SUMMARY
Purpose
To explore the association of baseline trabecular bone structure with incident tibiofemoral (TF) osteoarthritis (OA) and with increase in joint space narrowing (JSN) score.
Methods
The Multicenter Osteoarthritis Study (MOST) includes subjects with or at risk for knee OA. Knee radiographs were scored for Kellgren–Lawrence (KL) grade and JSN at baseline, 30, 60 and 84 months. Knees (KL ≤ 1) at baseline were assessed for incident OA (KL≥2) and increases in JSN score. For each knee image at baseline, a variance orientation transform method (VOT) was applied to subchondral tibial bone regions of medial and lateral compartments. Seventeen fractal parameters were calculated per region. Associations of each parameter with OA incidence and with medial and lateral JSN increases were explored using logistic regression. Analyses were stratified by digitized film (DF) vs computer radiography (CR) and adjusted for confounders.
Results
Of 894 knees with CR and 1158 knees with DF, 195 (22%) and 303 (26%) developed incident OA. Higher medial bone roughness was associated with increased odds of OA incidence at 60 and 84 months and also, medial and lateral JSN increases (primarily vertical). Lower medial and lateral anisotropy was associated with increased odds of medial and lateral JSN increase. Compared to DF, CR had more associations and also, similar results at overlapping scales.
Conclusion
Baseline trabecular bone texture was associated with incident radiographic OA and increase of JSN scores independently of risk factors for knee OA. Higher roughness and lower anisotropy were associated with increased odds for radiographic OA change.
Keywords: Trabecular bone, Radiography, Fractal, Radiographic osteoarthritis, Joint space narrowing
Introduction
Trabecular bone is constantly remodeling in response to stress. Different patterns of the bone structure have been detected and studied using texture analysis of plain radiographs. In cross sectional studies, differences have been found in tibial trabecular bone texture between subjects with and without radiographic knee osteoarthritis (OA), and in particular bone texture exhibited higher vertical medial roughness for knees with radiographic OA than control knees1,2. For subjects without radiographic tibiofemoral (TF) knee OA, those with cartilage defects on magnetic resonance imaging (MRI) had the highest vertical medial roughness compared to those without cartilage defects3. Cartilage defects have been shown to occur well before radiographic OA and predict longitudinal cartilage loss4 and joint replacement5. In longitudinal studies, tibial trabecular bone texture predicted an increase of medial joint space narrowing (JSN)6,7. Also, vertical medial trabecular bone texture predicted knee OA progression quantified by changes in medial radiographic and MRI measures of cartilage volumes8.
Those past studies have suggested that trabecular bone texture has a potential for predicting incidence of radiographic knee OA. However, those studies had limitations with regard to their sample size (ranging from 28 to 413), inadequate adjustment for potential confounders and known risk factors (such as age, meniscectomy, knee alignment), and because they included only a single follow-up time-point.
To address such limitations, we present a study in which we explored the association between measures of baseline trabecular bone texture and two radiographic outcomes: (a) radiographic TF OA incidence and (b) an increase in TF JSN score, with the outcomes determined at three follow-up time-points in a large number of subjects. Insights gained from the work could be used in future confirmatory research on a prognostic system for knee OA, including an imaging biomarker useful in the assessment of OA, for the development of disease modifying OA drugs and other treatments (e.g., exercise regimes).
Materials and methods
Subjects
We used data from the Multicenter Osteoarthritis Study (MOST) which is a longitudinal cohort study of 3026 subjects aged 50–79 years at baseline with, and at high risk for, knee OA and examined at 30, 60 and 84 months follow-up visits. Subjects were recruited from two US communities, Birmingham, Alabama and Iowa City, Iowa. The study protocol was approved by the Institutional Review Boards at the University of Iowa (UIowa), University of Alabama (UAB), Birmingham, University of California, San Francisco and Boston University School of Medicine.
We studied subjects without radiographic OA at baseline (Kellgren–Lawrence (KL) 0 or 1) in both knees and who had at least one follow-up X-ray available at 30, 60 or 84-months follow-up. From 6052 knees (3026 subjects) at baseline, 4426 knees (2547 subjects) with KL grade 0 or 1 at baseline were considered eligible for OA incidence and an increase in JSN grade. We excluded knees that had under- or over-exposed radiographs or had grid artifacts visible, or where non-anatomical objects (e.g., clothes) overlaid the subchondral tibial bone. Other exclusions were knee replacement, missing patella, osteonecrosis, amputation, rheumatoid arthritis, fracture, JSN grade = 2 or more at baseline, undetermined TF status at follow-up, missing knee alignment measurement, self-reported knee injury or surgery, leaving 2052 knees (1433 subjects) for analysis (Fig. 1).
Fig. 1.
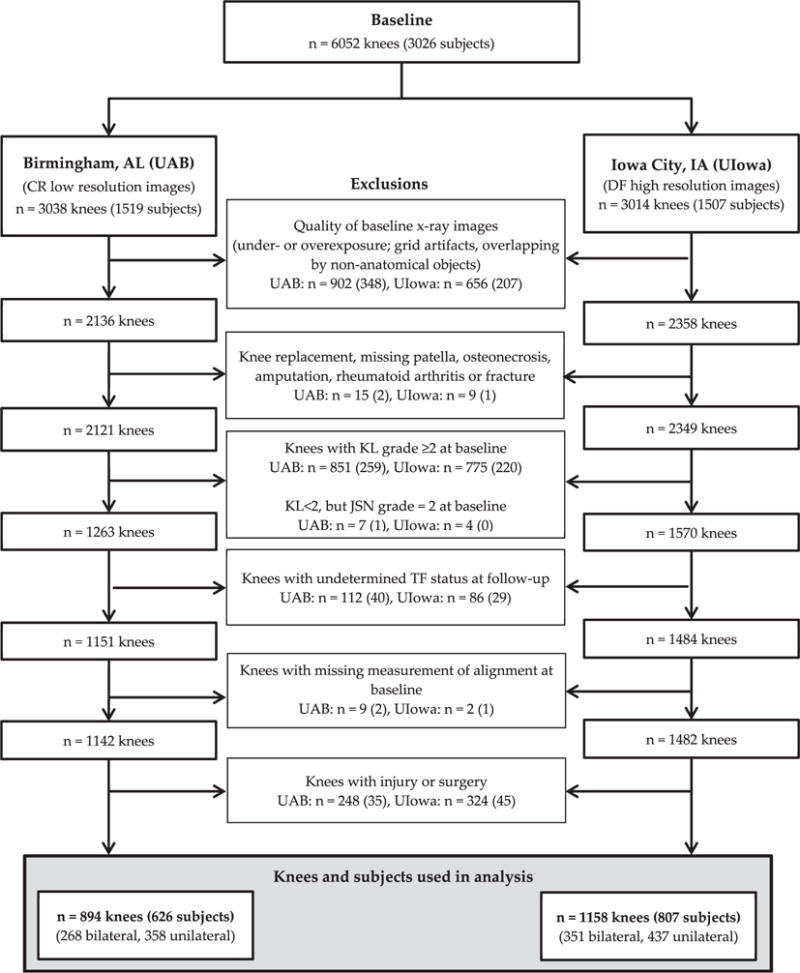
Flow chart of the knee exclusion criteria.
Acquisition of radiographs
Standing posteroanterior (PA) and lateral weight bearing semiflexed radiographs were acquired at baseline and follow-up visits using the MOST study protocols (Section 1 of the Appendix). Knee images were acquired at the UAB clinic using computer radiography (CR; pixel spacing = 0.17 mm), while digitized films (DF; pixel spacing = 0.1 mm) were used at the UIowa clinic.
Grading of knee radiographs and measurement of knee alignment
Radiographs of all knees were read for JSN, osteophytes and KL grade while knee alignment was measured as previously described (Sections 2 and 3 of the Appendix).
Definitions of knee OA incidence and increase in JSN
In knees without TF radiographic OA (KL grade 0 or 1) at baseline, we defined incident OA as a new onset KL grade ≥ 2 N representing development of a definite osteophyte (new or enlarging) at follow-up9 (Table I). Knee OA incidence in MOST can also be defined as the new combination of JSN and a definite osteophyte in a knee with respect to the previous visit10. The definition of OA incidence used in this analysis was more sensitive to OA changes since a knee with KL grade = 2 N does not have to have JSN at the time point when the incidence occurs. Definite osteophytes are sufficient to classify the knee as having OA10.
Table I.
Location and description of TF radiographic OA in knee joints, with incidence and space joint narrowing by subsets of compartment and radiographic modalities cumulative to 84-month follow-up
| Clinic site/Radiographic modality and image resolution | Birmingham, AL (UAB) CR low resolution images 894 knees | Iowa City, IA (UIowa) DF high resolution images 1158 knees |
|---|---|---|
| Definition/location | ||
| Incident tibiofemoral OA: K–L grade ≥ 2 N (PA view), N (%) | 195 (21.8) | 303 (26.2) |
| Medial compartment only | 108 (55.4) | 164 (54.1) |
| Lateral compartment only | 45 (23.1) | 61 (20.1) |
| Both compartments | 2 (1.0) | 10 (3.3) |
| Incident without JSN change | 40 (20.5) | 68 (22.4) |
| Medial JSN by ≥0.5 grade (both PA and lateral views), N (%) | 137 (15.3) | 213 (18.4) |
| Medial compartment only | 134 (97.8) | 201 (94.4) |
| Both compartments | 3 (2.2) | 12 (5.6) |
| Lateral JSN by ≥0.5 grade (both PA and lateral views), N (%) | 59 (6.6) | 86 (7.4) |
| Lateral compartment only | 56 (94.9) | 74 (86.0) |
| Both compartments | 3 (5.1) | 12 (14.0) |
JSN outcomes were defined as an increase in JSN score, which is an increase in medial or lateral TF JSN by a half grade or more at follow-up based on both PA and lateral views. Previous studies showed that an increase of JSN by a half-grade or more yields high rates of radiographic progression in knees10.
Region selection for fractal analysis
In each baseline knee X-ray image, trabeculae bone texture regions (12.8 mm × 12.8 mm) were selected on the subchondral bone immediately under the medial and lateral cortical plates of the tibia using an automated method11. The size and placement of bone regions were identical to those that produced the strongest signal related to OA detection12 and used in the prediction of OA6. Details of accuracy of the bone region selection are given in Section 4 of the Appendix.
Fractal texture parameters
All fractal parameters were calculated using a variance orientation transform (VOT) method13 separately for both medial and lateral compartments. The method was applied to each region. For the fractal analysis, all DICOM images were converted to 8-bit uncompressed TIFF format. Details of the method are described in Section 5 of the Appendix.
For the trabecular bone regions of MOST knees analyzed, fractal parameters were calculated over all nine scales and specifically at small (S), medium (M) and large (L) ranges of trabecular image sizes (three scales per range). In CR the size ranges were: S = 1.02–1.36 mm, M = 1.53–1.88 mm, and L = 2.05–2.39 mm. In DF they were: S = 0.60–0.80 mm, M = 0.90–1.10 mm, and L = 1.20–1.40 mm. Past studies showed that changes in TB occur at small, medium and large sizes on the development pathway to knee OA3.
The total number of fractal parameters calculated was seventeen and they are described below:
Four fractal dimensions (FDMEAN, FDV, FDH, FDSta): These FDs are a measure of the overall (FDMEAN), vertical (FDV) and horizontal (FDH) direction roughness of trabecular bone texture, respectively. Minor axis fractal dimension (FDSta) quantifies texture roughness in the direction of the roughest part of trabecular bone. This part contains the shortest bone length components. FDs are defined over all scales and their higher values correspond to rougher texture.
Nine fractal signatures (FSs) along the direction of the texture roughest part (FSSta_S, FSSta_M, FSSta_L), the horizontal (FSH_S, FSH_M, FSH_L) and vertical (FSV_S, FSV_M, FSV_L) directions; each FS is a mean value of FDs calculated at individual sizes that are within the S, M or L range. FSs quantify the mean roughness of bone texture at individual range.
Four aspect ratios (Str, StrSS, StrSM, StrSL); these aspect ratios measure a degree of the bone anisotropy (i.e., the amount by which the roughness of bone texture changes with direction) over all sizes or at individual size range; taking values between 0 and 1. A higher anisotropy corresponds to a lower value of the aspect ratio. If the aspect ratio is 1 then the bone texture is perfectly isotropic (i.e., in all directions the roughness is the same).
Statistical analysis
We assess the association of each individual fractal parameter with each outcome analyzed in a separate model. Associations were explored without a specific hypothesis for the form of relationship. We performed 17 individual tests for each outcome. Multivariable analysis (i.e., including all fractal parameters in the same model) was not conducted.
Subjects were stratified by radiographic modality since CR (computer radiography at UAB) and DF (digitized film at UIowa) had different resolutions. Baseline demographic characteristics of the subjects were tabulated. At the knee-level, KL, JSN and osteophyte grades and knee alignment were detailed. The characteristics of subjects who did, and those that did not, have radiographic OA at follow-up were compared using Student’s t-test, the Mann–Whitney U test, or Chi-square tests as appropriate. The comparisons were also performed using outcomes based on an increase in JSN score.
Baseline knees were categorized into four quartile groups (denoted in the Tables II–IV as Q1, Q2, Q3, Q4) on the basis of quartiles of each fractal parameter, determined separately for men and women. The first quartile group Q1 has the lowest 25% of values of parameter, while the group Q4 has the highest 25% of values. Q2 and Q3 comprise the remaining 50% of values, split at the median. Logistic regression was used to assess the association of each baseline medial and lateral fractal parameter with incident TF OA and with an increase in medial, and separately an increase in lateral, JSN scores. Generalized estimating equation methods were used to account correlations between knees in one subject. Odds ratios were calculated for the three groups with the higher parameters in comparison with the first group (Q1 = reference). Linear and U shaped trends were tested using continuous fractal parameters in logistic regression models. For the linear trend, the fractal parameters were modified to z-scores (mean = 0 and SD = 1) and for the U-shaped trend, to z-scores and the square term of z-scores.
Table II.
Incidence of TF radiographic OA by quartile groups of baseline roughness parameters. Lin denotes the linear trend
| Incident radiographic OA
|
|||||
|---|---|---|---|---|---|
| Birmingham, AL (UAB) computer radiography
|
Iowa City, IA (Iowa) Digitized film
|
||||
| 60 months
|
84 months
|
No significant results were found
|
|||
| No knees (incident %) | Adjusted OR (95% CI) | No of knees (incident %) | Adjusted OR (95% CI) | ||
| Medial bone regions | |||||
| FSV_L: 2.05–2.39 | |||||
| Q1 (low) | 223 (13.5) | 1.0 (ref) | |||
| Q2 | 223 (26.0) | 2.99 (1.83–4.90) | |||
| Q3 | 225 (25.3) | 3.06 (1.84–5.10) | |||
| Q4 (high) | 223 (22.4) | 2.35 (1.37–4.05) | |||
| Trend | P = 0.005 (Lin) | ||||
| FDV: all scales 1.02–2.39 | |||||
| Q1 (low) | 222 (18.5) | 1.0 (ref) | |||
| Q2 | 224 (21.0) | 1.56 (0.95–2.58) | |||
| Q3 | 223 (21.1) | 1.51 (0.88–2.60) | |||
| Q4 (high) | 225 (26.7) | 2.09 (1.23–3.57) | |||
| Trend | P = 0.009 (Lin) | ||||
| FSH_M: M = 1.53–1.88 | |||||
| Q1 (low) | 189 (16.9) | 1.0 (ref) | |||
| Q2 | 190 (14.7) | 0.72 (0.41–1.27) | |||
| Q3 | 190 (21.1) | 1.34 (0.76–2.35) | |||
| Q4 (high) | 190 (29.5) | 1.73 (1.02–2.93) | |||
| Trend | P = 0.007 (Lin) | ||||
| FDH: all scales 1.02–2.39 | |||||
| Q1 (low) | 187 (15.0) | 1.0 (ref) | |||
| Q2 | 192 (17.7) | 1.22 (0.68–2.17) | |||
| Q3 | 192 (20.3) | 1.47 (0.83–2.60) | |||
| Q4 (high) | 188 (29.3) | 2.03 (1.17–3.52) | |||
| Trend | P = 0.008 (Lin) | ||||
| FSSta_L: L = 2.05–2.39 | |||||
| Q1 (low) | 222 (18.0) | 1.0 (ref) | |||
| Q2 | 226 (19.5) | 1.42 (0.84–2.41) | |||
| Q3 | 222 (22.1) | 1.53 (0.91–2.58) | |||
| Q4 (high) | 224 (27.7) | 1.90 (1.14–3.17) | |||
| Trend | P = 0.014 (Lin) | ||||
| FDMEAN: all scales 1.02–2.39 | |||||
| Q1 (low) | 221 (19.5) | 1.0 (ref) | |||
| Q2 | 226 (19.5) | 1.19 (0.69–2.04) | |||
| Q3 | 225 (19.6) | 1.11 (0.65–1.89) | |||
| Q4 (high) | 222 (28.8) | 2.03 (1.21–3.41) | |||
| Trend | P = 0.012 (Lin) | ||||
Statistically significant associations are indicated in bold.
Table IV.
Increase of TF JSN ≥0.5 grade by quartile groups of baseline anisotropy parameter. U denotes the U-shaped trend
| Birmingham, AL (UAB) computer radiography | Iowa City, IA (Iowa) Digitized film
|
||||||
|---|---|---|---|---|---|---|---|
|
|
Medial tibiofemoral JSN increase
|
||||||
| No significant results were found
|
30 months
|
60 months
|
84 months
|
||||
| No knees (increase %) |
Adjusted OR (95% CI) |
No knees (increase %) |
Adjusted OR (95% CI) |
No knees (increase %) |
Adjusted OR (95% CI) |
||
| Medial bone regions | |||||||
| StrSL: L = 1.20–1.40 | |||||||
| Q1 (low) | 258 (12.4) | 1.0 (ref) | |||||
| Q2 | 259 (6.2) | 0.51 (0.28–0.92) | |||||
| Q3 | 260 (8.1) | 0.74 (0.42–1.30) | |||||
| Q4 (high) | 258 (8.9) | 0.72 (0.41–1.27) | |||||
| Trend | P = 0.026 (U) | ||||||
| Lateral bone regions | |||||||
| StrSL: L = 1.20–1.40 | StrSL: L = 1.20–1.40 | ||||||
| Q1 (low) | 251 (21.5) | 1.0 (ref) | 287 (23.0) | 1.0 (ref) | |||
| Q2 | 251 (10.8) | 0.48 (0.30–0.77) | 291 (14.4) | 0.60 (0.36–0.99) | |||
| Q3 | 254 (15.7) | 0.74 (0.46–1.17) | 291 (16.5) | 0.70 (0.44–1.13) | |||
| Q4 (high) | 250 (19.6) | 1.01 (0.64–1.60) | 289 (19.7) | 0.84 (0.52–1.35) | |||
| Trend | P = 0.002 (U) | P = 0.016 (U) | |||||
Statistically significant associations are indicated in bold.
Sex, race, age, BMI, knee alignment and KL grade were identified as potential confounders using a six-step directed acyclic graph14. A distribution of each confounder across the groups of each texture parameter was checked by means of Chi-square or ANOVA tests. No overlapping was found for gender. Because of this and the fact that differences in FDs between genders have been previously reported15, our analyses were performed using gender-specific quartile groups for fractal parameters. Regression models were adjusted for confounders.
Statistical analyses were performed using SAS system for Windows (version 9.2; SAS Institute, Cary, NC). Two-tailed P-values <0.05 were considered statistically significant.
Results
Of 6052 knees from 3026 subjects, 894 (UAB) and 1158 (UIowa) knees from 626 and 807 subjects respectively were included in our study (Fig. 1). No significant differences were found in demographics between those who were included in our study and those who were not (data not shown). Known risk factors for OA showed independent associations with the outcomes of OA incidence and increase in JSN score. Women had higher percentage of outcomes and BMI was higher at baseline (Supplementary Tables I–III). Knee level characteristics such as KL grade 1 vs 0, JSN grade 1 vs 0, presence of osteophytes had associations with outcomes as expected (Supplementary Tables I–III). Malalignment showed strong associations with increase of JSN score in both compartments (Supplementary Tables II and III).
We followed the subjects up to the last visit (the 84 months follow-up) if they did not have OA incidence or increase in JSN score at 30 or 60 months. The median follow-up times were 2.5, 5.7 and 7.7 years, respectively, and they were consistent across outcomes and clinics. Most of the OA incidence and the increases in JSN occurred in medial compartments (Table I).
Statistically significant results obtained for odds ratios and trends of fractal texture parameters have been listed in Table II (for incidence of radiographic OA) and Tables III and IV (for increase in JSN) for each follow-up.
Table III.
Increase of TF JSN ≥0.5 grade by quartile groups of baseline roughness parameters. Lin denotes the linear trend
| Birmingham, AL (UAB) computer radiography
|
Iowa City, IA (Iowa) Digitized film
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medial tibiofemoral JSN increase
|
Lateral tibiofemoral JSN increase
|
Medial tibiofemoral JSN increase
|
||||||||||
| 30 months
|
60 months
|
84 months
|
60 months
|
84 months
|
30 months
|
|||||||
| No of knees (increase %) |
Adjusted No OR (95% CI) |
No of knees (increase %) |
Adjusted No OR (95% CI) |
No of knees (increase %) |
Adjusted No OR (95% CI) |
No of knees (increase %) |
Adjusted No OR (95% CI) |
No of knees (increase %) |
Adjusted No OR (95% CI) |
No of knees (increase %) |
Adjusted No OR (95% CI) |
|
| Medial bone regions | ||||||||||||
| FSV_S: S = 1.02–1.36 | FSV_S: S = 1.02–1.36 | FSV_S: S = 1.02–1.36 | FSV_L: L = 2.05–2.39 | FSV_L: L = 2.05–2.39 | FSV_S: S = 0.60–0.80 | |||||||
| Q1 (low) | 203 (6.9) | 1.0 (ref) | 192 (12.5) | 1.0 (ref) | 223 (12.1) | 1.0 (ref) | 194 (2.6) | 1.0 (ref) | 223 (3.1) | 1.0 (ref) | 258 (5.0) | 1.0 (ref) |
| Q2 | 204 (4.9) | 0.70 (0.31–1.54) | 193 (13.5) | 1.07 (0.58–1.97) | 223 (14.8) | 1.52 (0.82–2.81) | 194 (6.7) | 2.93 (1.03–8.35) | 223 (7.6) | 3.29 (1.26–8.56) | 259 (8.1) | 1.45 (0.69–3.05) |
| Q3 | 204 (6.4) | 0.79 (0.36–1.75) | 194 (13.4) | 0.98 (0.53–1.83) | 224 (14.3) | 1.42 (0.77–2.63) | 195 (7.2) | 3.90 (1.39–10.95) | 225 (6.7) | 3.11 (1.18–8.20) | 259 (9.3) | 1.93 (0.98–3.78) |
| Q4 (high) | 203 (12.3) | 2.09 (1.03–4.22) | 193 (19.7) | 2.02 (1.14–3.58) | 224 (20.1) | 2.00 (1.10–3.63) | 194 (7.7) | 4.37 (1.58–12.10) | 223 (9.0) | 5.16 (1.94–13.75) | 259 (13.1) | 2.34 (1.20–4.57) |
| Trend | P = 0.042 (Lin) | P = 0.026 (Lin) | P = 0.035 (Lin) | P = 0.001 (Lin) | P = 0.001 (Lin) | P = 0.007 (Lin) | ||||||
| FDMEAN: all scales 1.02–2.39 | FSV_M: M = 0.90–1.10 | |||||||||||
| Q1 (low) | 221 (12.2) | 1.0 (ref) | 258 (5.4) | 1.0 (ref) | ||||||||
| Q2 | 226 (12.8) | 1.13 (0.62–2.05) | 259 (8.1) | 1.52 (0.75–3.05) | ||||||||
| Q3 | 225 (14.2) | 1.17 (0.60–2.28) | 259 (10.8) | 1.94 (1.03–3.67) | ||||||||
| Q4 (high) | 222 (22.1) | 1.91 (1.07–3.39) | 259 (11.2) | 2.04 (1.02–4.09) | ||||||||
| Trend | P = 0.025 (Lin) | P = 0.028 (Lin) | ||||||||||
| FSV_L: L = 1.20–1.40 | ||||||||||||
| Q1 (low) | 258 (6.6) | 1.0 (ref) | ||||||||||
| Q2 | 259 (7.7) | 1.10 (0.52–2.34) | ||||||||||
| Q3 | 260 (8.5) | 1.56 (0.79–3.08) | ||||||||||
| Q4 (high) | 258 (12.8) | 2.26 (1.13–4.54) | ||||||||||
| Trend | P = 0.007 (Lin) | |||||||||||
| FDV: all scales 0.60–1.40 | ||||||||||||
| Q1 (low) | 260 (4.6) | 1.0 (ref) | ||||||||||
| Q2 | 257 (9.3) | 1.92 (0.91–4.06) | ||||||||||
| Q3 | 260 (7.7) | 1.60 (0.77–3.30) | ||||||||||
| Q4 (high) | 258 (14.0) | 2.81 (1.41–5.57) | ||||||||||
| Trend | P = 0.007 (Lin) | |||||||||||
| Lateral bone regions | ||||||||||||
| FSV_S: S = 1.02–1.36 | ||||||||||||
| Q1 (low) | 223 (9.0) | 1.0 (ref) | ||||||||||
| Q2 | 224 (9.8) | 1.03 (0.53–1.99) | ||||||||||
| Q3 | 224 (4.5) | 0.45 (0.19–1.03) | ||||||||||
| Q4 (high) | 223 (3.1) | 0.32 (0.12–0.82) | ||||||||||
| Trend | P = 0.003 (Lin) | |||||||||||
| FSV_M: M = 1.53–1.88 | ||||||||||||
| Q1 (low) | 222 (9.5) | 1.0 (ref) | ||||||||||
| Q2 | 224 (7.6) | 0.88 (0.45–1.74) | ||||||||||
| Q3 | 224 (5.8) | 0.56 (0.26–1.24) | ||||||||||
| Q4 (high) | 224 (3.6) | 0.30 (0.11–0.80) | ||||||||||
| Trend | P = 0.006 (Lin) | |||||||||||
| FDV: all scales 1.02–2.39 | ||||||||||||
| Q1 (low) | 226 (10.6) | 1.0 (ref) | ||||||||||
| Q2 | 220 (7.3) | 0.79 (0.40–1.55) | ||||||||||
| Q3 | 224 (6.3) | 0.66 (0.32–1.35) | ||||||||||
| Q4 (high) | 224 (2.2) | 0.27 (0.10–0.73) | ||||||||||
| Trend | P = 0.006 (Lin) | |||||||||||
Statistically significant associations are indicated in bold.
Associations of bone roughness and anisotropy with incident OA (KL grade ≥2N)
Roughness
For CR images, roughness measured from medial compartment bone regions produced significant odds ratios with incident OA at 60 months follow-up, for the horizontal direction: odds ratios were 1.73 and 2.03 for Q4 of FSH_M (P = 0.007) and FSH (P = 0.008) respectively (Table II). For incidence at the 84 months follow-up, the vertical direction FSV_L and FDV had significant odds ratios values of 2.99, 3.06 and 2.35 for Q2, Q3 and Q4 (P = 0.005) and 2.09 for Q4 (P = 0.009) respectively (Table II). The roughest direction FDSta_L and the mean overall roughness FDMEAN had significant odds ratios and they were 1.90 and 2.03 for Q4 (P = 0.0014 and P = 0.012) (Table II).
Results obtained from the medial compartment bone regions of DF images were not statistically significant.
Anisotropy
No statistically significant results were found for associations between anisotropy measured by VOT and the outcome of incident OA.
Associations of bone roughness and anisotropy with increase in medial JSN (JSN grade ≥0.5)
Roughness
On CR images, an increase in medial JSN score occurred in 137 (15.3%) knees in 126 subjects (Table I, Supplementary Table II). The number of knees is cumulative to 84 months (i.e., 62 (45.3%) with JSN increase were first time detected at 30 months, plus 52 (38%) at 60 months and plus 23 (16.8%) at 84 months). For medial compartment bone regions of CR images, statistically significant odds ratios for the outcome of medial JSN increase were 2.09, 2.02 and 2.00 for FSV_S (P = 0.042, 0.0026 and 0.035) at 30, 60 and 84 months respectively, and at 84 months, 1.91 for FDMEAN (P = 0.025), and these significant associations were all for Q4 (Table III).
For DF images, an increase in medial JSN score occurred in 213 (18.4%) knees in 193 subjects, comprising 92 (38.0%), 78 (36.6%) and 43 (20.2%) knees at the 30, 60 and 84 months follow-up respectively (Table I, Supplementary Table II). For medial compartment bone regions of DF images, significant odds ratios for the outcome of medial JSN increase were found at 30 months follow-up; for the vertical direction they were 2.34, 2.04, 2.26 and 2.81 for Q4 of FSV_S, FSV_M, FSV_L and FDV (P = 0.007, 0.028, 0.007 and 0.007) (Table II). Also significant was odds ratio of 1.94 for Q3 of FDV_M (P = 0.028) (Table II).
Anisotropy
For CR images, no associations were found between anisotropy in the medial compartment and an increase in medial compartment JSN score.
For DF images, anisotropy analysis of medial compartment bone regions showed significant odds ratio of 0.51 at 30 months followup for Q2 (P = 0.026), and for anisotropy of lateral compartment bone regions, StrSL had significant odds ratios of 0.48 and 0.60 for Q2 (P = 0.002 and 0.016) at 60 and 84 months follow-ups (Table IV) for associations with an increase in medial compartment JSN. These results indicated that lower anisotropy was associated with increased odds of medial compartment JSN increase.
Associations of roughness and anisotropy with increase in lateral JSN (JSN grade ≥0.5)
Roughness
For CR images, 59 (6.6%) knees in 57 subjects had the increase in lateral JSN score. At each follow-up the increase occurred for 25 (42.4.0%), 22 (37.3%) and 12 (20.3%) knees respectively (Table I, Supplementary Table III). For roughness analysis of medial compartment bone regions of CR images, significant odds ratios for an increase in lateral JSN were 2.93, 3.90, 4.37 and 3.29, 3.11, 5.16 for Q2, Q3 and Q4 of FSV_L (both P = 0.001) at 60 and 84 months followups respectively (Table III). For roughness analysis of lateral compartment bone regions of CR images, odds ratios for an increase in lateral JSN were 0.32, 0.30 and 0.27 for Q4 of FSV_S, FSV_M and FSV (P = 0.003, 0.006 and 0.006) at 84 months follow-up.
For DF images, 86 (7.4%) knees in 80 subjects had the increase in lateral JSN score. At each follow-up the increase occurred for 23 (26.7%), 35 (40.7%) and 28 (32.6%) knees respectively (Table I, Supplementary Table III). No significant associations were found.
Anisotropy
No associations were found between VOT anisotropy and an increase in lateral compartment JSN score.
Linearity of associations of VOT results with radiographic score changes
All associations found for roughness exhibited linear trends (Tables II and III). For anisotropy, the results obtained had significant U-shaped trends (Table IV).
Discussion
This is a large-scale exploratory study of the association between knee trabecular bone structure patterns and both incident radiographic TF knee OA and increased knee JSN score. We found that tibial trabecular bone texture on baseline radiographs was associated with incident OA defined as development of a definite osteophyte (new or enlarging) at follow-up. Also, we found associations between the bone texture and loss of joint space longitudinally (defined by an increase of OARSI JSN score by a half-grade or more). All associations were independent of adjustment for baseline sex, age, race, BMI, knee alignment, and KL grade.
Our findings were reported for individual associations of each bone texture fractal parameter (one exploratory variable) and OA incidence or increasing JSN score (one outcome).
We found differences in results between clinics, likely attributed to the different resolution and acquisition modalities of the radiographs. At the UAB clinic, CR produced images with relatively large (0.17 mm) pixel size, and most of the associations were found at the bone texture large sizes (1.02–2.39 mm) over 60 and 84 months. The UIowa clinic had higher resolution images (pixel size = 0.10 mm) obtained from DF and most of the associations found were significant at the small sizes (0.60–1.40 mm) over 30 months. These findings indicate that the large size characteristics show associations in low-resolution images. In high-resolution images, associations were found for the small size characteristics. Therefore, we discussed our results by referring to CR (low resolution) and DF (high resolution) instead of UAB and UIowa.
OA incidence
For medial regions from CR images, we found that a higher horizontal roughness of trabecular bone texture at baseline (FSH_M, FDH) had an increased odds (1.73, 2.03) for incident OA over 60 months. This is consistent with cross-sectional results from previous studies which showed that subchondral bone regions may have higher horizontal roughness for knees with mild and definite OA15. We also found the increased odds (1.90–3.06) along the vertical (FSV_L, FDV) and roughest (FSSta_L) directions and for the overall roughness (FDMEAN) over 84 months, agreeing with cross-sectional studies in which an increase in medial vertical FSs was detected for knees with OA1,2. Medial vertical bone texture has also previously been shown to be cross-sectionally associated with marginal osteophyte size16. At early stages of OA the thinning, fenestration, or breakage of small rod-shaped trabeculae has been observed17 and such changes could explain the associations found for the higher roughness of trabecular bone (high values of FS parameters) with incident OA.
We found no associations for OA incidence at 30 months followup. Possible reason is that over this relatively short period, the incidence of knee OA was low (8.5%; 76 out of 894 knees, Supplementary Table I, Table I). Our results are in line with Dore et al.1 where no associations were seen over 48 months. Also, for lateral bone regions no associations were found. This could be due to the fact that most of the incident OA cases had JSN in the medial compartment; 110 medial vs 47 lateral (Table I).
Increase in JSN score
For medial bone regions from CR images and the increase of medial JSN score, associations between higher bone roughness and JSN increase were similar to those found for incident OA over 84 months. For CR and DF images, significant associations were found for JSN increase at 60, and especially 30, months follow-up. Also, for DF images, higher bone anisotropy was associated with medial JSN increase (ORs of 0.48–0.60 for StrSL) both medially and laterally. Our findings are consistent with previous studies in which an increase in the vertical FDs measured on medial bone regions was associated with an increase of medial JSN progression at 36 months7. Also, a previous study suggested that the baseline bone trabecular integrity (BTI; fractal measure) terms for vertical trabeculae are inversely proportional to loss of joint space width and area and cartilage volume over 24 months8.
The associations of VOT results with increasing JSN score found in this study and evidence from other studies suggest that the fractal parameters could reflect early stage subchondral bone changes due to increased biomechanical loading, i.e., remodeling of the bone that involves bone matrix formation and degradation by osteoblasts and osteoclasts18.
We found more pronounced associations for the outcome medial JSN score increase as compared to incident OA. This could be attributed to our definition of incident OA, which is based on the KL scale which involves growth of osteophytes and JSN, which are different pathological processes and occur in different tissues19. We had 40 OA incident cases (out of 195) without JSN change (Table I). Also, the amount and kind of OA changes from one KL grade to the next are not necessary the same throughout the scale. KL grades 1–2 track mainly the growth of osteophytes while KL grades 3–4 emphasize differences in JSN20.
Since KL grade 1 is a step on the path between a normal knee (KL = 0) and the one with OA (KL = 2) or one with an increase in JSN score, it could be argued that we should have adjusted for KL grade as an intermediate variable instead of a confounder. Past studies [e.g., 21,22] have suggested the FD differences between knees with KL = 1 and knees with KL = 0. However, there is no evidence supporting a causal pathway between FD and KL grade, i.e., that a particular value of FD leads to higher or lower KL (JSN, osteophyte) grade. Also, when we ran a sensitivity analysis on our data stratified by KL grade (grade 0 or 1), the results obtained (data not shown) did not alter our conclusions.
As the nature of this project is exploratory we decided to use the full range of 17 VOT parameters rather than only a limited number. Reducing the number of parameters to only those found as the most promising in previous studies could have compromised the purpose of our analysis. The results in previous studies were obtained for small sample sizes, one-point in time and/or models only partially controlled for potential confounders.
In this exploratory study, we performed many isolated tests. Our P-values reported were not corrected for multiplicity. We did this intentionally. In the context of an exploratory study of a large number of experimental parameters the adjustment for multiplicity could be counterproductive, resulting in finding no associations where there were associations (type II error)23. To assess the possible impact of collinearity between individual fractal parameters and the covariates in the models we calculated variance inflation factors. Inflation factors greater than 10 were found, suggesting collinearity between age and intercept and between BMI and intercept. Further investigation suggested that the collinearity was due to large differences in scale between BMI and age and the other confounders. Therefore we normalized the age and BMI into variables with standard deviation equals to 1. This normalization did not essentially change associations between fractal parameters and OA incident and JSN worsening.
We checked whether the odds ratios approximated the relative risk in our data24. We found that the relative risks were lower (for ORs > 1) or higher (for ORs < 1) and showed same trends as compared to the odds ratios presented. Statistical significances were found: for medial bone regions, the relative risk of OA incidence was 1.57 for FDV and for lateral regions, the risk of lateral JSN score increase was 0.39 and 0.30 for FSV_S and FDV. Thus, the odds ratios do not approximate the relative risk in our data, except when number of events is below 10% (lateral JSN increase).
There are important limitations to this study. First, FS analysis is a relatively new field and as the nature of our study is exploratory with multiple comparisons made, some significant results could be by chance alone. The high probability of false positives remains a concern. Thus, our findings need to be confirmed using other datasets. Second, the two clinics in MOST use different resolutions and acquisition techniques for their imaging. Despite this our results between clinics were similar at the trabecular image sizes that overlapped (i.e., for CR: S = 1.02–1.36 mm and DF: L = 1.20–1.40 mm). Also, at small trabecular sizes (0.60–1.40 mm) associations were found mainly for 30 months while at large sizes (1.02–2.39 mm) they were obtained for 60 and 84 months. These findings are consistent with the previous studies showing that early OA changes in bone occur in small trabeculae17. Third, the sample sizes available for the increase in lateral JSN were relatively small. This is because lateral compartment OA is rare. In previous studies, the lateral compartment was often not analyzed because of the low power of calculations.
In this study, we found that tibial trabecular bone texture on baseline radiographs was associated with incident OA defined as development of a definite osteophyte as well as loss of joint space longitudinally. All associations were independent of adjustment for sex, age, race, BMI, knee alignment, and KL grade at baseline.
Supplementary Material
Acknowledgments
The authors wish to thank the Curtin University, Department of Mechanical Engineering for their support during preparation of the manuscript. M. Englund was supported by the Swedish Research Council.
We would like to thank the participants and staff of the MOST study at the clinical sites in Birmingham, AL and Iowa City, IA, the staff at the Coordinating Center at University of California San Francisco, San Francisco, CA, and the X-ray Reading Center in Boston University School of Medicine, Boston, MA.
Funding sources
The MOST Study is supported by National Institutes of Health (NIH) grants from the National Institute on Aging to Drs. Lewis (U01-AG-18947), Nevitt (U01-AG-19069), and Felson (U01-AG-18820).
Footnotes
Author contributions
(a) Conception and design: PP, ME, MW, GWS, IT, MN.
(b) Acquisition of data: MN, DF, NS, CL, JAL, PP, MW, GWS.
(c) Analysis and interpretation of data: PP, MW, ME, IT, GWS, MN, JAL.
(d) Drafting the article or revising it critically for important intellectual content: PP, MW, GWS, ME, IT, MN, JAL.
(e) Final approval of the version to be published: All authors.
(f) Literature search: PP, ME, MW, IT, JAL.
(g) Statistical expertise: IT, PP, MW, ME, MN, JAL
(h) Guarantors of the integrity of the study: PP, ME, MN.
Conflict of interest
None declared.
Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.joca.2016.05.003.
References
- 1.Dore D, Lynch JA, Liu F, Li J, McCulloch CE, Jones G, et al. The association between fractal signature analysis of subchondral trabecular bone and incident radiographic knee osteoarthritis –data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2011;19(Suppl 1):S166–7. [Google Scholar]
- 2.Messent EA, Ward RJ, Tonkin CJ, Buckland-Wright C. Differences in trabecular structure between knees with and without osteoarthritis quantified by macro and standard radiography, respectively. Osteoarthritis Cartilage. 2006;14:1302–5. doi: 10.1016/j.joca.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Wolski M, Stachowiak GW, Dempsey AR, Mills PM, Cicuttini FM, Wang Y, et al. Trabecular bone texture detected by plain radiography and variance orientation transform method is different between knees with and without cartilage defects. J Orthop Res. 2011;29:1161–7. doi: 10.1002/jor.21396. [DOI] [PubMed] [Google Scholar]
- 4.Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G. Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults: a prospective study. Arthritis Rheum. 2005;52:2033–9. doi: 10.1002/art.21148. [DOI] [PubMed] [Google Scholar]
- 5.Wluka AE, Ding C, Jones G, Cicuttini FM. The clinical correlates of articular cartilage defects in symptomatic knee osteoarthritis: a prospective study. Rheumatology (Oxford) 2005;44:1311–6. doi: 10.1093/rheumatology/kei018. [DOI] [PubMed] [Google Scholar]
- 6.Woloszynski T, Podsiadlo P, Stachowiak GW, Kurzynski M, Lohmander LS, Englund M. Prediction of progression of radiographic knee osteoarthritis using tibial trabecular bone texture. Arthritis Rheum. 2012;64:688–95. doi: 10.1002/art.33410. [DOI] [PubMed] [Google Scholar]
- 7.Kraus VB, Feng S, Wang S, White S, Ainslie M, Brett A, et al. Trabecular morphometry by fractal signature analysis is a novel marker of osteoarthritis progression. Arthritis Rheum. 2009;60:3711–22. doi: 10.1002/art.25012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraus VB, Feng S, Wang SC, White S, Ainslie M, Hellio Le Graverand MP, et al. Subchondral bone trabecular integrity predicts and changes concurrently with radiographic and magnetic resonance imaging–determined knee osteoarthritis progression. Arthritis Rheum. 2013;65:1812–21. doi: 10.1002/art.37970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LaValley MP, McLaughlin S, Goggins J, Gale D, Nevitt MC, Felson DT. The lateral view radiograph for assessment of the tibiofemoral joint space in knee osteoarthritis: its reliability, sensitivity to change, and longitudinal validity. Arthritis Rheum. 2005;52:3542–7. doi: 10.1002/art.21374. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT, Niu J, Guermazi A, Sack B, Aliabadi P. Defining radiographic incidence and progression of knee osteoarthritis: suggested modifications of the Kellgren and Lawrence scale. Ann Rheum Dis. 2011;70:1884–6. doi: 10.1136/ard.2011.155119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Podsiadlo P, Wolski M, Stachowiak GW. Automated selection of trabecular bone regions in knee radiographs. Med Phys. 2008;35:1870–83. doi: 10.1118/1.2905025. [DOI] [PubMed] [Google Scholar]
- 12.Woloszynski T, Podsiadlo P, Stachowiak GW, Kurzynski M. A signature dissimilarity measure for trabecular bone texture in knee radiographs. Med Phys. 2010;37:2030–42. doi: 10.1118/1.3373522. [DOI] [PubMed] [Google Scholar]
- 13.Wolski M, Podsiadlo P, Stachowiak GW. Directional fractal signature analysis of trabecular bone: evaluation of different methods to detect early osteoarthritis in knee radiographs. Proc Inst Mech Eng H. 2009;223:211–36. doi: 10.1243/09544119JEIM436. [DOI] [PubMed] [Google Scholar]
- 14.Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8:70–84. doi: 10.1186/1471-2288-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Messent EA, Ward RJ, Tonkin CJ, Buckland-Wright C. Cancellous bone differences between knees with early, definite and advanced joint space loss; a comparative quantitative macroradiographic study. Osteoarthritis Cartilage. 2005;13:39–47. doi: 10.1016/j.joca.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Messent EA, Ward RJ, Tonkin CJ, Buckland-Wright C. Osteophytes, juxta-articular radiolucencies and cancellous bone changes in the proximal tibia of patients with knee osteoarthritis. Osteoarthritis Cartilage. 2007;15:179–86. doi: 10.1016/j.joca.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 17.Intema F, Hazewinkel HAW, Gouwens D, Bijlsma JWJ, Weinans H, Lafeber FPJG, et al. In early OA, thinning of the subchondral plate is directly related to cartilage damage: results from a canine ACLT-meniscectomy model. Osteoarthritis Cartilage. 2010;18:691–8. doi: 10.1016/j.joca.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 18.Burr DB, Gallant MA. Bone remodeling in osteoarthritis. Nat Rev Rheumatol. 2012;8:665–73. doi: 10.1038/nrrheum.2012.130. [DOI] [PubMed] [Google Scholar]
- 19.Spector TD, Cooper C. Radiographic assessment of osteoarthritis in population studies: whither Kellgren and Lawrence? Osteoarthritis Cartilage. 1993;1:203–6. doi: 10.1016/s1063-4584(05)80325-5. [DOI] [PubMed] [Google Scholar]
- 20.Emrani PS, Katz JN, Kessler CL, Reichmann WM, Wright EA, McAlindon TE, et al. Joint space narrowing and Kellgrene Lawrence progression in knee osteoarthritis: an analytic literature synthesis. Osteoarthritis Cartilage. 2008;16:873–82. doi: 10.1016/j.joca.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harrar K, Hamami L. The fractal dimension correlated to the bone mineral density. WSEAS Trans Signal Proc. 2008;4:110–26. [Google Scholar]
- 22.Lindsey CT, Narasimhan A, Adolfo JM, Jin H, Steinbach LS, Link T, et al. Magnetic resonance evaluation of the interrelationship between articular cartilage and trabecular bone of the osteoarthritic knee. Osteoarthritis Cartilage. 2004;12:86–96. doi: 10.1016/j.joca.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 23.Bender R, Langeb S. Adjusting for multiple testing–when and how? J Clin Epidemiol. 2001;54:343–9. doi: 10.1016/s0895-4356(00)00314-0. [DOI] [PubMed] [Google Scholar]
- 24.Wilber ST, Fu R. Risk ratios and odds ratios for common events in cross-sectional and cohort studies. Acad Emerg Med. 2010;17:649–51. doi: 10.1111/j.1553-2712.2010.00773.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


