforces the physician's inclination to use the approach routinely. But reeling in diagnoses in this fashion does nothing to improve the physician's medical knowledge or clinical skills, and it may harm the patient.
One additional point deserves attention. Many times, fishing with CT yields normal findings or uncovers abnormalities of uncertain clinical relevance or significance. Those situations call for skillful linking of all clinical information,13 a challenge that physicians often meet inappropriately with numerous consultations and myriad tests—including more CTs.
The other listed reasons for ordering CT are self-explanatory and will not be discussed here. Regrettably, ordering CT as the crucial means of substantiating or excluding a well-constructed clinical impression—the way it should be used—is among the least common of the reasons.
Misinterpretation Breeds Costly Mismanagement
As with all tests, CT can be misinterpreted. Witness the following case summaries:
Case 1
A 53-year-old woman presented with a distended urinary bladder that was mistaken clinically and on CT as a pelvic neoplasm, probably ovarian. The CT report prompted a host of additional studies, including 2 more CTs. But on the second hospital day, another staff radiologist read the initial CT study as normal. A Foley catheter then unveiled the true nature of the patient's illness.
Case 2
A 47-year-old man had a deep venous thrombosis and shortness of breath, findings that prompted a CT angiogram of the chest. The official CT report described bilateral pulmonary thromboemboli, and the patient received an inferior vena caval filter. Shortly thereafter, 2 other staff radiologists read the CT angiogram as normal. When the patient got his hospital bill, his shortness of breath understandably returned.
Case 3.
A 34-year-old woman underwent cranial CT for dizziness. When the CT report described lytic lesions in the skull suggestive of malignancy, her physician immediately ordered CTs of the chest and abdomen looking for the “primary,” and obtained a slew of tests for multiple myeloma. All produced normal results. After $23,600 of unnecessary testing, a neuroradiologist interpreted the lytic skull lesions as venous lakes—a benign, normal variant.
Comment
These cases show what can happen when no one questions the interpretation of a CT examination. They also are reminders that all of us, including radiologists, are fallible.
Limitations
Although Table III speaks for itself, I want to elaborate on 3 of the limitations.
TABLE III. Limitations of Computed Tomography
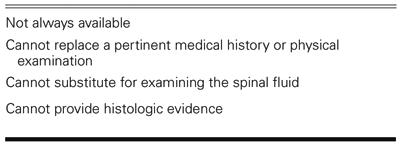
When the CT scanner breaks down, or is otherwise unavailable, patient-oriented activities largely come to a halt. I have observed this phenomenon in 3 different hospitals and consider it a sad reflection of today's practice of medicine.
Because findings from CT are so comprehensive, physicians sometimes allow themselves to be misled by a negative report, believing that more definitive testing is unnecessary. This is particularly true regarding cranial CTs. We forget, however, that CT cannot substitute for examining the spinal fluid. Each year, for example, I come across patients in whom the cranial CT is normal but the lumbar puncture yields findings diagnostic of a specific disorder. In that group are 3 to 4 patients with active central nervous system syphilis, 2 to 3 with subarachnoid hemorrhage, many with various forms of meningitis, and several with other types of intracranial or intraspinal disease.
We should remember, too, that CT cannot provide histologic evidence. In fact, it was never designed to do so. Yet, I continue to see CT reports—especially when the head is scanned—that conclude with precise diagnoses, such as “metastases,” “infarct,” and “toxoplasmosis.” Because CT is such a powerful diagnostic tool, physicians tend to accept these reports as gospel. Nevertheless, these “imaging diagnoses” are sometimes wrong. Reports of this sort do more to boost tunnel vision than to enhance patient care.
What Should Be Done?
Computed tomography is a magnificent diagnostic procedure. Its indiscriminate use, however, is rampant and may be doing more harm than good. What, then, should we do about this situation?
First, all health-care professionals should use CT only when no other test or procedure can supply the information needed. Second, all radiologists, particularly those who deal with children, should strive to reduce the radiation dose in each patient to the lowest level capable of yielding acceptable image quality. They should also question the use of CT when the indications do not seem appropriate. Finally, the faculty of every medical school should bring these issues to the attention of students and house officers.
Coda
The good doctor knows what to do and when to do it. But the very good doctor knows what not to do and when not to do it. In that light, I hope you will think twice before ordering your next CT scan.
Footnotes
Address for reprints: Herbert L. Fred, MD, Department of Internal Medicine, 8181 Fannin, Suite 316, The University of Texas Health Science Center at Houston, Houston, TX 77054
References
- 1.Fred HL. The tyranny of technology. Hosp Pract (Off Ed) 1997;32:17–8, 21. [DOI] [PubMed]
- 2.Renston JP, Connors AF Jr, DiMarco AF. Survey of physicians' attitudes about risks and benefits of chest computed tomography. South Med J 1996;89:1067–73. [DOI] [PubMed]
- 3.Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors' knowledge of radiation exposure: questionnaire study. BMJ 2003;327:371–2. [DOI] [PMC free article] [PubMed]
- 4.Wiest PW, Locken JA, Heintz PH, Mettler FA Jr. CT scanning: a major source of radiation exposure. Semin Ultrasound CT MR 2002;23:402–10. [DOI] [PubMed]
- 5.National Council on Radiation Protection and Measurements. Exposure of the population in the United States and Canada from natural background radiation, NCRP Report No. 94. Bethesda (MD): The Council; 1987. p. 148.
- 6.Golding SJ, Shrimpton PC. Commentary. Radiation dose in CT: are we meeting the challenge? Br J Radiol 2002;75: 1–4. [DOI] [PubMed]
- 7.Berrington de Gonzalez A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 2004;363:345–51. [DOI] [PubMed]
- 8.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176:289–96. [DOI] [PubMed]
- 9.Shrimpton PC, Edyvean S. CT scanner dosimetry. Br J Radiol 1998;71:1–3. [DOI] [PubMed]
- 10.Frush DP. Review of radiation issues for computed tomography. Semin Ultrasound CT MR 2004;25:17–24. [DOI] [PubMed]
- 11.Slovis TL. ALARA conference proceedings: the ALARA concept in pediatric CT intelligent dose reduction [panel discussion]. Pediatr Radiol 2002;32:242–4. [DOI] [PubMed]
- 12.Slovis TL, Hall ET, Huda W, Frush D. ALARA conference proceedings: the ALARA concept in pediatric CT intelligent dose reduction [executive summary]. Pediatr Radiol 2002;32:221.
- 13.Schattner A, Fletcher RH. Pearls and pitfalls in patient care: need to revive traditional clinical values. Am J Med Sci 2004; 327:79–85. [DOI] [PubMed]


