Abstract
Background:
Australian Rules football is a highly aerobic and anaerobic game that at times requires players to perform cutting or pivoting maneuvers, potentially exposing them to anterior cruciate ligament (ACL) injury. At present, there are limited data available addressing the impact of ACL injury on return to play and preinjury form after ACL reconstruction.
Purpose:
To determine the prevalence of ACL injury and the incidence of further ACL injury, and to consider player return to play and return to preinjury form after ACL reconstruction. It was hypothesized that elite-level Australian Football League (AFL) players do not return to preinjury form until, at minimum, 2 years after returning to play.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective analysis was undertaken on a cohort of elite AFL players who injured their ACL between 1990 and 2000. Return to play after ACL reconstruction was determined by the mean number of ball disposals, or release of the ball by the hand or foot, at 1, 2, and 3 years after return to play and compared with preinjury form. Associations between player and injury characteristics, method of reconstruction, and outcomes (return to play, preinjury form, and further ACL injury) were examined.
Results:
During the included seasons, a total of 2723 AFL players were listed. Of these, 131 (4.8%) sustained an ACL injury, with 115 players eligible for inclusion. Of 115 players, 26% did not return to elite competition, while 28% of those who did return experienced further ACL injury. The adjusted mean number of disposals (± standard error of the mean) was significantly lower at 1 year (12.21 ± 0.63; P = .003), 2 years (12.09 ± 0.65; P = .008), and 3 years (11.78 ± 0.77; P = .01) after return to play compared with preinjury (14.23 ± 0.67). On average, players did not return to preinjury form by 3 years (P < .01). Players aged 30 years or older were less likely to return to play compared with younger players (P = .0002), moderate-weight players were more likely to return to play compared with lighter-weight players (P = .007), and there were significantly increased odds of not returning to play if the dominant side was injured (odds ratio, 0.10; 95% CI, 0.03-0.34; P = .0002).
Conclusion:
On average, AFL players do not return to their preinjury form after ACL injury and reconstruction, a common injury in this sporting population. This along with the high occurrence of reinjury highlights the career-threatening nature of ACL injury for elite AFL players.
Keywords: anterior cruciate ligament, sports injury, Australian Rules football, functional outcome, ACL reconstruction
Australian Rules football played under the auspices of the Australian Football League (AFL) is a highly athletic game. It is played over 120 minutes on a grass surface oval in shape, which measures between 135 and 185 m long by 110 and 155 m wide. From initiation to 2008, the elite competition was made up of 16 teams, which at present has increased to 18. Teams have 40 listed players, from which 22 are selected to play per week.
The season runs from March to October inclusive. Twenty-four minor round games are played, and this is followed by a finals series. The break between games is no less than 4 days and no more than 8 days. In addition to this playing time, players begin formal preseason training 6 weeks after their last game and have 6 weeks of preseason games to attain match fitness.
During the game, which is both highly aerobic and anaerobic, players are required to make and avoid contact with the opposition while coordinating ball skills and disposing of the ball by hand (handball) or by foot (kick). As there are no “offside” rules in AFL football, the ball may be disposed of in any direction and, similarly, tackles may come from any direction, necessitating that players perform a large number of cutting and pivoting maneuvers (Figure 1).
Figure 1.

Match photograph of an Australian Rules football player with ball possession performing a cutting and pivoting maneuver while being tackled by 2 opposing team players from 2 directions. Used with acknowledgment: Ray Titus, photographer, The Advertiser Newspapers Ltd.
The anterior cruciate ligament (ACL) is one of the most common areas that can be injured during sports, particularly those involving cutting and pivoting.5,13,19 The prevalence of ACL injury in Australian Rules football players at all levels has been attributed, in part, to these maneuvers.5,13,19,20 Other factors, including previous ACL injury, narrow intercondylar notch, female sex, hormonal factors, familial tendency, and extrinsic environmental factors such as shoe surface interference, weather conditions, playing surface hardness, and grass type, have also been associated with an increased risk of ACL injury in sporting populations.18–23
Reconstruction of the ACL is commonly performed to restore knee stability to enable athletes to return to their sport. From 2003 to 2008, approximately 10,000 ACL reconstructions were reported in Australia annually, with AFL football identified as the second most frequent sport played at the time of injury.12 Players do return to play AFL football after ACL reconstruction; however, the functional outcomes, and whether these players return to their preinjured form, have not been explored. A good functional outcome after ACL injury maintains that players return to the elite level of play, quickly return to their preinjury form, and have a low likelihood of further injury after return. Such an outcome is of major importance to elite players, particularly in terms of their professional earning capacity; it is also important to the team, the coach, team administrators and, not least, the spectators, all of whom want the best players selected to produce optimal results.
Managing the impact of ACL injury in elite AFL players may only be improved by better data on the outcomes of this injury. Objective and subjective outcomes after ACL reconstruction have been reported using a number of different knee-rating questionnaires.1,2,15,28 Although many of the knee ratings include a functional outcomes domain that enables comparison of results across different cohorts, the questions asked are not specific to the sporting population. In elite athletes, highly important outcomes are the ability to return to their sport and the ability to return to their preinjury level of sporting performance. To objectively measure this, sport-specific outcomes are required. For AFL football during the period of data collection, the total number of ball disposals, representing handballs and kicks, was regarded as the key player-performance indicator, independent of player position.
The primary objective of this study was to use AFL football–specific objective functional outcomes (total ball disposals) to examine if players who return to play after ACL injury return to their preinjury playing form. The characteristics of AFL football players who sustained ACL injuries while playing at the elite level were also described and, using multivariate analysis, the player and injury characteristics that influenced return to play, return to form, and occurrence of subsequent ACL injury were examined. It was hypothesized that elite-level AFL players do not return to preinjury form until, at minimum, 2 years after return to play.
Methods
A retrospective analysis was undertaken on a cohort of listed AFL players who played at the elite level from 1990 to the end of the 2000 final series. Players were identified using prospective records made available by the AFL Medical Officers Association (AFLMOA). The AFLMOA released these data in accordance with Privacy and Player Consent Guidelines for ethical observational research; retrospective approval was also received from a human research ethics committee. All data were deidentified for the purpose of analysis.
The AFLMOA provided data regarding injury and ACL injury management, including the surgical procedure performed. Listed players who sustained a first-time ACL injury that was surgically treated were included in the study cohort. Player characteristic data included age, height, and weight at the time of injury. Injury data included side of the injury, whether it was the dominant or nondominant side, surgical reconstruction technique, if and when players returned to play at the elite level, and if they sustained a further ipsilateral or contralateral ACL injury. The timing of the return to play was categorized as less than 1 year, or 1 year or longer after injury.
To determine players’ return to form, AFL match statistics data on the players’ average total ball disposals for the 5 games preinjury were compared with their average total disposals at the 5 games closest to 1, 2, and 3 years after return to play. The criterion for return to preinjury form was that the players’ number of disposals postinjury was equal to or greater than the number of disposals before their injury.
Statistical analyses were performed using SAS V9.1 software (SAS Institute Inc). Player and injury characteristics were categorized for analyses (Tables 1–3). Repeated-measures binomial logit generalized estimating equations were used to determine associations between player and injury characteristics on 3 main outcomes: (1) whether a player returned to play, (2) whether a player was reinjured, and (3) whether the player returned to preinjury form. Odds ratios (ORs) were determined and post hoc comparisons of incidences were undertaken using the chi-square test. To examine the association between player and injury characteristics and the extent of player return to preinjury form, a mixed-model repeated-measures analysis of variance of the outcome (average number of disposals) was performed with the repeated measures being the time points preinjury and 1, 2, and 3 years after return to play. Disposals were adjusted for player and injury characteristics, which were entered as interactive terms. Statistical significance was set at 5%, but near-significant effects for interactive terms were also investigated in an exploratory manner.
TABLE 1.
Player and Injury Characteristics of Elite Australian Rules Football Players With ACL Injuries During 1990-2000: Return to Play at the Elite Levela
| All Players (Range) [% of Overall Category] | Did Not Return to Play (Range) [% of Each Subcategory] | Returned to Play (Range) [% of Each Subcategory] | Return to Play After ACL Injury Compared With Reference Group, OR [95% CI] (P Value)b | |
|---|---|---|---|---|
| No. of players | 115 | 30 [26] | 85 [74] | |
| Mean age, y | 24 (17-35) | 25 (20-35) | 23 (17-32) | |
| 17-20c | 17 [15] | 1 [6] | 16 [94] | — |
| 21-24 | 58 [50] | 17 [29] | 41 [71] | 0.16 [0.02-1.19] (.073) |
| 25-29 | 34 [30] | 8 [24] | 26 [76] | 0.24 [0.03-2.16] (.205) |
| 30+ | 6 [5] | 4 [67] | 2 [33] | 0.01 [0.00-0.12] (<.0002) |
| Mean height, cm | 185 (163-203) | 183 (173-193) | 185 (163-203) | |
| <179c | 34 [30] | 10 [29] | 24 [71] | — |
| 180-189 | 45 [39] | 13 [29] | 32 [71] | 0.46 [0.09-2.15] (.323) |
| >190 | 36 [31] | 7 [19] | 29 [81] | 0.29 [0.05-1.63] (.161) |
| Mean weight, kg | 88 (70-109) | 84 (70-102) | 89 (73-109) | |
| 70-79c | 26 [23] | 10 [38] | 16 [62] | — |
| 80-89 | 43 [37] | 13 [30] | 30 [70] | 3.22 [0.68-15.12] (.139) |
| 90-99 | 34 [30] | 6 [18] | 28 [82] | 14.93 [2.13-104.76] (.007) |
| 100+ | 12 [10] | 1 [8] | 11 [92] | 17.77 [0.60-522.038] (.095) |
| Side of injuryd | ||||
| Nondominantc | 61 [53] | 7 [11] | 54 [89] | — |
| Dominant | 54 [47] | 23 [43] | 31 [57] | 0.10 [0.03-0.34] (.0002) |
| Surgical techniqued | ||||
| HSc | 39 [34] | 9 [23] | 30 [77] | — |
| BPTB | 72 [63] | 20 [28] | 52 [72] | 0.73 [0.23-2.37] (.601) |
| ITB | 3 [3] | 1 [33] | 2 [67] | 0.35 [0.01-8.27] (.515) |
aStatistics in bold are significant. ACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone autograft; HS, hamstring tendon autograft; ITB, iliotibial band autograft; OR, odds ratio.
bAdjusted OR—for covariates, binomial logit generalized estimating equations.
cReference group.
dThe type of ACL reconstruction technique was not documented for 1 player.
TABLE 2.
Player and Injury Characteristics of Elite Australian Rules Football Players Who Returned to Play After ACL Injury: Further Injuries to the ACLa
| All Players (Range) [% of Overall Category] | No Further Injury (Range) [% of Each Subcategory] | Further Injury (range) [% of Each Subcategory] | Further ACL Injury After Index Injury Compared With Reference Group, OR [95% CI] (P Value)b | |
|---|---|---|---|---|
| No. of players | 85 | 61 [72] | 24 [28] | |
| Mean age, y | 23 (17-32) | 24 (17-31) | 23 (17-32) | |
| 17-20c | 16 [19] | 12 [75] | 4 [25] | — |
| 21-24 | 41 [48] | 26 [63] | 15 [37] | 1.87 [0.42-8.21] (.409) |
| 25-29 | 26 [31] | 22 [85] | 4 [15] | 0.69 [0.12-3.76] (.664) |
| 30+ | 2 [2] | 1 [50] | 1 [50] | 3.54 [0.14-87.1] (.439) |
| Mean height, cm | 185 (163-203) | 185 (173-201) | 187 (163-203) | |
| <179c | 24 [28] | 19 [79] | 5 [21] | — |
| 180-189 | 32 [38] | 25 [78] | 7 [22] | 1.22 [0.31-4.81] (.782) |
| ≥190 | 29 [34] | 17 [59] | 12 [41] | 2.49 [0.32-19.58] (.385) |
| Mean weight, kg | 89 (73-109) | 87 (73-105) | 92 (75-109) | |
| 70-79c | 16 [19] | 13 [81] | 3 [19] | — |
| 80-89 | 30 [35] | 22 [73] | 8 [27] | 1.40 [0.28-6.90] (.682) |
| 90-99 | 28 [33] | 21 [75] | 7 [25] | 0.81 [0.11-5.98] (.834) |
| 100+ | 11 [13] | 5 [45] | 6 [55] | 1.68 [0.14-20.69] (.687) |
| Side of injury | ||||
| Nondominantc | 54 [64] | 36 [68] | 17 [32] | — |
| Dominant | 31 [36] | 24 [77] | 7 [23] | 0.74 [0.24-2.28] (.599) |
| Surgical techniqued | ||||
| HSc | 30 [35] | 22 [73] | 8 [27] | — |
| BPTB | 52 [61] | 36 [69] | 16 [31] | 1.42 [0.49-4.08] (.519) |
| ITB | 2 [2] | 2 [100] | 0 | |
| Timing of return | ||||
| <1 y after injuryc | 41 [48] | 27 [66] | 14 [34] | — |
| 1 y or longer | 44 [52] | 34 [77] | 10 [23] | 0.61 [0.21-1.80] (0.370) |
aACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone autograft; HS, hamstring tendon autograft; ITB, iliotibial band autograft; OR, odds ratio.
bAdjusted OR—for covariates, binomial logit generalized estimating equations.
cReference group.
dThe type of ACL reconstruction technique was not documented for 1 player.
TABLE 3.
Player and Injury Characteristics of Elite Australian Rules Football Players Who Returned to Play After ACL Injury: Return to Preinjury Forma
| All Players (Range) [% of Overall Category] | Did Not Return to Form (Range) [% of Each Subcategory] | Returned to Form (Range) [% of Each Subcategory] | Return to Preinjury Form Compared With Reference Group, OR [95% CI] (P Value)b | |
|---|---|---|---|---|
| No. of players | 71 | 35 [49] | 36 [51] | |
| Mean age, y | 24 (18-32) | 24 (19-32) | 24 (18-28) | |
| 17-20c | 10 [14] | 4 [40] | 6 [60] | — |
| 21-24 | 36 [51] | 18 [50] | 18 [50] | 0.34 [0.08-2.08] (.283) |
| 25-29 and 30+ | 25 [35] | 13 [52] | 12 [48] | 0.58 [0.12-3.68] (.632) |
| Mean height, cm | 185 (163-203) | 184 (174-203) | 186 (163-201) | |
| <179c | 21 [30] | 13 [62] | 8 [38] | — |
| 180-189 | 27 [38] | 12 [44] | 15 [56] | 1.67 [0.64-9.33] (.194) |
| >190 | 23 [32] | 10 [43] | 13 [57] | 1.75 [0.23-12.81] (.605) |
| Mean weight, kg | 89 (73-109) | 88 (73-106) | 89 (74-109) | |
| 70-79c | 13 [18] | 6 [46] | 7 [54] | — |
| 80-89 | 26 [37] | 16 [62] | 10 [38] | 0.38 [0.11-2.23] (.354) |
| 90-99 | 22 [31] | 9 [41] | 13 [59] | 0.93 [0.16-6.14] (.997) |
| 100+ | 10 [14] | 4 [40] | 6 [60] | 1.83 [0.11-17.82] (.787) |
| Side of injury | ||||
| Nondominantc | 44 [63] | 24 [55] | 20 [45] | — |
| Dominant | 27 [37] | 11 [41] | 16 [59] | 1.51 [0.55-4.15] (.426) |
| Surgical techniqued | ||||
| HSc | 26 [40] | 12 [43] | 14 [57] | — |
| BPTB | 42 [60] | 23 [55] | 19 [45] | 0.29 [0.18-1.53] (.239) |
| ITB | 2 | 0 | 2 | |
| Timing of return | ||||
| <1 y after injuryc | 38 [54] | 20 [53] | 18 [47] | – |
| 1 y or longer | 33 [46] | 15 [45] | 18 [55] | 0.51 [0.35-2.73] (.97) |
aComplete player match statistics data available for 71 of the 85 players who returned to play after injury. ACL, anterior cruciate ligament; BPTB, bone–patellar tendon–bone autograft; HS, hamstring tendon autograft; ITB, iliotibial band autograft; OR, odds ratio.
bAdjusted OR—for covariates, binomial logit generalized estimating equations.
cReference group.
dThe type of ACL repair technique was not documented for 1 player.
Results
ACL Injury Prevalence
During the 1990 to 2000 seasons, 2723 AFL players were listed. Of these listed players, 131 players sustained an ACL injury, giving an ACL injury prevalence of 4.8%. Fourteen of the players who experienced an ACL injury had not played at the elite level by the time of the injury and were therefore excluded from the study. A further 2 players did not have a documented ACL reconstruction and were also excluded. The study cohort included a total of 115 AFL players who played at the elite level, incurred an ACL knee injury, and were documented as having undergone ACL surgical reconstruction.
Sixty injuries occurred in the left knee (52%) and 55 in the right knee (48%). The characteristics of the injured players and the injury are summarized in Table 1. Fifty-four injuries occurred on the dominant side (47%) and 61 on the nondominant side (53%). Seventy-two (63%) knees were reconstructed using the bone–patellar tendon–bone (BPTB) autograft technique, 39 (34%) with the hamstring tendon (HS) autograft technique, and 3 knees (3%) with an iliotibial band (ITB) extra- and intra-articular autograft technique. The ACL reconstruction technique used was not adequately documented for 1 player.
Return to Play
Thirty of the 115 players (26%) did not return to play AFL football at the elite level after injury and ACL reconstruction. A total of 85 players (74%) returned to play at the elite level. Of these 85, 41 (48%) players returned at less than 1 year after injury, while 44 (52%) returned at 1 year or longer after injury.
After adjustment for all player and injury characteristics, side of injury, player age, and player weight were identified as significantly associated with returning to play at the elite level (Table 1). Players were 9 times less likely to play again if their dominant side was injured compared with their nondominant side (OR = 0.10, 95% CI = 0.03-0.34, P = .002). When compared with players aged between 17 and 20 years, older players displayed a tendency to be less likely to return to play at the elite level, with a significant association identified for players aged 30 years or older (Table 1) (OR, 0.01; 95% CI, 0.00-0.12; P < .0002). Heavier players displayed a tendency to be more likely to return to play at the elite level when compared with lighter players (70-79 kg). Players weighing between 90 and 99 kg were nearly 15 times more likely to return to play at the elite level (OR, 14.93; 95% CI, 2.13-104.76; P = .007).
Reinjury
Of the 85 players who returned to play at the elite level, 24 (28%) had a further ACL injury. Fourteen players had reinjury to the ipsilateral knee (16% of returned players) and 10 players injured their contralateral knee (12% of returned players). Fourteen further ACL injuries occurred in the 41 players who returned within 1 year of the original injury (34%), while an additional 10 injuries occurred in the 44 players (23%) who returned at 1 year or longer after the original injury. After adjusting for all player and injury characteristics, there were no characteristics that were associated with the outcome of further ACL injury (Table 2).
Of the 14 reinjuries to the ipsilateral knee, 11 knees were reconstructed using the BPTB technique and 3 with the HS technique. Ten of the 41 (24%) players who returned within 1 year after injury reinjured their ipsilateral knee, as compared with 4 of the 44 players (9%) who returned at more than 1 year (OR, 0.31; 95% CI, 0.09-1.08; P = .079). Of the 10 players who reinjured their ipsilateral knee after return to play within 1 year, 2 had received an HS autograft, compared with 8 players who received a BPTB autograft.
Return to Form
Sufficient match statistics data were available for 71 of the 85 players who returned to play after ACL injury (84%), allowing analysis of return to form after injury. The adjusted mean number (± standard error of the mean [SEM]) of disposals for the 5 games prior to injury was 14.23 ± 0.67. On average, players who returned to play at the elite level after ACL injury and reconstruction did not return to preinjury form within 3 years of return to play. The adjusted mean number (±SEM) of disposals was significantly lower at 1 year (12.21 ± 0.63; P = .003), 2 years (12.09 ± 0.65; P = .008), and 3 years (11.78 ± 0.77; P = .01) after return to play compared with the preinjury disposals (Figure 2). There were no statistically significant differences in the adjusted mean number of disposals between 1, 2, and 3 years after return to play. In comparison with preinjury disposals, the mean percentage of disposals at 1, 2, and 3 years after return to play were 90.6%, 88.6%, and 84.6%, respectively. Using adjusted means, the percentage of disposals in comparison with preinjury at 1, 2, and 3 years after return to play were 85.8%, 85.0%, and 82.8%, respectively. Adjusting for all player and injury characteristics demonstrated no significant association with whether a player returned to preinjury form at any time point after return to play (Table 3).
Figure 2.
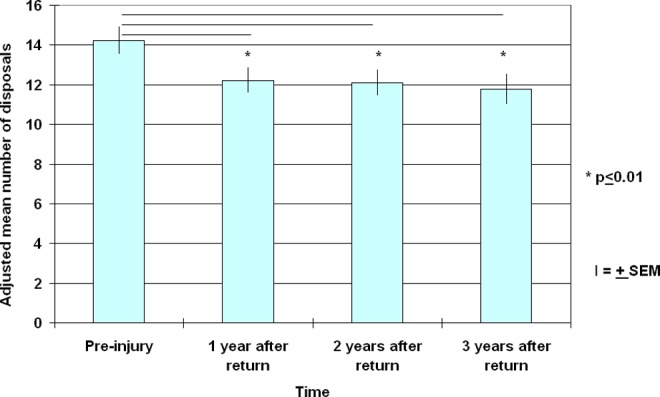
Player performance, measured by adjusted mean number of disposals over 5 games, before injury and at 1, 2, and 3 years after return to play.
Significant changes were identified in player form over time according to player age group and ACL reconstruction technique. For players in the 25- to 29-year age group, there was no significant change in adjusted mean number of disposals between preinjury and at 1 or 2 years after return to play. In contrast, significant reductions in the adjusted mean number of disposals at 1 year after return to play were identified for players in the 17–20, 21–24, and 30 years or older age groups, when compared with their preinjury form (Figure 3). These 3 age groups also displayed subsequent significant improvement in the adjusted mean number of disposals from 1 to 2 years after return to play.
Figure 3.
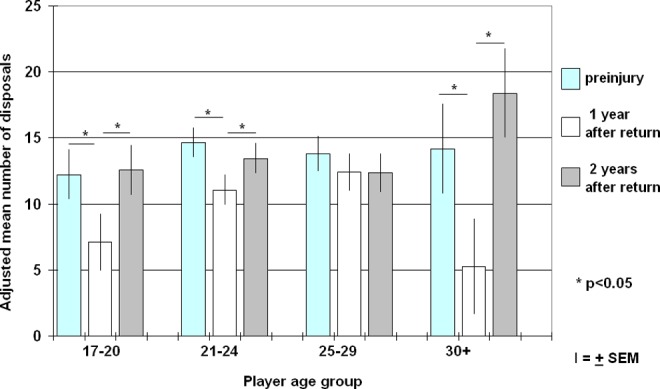
Adjusted mean number of disposals at 1 and 2 years after return to play, according to player age.
For players who underwent reconstruction with the HS technique, although there was a decrease in the number of disposals, there was no significant change in the average number of disposals between preinjury and 1 and 2 years after return to play (Figure 4). In contrast, the average number of disposals was significantly lower 1 year after return to play compared with preinjury for those players with BPTB reconstruction (P < .0001). At 2 years after return to play, there was a significant improvement in the average number of disposals compared with that at 1 year for players who underwent BPTB surgery (P = .001). For both groups, the average number of disposals at 2 years after return was not significantly different from that at preinjury.
Figure 4.
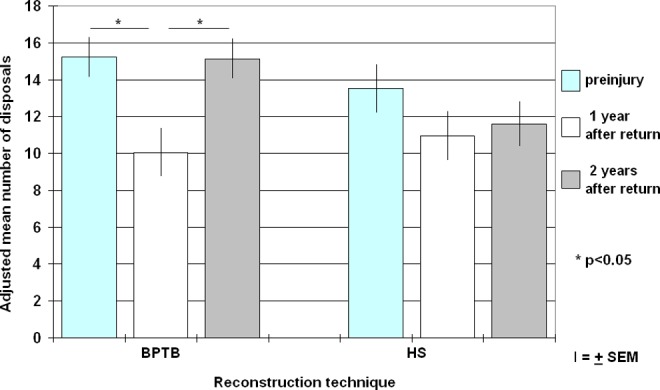
Adjusted mean number of disposals at 1 and 2 years after return to play according to anterior cruciate ligament reconstruction technique. BPTB, bone–patellar tendon–bone; HS, hamstring.
Discussion
Reconstruction of the ACL has been shown to restore stability to the unstable knee and enable return to sporting activities.8,10,11,14,27 However, the level of performance achieved after ACL reconstruction in the elite athlete has rarely been reported. This study is the first formal analysis, using objective player-relevant quantitative match statistics data, to examine return to form in elite AFL players after ACL knee injury and reconstruction. A poor functional outcome, defined as either not returning to play at the elite level or a subsequent ACL injury, occurred in 47% of players in this elite sporting population. Furthermore, for those players who returned to the elite level, this study suggests that on average, they were unlikely to return to preinjury form within 3 years of the injury. We were therefore unable to support our study hypothesis that elite-level AFL players do not return to preinjury form until at least 2 years after injury.
A total of 26% of AFL players did not return to play at the elite level after ACL injury. This finding is similar to that reported by Carey et al4 for a study of elite National Football League players, which showed that 21% of players did not return to play at the elite level. We found that players who did not return to play at the elite level were 9 times more likely to have injured their dominant side than their nondominant side. In Australian Rules football, players kick most often with their dominant leg; furthermore, players rely on the strength of their dominant leg to coordinate the pivoting, twists, turns, jumps, and landings that are required to make and break tackles, which are fundamental to the AFL football game. Thus, proprioreceptive factors, as well as muscle strength and coordination, may play a role in why these players who have injured their dominant leg find it more difficult to return.
The BPTB technique was used to treat 63% of knees, compared with 34% of knees where the HS method was used. This frequency is a reflection of surgical experience and preference during the 1990s in Australia, and it also represents the international preference.3 Both the BPTB and HS techniques have been reported to be equally effective; however, in this AFL population, neither technique ensured return to play.
The outcomes of ACL reconstruction have been extensively studied, as has the comparison of different open and arthroscopic procedures as well as the different types of grafts utilized. A meta-analysis6 found that both the BPTB and the HS techniques provided stability to the knee and that, for both techniques, two-thirds of all patients, regardless of sporting participation prior to ACL injury, returned to their preinjury level of activity.
The bone-to-bone fixation of the BPTB technique is thought to allow for earlier and stronger graft incorporation and thus accelerated rehabilitation, avoidance of complications, and earlier return to sport.9,25,29,30 These assumptions are, however, contentious and have yet to be supported adequately by valid data. Our analysis of an AFL football cohort suggests that rehabilitation is longer after BPTB reconstruction. We found that return to form, in terms of disposals, drops off significantly in the first year after return to play but returns to preinjury form by 2 years for players who underwent BPTB reconstruction. In contrast, after HS reconstruction, there was no significant change in form, suggesting that in this cohort, HS reconstruction may yield better early results. Tunnel placement for ACL reconstruction has become increasingly anatomic. Throughout the 1990s, most ACL reconstructions were performed using the transtibial approach. With the advent of more surgeons using a medial portal approach to the femoral tunnel, anatomic femoral tunnel position was more likely to be achieved. By correcting the surgical tunnel position, improved outcomes may be achieved.
We found that 28% of players who returned at the elite level had a further ACL injury on either the ipsilateral or contralateral knee. A similar prevalence of further knee injury was found in a 10-year prospective longitudinal study of a mixed population of ACL injuries.24 In our study, the prevalence of reinjury to the ipsilateral knee only was 16%, which could represent the prevalence of graft failure for this population. This prevalence was higher for players originally treated by BPTB technique (22%) compared with players originally treated by HS reconstruction (7%), again suggesting a place for HS over BPTB reconstruction for this player cohort. Regardless, this reinjury prevalence is considerably higher than the 2% prevalence of patellar tendon graft failure and 5% prevalence for hamstring graft failure reported by D’Amato and Bach.6 This possibly shows that at the elite level of the AFL, the physical contact combined with the cutting and pivoting skills required of players may expose the reconstructed knees to more physical stresses than in other sports.
In their study of elite National Football League players, Carey et al4 found a statistically significant reduction in player form, defined as running and wide receiver performance, on return to competition after ACL injury. In our study, there were some players whose postinjury disposal statistics at early return to play were superior to others, although after controlling for potentially confounding variables, player or injury characteristics that were associated with increased odds of returning to form at any time point after ACL injury were not found. If the player and injury characteristics that are associated with increased odds of returning to play after injury are known, and also the characteristics of players who performed better than others after return from injury, guidelines for player rehabilitation could be given. These would include expectations regarding return to play, likelihood of reinjury, and probability of return to preinjury form, which could also facilitate planning at the club level. In the present study, the characteristics associated with increased odds of returning to play after injury were younger age, moderate weight, and injury of the nondominant side.
Study results found no significant difference in player form over time when comparing players who returned at less than 1 year after injury with those who returned at 1 year or longer after injury. Therefore, no data supported an early return to play, based purely on return to form. Twenty-four percent of players who returned within 1 year after injury reinjured their ipsilateral knee, compared with 9% of players who returned at more than 1 year. Although not statistically significant (P = .079), the trend for greater odds of reinjury to the ipsilateral knee in the early-return-to-play group is important. Thus, a minimum of 1 year after ACL injury and reconstruction is recommended as the appropriate amount of time before returning to play at the elite level in the AFL. Although in other sports, a shorter time to return to play after injury has proven to be successful,7,16,17,26 there may be sufficient differences in the extent of physical contact and cutting and pivoting maneuvers in AFL and thus demands on reconstructed knees to justify this longer recommendation.
Return to sport, regardless of the level, is heavily reliant on player confidence that the knee is stable in elite-level game situations, confidence being gained from both player intuition and also from medical advice. In elite sports, where other players are readily available on lists and commercial interests are at stake, delays in restoration of player confidence are not tolerated. Thus, the medical community, sporting clubs, coaching staff, and players need to accept the responsibility of medical and psychological rehabilitation of the injured athlete to allow them to return to play in their best medical and psychological fitness, and with the least chance of reinjury.
A limitation of this study is that data on the complications of ACL reconstruction surgery were not available. Graft harvest morbidity, including patellar tendinitis, patellar fracture, patellar tendon rupture, anterior knee pain, and numbness, are infrequent but important complications that can occur in this elite sporting population and that may have contributed to the results reported. A second limitation is the age of the data reported and analyzed in this study. However, more recent publications have not assessed total ball disposals, which could be considered a more relevant player-performance indicator for outcomes related to AFL football athletes.
Conclusion
This retrospective longitudinal study has produced objective data that demonstrate the potentially career-threatening outcome of ACL injuries in elite AFL football players. The findings of this study may assist players, coaches, clubs, and supporters with their expectations of players after ACL injury. Furthermore, these results provide an opportunity for players, coaches, and clubs to establish objective criteria on which decisions can be made regarding whether players should return from ACL injury and, if so, the timing of return to elite-level competition. In view of these findings, the orthopaedic community should also review their expectations of current management of elite AFL players with ACL injuries, in particular with regard to timing of return and potential recurrence rates.
Acknowledgment
The authors thank the Australian Football League for providing the player match statistics; Thomas Sullivan and Justin Lokhorst, Department of Public Health, University of Adelaide, for undertaking the statistical analyses; Margaret McGee and Jill Pope for assistance with the preparation of this article; and Annika Theodoulou, International Musculoskeletal Research Institute Inc and Flinders University, for manuscript review, editing, and preparation for journal submission and publication.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Research Ethics Committee at Royal Adelaide Hospital and the Australian Football League Medical Officers Association.
References
- 1. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; and International Knee Documentation Committee. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34:128–135. [DOI] [PubMed] [Google Scholar]
- 2. Barber-Westin SD, Noyes FR, McCloskey JW. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati knee rating system in 350 subjects with uninjured, injured, or anterior cruciate ligament–reconstructed knees. Am J Sports Med. 1999;27:402–416. [DOI] [PubMed] [Google Scholar]
- 3. Bartlett RJ, Clatworthy MG, Nguyen TN. Graft selection in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2001;83:625–634. [DOI] [PubMed] [Google Scholar]
- 4. Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34:1911–1917. [DOI] [PubMed] [Google Scholar]
- 5. Cochrane JL, Lloyd DG, Buttfield A, Seward H, McGivern J. Characteristics of anterior cruciate ligament injuries in Australian football. J Sci Med Sport. 2007;10:96–104. [DOI] [PubMed] [Google Scholar]
- 6. D’Amato MJ, Bach BR. Anterior cruciate ligament injuries in the adult In: DeLee JC, Drez D, Jr, eds. Orthopaedic Sports Medicine. Anterior Cruciate Ligament Injuries, Vol 2. Philadelphia, PA: WB Saunders; 2003:2012–2067. [Google Scholar]
- 7. Delay BS, Smolinski RJ, Wind WM, Bowman DS. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. Am J Knee Surg. 2001;14:85–91. [PubMed] [Google Scholar]
- 8. Feller JA, Cooper R, Webster KE. Current Australian trends in rehabilitation following anterior cruciate ligament reconstruction. Knee. 2002;9:121–126. [DOI] [PubMed] [Google Scholar]
- 9. Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1997;79:1556–1576. [DOI] [PubMed] [Google Scholar]
- 10. Gobbi A, Diara A, Mahajan S, Zanazzo M, Tuy B. Patellar tendon anterior cruciate ligament reconstruction with conical press-fit femoral fixation: 5-year results in athletes population. Knee Surg Sports Traumatol Arthrosc. 2002;10:73–79. [DOI] [PubMed] [Google Scholar]
- 11. Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14:1021–1028. [DOI] [PubMed] [Google Scholar]
- 12. Janssen KW, Orchard JW, Driscoll TR, van Mechelen W. High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003-2004 to 2007-2008: time for an anterior cruciate ligament register by Scandinavian model? Scand J Med Sci Sports. 2012;22:495–501. [DOI] [PubMed] [Google Scholar]
- 13. Junge A, Dvorak J, Graf-Baumann T, Peterson L. Football injuries during FIFA tournaments and the Olympic Games, 1998-2001: development and implementation of an injury-reporting system. Am J Sports Med. 2004;32(suppl 1):80S–89S. [DOI] [PubMed] [Google Scholar]
- 14. Kaplan MJ, Howe JG, Fleming B, Johnson RJ, Jarvinen M. Anterior cruciate ligament reconstruction using quadriceps patellar tendon graft. Part II. A specific sport review. Am J Sports Med. 1991;19:458–462. [DOI] [PubMed] [Google Scholar]
- 15. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. [DOI] [PubMed] [Google Scholar]
- 16. MacDonald PB, Hedden D, Pacin O, Huebert D. Effects of an accelerated rehabilitation program after anterior cruciate ligament reconstruction with combined semitendinosus-gracilis autograft and a ligament augmentation device. Am J Sports Med. 1995;23:588–592. [DOI] [PubMed] [Google Scholar]
- 17. Marcacci M, Zaffagnini S, Iacono F, et al. Intra- and extra-articular anterior cruciate ligament reconstruction utilizing autogeneous semitendinosus and gracilis tendons: 5-year clinical results. Knee Surg Sports Traumatol Arthrosc. 2003;11:2–8. [DOI] [PubMed] [Google Scholar]
- 18. Orchard J. Is there a relationship between ground and climatic conditions and injuries in football? Sports Med. 2002;32:419–432. [DOI] [PubMed] [Google Scholar]
- 19. Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997-2000. Br J Sports Med. 2002;36:39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29(2):196–200. [DOI] [PubMed] [Google Scholar]
- 21. Orchard J, Seward H, McGivern J, Hood S. Rainfall, evaporation and the risk of non-contact anterior cruciate ligament injury in the Australian Football League. Med J Aust. 1999;170:304–306. [DOI] [PubMed] [Google Scholar]
- 22. Orchard J, Wood T, Seward H, Broad A. Comparison of injuries in elite senior and junior Australian football. J Sci Med Sport. 1998;1:83–88. [DOI] [PubMed] [Google Scholar]
- 23. Orchard JW, Chivers I, Aldous D, Bennell K, Seward H. Rye grass is associated with fewer non-contact anterior cruciate ligament injuries than Bermuda grass. Br J Sports Med. 2005;39:704–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35:564–574. [DOI] [PubMed] [Google Scholar]
- 25. Safran MR. Graft selection in knee surgery. Current concepts. Am J Knee Surg. 1995;8:168–180. [PubMed] [Google Scholar]
- 26. Shelbourne KD, Urch SE. Primary anterior cruciate ligament reconstruction using the contralateral autogenous patellar tendon. Am J Sports Med. 2000;28:651–658. [DOI] [PubMed] [Google Scholar]
- 27. Smith FW, Rosenlund EA, Aune AK, MacLean JA, Hillis SW. Subjective functional assessments and the return to competitive sport after anterior cruciate ligament reconstruction. Br J Sports Med. 2004;38:279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 29. Webb JM, Corry IS, Clingeleffer AJ, Pinczewski LA. Endoscopic reconstruction for isolated anterior cruciate ligament rupture. J Bone Joint Surg Br. 1998;80:288–294. [DOI] [PubMed] [Google Scholar]
- 30. West RV, Harner CD. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197–207. [DOI] [PubMed] [Google Scholar]


