Abstract
What has been accomplished does not die, but too often, alas, the personality of those who have handed the torch from one generation to another soon fades into oblivion.
— Harvey Williams Cushing (1869–1939)1
Vasilii I. Kolesov (1904–1992) was one of the pioneers of cardiovascular surgery. He is often referred to as the surgeon who performed the first successful coronary artery bypass operation. Kolesov was the first to successfully apply the suture technique to clinical coronary artery bypass surgery. He was also the first—and remains the only— surgeon to use coronary stapling clinically. Recent rapid development in robotic and video-assisted coronary surgery has revived interest in Kolesov's original work on coronary stapling and off-pump coronary surgery. However, little is known about the personality of Dr. Kolesov, his early work that led to his pioneering effort, and the circumstances under which his work was done.
Key words: Cardiac surgical procedures/history; history of medicine, 20th cent.; internal mammary-coronary artery anastomosis;; myocardial revascularization/history; portraits; thoracic arteries/transplantation
The development of the coronary artery bypass grafting (CABG) operation is undoubtedly one of the greatest surgical achievements of the 20th century. Millions of patients have undergone CABG since it was introduced into clinical practice in the 1960s. Since 1964, CABG has been performed regularly and the number of procedures has increased dramatically. During the last 40 years, the CABG operation became one of the most successful and most frequently performed surgical procedures. Yet it should be remembered that from 25 February 1964 to 9 May 1967 the department of surgery headed by Vasilii I. Kolesov was the only place in the world where CABG operations were performed.2,3 Furthermore, Kolesov's contributions are not merely of historical interest. Recent rapid advances in robotic and video-assisted CABG have revived interest in coronary artery stapling and off-pump surgery.4 Today, much could be learned from Kolesov's early work, and variations on the original stapling technique that he used 40 years ago may find new application in modern coronary surgery.5 Herein the personality of the man behind the first CABG operations, his ideas, and the pioneering effort of his team are described.
Landmarks of Myocardial Revascularization before Kolesov
The internal thoracic artery (ITA) was the first conduit used for clinical myocardial revascularization. It was applied experimentally as early as 1945 by the Canadian surgeon Arthur Vineberg.6 Instead of being anastomosed to a coronary artery, however, it was implanted directly into the myocardium. This procedure is referred to as the Vineberg operation.
In the early 1950s, many surgeons attempted to experimentally anastomose the ITA to the coronary artery. The first successes were achieved independently and almost simultaneously by Vladimir P. Demikhov in Russia7,8 and Gordon Murray in Canada.9
On 29 July 1953, Demikhov performed his first successful experimental coronary artery bypass surgery, using a Payr cannula. Four dogs survived more than 2 years, and patency was demonstrated in each.7,8 Demikhov published his results in Russian surgical journals and in his monograph of 1960.7 Kolesov became aware of Demikhov's work in the late 1950s. During the late 1950s, Robert H. Goetz, independently of Demikhov, began his experiments in New York. Goetz also used a modified Payr technique. On 2 May 1960, Goetz performed the world's first successful clinical coronary artery bypass operation and reported it in 1961 in an addendum to his experimental study on dogs.10 Goetz used a tantalum ring to create an almost instantaneous ITA-to-coronary artery anastomosis.10,11 Goetz never again repeated clinical CABG.11 In 1962, Pronin performed successful CABG on dogs using a suture technique and continuous autoperfusion, so that coronary blood flow was maintained uninterrupted during creation of the anastomosis.12 Kolesov was well aware of the work of his predecessors on direct coronary revascularization and gave credit to Demikhov, Murray, Goetz, and Pronin in his first article reporting successful clinical CABG.13
Biographical Notes
In order to fully appreciate an individual's work, it is important not only to have a good idea of what had been accomplished beforehand, but also to learn about the personality of the one who took up the work where others left it. Who was Vasilii I. Kolesov? What compelled him to go into surgery and make clinical off-pump CABG a reality? What helped him to stay focused despite the adversity he endured? It is hoped that this paper will reveal facts not yet known to most surgeons and contributions not adequately acknowledged.
Vasilii Ivanovich Kolesov was born on 24 September 1904 in the small village of Marthianovskaia, in the Vologda province of Russia. His parents were well-to-do farmers, Maria K. and Ivan N. Kolesov. He had 3 brothers and 2 sisters. Kolesov left home to study medicine in Leningrad. The city of St. Petersburg, where Kolesov studied and worked, changed its name several times (St. Petersburg, 1703–1914; Petrograd, 1914–1924; Leningrad, 1924–1992) and is referred to here by the name it bore during the time period under discussion. Upon graduation from the Leningrad Medical Institute in 1931, Kolesov received an appointment as a physician at a large metallurgic factory in the town of Chusovoi, Perm province, in the Ural Mountains. Here Kolesov met his wife to be, Ettel I. Kerstein (1904–1994), who was a recent medical graduate in obstetrics and gynecology. During this time, his parents endured forced “collectivization,” lost their farm, and were obliged to move to Chusovoi, where they shared the young couple's home. On 15 June 1935, Kolesov's son, Evgenii, was born.
From 1934 to 1938, Kolesov undertook training in general surgery at the department of surgery headed by Professor Vasilii N. Parin (1877–1947). It was Parin who fueled Kolesov's interest in academic surgery.14 Kolesov cherished the memories of his surgical training all his life and later published biographical articles on Professor Parin.14,15 Under the supervision of Parin, Kolesov completed his experimental project for his “candidate” thesis (the equivalent of a master's thesis) titled “On eventration of spleen into the abdominal wound.” In 1938, Kolesov defended his thesis, became an assistant professor at the Institute of Post-Graduate Medical Studies in Leningrad, and moved to that city with his family (Fig. 1). There, Kolesov began his studies on the use of bacteriophages in infected wounds. He planned to defend his doctor of medical sciences thesis (the equivalent of a doctoral dissertation), and the future of his family seemed secure. But World War II interfered with his plans.

Fig. 1 Dr. Vasilii I. Kolesov with his wife and son, Evgenii, in 1940. (Courtesy of Dr. Evgenii V. Kolesov)
After Nazi troops invaded the Soviet Union in 1941, Kolesov was given the rank of major in the Medical Corps of the Army and was appointed surgeon-in-chief to one of the municipal hospitals. The hospital was in the heart of the city, in the spacious building of the former German Embassy (Fig. 2A). Less than 2 months after the Soviet Union was attacked, Nazi troops were rapidly approaching Leningrad, a city of 3 million people. An emergency evacuation of the civilian population began. Kolesov's wife and son were able to escape to Chusovoi just a few days before the siege of the city.
Kolesov and the Siege
On 8 September 1941, Leningrad was surrounded by German troops and effectively shut off from the rest of Russia. The siege of the city began. By that time, the Nazis occupied almost all of Europe. The German war machine was nearly overwhelming. While France withstood the Nazis for only 42 days before surrendering, the people of Leningrad endured starvation, cold, and almost daily bombardments for 872 days and never surrendered. Kolesov was among them. His brother Nikolai lived in the suburbs but worked in the city. One day, as the Germans advanced, Nikolai found himself cut off from the rest of his family and went to live with his brother. Thus, Vasilii shared a room with his brother in the basement of his hospital. Their sister Polina and 2 of her children did not have time to escape and remained in the besieged city as well.
The shining golden cupola of St. Isaac's Cathedral (Fig. 2A) was visible from the heights occupied by Nazi troops and provided an excellent target for long-range artillery. Thus, good weather in the autumn of 1941 meant relentless shelling of St. Isaac's Square and the disruption of Kolesov's work. The Russian air force was almost completely destroyed during the first months of the war. In a desperate attempt to protect Kolesov's hospital and the central part of the city from German planes that approached at low altitude, the defenders deployed giant barrage balloons (Fig. 2A) in the sky to impede aerial maneuvers during the merciless raids.
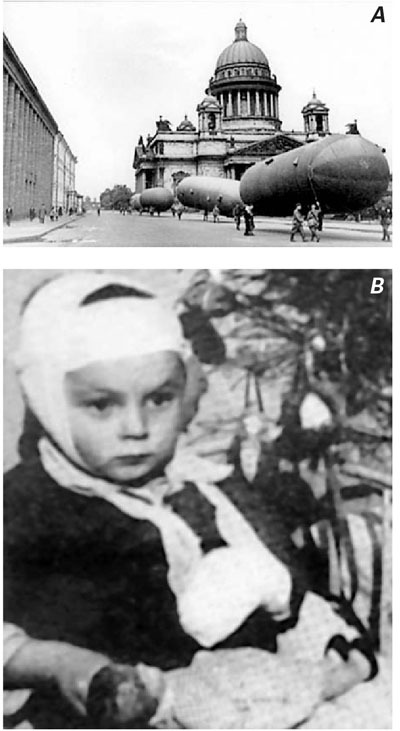
Fig. 2 A) Barrage balloons prior to deployment during the siege of Leningrad in 1941. St. Isaac's Cathedral is in the background, and Kolesov's hospital is the dark-walled building on the left. B) One of the patients operated on during the siege. A decorated Christmas tree appears in the background. (Courtesy of the Military Medical Museum, St. Petersburg, Russia)
Emergent surgery had to be performed no matter what, so Kolesov and his coworkers took their chances. Elective surgery was done at night. Once during a surgery, a bomb exploded in the back yard of the hospital. The windows in the operating room were blown out, and a fragment of the shell flew above the operating table, missing Kolesov's head by only a few inches. Another fragment ricocheted into the ceiling, sending dust and rubble into the open wound. All Kolesov could do was to lean over the wound so that the rubble from the ceiling fell on his back instead. In December 1941, the situation became even more desperate. Nevertheless, Christmas trees were decorated in all hospitals (Fig. 2B), and young patients were given gifts, though often no more than a piece of sugar and a rag doll. In January 1942, in the depths of an unusually cold winter, the city's daily food rations reached an all-time low of only 150 g of “bread,” a black mixture of flour and sawdust. In just 2 months, January and February of 1942, 200,000 people died in Leningrad of cold and starvation. The rations at the hospital were better, yet hardly sufficient for normal wound recovery. Wounds took months to heal. Often lacking antibiotics, Kolesov tried to prevent infection by maintaining pristine cleanliness in the operating room and by thorough hand washing. It was then that his previous studies on bacteriophagia became handy. Using bacteriophages, Kolesov managed to clean many infected wounds. Ever-industrious doctors were making a beverage from spruce twigs, to prevent scurvy in their starving patients.
Kolesov and his brother felt responsible for Polina and her children and saved rations to share with them. As the siege continued, the brothers grew weaker every day. Soon Nikolai became too weak to move. Despite Vasilii's care, Nikolai soon died. During this time, Kolesov developed effusive pericarditis and could barely walk a few steps before the onset of severe shortness of breath. Kolesov himself became a patient and was bedridden; however, in a few days he felt somewhat better and resumed his duties (Fig. 3). Kolesov lost contact with his sister during this time. He rushed to see her at the first opportunity, only to learn that his nephew and niece had died of starvation. At least 641,000 people died of starvation alone during the siege, bringing the total number of dead close to 1 million. On 27 January 1944, the siege ended and Kolesov soon reunited with his wife and son. Evgenii Kolesov* recalls that when he saw his father in July 1944 for the first time after the siege, “he was still very thin, but nonetheless very energetic.”

Fig. 3 Dr. Vasilii I. Kolesov, a surgeon-in-chief of the hospital in Leningrad in 1943, in the uniform of a major of the Medical Corps of the Army. (Courtesy of Dr. Evgenii V. Kolesov)
The Path to Cardiac Surgery
In January 1945, Kolesov's hospital unit was transferred to Poland, to follow the advancing Red Army. His wife and son bade their farewells and returned home upset, expecting yet another long separation. However, early the following morning Kolesov returned home. At the very last moment, after Kolesov had boarded the train, he was recalled by Professor Petr A. Kupriianov (1893–1963), who was in the midst of gathering staff for a new department of cardiovascular surgery at the Military Medical Academy. Thus, unexpectedly, Kolesov started on the path to academic cardiovascular surgery.
In 1946, Kolesov at last defended his doctor of medical sciences thesis (which defense had been postponed by the war) titled “Bacteriologic control and bacteriophage therapy in purulent wounds.” Kolesov worked at the Military Medical Academy until 1950. He later credited Professor Kupriianov as his teacher of cardiac surgery.16 Then for 2 years, Kolesov served a dual appointment as surgeon-in-chief to the Central Military Group (Soviet troops in Hungary and Austria) and as the chairman of military surgery in Kharkov, Ukraine. In 1953, he left the military service with the rank of colonel of the Medical Corps and became chairman of the Department of Surgery at the First Leningrad Medical Institute. Kolesov headed this department until 1976. After the war, he summarized his experience in treating combat injuries17,18 and wrote a few articles on the history of surgery.14,16,19
The Beginning of Coronary Bypass Surgery
A recent study of men who had undergone severe starvation and chronic stress during the siege of Leningrad found that those who experienced the siege at around the age of puberty tended, 3 to 6 decades later, to display higher blood pressure and to die at higher rates from ischemic heart disease and stroke.20 Although there has been no comparable study of women, a likely guess is that the incidence of cardiovascular disease among both sexes was abnormally high in Leningrad during the postwar years, when Kolesov maintained his surgical practice there.
In the mid-1950s, Kolesov became aware of the experimental work of Demikhov, who successfully performed ITA-to-coronary artery end-to-end anastomoses in dogs using a vascular stapler.7,8 However, Kolesov's own initial work was discouraging. A few minutes of coronary occlusion in dogs caused irreversible ventricular fibrillation. Both the coronary suture and the stapling techniques required experimental refinement. In the meantime, Kolesov began to ligate the ITA bilaterally in an attempt to treat coronary insufficiency in his patients21–23 and performed Vineberg's operation.24 In 1963, Kolesov (Fig. 4) became aware of successful experimental work by Pronin, who used a collapsible cannula (Fig. 5A) in dogs to provide continuous blood flow into a coronary artery while the suture anastomosis was created.12 Kolesov successfully tried this technique in dogs,13 and constructed an instrument for application of the principle of continuous, coronary autoperfusion (Fig. 5B).25 Using a modified collapsible cannula, Kolesov was able to create an anastomosis between the ITA and a coronary artery without interruption of coronary blood flow.13,25 Eight dogs underwent follow-up for as long as 19 months, and the patency of the anastomosis was demonstrated in all animals.13,25 On 25 February 1964, Kolesov performed the first successful clinical CABG, using a suture technique.13 Kolesov noticed that chronically ischemic human myocardium was much more resistant to coronary occlusion than that of dogs and did not require continuous autoperfusion. Kolesov used specially designed precise scissors and magnifying glasses to open the coronary arteries.25 The era of modern coronary surgery had begun.

Fig. 4 Dr. Vasilii I. Kolesov in the 1960s, during the time when his first coronary bypass operations were performed. (Courtesy of Dr. Evgenii V. Kolesov)
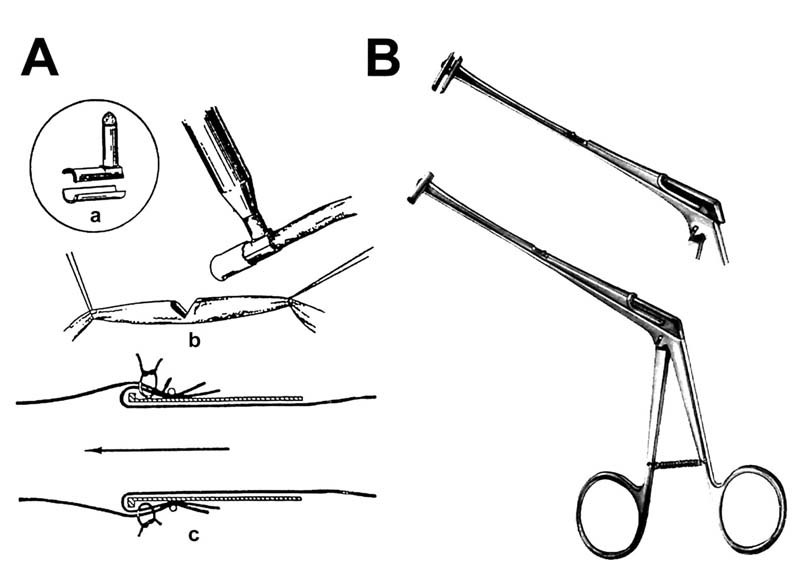
Fig. 5 A) Pronin's collapsible cannula for continuous coronary autoperfusion during surgery. The collapsible cannula (a) is used to hold the internal thoracic artery and introduce it into the coronary artery (b), so that the coronary blood flow is continuously maintained while the suture anastomosis is being created (c). (From: Pronin VI et al.12) B) Kolesov's instrument to apply the principle of continuous coronary autoperfusion to coronary bypass surgery. (From: Kolesov VI.25 With permission from the American Association for Thoracic Surgery.)
Acceptance of Coronary Bypass Surgery
Soon Kolesov published his first early follow-up results26 and his first book on direct coronary revascularization.27 Although the early results were most encouraging, Kolesov's innovations were not accepted easily. The unknown often creates anxiety, and anxiety often creates resistance. However, such an attitude was not unique to Kolesov's work: Drs. Robert H. Goetz and René G. Favaloro also faced criticism from their more conservative colleagues.11,28 When Kolesov's initial experience was first published in English in 1967, it was accompanied by the following editorial foreword: “The opinions concerning the management and surgical treatment of angina pectoris as expressed in this paper by Professor V.I. Kolesov are at variance with the concepts of many surgeons in the United States.”25 Ironically, the initial attitude toward his work was even worse in his home country. In June of 1967, Kolesov presented the results of the ITA-to-coronary artery grafting at the meeting of the Cardiology Society in Leningrad. The plenum of the Society accepted the following resolution: “the surgical treatment of coronary artery disease is impossible and has not prospects for the future.”2,29
Kolesov appreciated the importance of coronary angiography and conducted an investigation of the method.30 In Surgical Treatment of Coronary Disease of the Heart, edited by Kolesov and published in 1966, there is a chapter describing the angiographic method in much detail.27 By the late 1960s, most CABG patients underwent preoperative coronary angiography and subsequently underwent long-term evaluation of the anastomoses.31
Off-Pump CABG
Kolesov advocated the use of off-pump CABG. In the early 1960s, Kolesov conducted a study of artificial circulation. He concluded that while cardiopulmonary bypass is safe and reliable for use during open heart surgery, the global inflammatory response following the extracorporeal circulation is too great to justify its use for CABG.32 By the end of the 1960s, the extracorporeal circulation technique was as well established in Kolesov's clinic as anywhere else in the world. In the late 1960s, Kolesov's team undertook one of the earliest experimental studies of mitral valve homotransplantation33 with the support of extracorporeal circulation. The heart-lung machine was used routinely for intracardiac correction of congenital heart defects (Fig. 6) and for valvular surgery.34 Nonetheless, Kolesov continued to perform CABG without extracorporeal circulation, believing in the superiority of the off-pump technique;29 only 18% of his CABG procedures were done on pump from 1964 to 1974.*

Fig. 6 Dr. Vasilii I. Kolesov closes a ventricular septal defect in a child in 1965. The operation is performed with support of the first Soviet bubble oxygenator (seen in the upper left-hand corner) constructed by Drs. F.V. Baliuzek and N.I. Ermilov at the Military Medical Academy in Leningrad in the late 1950s. Drs. A.O. Levin and L.V. Potashov assist, Dr. G.L. Kotomina gives anesthesia, and Drs. S.M. Pudiakov and E.V. Kolesov (wearing glasses) observe. (Courtesy of Dr. Evgenii V. Kolesov)
Coronary Staplers
Kolesov's team was the first—and remains the only—to use coronary stapling clinically. The first coronary stapling device, called the “vascular circular stapling apparatus” (VCA), underwent several modifications.5,35 Its earliest prototype, the VCA-4, was first applied to clinical surgery on 22 March 1967, when Kolesov constructed an end-to-end anastomosis between the left ITA and the left anterior descending coronary artery in a 52-year-old man with class IV angina pectoris. Three years later, the patient remained free of angina.2,35 A modification of the stapler with elongated bushing (Fig. 7A) and vacuum suction (U.S. patent 4,350,160; 21 September 1982), to hold the ITA wall while the stapling was performed, produced good results (Fig. 7B).4,5,29
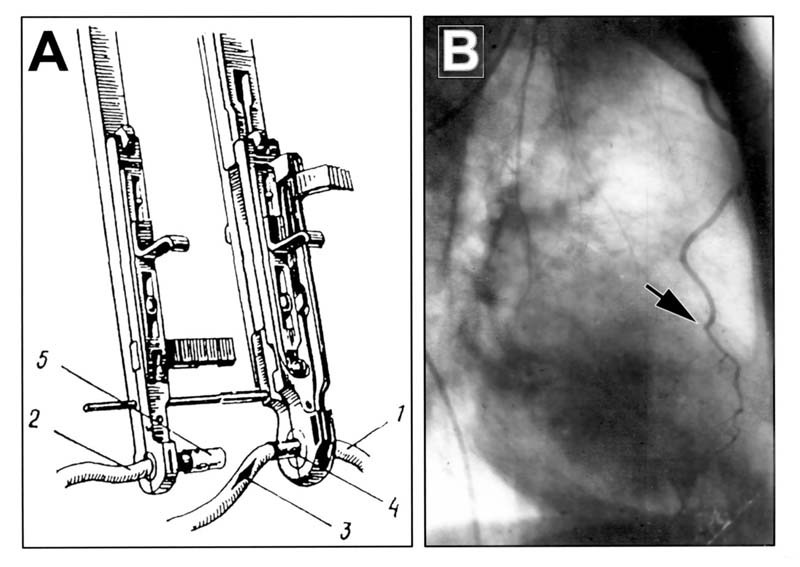
Fig. 7 A) The vascular circular stapler with elongated bushing that was used by V.I. and E.V. Kolesov in coronary surgery. 1 = coronary artery; 2 = internal thoracic artery; 3 = incision in the coronary artery; 4 = bushing; 5 = elongated bushing. (From: Kolesov VI.29) B) Angiogram done in the late 1960s, 3 years and 7 months after surgery, demonstrating a patent end-to-end anastomosis (arrow) that had been made by a vacuum-facilitated stapler. (Courtesy of Dr. Evgenii V. Kolesov. From Konstantinov IE.5 With permission from the American Association for Thoracic Surgery.)
Venous versus Arterial Grafts
On 9 May 1967, at the Cleveland Clinic, René G. Favaloro performed the first CABG in which a saphenous vein was used as the graft (SVG).36 In April 1971, Donald B. Effler and colleagues, reporting on CABG with SVGs, mentioned the work of Kolesov on the ITA and commented on the use of the ITA graft: “This is an interesting and practical possibility, and it has been used to a very limited degree by the Cleveland Clinic team. This can be a useful revascularization tool in carefully selected cases, but it hardly constitutes simple surgery.”37 For a few years, the explosive development and success of CABG using the SVG by the Cleveland Clinic team28 overshadowed Kolesov's initial work on the ITA graft.
Kolesov continued to believe in the advantages of all-arterial CABG and explored the possibility of using the arteries of the abdominal cavity as bypass conduits.38,39 It was only during the mid-1980s that the advantage of arterial grafts in terms of superior long-term patency was first appreciated. Kolesov diligently continued his work, remaining a compassionate physician and an enthusiastic research scientist. There were 2 striking features about Kolesov that his colleagues noticed. First, Kolesov always took time to listen to what his patients had to say, despite being very busy with his clinical and research work. He stood in front of each patient in his typical pose, holding his hands together and listening thoroughly to every word (Fig. 8A). His every patient was dear to him. Second, Kolesov took an extra long time to wash his hands meticulously, a habit he had acquired during the war (Fig. 8B).
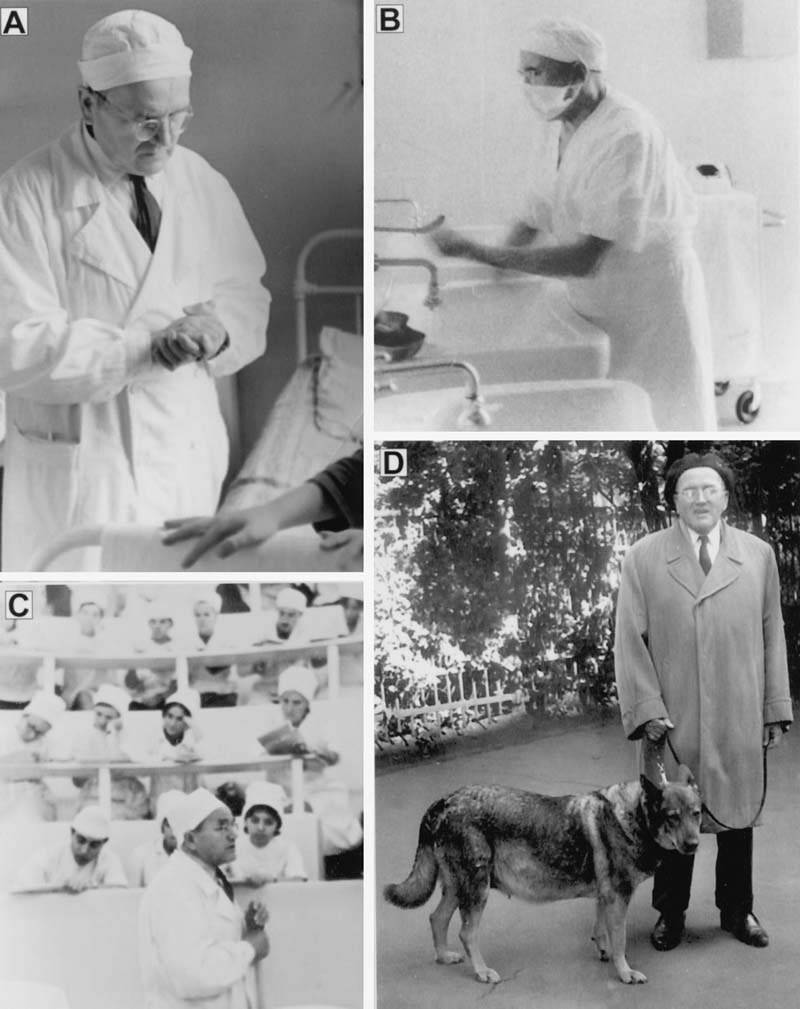
Fig. 8 Dr. Vasilii I. Kolesov A) talks to a patient, B) scrubs his hands before surgery, C) lectures to medical students in the late 1970s, and D) takes a walk with his dog in the late 1970s. (Courtesy of Dr. Evgenii V. Kolesov)
International Visitors
The progress made by Kolesov's team in the 1960s drew international attention. Several visitors came to see Kolesov's department and left notes in the guest book from 1965 to 1975, including Drs. Earl B. Kay, René G. Favaloro, Denton A. Cooley, Vincent M. Dor, Gordon K. Danielson, and Joseph J. Verska, and Mr. John V. Lindsay (mayor of New York, 1966–1973). However, the full significance of Kolesov's innovations was yet to be appreciated.
Kolesov's department was very poorly equipped according to American standards.* It should be remembered, however, that the Soviet Union had suffered unspeakable devastation and had lost some 27 million people during World War II. While the United States emerged from World War II in justifiable grief for the 450,000 men and women it had lost in combat, no bomb had fallen on the continental United States, and the war itself lifted the country out of the Depression. During the siege of Leningrad alone, the Soviet Union lost twice as many people as all American casualties combined. These facts, perhaps, are of little interest from the surgical point of view, yet they provide a proper appreciation of the scale of Kolesov's postwar work and of the circumstances under which it was performed.
Long-Term Results of Coronary Bypass Surgery
In the late 1970s, Kolesov's reported angiographic evaluations of CABG demonstrated an excellent patency rate31 and functional results.40 Upon his retirement in 1976, Kolesov published a monograph devoted entirely to CABG.29 After retirement, he continued his long-term follow-up studies,41 lectured to medical students (Fig. 8C), and enjoyed going for long walks with his dog (Fig. 8D) and meeting with friends.42 In the mid-1980s, the superior patency rate of ITA grafts compared with SVG grafts,43 together with the improved survival rate of patients who had received ITA grafts versus those who had received only SVGs,44 were demonstrated. In 1988, Effler wrote: “In retrospect, some might say that the Kolesov team in Leningrad acted prematurely because surgical treatment preceded accurate diagnosis (coronary arteriography). In my opinion, this is not the case. The Kolesov saga deserves the recognition of all who are interested in the surgical treatment of coronary artery disease.”45 Kolesov remained active and published his last paper 1 year before his death.46 Kolesov died on 2 August 1992.
Epilogue
Today, CABG is one of the most frequently performed operations in the world. The patency of arterial grafts is superior to that of venous grafts. The ITA is the graft of choice. Off-pump CABG has important advantages over the on-pump technique, and rapid advances in robotic surgery have revived an interest in coronary stapling. Who could have foreseen all of this 40 years ago? Perhaps Kolesov was one of the few. Kolesov started the era of modern coronary surgery, and his contributions to the field cannot be overemphasized. Yet, I often wonder when his service to humanity was greatest. Was it when he developed coronary bypass surgery? Or was it when he gave a beverage made of spruce twigs to prevent scurvy in an emaciated patient who never made it through the war?
Acknowledgments
I am very grateful to Dr. Evgenii V. Kolesov for providing me with original photographs and recollecting some facts from his father's life that made this paper historically accurate. I am also grateful to Drs. Dmitri D. Tcherkas and Andrew S. Olearchyk for their kind encouragement and most valuable suggestions.
Footnotes
*Oral and written communications, 2004.
*E.V. Kolesov, oral and written communications, 2004.
*D.A. Cooley, written communication, 2004; G.K. Danielson, oral communication, 1999, and written communication, 2004; V.M. Dor, written communication, 2004; R.G. Favaloro, written communication, 1996; J.J. Verska, oral communication, 2004.
Address for reprints: Igor E. Konstantinov, MD, Division of Cardiovascular Surgery, Hospital for Sick Children, 555 University Avenue, Toronto M5G 1X8, Canada
E-mail: igorkonst@hotmail.com
References
- 1.Fulton JF. Harvey Cushing. A Biography. The story of a great medical pioneer. New York: Blackwell Scientific, 1946, p. 609.
- 2.Olearchyk AS. Vasilii I. Kolesov. A pioneer of coronary revascularization by internal mammary-coronary artery grafting. J Thorac Cardiovasc Surg 1988;96:13–8. [PubMed]
- 3.Konstantinov IE. The last word on “a proper name for the internal mammary artery”? Ann Thorac Surg 1999;68:1440–1. [DOI] [PubMed]
- 4.Konstantinov IE. Circular vascular stapling in coronary surgery. Ann Thorac Surg 2004;78:369–73. [DOI] [PubMed]
- 5.Konstantinov IE. The return of the coronary stapler: will a new technique overcome an old obstacle? J Thorac Cardiovasc Surg 2004;128:330–1. [DOI] [PubMed]
- 6.Vineberg AM. Development of anastomosis between coronary vessels and transplanted internal mammary artery. Can Med Assoc J 1945;55:117–9. [PubMed]
- 7.Demikhov VP. Transplantation of vital organs in experiments. Moscow: Medgiz; 1960.
- 8.Demikhov VP. Experimental transplantation of vital organs. Authorized translation from the Russian by Basil Haigh. New York: Consultant's Bureau; 1962.
- 9.Murray G, Hilario J, Porcheron R, Roschlau W. Surgery of coronary heart disease. Angiology 1953;4:526–31. [DOI] [PubMed]
- 10.Goetz RH, Rohman M, Haller JD, Dee R, Rosenak SS. Internal mammary-coronary artery anastomosis. A nonsuture method employing tantalum rings. J Thorac Cardiovasc Surg 1961;41:378–86. [PubMed]
- 11.Konstantinov IE. Robert H. Goetz: the surgeon who performed the first successful clinical coronary artery bypass operation. Ann Thorac Surg 2000;69:1966–72. [DOI] [PubMed]
- 12.Pronin VI, Dobrova NB, Kurilovich JB. Revascularization of the heart by the method of anastomosis of the left thoracic and coronary arteries [in Russian]. Grudn Khir 1963; 5:81–6. [PubMed]
- 13.Kolesov VI, Potashov LV. Surgery of coronary arteries [in Russian]. Eksp Khir Anesteziol 1965;10:3–8. [PubMed]
- 14.Kolesov VI. Vasilii Nikolaevich Parin (1877–1947). Khirurgiia (Mosk.) 1958;34:135–8. [PubMed]
- 15.Kolesov VI. 100th anniversary of the birth of V.N. Parin [in Russian]. Vestn Khir Im I I Grek 1978;120:141–2. [PubMed]
- 16.Kolesov VI. P.A. Kupriianov – surgeon and scientist [in Russian]. Khirurgiia (Mosk.) 1963;39:3–8. [PubMed]
- 17.Kolesov VI, Makarova EN, Saraeva AN. Rational utilization of antibiotics and bacteriolytic control during the treatment of infected wounds [in Russian]. Vestn Khir Im I I Grek 1957;78:13–21. [PubMed]
- 18.Kolesov VI. Chronic pulmonary suppurations following gunshot wounds [in Russian]. Khirurgiia (Mosk) 1952;69:32–8. [PubMed]
- 19.Kolesov VI. Surgical schools of Petersburg-Petrograd-Leningrad; 250th anniversary of the city [in Russian]. Vestn Khir Im I I Grek 1957;78:7–14. [PubMed]
- 20.Sparen P, Vagero D, Shestov DB, Plavinskaja S, Parfenova N, Hoptiar V, et al. Long term mortality after severe starvation during the siege of Leningrad: prospective cohort study. BMJ 2004;328:11. [DOI] [PMC free article] [PubMed]
- 21.Kolesov VI, Vishneevskaia IaN, Drevina AI, Tsalolikhina EIa. Treatment of coronary insufficiency by bilateral ligation of the internal mammary artery [in Russian]. Vestn Khir Im I I Grek 1959;82:33–41. [PubMed]
- 22.Kolesov VI. The physiological features and results of treatment of chronic coronary insufficiency with bilateral ligation of the internal mammary artery [in Russian]. Klin Med (Mosk) 1960;38:71–7. [PubMed]
- 23.Kolesov VI. Ligation of the internal mammary arteries in the treatment of angina pectoris. Bull Soc Int Chir 1962;21:684–90. [PubMed]
- 24.Kolesov VI. Results of surgical treatment of stenocardia and acute myocardial infarct [in Russian]. Vestn Khir Im I I Grek 1963;90:87–95. [PubMed]
- 25.Kolessov VI. Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Thorac Cardiovasc Surg 1967;54:535–44. [PubMed]
- 26.Kolesov VI. Coronary-thoracic artery anastomosis as a means of treating coronary heart disease [in Russian]. Klin Med (Mosk.) 1966;44:7–12. [PubMed]
- 27.Kolesov VI, editor. Surgical treatment of coronary disease of the heart. Leningrad: Meditsina; 1966.
- 28.Favaloro RG. The challenging dream of heart surgery: from the Pampas to Cleveland. Boston: Little Brown; 1994.
- 29.Kolesov VI. The surgery of coronary arteries of the heart. Leningrad: Meditsina; 1977.
- 30.Kolesov VI, Potashov LV, Figurina TD, Volodkovich NG, Vasilchuk IV. Coronary arteriography in cardioplegia and subsequent electrostimulation of the heart. Cor Vasa 1966; 8:252–8. [PubMed]
- 31.Kolesov VI. Angiographic evaluation of the results of the surgical treatment of ischemic heart disease [in Russian]. Grudn Khir 1978;6:31–8. [PubMed]
- 32.Kolesov VI, Levin AO, Vinogradov AG, Danilova LD. On changes of morphological and functional properties of the blood and hemodynamics during the use of the NIIEKHAII (AIK-59) and Baliuzek's (ISL-2) artificial circulation apparatus [in Russian]. Grudn Khir 1963;49:34–40. [PubMed]
- 33.Kolesov VI, Vinogradov AG, Gel'fond ML, Krasnorogov VB, Fishbukh AA, Sizov MG. Homotransplantation of the mitral valve of the heart [in Russian]. Grudn Khir 1970;12: 13–6. [PubMed]
- 34.Kolesov VI, Vinogradov AG, Kolesov EV. Surgical correction of mitral valve insufficiency [in Russian]. Grudn Khir 1975;5:7–11. [PubMed]
- 35.Kolesov VI, Kolesov EV, Gurevich IY, Leosko VA. Vasosuturing apparatuses in surgery of coronary arteries [in Russian]. Med Tekh 1970;6:24–8.
- 36.Favaloro RG. Saphenous vein autograft replacement of severe segmental coronary artery occlusion: operative technique. Ann Thorac Surg 1968;5:334–9. [DOI] [PubMed]
- 37.Effler DB, Favaloro RG, Groves LK, Loop FD. The simple approach to direct coronary artery surgery. Cleveland Clinic experience. J Thorac Cardiovasc Surg 1971;62:503–10. [PubMed]
- 38.Kolesov VI, Romankova MP, Drozdova MM, Sidorov AM. Revascularization of the myocardium by implanting arteries of the abdominal cavity [in Russian]. Vestn Khir Im I I Grek 1971;106:43–8. [PubMed]
- 39.Kolesov VI, Romankova MP, Volodkovich NG, Dulaev VK. Experimental study of coronary-splenic arterial anastomosis with the aim of myocardial revascularization [in Russian]. Vestn Khir Im I I Grek 1975;114:9–14. [PubMed]
- 40.Kolesov VI. Remote results of direct myocardial revascularization in atherosclerosis of coronary arteries [in Russian]. Khirurgiia (Mosk) 1977;7:17–21. [PubMed]
- 41.Kolesov VI. Late results of a mammary-coronary anastomosis [in Russian]. Vestn Khir Im I I Grek 1982;128:49–53. [PubMed]
- 42.Olearchyk AS, Olearchyk RM. Reminiscences of Vasilii I. Kolesov. Ann Thorac Surg 1999;67:273–6. [DOI] [PubMed]
- 43.Olearchyk AS, Magovern GJ. Internal mammary artery grafting. Clinical results, patency rates, and long-term survival in 833 patients. J Thorac Cardiovasc Surg 1986;92:1082–7. [PubMed]
- 44.Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1–6. [DOI] [PubMed]
- 45.Effler DB. Vasilii I. Kolesov: pioneer in coronary revascularization [letter]. J Thorac Cardiovasc Surg 1988;96:183. [PubMed]
- 46.Kolesov VI, Kolesov EV. Twenty years' results with internal thoracic artery-coronary artery anastomosis [letter]. J Thorac Cardiovasc Surg 1991;101:360–1. [PubMed]


