Abstract
Objective To determine whether atrial fibrillation is a stronger risk factor for cardiovascular disease and death in women compared with men.
Design Meta-analysis of cohort studies.
Data sources Studies published between January 1966 and March 2015, identified through a systematic search of Medline and Embase and review of references.
Eligibility for selecting studies Cohort studies with a minimum of 50 participants with and 50 without atrial fibrillation that reported sex specific associations between atrial fibrillation and all cause mortality, cardiovascular mortality, stroke, cardiac events (cardiac death and non-fatal myocardial infarction), and heart failure.
Data extraction Two independent reviewers extracted study characteristics and maximally adjusted sex specific relative risks. Inverse variance weighted random effects meta-analysis was used to pool sex specific relative risks and their ratio.
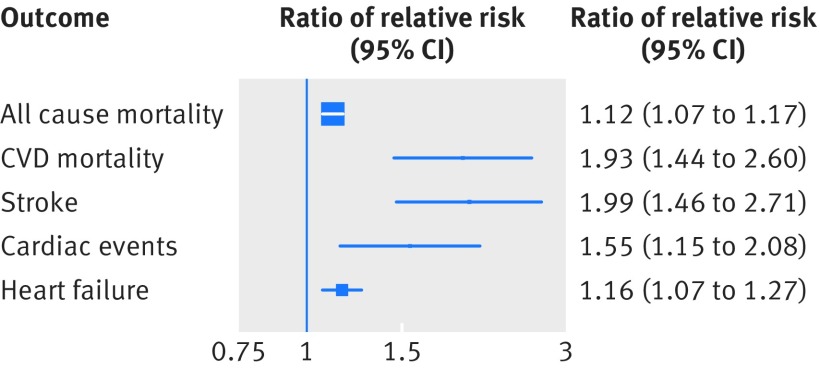
Results 30 studies with 4 371 714 participants were identified. Atrial fibrillation was associated with a higher risk of all cause mortality in women (ratio of relative risks for women compared with men 1.12, 95% confidence interval 1.07 to 1.17) and a significantly stronger risk of stroke (1.99, 1.46 to 2.71), cardiovascular mortality (1.93, 1.44 to 2.60), cardiac events (1.55, 1.15 to 2.08), and heart failure (1.16, 1.07 to 1.27). Results were broadly consistent in sensitivity analyses.
Conclusion Atrial fibrillation is a stronger risk factor for cardiovascular disease and death in women compared with men, though further research would be needed to determine any causality.
Introduction
Atrial fibrillation (AF) is a leading cause of cardiovascular disease worldwide,1 with an estimated 33.5 million people affected in 2010.2 Recent estimates from the Global Burden of Disease study indicated that AF was associated with an age adjusted mortality rate of 1.7 per 100 000 people (95% uncertainty interval 1.4 to 2.1) in 20103 and that the prevalence is increasing in both developed and developing countries.2
Although AF is associated with an increased risk of stroke4 and death5 in men and women, a growing body of literature suggests that women and men experience risk factors for cardiovascular disease differently. Previous analyses have shown that smoking and diabetes are associated with greater proportional risks of coronary heart disease in women than in men.6 7 Diabetes is also associated with a greater relative risk of stroke in women.8 It is currently unclear, however, whether such sex differences exist for AF. While being female is a risk factor for stroke among individuals with AF,9 this could reflect differences in the multivariable adjusted risk of stroke by sex in the general population rather than differential effects of AF by sex. To explore sex differences in the effect of AF, it is necessary to compare sex specific estimates of the effect of AF on risk of death and cardiovascular disease. While some studies have suggested that AF is more strongly associated with the risk of stroke10 and death11 in women than men, others have suggested not.12 13 14 Sex differences in the association between AF and death and cardiovascular disease would have substantial implications for the estimation of the global and regional burden, for the targeting of treatment to manage it, and for future research into causes of sex differences.
Accordingly, we conducted a meta-analysis of cohort studies to estimate the association between AF and cardiovascular disease and death in women and men and to compare the sexes.
Methods
Search strategy and selection criteria
We conducted a systematic review of cohort studies that reported associations between AF and death or cardiovascular events in men and women. This was done in accordance with the MOOSE (meta-analysis of observational studies in epidemiology) guidelines.15 An experienced research librarian designed and conducted the search strategy. Medline and Embase were searched from 1966 to March 2015 with a combined text and MeSH subheading search with the following terms: “atrial fibrillation”, “mortality”, “death”, “cardiovascular disease”, “heart failure”, “myocardial infarction”, “death, sudden, cardiac”, “stroke”, “kidney”, “renal”, “peripheral”, and “risk factors”. We conducted a review of the references of identified studies.
We included any study that reported sex specific associations between AF and any of the following outcomes: all cause mortality, cardiovascular mortality, stroke (fatal and non-fatal), cardiac events (a composite of cardiac death and non-fatal myocardial infarction, excluding heart failure), heart failure, peripheral arterial disease, and chronic kidney disease. For inclusion in the analysis, studies were required to have a minimum of 50 participants with AF, a minimum of 50 participants without AF, and a median follow-up of at least six months. Importantly, we included only studies that reported associations for both men and women to restrict our analysis to comparisons of men and women within studies and to reduce the risk of heterogeneity between studies influencing our results. Additionally, we required all studies to adjust for, at a minimum, age and the presence of cardiovascular disease at baseline. We excluded studies that examined postoperative atrial fibrillation because the differing epidemiology and duration of postoperative atrial fibrillation relative to chronic atrial fibrillation.16 There were no language restrictions, and an investigator with extensive experience in epidemiological study translation (AJH) translated non-English studies. We contacted authors of studies that did not report separate associations for women and men to provide any unpublished data on adjusted sex specific associations.
Data extraction
Data were extracted, in duplicate, from studies deemed to meet the eligibility criteria. These included details on general study characteristics (study name, duration of follow-up, year of publication), information about the studied population (number of participants with and without AF, mean age, number of men and women, number of participants with a history of coronary heart disease, stroke, and heart failure), and information on the outcomes in the study (all cause mortality, cardiovascular mortality, stroke, cardiac events, heart failure, peripheral arterial disease, and chronic kidney disease). We extracted sex specific adjusted measures of relative risk (hazard ratios, relative risks, and odds ratio) and 95% confidence intervals. We used the maximally adjusted relative risk that was available and risk estimates corresponding to the longest period of follow-up. For cohorts that had multiple reports of the same outcome, we used the report with the largest number of events. Study quality was assessed with the Newcastle-Ottawa scale for cohort studies.17
Statistical analysis
For the primary analysis, we derived a ratio of relative risks with 95% confidence intervals of AF for each outcome in women compared with men, as previously described.8 This relative risk ratio for each study was then pooled with inverse variance weighted random effects meta-analysis. We also pooled relative risks for men and women separately. For one study, which reported separate hazard ratios for men and women in different age groups, we first used inverse variance weighted fixed effects meta-analysis to generate a summary hazard ratio for men and for women.18 We used funnel plots to examine if publication bias seemed to be present for outcomes that had at least 10 studies present (all cause mortality and stroke).19 If publication bias was present, we used the trim and fill method to adjust for publication bias.20 Heterogeneity was quantified with the I2 statistic and the Q test. P<0.05 was considered significant.
To estimate the difference in absolute risks associated with AF between women and men, we multiplied estimated sex specific excess incidence rates for all cause mortality,21 cardiovascular mortality,21 coronary heart disease21 (restricted to coronary heart disease mortality as an incidence rate for the composite of coronary heart disease death and non-fatal myocardial infarction could not be obtained), stroke,22 and heart failure23 in the United Kingdom general population by sex specific associations of each outcome with AF. The relative risk associated with each outcome in women was calculated by multiplying the pooled ratio of relative risks by the relative risk in men. We then subtracted the excess risk in men from the excess risk in women to estimate the difference in absolute risks associated with AF between men and women. Confidence intervals were derived through simulation with 10 000 draws from the distribution of the men’s relative risk and ratio of relative risks performed.
Sensitivity analyses
We undertook seven sensitivity analyses to determine if the ratio of relative risks in women versus men for mortality and stroke differed by methodological and study characteristics. Firstly, we stratified studies by whether AF was ascertained through electrocardiography at baseline or through medical records. Secondly, we stratified by region (Europe versus non-Europe). For these two stratified analyses (which stratified on categorical variables), we performed tests for interactions between subgroups. Thirdly, we stratified by size of the study (>100 000 versus <100 000 participants) to examine whether the results were consistent we excluded two large studies24 25 (each with more than 100 000 participants). Fourthly, we stratified by baseline year of enrolment of each cohort (1990 and before versus 1991 or later). Fifthly, we stratified by length of follow-up (≤10 versus >10 years). Sixthly, we stratified by median age (≤65 versus >65 at baseline). Finally, we stratified studies by the ratio of the event rate in women to men to examine whether our results were influenced by potentially lower absolute risk of outcomes in women than men. For the five analyses that stratified on continuous variables we performed tests for trend using meta-regression. The seven sensitivity analyses were restricted to stroke and all cause mortality because there were too few studies to conduct sensitivity analyses for other outcomes. All statistical analyses were conducted with R version 3.0.
Patient involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in the design and implementation of the study. There are no plans to involve patients in dissemination.
Results
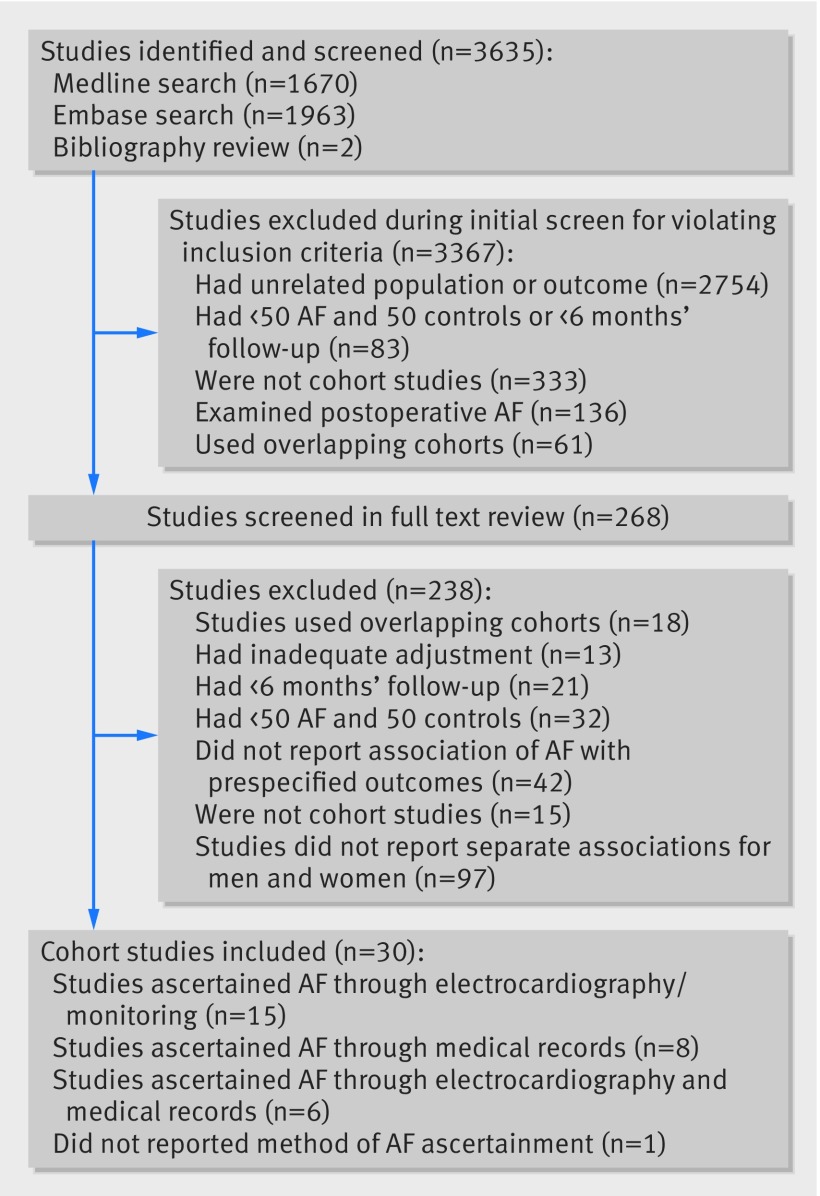
The systematic search identified 3635 studies, of which 268 were examined in the full text review (fig 1) and 238 were excluded. Accordingly, we included 30 cohort studies. None of these studies reported sex specific associations for either peripheral arterial disease or chronic kidney disease. Twenty studies provided published sex specific associations, while 10 studies provided unpublished associations.
Fig 1 Identification of cohort studies that reported associations between atrial fibrillation (AF) and death or cardiovascular events in men and women
Table 1 shows the characteristics of the included studies. Ascertainment of AF status was through electrocardiography or continuous monitoring in 15 studies, medical records in eight studies, and a combination in six studies. One study did not report the method of ascertainment. Quality of included studies, as assessed by the Newcastle-Ottawa Scale, was high (appendix table A).
Table 1.
Characteristics of included cohort studies that reported associations between atrial fibrillation (AF) and death or cardiovascular events in men and women
| Study | Location | Baseline year(s) | AF ascertainment | Total No (with AF) | No of women | Age (years) | Follow-up (years) | No of individuals at baseline with | Maximum adjustment available | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IHD | Stroke | HF | |||||||||
| Andersson 201426 | Sweden | 1995-2008 | Medical records | 21 987 (9519) | 6816 | 59 | NA | NA | NA | NA | Matched by sex, adjusted for age, comorbidities excluded |
| Bejot et al, 200927 | France | 1985-2006 | ECG | 3064 (572) | 1615 | 75 | 2.0 | 620 | 3064 | NA | Age |
| Benjamin 19985 | US | 1948 | ECG | 1863 (621) | 975 | 75 | 25.6 | 252 | 213 | 201 | Age, hypertension, smoking, diabetes, ECG left ventricular hypertrophy, vascular disease |
| Bouzas-Mosquera et al, 201028 | Spain | 1995-2008 | ECG | 17 100 (619) | 6999 | 64 | 6.5 | 2963 | NA | NA | Age, diabetes mellitus, hypertension, hypercholesterolemia, smoking habit, family history of CAD, MI, PCI, CABG, angina, LBBB, medication, chest pain, exercise ECG, METs, peak SBP, heart rate |
| Chamberlain et al, 201129 | US | 1983-2006 | ECG and medical records | 1664 (553) | 905 | 76 | 4.0 | 353 | NA | 1664 | Age, BMI, year of heart failure diagnosis, smoking status, derived NYHA class, estimated glomerular filtration rate, anaemia, hypertension, diabetes mellitus, COPD, MI, medication |
| Chao 201210 | Taiwan | 2000-09 | Medical records | 9119 (829) | 3520 | 45 | 4.8 | NA | NA | NA | Age, dyslipidaemia, CKD, asthma, malignancy, liver cirrhosis, autoimmune diseases (stepwise regression) |
| Chen 201330 | US | 1989 | ECG and medical records | 20 918 (2352) | 11 713 | 59 | 13.1 | 1786 | NA | 927 | Age, race, field centre, heart rate, smoking status, BMI, hypertension, diabetes mellitus, coronary heart disease |
| D’Agostino 199431 | US | 1948 | ECG | 5734 (140) | 3362 | 66 | 10 | NA | 0 | NA | Age, systolic blood pressure, antihypertensive therapy, cardiovascular disease, left ventricular hypertrophy, cigarettes, diabetes |
| Friberg 200411 | Denmark | 1976-78 | ECG | 29 310 (276) | 16 314 | 58 | 4.70 | 763 | 0 | NA | Age, arterial hypertension, SBP, diabetes, myocardial infarction, left ventricular hypertrophy, smoking, FEV1 |
| Genovesi et al, 200932 | Italy | 2003-06 | ECG | 476 (127) | 199 | NA | 3.0 | 112 | NA | 45 | Age, ischaemic heart disease, diabetes |
| Guize 200725 | France | 1972-1988 | ECG | 154 070 (298) | 55 109 | 51 | 15.2 | NA | NA | NA | Age, cardiomyopathy, left ventricular hypertrophy, blood pressure, cholesterol, glycaemia, BMI, smoking, alcohol, vital capacity |
| Hamaguchi 200913 | Japan | 2004-05 | ECG | 2659 (937) | 1069 | 71 | 2.4 | 851 | 399 | 2659 | Age, cause of heart failure, medical history, serum creatinine, haemoglobin and BNP levels, LVEF, medication use |
| Hermann et al, 201333 | Germany | 2000-03 | ECG | 4180 (52) | 2212 | 59.2 | 7.9 | 0 | 0 | 0 | Age, systolic blood pressure, LDL and HDL cholesterol, diabetes mellitus, and smoking |
| Hippisley-Cox et al, 201034 | UK | 1994-2010 | Medical records | 2 343 759 (12 031) | 1 189 845 | 48.1 | 7.0 | 0 | 0 | 0 | BMI, SBP, cholesterol, deprivation, ethnic group, family history of coronary heart disease, type 2 diabetes, treated hypertension, rheumatoid arthritis, atrial fibrillation, chronic renal disease (age used as underlying time variable) |
| Hippisley-Cox 201324 | England and Wales | 1998-2012 | Medical records | 3 549 478 (15 371) | 1 801 370 | 45 | 7 | 99 561 | 0 | 16 294 | Age, BMI, BP, cholesterol, deprivation, smoking, ethnicity, vascular disease, other comorbidities |
| Hippisley-Cox et al, 201535 | UK | 1998-2014 | Medical records | 437 806 (13 953) | 192 896 | 60 | NA | NA | NA | 0 | Age, cholesterol/HDL ratio, deprivation, duration of diabetes, smoking status, ethnicity, type 1 diabetes, cardiovascular disease, chronic renal disease |
| Iwahana 201136 | Japan | 1992-95 | ECG | 10 929 (54) | 6782 | 56 | 10.7 | NA | 0 | NA | Area, age, smoking, drinking status, obesity, hypertension, dyslipidaemia, diabetes mellitus |
| Kaarisalo 199737 | Finland | 1983-92 | ECG and medical records | 2635 (767) | 1880 | 82 | 1 | 457 | 2635 | NA | Age, recent MI, previous MI, hypertension |
| Nakayama 199738 | Japan | 1977 | ECG | 2302 (NA) | 1341 | NA | 15.5 | NA | 0 | NA | Age, BP, cholesterol, haematocrit, BMI, ECG abnormality, albumin, glucose, optic fundus, cigarettes, alcohol, physical activity, IHD |
| Ohsawa 200739 | Japan | 1980 | ECG | 9483 (60) | 5329 | 51 | 19 | NA | 0 | NA | Age, BMI, SBP, glucose, cholesterol, history of valvular heart disease, left ventricular hypertrophy, alcohol, smoking |
| Ruigomez et al. 2002 40 | UK | 1996 | Medical records | 6035 (1035) | NA | NA | 2 | NA | NA | NA | Age, smoking, diabetes, heart failure, ischaemic heart disease, hypertension, cerebrovascular disease |
| Saposnik et al, 201141 | Canada | 2002-04 | Medical records | 8223 (1405) | 3901 | 72 | 1 | 1936 | 8223 | 734 | Age, sex, severe stroke, nonlacunar stroke subtype, glucose, coronary artery disease, congestive heart failure, cancer, dementia, dialysis, dependency before stroke |
| Siontis et al, 201442 | US | 1975-2012 | ECG and medical records | 3673 (650) | 1661 | 55 | 4.1 | NA | NA | NA | Age, sex, FHx SCD, NYHA class III/IV, obstructive phenotype, aspirin/warfarin |
| Soliman et al, 201443 | US | 2003-07 | ECG and self-reported history | 23 928 (1631) | 13 937 | 64 | 4.5 | 0 | NA | NA | Age, race, region, education, income, cholesterol, smoking, SBP, BMI, diabetes, medication, and history of noncardiac vascular disease, eGFR, CRP, albumin |
| Soliman et al, 201544 | US | 1987-89 | ECG and medical records | 14 462 (1545) | 8172 | 54 | 21.6 | 0 | 249 | 71 | Age, race, study field centre, education, income, cholesterol, smoking status, SBP, BMI, diabetes, eGFR, cardiovascular disease, medication use |
| Stewart et al, 200212 | Scotland | 1972-76 | ECG | 15 406 (100) | 8354 | 54 | 20 | NA | 197 | NA | Age, stroke, chest pain, cholesterol, DBP, cardiothoracic ratio, glucose, FEV1, bronchitis, Q waves, ST segment, LBBB |
| Stortecky et al, 201314 | Switzerland | 2007-11 | Continuous monitor | 389 (131) | 224 | 83 | 1 | 238 | 30 | 364 | Age, BMI, hypertension, diabetes, medical history, symptoms, cardiovascular risk (stepwise regression) |
| van Wijk et al, 200745 | Netherlands | 1986-93 | ECG | 2659 (186) | 946 | 66 | 10.1 | 277 | 2659 | NA | Age, hypertension, smoking, diabetes, Rankin scale, any infarct, white matter lesion on CT scan |
| Wolf et al, 199818 | US | 1989 | Medical records | 26 753 (13 558) | 14 416 | NA | 3 | NA | NA | NA | Matched for age and sex, adjusted for AMI, unstable angina, stable angina, heart failure, hypertension, diabetes, valvular disease, stroke, COPD |
| Wolfe et al, 200646 | UK and Barbados | 1995-2003 | NA | 848 (64) | 464 | 69.6 | 1.7 | 94 | 848 | NA | Age, Barbados resident, living alone, Bathel score, smoking, alcohol, IHD untreated and treated, hypertension untreated and treated, diabetes, TIA untreated and treated, incontinence, swallow test, hospital admission |
NA=not available, ECG=electrocardiogram, CKD=chronic kidney disease, BP=blood pressure, BMI=body mass index, SBP=systolic blood pressure, DBP=diastolic blood pressure, eGFR=estimated glomerular filtration rate, CRP=C reactive protein, LBBB=left bundle branch block, AMI=acute myocardial infarction, COPD=chronic obstructive pulmonary disease, FEV1=forced expiratory volume, LVEF=left ventricular ejection fraction, BNP=B type natriuretic peptide, NYHA=New York Heart Association, IHD=ischaemic heart disease.
Studies included a total of 4 371 714 participants, 66 511 with AF (not counting one study34 with an overlapping cohort as a second study24). Twenty six studies reported the number of events. Of these, 14 studies reported on all cause mortality (18 563 events), four studies on cardiovascular mortality (7702 events), 11 studies reported on stroke (83 030 events), six studies on cardiac events (3583 events), and three studies on heart failure (27 468 events). Four additional studies reported relative risks for all cause mortality, cardiovascular mortality, and stroke associated with AF but did not report the number of events. Appendix table B shows pooled incidence rates for studies that reported number of events for men and women separately are provided.
Risk of cardiovascular disease and all cause mortality in women versus men
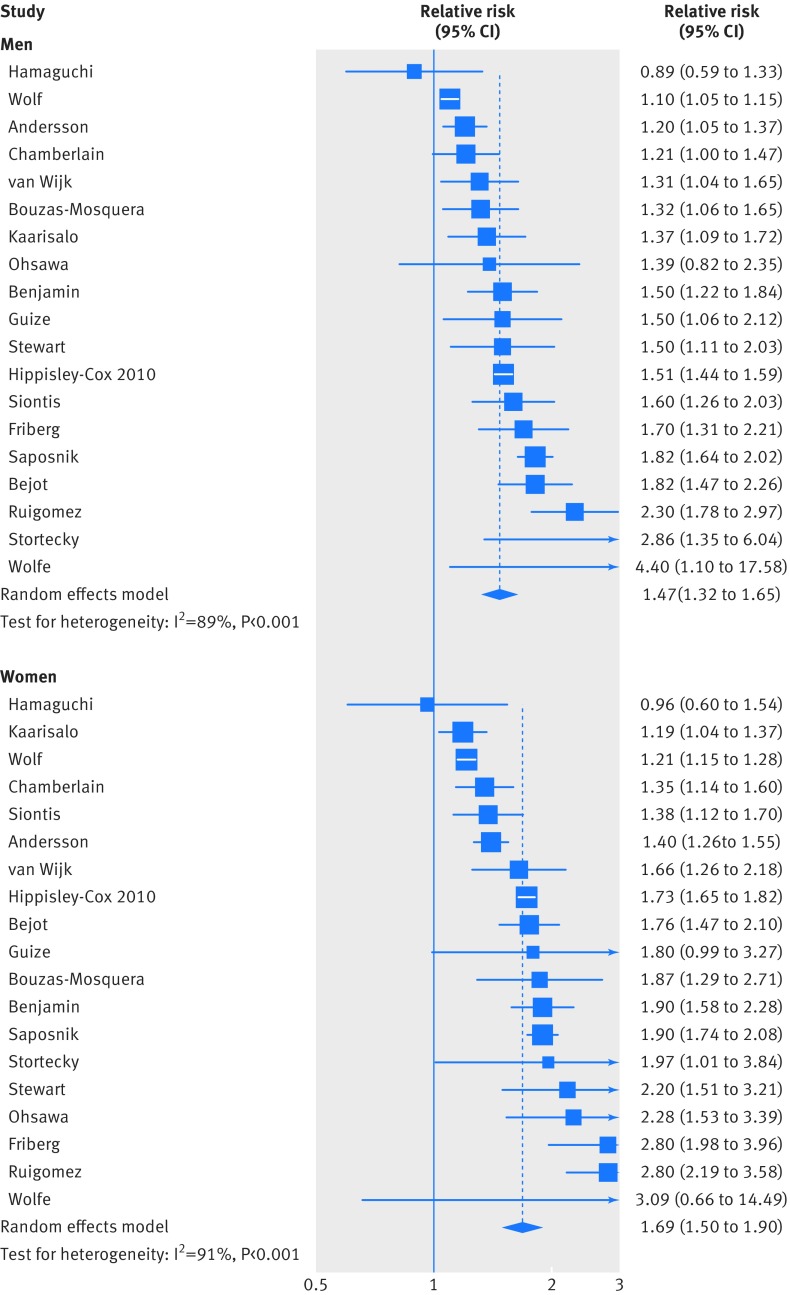
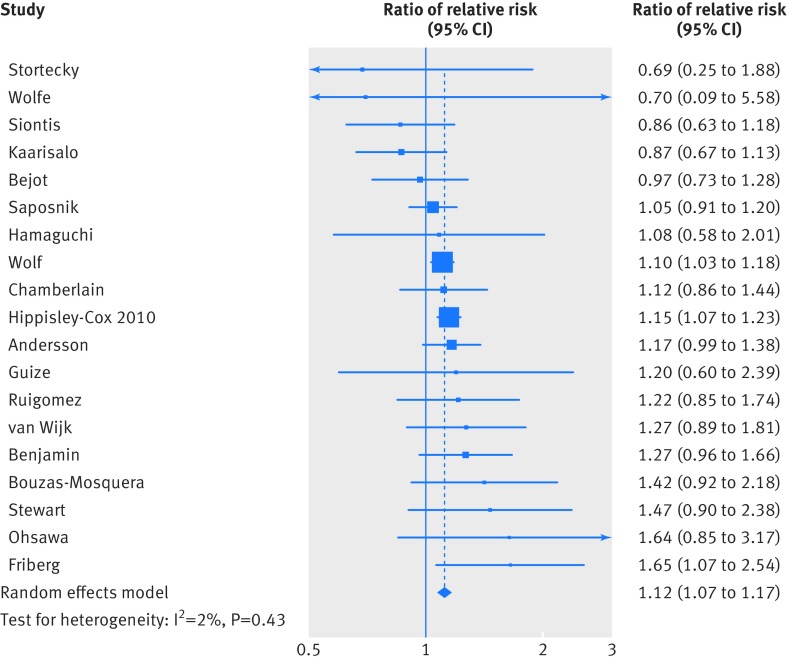
The pooled relative risk of all cause mortality for individuals with AF compared with those without AF was higher in women than in men (relative risk 1.69 (95% confidence interval 1.50 to 1.90) v 1.47 (1.32 to 1.65); fig 2). The pooled ratio of relative risks for women versus men showed a 12% greater risk of all cause mortality associated with AF in women than in men (relative risk ratio 1.12, 95% confidence interval 1.07 to 1.17l; fig 3). Although heterogeneity was observed in the relative risk of all cause mortality associated with AF in both women and men (I2=91% and I2=89%, respectively, P<0.001; fig 2), no significant heterogeneity was observed in the pooled ratio of relative risks (I2=2%, P=0.43; fig 3).
Fig 2 Maximally adjusted relative risk for all cause mortality for individuals with and without AF by sex. Area of each square is proportional to inverse variance of estimate. Horizontal lines indicate 95% confidence intervals
Fig 3 Maximally adjusted women-to-men ratio of relative risks for any all cause mortality for individuals with and without AF. Area of each square is proportional to inverse variance of estimate. Horizontal lines indicate 95% confidence intervals
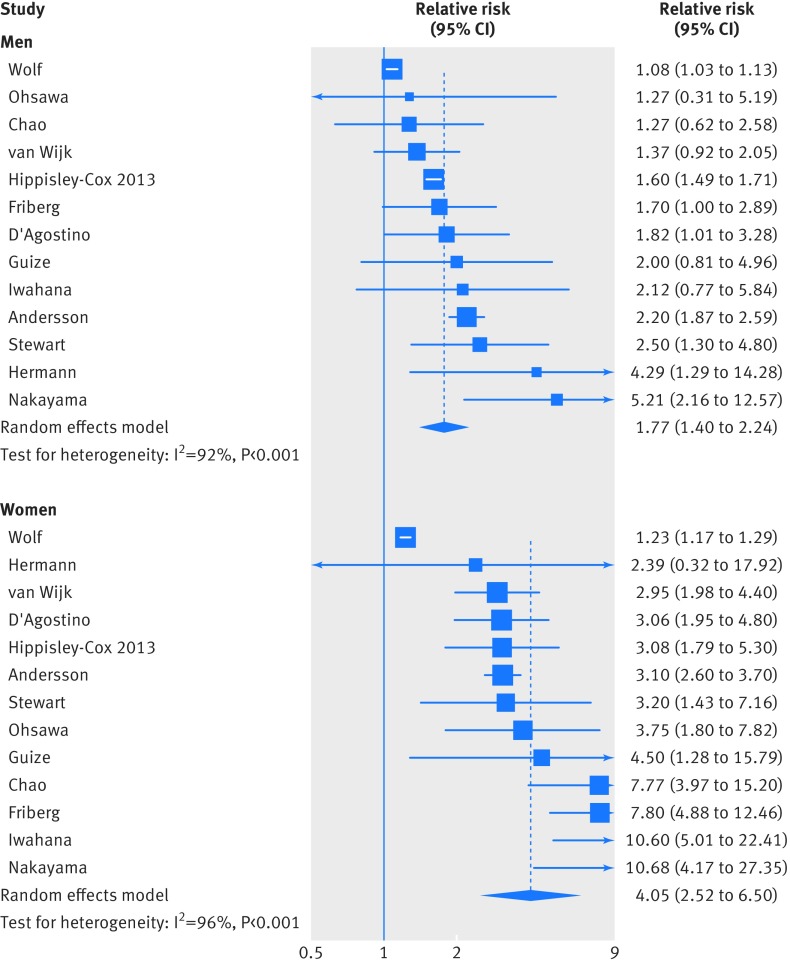
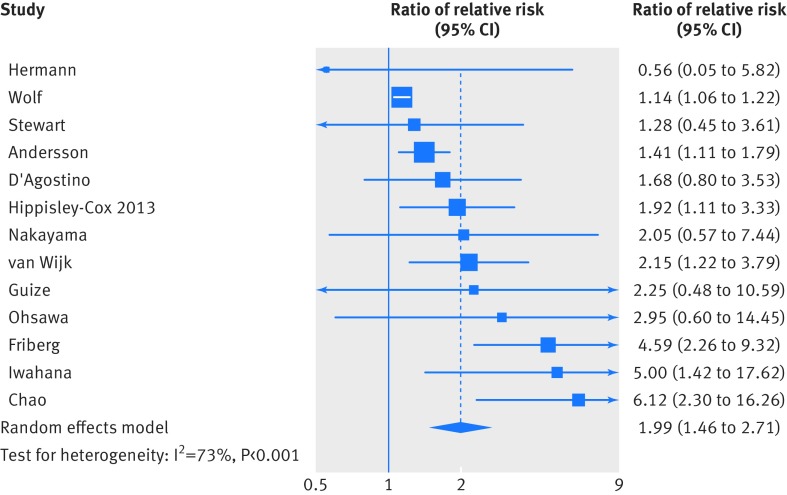
The relative risk of stroke was also greater in women than in men (relative risk 4.05 (95% confidence interval 2.52 to 6.50) v 1.77 (1.40 to 2.24); fig 4). When we pooled the ratios of relative risks, AF was observed to be associated with twice the relative risk of stroke in women than in men (relative risk ratio 1.99, 95% confidence interval 1.46 to 2.71; fig 5). There was significant heterogeneity between studies (I2=73%, P<0.001).
Fig 4 Maximally adjusted relative risk for stroke for individuals with and without AF by sex. Area of each of each square is proportional to inverse variance of estimate. Horizontal lines indicate 95% confidence intervals
Fig 5 Maximally adjusted women-to-men ratio of relative risks for stroke for individuals with and without AF. Area of each square is proportional to inverse variance of estimate. Horizontal lines indicate 95% confidence intervals
AF was associated with a higher relative risk of cardiovascular mortality in women than in men (relative risk ratio 1.93, 95% confidence interval 1.44 to 2.60; fig 6; appendix fig A), with little heterogeneity observed between studies (I2=8%), and was associated with a 55% higher relative risk of cardiac events (cardiac death or non-fatal myocardial infarction) in women versus men (1.55, 1.15 to 2.08; fig 6; appendix fig B). This was consistent when we restricted our analysis to three studies that reported only myocardial infarction, excluding the one study that reported sudden cardiac death30 (1.64, 1.15 to 2.34). AF was also associated with an increased risk of heart failure in women compared with men (1.16, 1.07 to 1.27; appendix fig C).
Fig 6 Maximally adjusted pooled women-to-men ratio of relative risks for all cause mortality, CVD (cardiovascular) mortality, stroke, cardiac events, and heart failure, comparing individuals with and without AF. Area of each square is proportional to inverse variance of estimate. Horizontal lines indicate 95% confidence intervals
When we looked at events per 1000 patient years, corresponding absolute risk increases in outcomes associated with AF in women compared with men were 1.8 (95% confidence interval 1.1 to 2.6) for all cause mortality, 4.3 (1.9 to 7.5) for cardiovascular mortality, 3.1 (1.1 to 6.1) for stroke, 0.6 (0.03 to 1.3) for cardiac events, and 6.1 (2.1 to 12.7) for heart failure.
Sensitivity analyses
Ratios of relative risk for all cause mortality were broadly consistent in seven sensitivity analyses (appendix fig D). Results of tests of interaction were non-significant when we stratified studies by ascertainment of AF through electrocardiography versus use of medical records/self reported history and region (Europe, non-Europe; all P>0.05 for interaction). Results of tests for trend by number of participants, baseline year, and ratio of mortality rate in women to men were also non-significant. Ratios of relative risk, however, declined with increasing length of follow-up and increasing age (appendix fig D).
For ratios of relative risks for stroke, results of tests of interaction by ascertainment method and region were non-significant (appendix fig E). Results of tests for trend by number of participants, baseline year, length of follow-up, and median age were also non-significant. Relative risks were significantly higher in studies with a lower ratio of absolute rate of stroke in women compared with men (P=0.027 for trend for ratio of stroke rate in women to men). When we restricted the meta-analysis to three studies with a ratio of stroke rate in women to men greater than 1 (that is, a greater absolute rate of stroke in women than men), however, atrial fibrillation continued to be associated with a higher relative risk of stroke in women than men (1.47, 95% confidence interval 1.18 to 1.83).
We found no evidence of publication bias for all cause mortality (appendix fig F), though we observed significant publication bias for stroke (appendix fig G; P=0.002). When we used the trim and fill method to control for publication bias, AF was associated with a non-significantly higher risk of stroke in women than in men (relative risk ratio 1.28, 95% confidence interval 0.94 to 1.73).
Discussion
In this systematic review and meta-analysis of 30 studies with 4 371 714 participants, we observed atrial fibrillation (AF) to be a significantly greater risk factor for death and cardiovascular disease in women than in men. AF was associated with a higher relative risk of all cause mortality, stroke, cardiovascular mortality, cardiac events, and heart failure in women compared with men.
Comparison with previous individual studies
Previous studies have presented conflicting evidence on the effect of AF on the risk of death and cardiovascular disease in women. Of the 19 studies on the association of AF with the risk of all cause mortality (fig 2) we included in our analysis, the ratio of relative risks was greater than one but not significant for 11 studies. When we pooled these studies using random effects meta-analysis, the estimate for all cause mortality was significant, indicating that individual studies were underpowered to detect a differential effect of AF on risk of all cause mortality in women compared with men. Similarly, six of the 13 studies that reported a sex specific association of AF with stroke did not detect a significant interaction between women and men (fig 3). When we pooled these studies, however, we observed a significant ratio of relative risks, again indicating a lack of power of some previous individual studies to detect an interaction by sex.
Recent meta-analyses have shown that type 2 diabetes is a greater risk factor for coronary heart disease7 47 (ratio of relative risk 1.44, 95% confidence interval 1.27 to 1.63) and for stroke8 (1.27, 1.10 to 1.46) in women than in men and that type 1 diabetes is also a greater risk factor for death and cardiovascular disease in women.48 Evidence of an increased risk of coronary heart disease associated with type 2 diabetes in women has been cited in European Society of Cardiology guidelines for the treatment of cardiovascular disease in patients with type 2 diabetes.49 Similarly, evidence of an increased risk of stroke associated with type 2 diabetes in women has been included in American Heart Association/American Stroke Association guidelines for stroke prevention in women.50 Our results show that AF is also a greater risk factor for death and cardiovascular disease in women than in men and extend these previous works showing that women experience the effects of some key risk factors for cardiovascular disease differently to men.
It is unclear what could cause the observed differences in risk of mortality and cardiovascular disease associated with AF between women and men. One possibility is that women with AF are undertreated relative to men. The results of a cohort study of Canadian patients with AF enrolled in 1990-94 support this hypothesis. Canadian women were half as likely as Canadian men to receive warfarin.51 Analyses of more contemporary cohorts, including a global registry of 17 814 patients with AF52 and an analysis of 83 513 patients with AF in Quebec,53 however, showed no differences in use of anticoagulants between men and women with AF.53 It is therefore unlikely that broad differences in treatment between the sexes are responsible for the increased relative risks we observed in women. Physiological or psychosocial differences between women and men could result in differential effects of AF on cardiovascular risk. For example, women are at a higher risk of torsade de pointes, an often lethal adverse event of antiarrhythmic drugs prescribed for AF.54 Response to oral anticoagulants could also differ between the sexes, with a higher risk of bleeding observed among women.55 Future research is needed to distinguish if one or many of these potential mechanisms underlie the differential effects of AF observed in our analysis.
Strengths and limitations
This analysis has several strengths. Firstly, as a systematic review and meta-analysis of all available studies of AF and risk of death and cardiovascular disease in women compared with men, it has greater power than any of the included individual studies to detect differences. This is evident in the meta-analysis of all cause mortality, in which 16 of the included 19 studies did not detect a difference. Secondly, we included only studies that reported the effect of AF on risk of cardiovascular disease and death separately in men and women. This ensured that our primary analysis (the ratio of relative risks) was a within study comparison, minimising the effect of heterogeneity between studies. Thirdly, we included only cohort studies that were adequately adjusted (prespecified requirement to adjust by at least age and history of cardiovascular disease) and that had a minimum of 100 participants with six months’ follow-up to reduce the risk of confounding and small study effects. Fourthly, pooled ratios of relative risk for all cause mortality or stroke were broadly consistent in several different sensitivity analyses.
This analysis also has several limitations. Firstly, while we attempted to contact and acquire unpublished data from eligible cohorts, our results might be influenced by publication bias because studies that detect an interaction between AF and risk of death and cardiovascular disease by sex might be more likely to be published. While there was evidence of publication bias for stroke, however, we found no evidence of this for all cause mortality. Furthermore, use of trim and fill procedures resulted in a non-significantly increased effect of AF on risk of stroke in women compared with in men similar in magnitude to other outcomes. Secondly, as a meta-analysis of observational studies, sex differences in the association of AF with risk of death and cardiovascular disease might be caused by unobserved confounding between sexes. For example, women might have had a greater number of comorbidities at the time of diagnosis of AF, which could not be fully adjusted for. However, we required included studies to adjust for, at minimum, age and presence of cardiovascular comorbidities, and we used the maximally adjusted model available. Thirdly, many of the studies had differences in design, duration of follow-up, outcome ascertainment, and populations. Indeed, we observed a greater absolute increase in cardiovascular death than all cause death because of differing studies contributing to either outcome. Because our primary analysis was focused on comparisons within studies (the ratio of relative risks between women and men), however, heterogeneity was low for outcomes other than stroke. Fourthly, our primary analysis focused on the ratio of relative risks, which might not reflect absolute differences in risk of death and cardiovascular disease associated with AF between sexes. We found no evidence of a difference in ratios of relative risk in studies in which the absolute risk of all cause mortality was higher in men (appendix fig D), and a higher ratio of relative risks continued to be observed in studies in which women had a higher absolute rate of stroke than men (appendix fig E). Finally, we were unable to ascertain the underlying cause of the sex differences in the association of AF with risk of mortality and cardiovascular disease.
Implications for clinicians, policy makers, and future research
This analysis has several implications. With respect to clinical care, our results indicate that AF is associated with worse outcomes in women than in men. Although female sex is incorporated as a risk factor for stroke in the widely used CHA2DS2-VASc score,56 AF seems to affect women and men differently. The American Heart Association recently recommended the development of a specific risk score for stroke in women as some risk factors for stroke are unique to women, others are more prevalent in women, and others differentially increase the risk of stroke in women.57 These results support the development of such a score. They also, however, show that AF is associated with an increased risk of all cause mortality, cardiovascular mortality, and cardiac events in women relative to men. Therefore, it might be appropriate for clinicians to consider more aggressive treatment of risk factors in women with AF as they seem to be at higher proportional risk of death and cardiovascular disease.
With regard to public health policy, these results indicate that sex differences in the effect of AF on risk of death and cardiovascular disease exist. Consequently, estimation of the global and regional burden of AF should be independent of sex. Allocation of public health resources for prevention and treatment of AF should also consider the differential effects of AF by sex. Future research should be encouraged to determine the underlying causes of the observed sex differences.
What is already known on this topic
Atrial fibrillation (AF) is associated with an increased risk of stroke and death in men and women
A growing body of literature suggests that women and men experience risk factors for cardiovascular disease differently, including diabetes, smoking, and body mass index
What this paper adds
AF is associated with a stronger relative risk of all cause mortality, cardiovascular mortality, stroke, ischaemic heart disease, and heart failure in women than in men
Whether the differential association of AF with death and cardiovascular disease in women relative to men is causal is unclear
Web Extra.
Extra material supplied by author
Appendix: Supplementary tables A and B; figures A-G; extra references
We thank the following for contributing unpublished data: Julia Hippisley-Cox (QRisk); Janine Gronewold and Dick Hermann (Heinz Nixdorf Recall Study); Ale Algra (Life Long After Cerebral Ischaemia study); Charles Wolfe and Siobhan Crichton (South London Stroke Register and Barbados Register of Strokes, funded by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London); Konstantinos Siontis, Bernard Gersh, and Jeffrey Geske (Mayo Clinic); Alberto Bouzas-Mosquera (Madrid, Spain); Gustavo Saposnik (Registry of the Canadian Stroke Network); Yannick Bejot (stroke registry of Dijon, France); Veronique Roger and Alanna Chamberlain (Olmsted County); and Emanuela Rossi and Simonetta Genovesi (Lombardi, Italy). Your contributions are greatly appreciated.
Contributors: CAE, CXW, and AAO were involved in the design, implementation, and analysis of the study and in writing the final manuscript. AJH was involved in the implementation of the study and in commenting on drafts of the final manuscript. MW, SAEP, and DGA were involved in the analysis of the study and in commenting on drafts of the final manuscript. CAE is guarantor.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. CAE, CXW, AJH, and AAO are funded by Rhodes Scholarships. CXW is also supported by a Neil Hamilton Fairly Fellowship from the National Health and Medical Research Council of Australia. No funders were involved in the design, implementation, analysis, or reporting of this study.
Ethical approval: Not required.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf. MW declares consultancy fees from Amgen and Novartis. All other authors declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Data sharing: Data and code are available from the lead author on request.
Transparency: The lead author (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1.Murray CJL, Vos T, Lozano R etal. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380: 2197-223. 10.1016/S0140-6736(12)61689-4. 23245608 [DOI] [PubMed] [Google Scholar]
- 2.Chugh SS, Havmoeller R, Narayanan K etal. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 2014;129: 837-47. 10.1161/CIRCULATIONAHA.113.005119. 24345399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lozano R, Naghavi M, Foreman K etal. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380: 2095-128. 10.1016/S0140-6736(12)61728-0. 23245604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22: 983-8. 10.1161/01.STR.22.8.983 1866765 [DOI] [PubMed] [Google Scholar]
- 5.Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 1998;98: 946-52. 10.1161/01.CIR.98.10.946 9737513 [DOI] [PubMed] [Google Scholar]
- 6.Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet 2011;378: 1297-305. 10.1016/S0140-6736(11)60781-2. 21839503 [DOI] [PubMed] [Google Scholar]
- 7.Peters SAE, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia 2014;57: 1542-51. 10.1007/s00125-014-3260-6. 24859435 [DOI] [PubMed] [Google Scholar]
- 8.Peters SAE, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet 2014;383: 1973-80. 10.1016/S0140-6736(14)60040-4. 24613026 [DOI] [PubMed] [Google Scholar]
- 9.Friberg L, Benson L, Rosenqvist M, Lip GYH. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ 2012;344: e3522. 10.1136/bmj.e3522. 22653980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chao T-F, Liu C-J, Chen S-J etal. Atrial fibrillation and the risk of ischemic stroke: does it still matter in patients with a CHA2DS2-VASc score of 0 or 1?Stroke 2012;43: 2551-5. 10.1161/STROKEAHA.112.667865. 22871677 [DOI] [PubMed] [Google Scholar]
- 11.Friberg J, Scharling H, Gadsbøll N, Truelsen T, Jensen GBCopenhagen City Heart Study. Comparison of the impact of atrial fibrillation on the risk of stroke and cardiovascular death in women versus men (The Copenhagen City Heart Study). Am J Cardiol 2004;94: 889-94. 10.1016/j.amjcard.2004.06.023. 15464671 [DOI] [PubMed] [Google Scholar]
- 12.Stewart S, Hart CL, Hole DJ, McMurray JJV. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med 2002;113: 359-64. 10.1016/S0002-9343(02)01236-6 12401529 [DOI] [PubMed] [Google Scholar]
- 13.Hamaguchi S, Yokoshiki H, Kinugawa S etalJapanese Cardiac Registry of Heart Failure in Cardiology Investigators. Effects of atrial fibrillation on long-term outcomes in patients hospitalized for heart failure in Japan: a report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J 2009;73: 2084-90. 10.1253/circj.CJ-09-0316 19755750 [DOI] [PubMed] [Google Scholar]
- 14.Stortecky S, Buellesfeld L, Wenaweser P etal. Atrial fibrillation and aortic stenosis: impact on clinical outcomes among patients undergoing transcatheter aortic valve implantation. Circ Cardiovasc Interv 2013;6: 77-84. 10.1161/CIRCINTERVENTIONS.112.000124. 23386662 [DOI] [PubMed] [Google Scholar]
- 15.Stroup DF, Berlin JA, Morton SC etal. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283: 2008-12. 10.1001/jama.283.15.2008 10789670 [DOI] [PubMed] [Google Scholar]
- 16.Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med 2001;135: 1061-73. 10.7326/0003-4819-135-12-200112180-00010 11747385 [DOI] [PubMed] [Google Scholar]
- 17.Wells GA, Shea B, O’connell D, Peterson J, Welch V. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. www.ohri.ca/programs/clinical_epidemiology/oxford.asp. (accessed 3 Jul2015).
- 18.Wolf PA, Mitchell JB, Baker CS, Kannel WB, D’Agostino RB. Impact of atrial fibrillation on mortality, stroke, and medical costs. Arch Intern Med 1998;158: 229-34. 10.1001/archinte.158.3.229 9472202 [DOI] [PubMed] [Google Scholar]
- 19.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315: 629-34. 10.1136/bmj.315.7109.629 9310563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000;56: 455-63. 10.1111/j.0006-341X.2000.00455.x 10877304 [DOI] [PubMed] [Google Scholar]
- 21.Bhatnagar P, Wickramasinghe K, Williams J, Rayner M, Townsend N. The epidemiology of cardiovascular disease in the UK 2014. Heart 2015;101: 1182-9. 10.1136/heartjnl-2015-307516. 26041770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carroll K, Murad S, Eliahoo J, Majeed A. Stroke incidence and risk factors in a population-based prospective cohort study. Health Stat Q 2001;12; 18- 26. [Google Scholar]
- 23.de Giuli F, Khaw K-T, Cowie MR, Sutton GC, Ferrari R, Poole-Wilson PA. Incidence and outcome of persons with a clinical diagnosis of heart failure in a general practice population of 696,884 in the United Kingdom. Eur J Heart Fail 2005;7: 295-302. 10.1016/j.ejheart.2004.10.017. 15718168 [DOI] [PubMed] [Google Scholar]
- 24.Hippisley-Cox J, Coupland C, Brindle P. Derivation and validation of QStroke score for predicting risk of ischaemic stroke in primary care and comparison with other risk scores: a prospective open cohort study. BMJ 2013;346: f2573. 10.1136/bmj.f2573. 23641033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guize L, Thomas F, Bean K, Benetos A, Pannier B. [ Atrial fibrillation: prevalence, risk factors and mortality in a large French population with 15 years of follow-up]. Bull Acad Natl Med 2007;191: 791- 805. [PubMed] [Google Scholar]
- 26.Andersson T, Magnuson A, Bryngelsson I-L etal. Gender-related differences in risk of cardiovascular morbidity and all-cause mortality in patients hospitalized with incident atrial fibrillation without concomitant diseases: a nationwide cohort study of 9519 patients. Int J Cardiol 2014;177: 91-9. 10.1016/j.ijcard.2014.09.092. 25499348 [DOI] [PubMed] [Google Scholar]
- 27.Béjot Y, Ben Salem D, Osseby GV etal. Epidemiology of ischemic stroke from atrial fibrillation in Dijon, France, from 1985 to 2006. Neurology 2009;72: 346-53. 10.1212/01.wnl.0000341280.31919.bd. 19171832 [DOI] [PubMed] [Google Scholar]
- 28.Bouzas-Mosquera A, Peteiro J, Broullón FJ etal. Effect of atrial fibrillation on outcome in patients with known or suspected coronary artery disease referred for exercise stress testing. Am J Cardiol 2010;105: 1207-11. 10.1016/j.amjcard.2009.12.037. 20403467 [DOI] [PubMed] [Google Scholar]
- 29.Chamberlain AM, Redfield MM, Alonso A, Weston SA, Roger VL. Atrial fibrillation and mortality in heart failure: a community study. Circ Heart Fail 2011;4: 740-6. 10.1161/CIRCHEARTFAILURE.111.962688. 21920917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen LY, Sotoodehnia N, Bůžková P etal. Atrial fibrillation and the risk of sudden cardiac death: the atherosclerosis risk in communities study and cardiovascular health study. JAMA Intern Med 2013;173: 29-35. 10.1001/2013.jamainternmed.744. 23404043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.D’Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke 1994;25: 40-3. 10.1161/01.STR.25.1.40. 8266381 [DOI] [PubMed] [Google Scholar]
- 32.Genovesi S, Valsecchi MG, Rossi E etal. Sudden death and associated factors in a historical cohort of chronic haemodialysis patients. Nephrol Dial Transplant 2009;24: 2529-36. 10.1093/ndt/gfp104. 19293137 [DOI] [PubMed] [Google Scholar]
- 33.Hermann DM, Gronewold J, Lehmann N etalHeinz Nixdorf Recall Study Investigative Group. Coronary artery calcification is an independent stroke predictor in the general population. Stroke 2013;44: 1008-13. 10.1161/STROKEAHA.111.678078. 23449263 [DOI] [PubMed] [Google Scholar]
- 34.Hippisley-Cox J, Coupland C, Robson J, Brindle P. Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using QResearch database. BMJ 2010;341: c6624. 10.1136/bmj.c6624. 21148212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hippisley-Cox J, Coupland C. Development and validation of risk prediction equations to estimate future risk of heart failure in patients with diabetes: a prospective cohort study. BMJ Open 2015;5: e008503. 10.1136/bmjopen-2015-008503. 26353872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iwahana H, Ishikawa S, Ishikawa J etal. Atrial fibrillation is a major risk factor for stroke, especially in women: the Jichi Medical School cohort study. J Epidemiol 2011;21: 95-101. 10.2188/jea.JE20090149 21307613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaarisalo MM, Immonen-Räihä P, Marttila RJ etal. Atrial fibrillation in older stroke patients: association with recurrence and mortality after first ischemic stroke. J Am Geriatr Soc 1997;45: 1297-301. 10.1111/j.1532-5415.1997.tb02927.x 9361653 [DOI] [PubMed] [Google Scholar]
- 38.Nakayama T, Date C, Yokoyama T, Yoshiike N, Yamaguchi M, Tanaka H. A 15.5-year follow-up study of stroke in a Japanese provincial city. The Shibata Study. Stroke 1997;28: 45-52. 10.1161/01.STR.28.1.45 8996487 [DOI] [PubMed] [Google Scholar]
- 39.Ohsawa M, Okayama A, Okamura T etal. Mortality risk attributable to atrial fibrillation in middle-aged and elderly people in the Japanese general population: nineteen-year follow-up in NIPPON DATA80. Circ J 2007;71: 814-9. 10.1253/circj.71.814 17526974 [DOI] [PubMed] [Google Scholar]
- 40.Ruigómez A, Johansson S, Wallander MA, García Rodríguez LA. Risk of mortality in a cohort of patients newly diagnosed with chronic atrial fibrillation. BMC Cardiovasc Disord 2002;2: 5. 10.1186/1471-2261-2-5 11897013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saposnik G, Kapral MK, Liu Y etalInvestigators of the Registry of the Canadian Stroke Network Stroke Outcomes Research Canada (SORCan) Working Group. IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke. Circulation 2011;123: 739-49. 10.1161/CIRCULATIONAHA.110.983353. 21300951 [DOI] [PubMed] [Google Scholar]
- 42.Siontis KC, Geske JB, Ong K, Nishimura RA, Ommen SR, Gersh BJ. Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical correlations, and mortality in a large high-risk population. J Am Heart Assoc 2014;3: e001002. 10.1161/JAHA.114.001002. 24965028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Soliman EZ, Safford MM, Muntner P etal. Atrial fibrillation and the risk of myocardial infarction. JAMA Intern Med 2014;174: 107-14. 10.1001/jamainternmed.2013.11912. 24190540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Soliman EZ, Lopez F, O’Neal WT etal. Atrial Fibrillation and Risk of ST-Segment-Elevation Versus Non-ST-Segment-Elevation Myocardial Infarction: The Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2015;131: 1843-50. 10.1161/CIRCULATIONAHA.114.014145. 25918127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van Wijk I, Koudstaal PJ, Kappelle LJ, van Gijn J, Gorter JW, Algra ALiLAC Study Group. Long-term occurrence of death and cardiovascular events in patients with transient ischaemic attack or minor ischaemic stroke: comparison between arterial and cardiac source of the index event. J Neurol Neurosurg Psychiatry 2008;79: 895-9. 10.1136/jnnp.2007.133132. 18096680 [DOI] [PubMed] [Google Scholar]
- 46.Wolfe CDA, Corbin DOC, Smeeton NC etal. Poststroke survival for black-Caribbean populations in Barbados and South London. Stroke 2006;37: 1991-6. 10.1161/01.STR.0000230647.77889.84. 16794207 [DOI] [PubMed] [Google Scholar]
- 47.Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 2006;332: 73-8. 10.1136/bmj.38678.389583.7C. 16371403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Huxley RR, Peters SAE, Mishra GD, Woodward M. Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2015;3: 198-206. 10.1016/S2213-8587(14)70248-7. 25660575 [DOI] [PubMed] [Google Scholar]
- 49.Rydén L, Grant PJ, Anker SD etal. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 2013;34: 3035-87. 10.1093/eurheartj/eht108. 23996285 [DOI] [PubMed] [Google Scholar]
- 50.Bushnell C, McCullough L. Stroke prevention in women: synopsis of the 2014 American Heart Association/American Stroke Association guideline. Ann Intern Med 2014;160: 853-7. 10.7326/M14-0762. 24935489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Humphries KH, Kerr CR, Connolly SJ etal. New-onset atrial fibrillation: sex differences in presentation, treatment, and outcome. Circulation 2001;103: 2365-70. 10.1161/01.CIR.103.19.2365 11352885 [DOI] [PubMed] [Google Scholar]
- 52.Lip GYH, Rushton-Smith SK, Goldhaber SZ etalGARFIELD-AF Investigators. Does sex affect anticoagulant use for stroke prevention in nonvalvular atrial fibrillation? The prospective global anticoagulant registry in the FIELD-Atrial Fibrillation. Circ Cardiovasc Qual Outcomes 2015;8(Suppl 1): S12-20. 10.1161/CIRCOUTCOMES.114.001556. 25714828 [DOI] [PubMed] [Google Scholar]
- 53.Avgil Tsadok M, Jackevicius CA, Rahme E, Humphries KH, Behlouli H, Pilote L. Sex differences in stroke risk among older patients with recently diagnosed atrial fibrillation. JAMA 2012;307: 1952-8. 10.1001/jama.2012.3490. 22570463 [DOI] [PubMed] [Google Scholar]
- 54.Roden DM, Kannankeril P, Darbar D. On the relationship among QT interval, atrial fibrillation, and torsade de pointes. Europace 2007;9(Suppl 4): iv1-3. 10.1093/europace/eum165. 17766319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alotaibi GS, Almodaimegh H, McMurtry MS, Wu C. Do women bleed more than men when prescribed novel oral anticoagulants for venous thromboembolism? A sex-based meta-analysis. Thromb Res 2013;132: 185-9. 10.1016/j.thromres.2013.07.017. 23932014 [DOI] [PubMed] [Google Scholar]
- 56.Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJGM. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010;137: 263-72. 10.1378/chest.09-1584. 19762550 [DOI] [PubMed] [Google Scholar]
- 57.Bushnell C, McCullough LD, Awad IA etalAmerican Heart Association Stroke Council Council on Cardiovascular and Stroke Nursing Council on Clinical Cardiology Council on Epidemiology and Prevention Council for High Blood Pressure Research. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45: 1545-88. 10.1161/01.str.0000442009.06663.48. 24503673 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix: Supplementary tables A and B; figures A-G; extra references