Abstract
Objective:
Identify the environmental factors that influence stroke-survivors’ reengagement in personally valued activities and determine what specific environmental factors are related to specific valued activity types.
Data sources:
PubMed, CINAHL and PsycINFO were searched until June 2016 using multiple search-terms for stroke, activities, disability, and home and community environments.
Review methods:
An integrated mixed-method systematic review of qualitative, quantitative and mixed-design studies was conducted. Two researchers independently identified relevant studies, assessed their methodological quality and extracted relevant findings. To validly compare and combine the various findings, all findings were classified and grouped by environmental category and level of evidence.
Results:
The search yielded 4024 records; 69 studies were included. Most findings came from low-evidence-level studies such as single qualitative studies. All findings were consistent in that the following factors facilitated reengagement post-stroke: personal adapted equipment; accessible environments; transport; services; education and information. Barriers were: others’ negative attitudes and behaviour; long distances and inconvenient environmental conditions (such as bad weather). Each type of valued activity, such as mobility or work, had its own pattern of environmental influences, social support was a facilitator to all types of activities. Although in many qualitative studies others’ attitudes, behaviour and stroke-related knowledge were seen as important for reengagement, these factors were hardly studied quantitatively.
Conclusion:
A diversity of environmental factors was related to stroke-survivors’ reengagement. Most findings came from low-evidence-level studies so that evidence on causal relationships was scarce. In future, more higher-level-evidence studies, for example on the attitudes of significant others, should be conducted.
Keywords: Stroke, systematic review, activities of daily living, social and leisure activities, context
Introduction
After stroke, many stroke-survivors suffer from activity loss,1,2 which is related to a decline in their life satisfaction3,4 and well-being.5 To enable stroke-survivors to restore at least those activities that they most value, rehabilitation trajectories include many efforts to remediate the functions and skills that underlie these valued activities.6 However, as many stroke-survivors are left with persisting disability in spite of these efforts,7,8 it is highly relevant that rehabilitation also focuses on the creation of a supportive ‘post-discharge environment’.9 Reengagement in valued activities may be enhanced by recognising and eliminating barriers and integrating available resources in the stroke-survivor’s environment as part of the rehabilitation programme. So far, however, it remains unclear which environmental features of stroke-survivors’ living environments help or hinder their attempts to resume their valued activities.10,11 This mixed-method systematic review used an integrative design to combine all relevant qualitative and quantitative evidence available on this topic. It aimed to identify the environmental factors that facilitate or hinder stroke-survivors’ reengagement in personally valued activities, and to determine what specific environmental factors are related to specific types of valued activities post-stroke.
In the context of this review, environmental factors included all physical, social and system-related factors that are present in the stroke-survivor’s living environment. These include their housing; city; family and friends as well as the organisational; infrastructural; sociocultural and political features of their community. Valued activities were defined as activities that were voluntary chosen and of specific value to stroke-survivors, for example because these activities were directly related to a stroke-survivor’s valued family role or social position.
Methods
We performed a systematic literature search in Pubmed, Cinahl and Psychinfo from database onset to June 2016 to identify relevant studies. Since there are only a few suitable MeSH headings on environmental factors and relevant keywords vary widely, we needed to use a two-step search strategy. First, we identified all qualitative, quantitative and mixed-design studies on stroke and reengagement in valued activities; then we extracted all the relevant articles on environmental factors. For the full search string (Pubmed), see the appendix (supplementary material).
Two experts in stroke rehabilitation (JZ, SJ) independently identified articles that met the inclusion criteria by title and by abstract. Prior to each inclusion step, a sample of 10 reports was used to verify agreement in applying the inclusion criteria. The inclusion criteria were as follows: non-biomedical, scientific studies of community-dwelling adult stroke-survivors, containing findings on environmental factors that influenced survivors’ reengagement in valued activities, written in English. Because we were specifically interested in environmental factors that influence reengagement in valued activities after stroke and single case studies were expected to also describe environmental factors that are not particularly related to stroke, we excluded single case studies. We also excluded studies about professional health services because the aim was to provide knowledge about environmental factors rather than to present evidence on specific health interventions.
Two researchers (SH, SJ) independently read the full texts and decided whether articles should be included. Disagreement was resolved by discussion. If necessary, they consulted a third subject matter expert (ES), whose decision was final.
The methodological quality of each original study was assessed using the Critical Appraisal Skills Programme (CASP) lists.12 Each original study was assessed by SH and SJ independently using the specific list per design (qualitative, case control, cohort, randomised controlled trial, systematic review). Any disagreement was resolved by discussion. Percentage scores were calculated based on fulfilled items divided by the total number of relevant items. Studies of sufficient methodological quality (i.e. with CASP scores higher than 65%) were included for further analysis.
Data extraction was done by the two researchers (SH, SJ). They independently extracted findings on the influence of environmental factors from all qualitative, quantitative and mixed-design studies. Qualitative data were extracted by identifying all relevant text passages on the facilitating or hindering role of environmental factors on valued activities and by briefly describing their central meaning while staying as close to the original text as possible. In case a direction of influence (facilitator or barrier) was clear in the context of a particular study but was not explicitly described by the author, this was noted. Quantitative findings were extracted by describing relevant results of univariate and bivariate analyses.
An integrated design was used to combine qualitative and quantitative data. In such a design, methodological differences between qualitative and quantitative studies are seen as minimal because both kinds of data are viewed as producing findings that can readily be transformed into each other.13 After such a data transformation, it becomes possible to synthesise all the findings.13 In this particular systematic review, we made quantitative findings comparable to qualitative findings by describing whether the quantitative findings referred to a facilitating or a hindering role with regard to reengagement.
We expected that various environmental factors, described in diverse terms, would be present within all the qualitative, quantitative and mixed-design studies. To be able to validly compare the diverse findings and, if suitable, combine them, we classified all the findings by the type of environmental factor they described, using the International Classification of Functioning, Disability and Health (ICF).14 Categorising findings using an existing classification system can be referred to as directed content analysis and is used when substantial knowledge of existing categories is available.15 For each environmental factor described in a particular finding, we sought the ICF-environmental category or subcategory that best described its content. In some cases, a global ICF-category best fit the description of such a factor; in other cases, a more refined ICF-category was a better fit. When a suitable ICF-category was not available, the factor was classified as ‘n.c.’ (not covered by the ICF), in accordance with the ICF linking rules.16
Furthermore, to understand the value of a specific finding as compared to others, we used the Melnyk hierarchy of levels of evidence17 to arrange our findings. Although there are many hierarchies of evidence available in the literature,18 this particular hierarchy of evidence encompasses a broad range of evidence, including quantitative and qualitative evidence.17 See Figure 1 (supplementary material) for this hierarchy (levels ranging from low to high evidence: VII to I). Because we only included literature from scientific, peer-reviewed studies, level VII (evidence from expert opinions) and narrative reviews did not apply to this review study.
After transforming the data and arranging findings by type of environmental category and level of evidence, an overall comparison between all findings arranged under the same, and subsequently under different ICF environmental categories was made. This was done by one researcher (SJ) using thematic analysis19 while continually checking the study characteristics (see supplementary Tables I-a, II-a and III-a) to confirm it was valid to compare or combine findings. Similarities and inconsistencies between findings (e.g. with regard to the content or the directionality of the environmental influence) as well as the related levels of evidence were noted. In accordance with the lines-of-argument synthesis,20 the researcher subsequently tried to explain as a whole the findings arranged under the same and under different ICF environmental categories. This resulted in a conclusion about what environmental factors generally facilitate or hinder reengagement in valued activities post-stroke, as well as about the related levels of evidence.
Finally, to be able to draw a more precise conclusion about what specific environmental factors facilitate or hinder the specific types of valued activities that stroke survivors try to resume, the researcher used thematic analysis to subdivide in categories the various activities described in the studies. This resulted in a description of several main types of activities valued by stroke survivors. All the findings from the qualitative, quantitative and mixed-design studies subsequently were arranged by these main types of valued activities. The researcher then described those environmental factors that, according to at least two qualitative/descriptive studies (i.e. two studies with evidence level VI) or according to one or more studies with a higher level of evidence (level V to I), facilitated or hindered a particular main type of activity. When, for a specific main type of valued activity, findings with regard to the influence of a particular environmental factor were contradictory, the factor was not taken into account. All conclusions drawn about the influence of environmental factors in general and about the specific main types of valued activities finally were checked by the other researchers involved in this review study (SH, ES, RS, RN). Disagreement was resolved by discussion.
Results
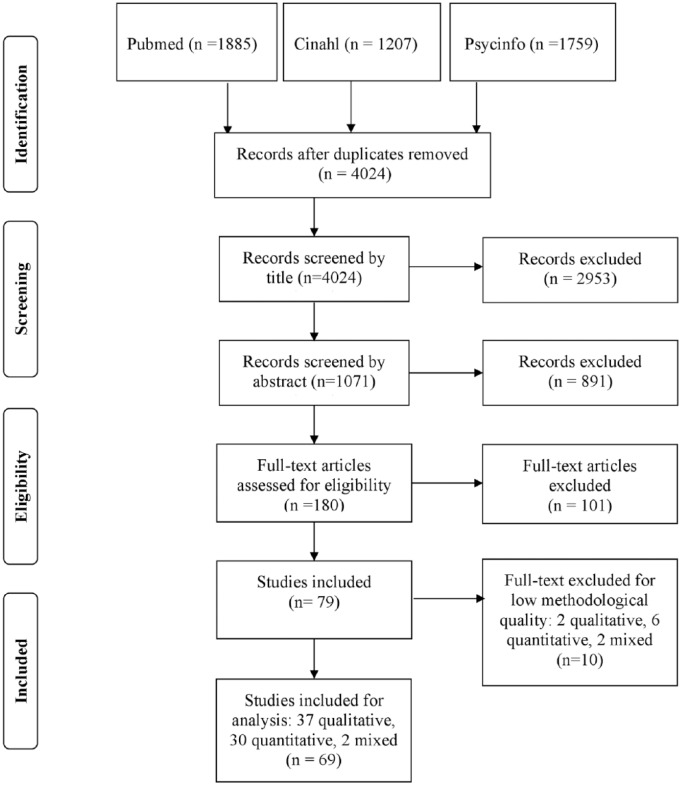
As shown in Figure 1, we identified 4024 studies, of which 69 fulfilled the inclusion criteria and had CASP scores higher than 65%. Of these, 37 reported qualitative data, 30 reported quantitative data and two had a mixed design. Supplementary Tables I-a, II-a and III-a list all the studies that fulfilled the inclusion criteria, including their methodological quality; characteristics; measures; levels of evidence and extracted study findings (studies with low methodological quality are listed in Tables I-b, II-b and III-b).
Figure 1.
Inclusion of studies.
Of the 37 included high-quality qualitative studies, seven described specific environmental factors and their influence on reengagement21–26 (e.g. the influence of wheelchair use on community reengagement).21 The other studies focused on stroke-survivors’ reengagement experiences in general. One study27 was a systematic meta-synthesis (Melnyk evidence level V), one study28 thematically analysed blogs written by stroke-survivors (level VI). Thirty five studies (level VI) used semi-structured individual or focus group interviews. Additionally, three of these interview studies also used other methods of data collection including diaries, photographs or observations. All qualitative studies reported experiences of stroke-survivors resuming activities according to standards they personally found satisfactory. The participant characteristics of the qualitative studies were variable: some studies researched a specific group such as aphasic or cognitively impaired stroke-survivors, while others studied stroke-survivors ‘in general’. Nine studies included significant others, such as informal caregivers, in addition to stroke-survivors. Reported ages ranged from 18 to 94 years; measurement time-points ranged from a number of weeks to 32 years post-stroke.
Of the 30 included high-quality quantitative studies (13 cross-sectional, 12 cohort, two case control and three randomised controlled trials) three29–31 descriptively reported facilitators and barriers experienced by stroke-survivors. The other studies examined a statistical relationship between environmental factors and valued activities. Reengagement was not quantified uniformly within the studies: it was measured by counting the number of daily activities performed32–35 or the number that could be performed without help;32,34–37 the amount of help needed;32,38–40 the relative difficulty experienced;33,38,40–45 the satisfaction felt with performance;33,46 or by exploring the subjective experience of feeling integrated within one’s living environment.47,48 Melnyk evidence levels varied between the studies: 13 studies had level VI, 14 level IV and three level II. Some studies included a specific group (e.g. wheelchair users), while others included stroke-survivors ‘in general’. Reported ages ranged from 27 to 97 years; measurement time-points ranged from four weeks to 27 years post-stroke.
The two included high-quality mixed-design studies were both cross-sectional (level VI). They combined reengagement measures with open-ended questions. One study examined stroke-survivors with aphasia, while the other examined stroke-survivors ‘in general’. Reported ages ranged from 47 to 81 years; measurement time-points ranged from nine months to one year post-stroke.
For a more detailed description of all the high-quality studies and their findings, see supplementary Tables I-a, II-a and III-a.
Environmental facilitators and barriers to reengagement post-stroke
A variety of facilitators and barriers were described in the included qualitative, quantitative and mixed-design studies. Most findings were related to the social and system-related aspects of stroke-survivors’ living environments (ICF-categories e3-5). They mainly came from low-evidence-level, single qualitative studies (level VI). Findings from controlled trials (level III) or from systematic reviews of randomised controlled trials (level I) were not identified. Supplementary Table IV displays all the environmental factors found in the 69 included studies, as well as the direction of their influence and their level of evidence.
As shown in the first column of Supplementary Table IV, most environmental factors found could be allocated to existing ICF-environmental categories. We added some extra categories (e.g. ‘skills/features of network members’) and refined some existing ICF-categories (e.g. the attitudes category). Within all the original ICF- and new categories, the directions of the environmental influences found (facilitator or barrier) were largely in accordance with each other. For example, regardless of each study’s participants or design, all the findings suggested that personal adapted equipment (e.g. assistive devices or communication aids); accessible environments (e.g. a well-adapted public space, accessible buildings and even terrain); high-quality transport; services, educational opportunities and, in most cases, money and social support were all facilitators to reengagement in valued activities post-stroke. Other people’s negative perceptions, attitudes and behaviours as well as long distances were all barriers to reengagement. A comparison of the findings from different ICF-environmental categories found that reengagement in valued activities is facilitated by access to information (e.g. about alternative transport). Inconvenient, complex and unstable conditions (e.g. bad weather or darkness, crowds, unstable prerequisites at work) generally hinder stroke-survivors’ ability to resume their valued activities.
However, we also found some inconsistencies with regard to directionally or content of the findings. First, although most findings suggested that wheelchairs were related to better reengagement, in work situations they were mainly seen as a barrier that made it difficult to socialise with colleagues or do heavy work.49 Second, some qualitative studies found living in a rural area (instead of an urban area) to be a facilitator to reengagement.50,51 This was in line with the finding that crowds52 and fast-moving traffic53,54 were seen as barriers to reengagement. However, it was not consistent with the finding that uneven terrain,55 soil,51 farm animals,51 long distances54–58 or poor geographic coverage of public transport57,59 were also seen as barriers. In addition, quantitative studies found no significant relationship between type of living area and reengagement post-stroke.34,39 As a whole, these findings may suggest that the disadvantages of living in a rural area largely outweighs the advantages.
In several cases inconsistency between findings from qualitative and quantitative studies was present. For example, according to many qualitative studies,25,26,50,52,53,58,60–63 the availability of spouses, family and friends was related to better stroke-survivors’ reengagement. However, most cross-sectional or cohort studies did not confirm a relationship between the presence of spouses, family or friends and reengagement in valued activities.33,34,38,39,45,46,64–66 Sometimes, their presence was even found to worsen reengagement.67 For a detailed description of the similarities and inconsistencies between findings and related levels of evidence, see Supplementary Table IV, last column; ‘synthesis’.
Environmental influences per specific type of valued activity
Thematic analysis revealed that valued activities could be divided into the following categories: reengagement in valued activities in general (studies about outdoor and indoor activities); 22,25,26,32,33,35–46,48,60–64,67–72 social and community reengagement (studies about social activities outside the home and in the community);21,23,27, 28,34,47,50,52,55,58,73,74 mobility (studies about moving around as a meaningful activity)29,51,53,54,56,57,59 and work.24,49,65,66,75–86 Some single remaining studies on activities such as eating, exercise or leisure30,31,87–90 did not fit this format. In all the types of valued activities social support was identified as a facilitator to reengagement. In most cases, adequate transport was recognised as being facilitating while others’ unsupportive attitudes and behaviours were seen as hindering to most types of valued activities.
Each type of valued activity also had its own pattern of influencing environmental factors. Studies on reengagement in valued activities in general, exclusively found the following facilitators: powered wheelchairs, home adaptations and adequate services, while studies on social and community reengagement exclusively found adaptation for communication and information access to be important. Studies on mobility specifically mentioned different aspects of traffic, public transport, the behaviour of bus drivers, distances and costs, while studies on work exclusively found features of the job itself to be relevant. In relatively many studies on social and community reengagement and on work, others’ attitudes, behaviours and stroke-related knowledge were seen as important for reengagement.
Supplementary Table V displays all the environmental factors that influence a particular type of valued activity (according to non-contradictory findings of at least two studies at level VI, or according to at least one study with a higher level of evidence). The table also shows all the related levels of evidence.
Discussion
This review identified an extensive list of environmental factors that may influence a stroke-survivor’s reengagement in valued activities. The majority of the findings were related to the social and system-related aspects of stroke-survivors’ living environments, such as the availability of family and friends and the quality of organisations and community services. Although different types of valued activities each had their own patterns of environmental influences, social support was identified as important to all types of activities. In relatively many studies on social and community reengagement and on work, the attitudes, behaviours and stroke-related knowledge of familiar other people were seen as important for reengagement in stroke-survivors’ valued activities. When in complex social environments such as the community or the workplace, others’ willingness to adapt to the stroke-survivor, their encouragement and their knowledge about stroke are probably crucial to enable stroke-survivors to resume their activities. However, quantitative higher-level studies rarely studied the impact of these factors on reengagement. Since a range of negative individual and societal attitudes and behaviours seems to hinder reengagement in disabilities,91 it is of the utmost importance to better examine and understand the influence of these attitudes and behaviours and the convictions and gaps in knowledge that underlie them.
This study used the ICF-environmental categories and the Melnyk levels of evidence to classify and compare findings. Most findings fit the ICF. However, the ICF was not refined enough to allocate specific features, skills or attitudes and behaviours of others (e.g. others’ fatigue, problem-solving skills or willingness). Some other factors, such as ‘time’, could not be linked to any existing ICF-chapter at all. In future, the ICF could be improved by further mapping such factors, so that a comprehensive and consistent set of relevant environmental factors will become available to clinicians and researchers. Other authors91,92 have confirmed the necessity to add additional factors, such as time.
The levels of evidence found in this review were generally low: most findings on environmental factors and stroke-survivors’ valued activities came from single qualitative and cross-sectional studies (level VI). We found no studies with an evidence level of III or I. As a result, although we gained some insight into the environmental factors related to stroke-survivors’ reengagement in valued activities, there is a lack of knowledge about causal relationships between environmental factors and reengagement. Further research should address this knowledge gap, for example by developing an educational programme for family members, friends and colleagues on how best to support stroke-survivors’ reengagement and evaluating this programme in a controlled trial.
There is also a scarcity of high-level evidence on the influence of environmental factors on conditions other than stroke. In one of the few review studies done on environmental factors, Heinemann et al.93 found a set of environmental factors that were relevant to stroke, traumatic brain injury and spinal cord injury. That review found that the following factors influence reengagement: assistive technology; the built and natural environments; the social environment; services, systems and policies; access to information and technology, and economic quality of life. These categories largely match the findings in our study, although we found some inconsistencies between qualitative and quantitative evidence (e.g. about the availability of spouses, family or friends).
With regard to such inconsistencies, a recent narrative review of the influence of the environment on reengagement94 found that, although disabled people had identified several environmental facilitators and barriers to their reengagement, a corresponding facilitating or hindering environment generally did not lead to greater or lower reengagement outcomes. It could be that these facilitators and barriers were not strong enough to actually make a difference94 or that the measures used to capture the difference were not sensitive enough to register it. However, it could also be due to a difference in underlying ideas about what is ‘optimal’ in respect to reengagement. As was shown in our review study, quantitative studies often see independence or easy performance as ideal, whereas for stroke-survivors themselves, reengagement is primarily about feeling respected and being a valued member of society.95 Perhaps the availability of significant others (e.g. spouses or colleagues) does not always add to stroke-survivors’ objective levels of independence or easy performance, but it nevertheless seems vital for stroke-survivors to feel included within family, work or society.
Future research should clarify the inconsistency between outcomes from qualitative and quantitative research. Developing quantitative measures that reflect the meaning of optimal reengagement as it is understood by stroke-survivors could help make qualitative and quantitative findings more comparable.
Clinicians can use the findings from this review to verify barriers and resources present in the living environments of stroke-survivors. Because these findings came from studies with various objectives, inclusion criteria and designs, not all of them apply to all stroke-survivors in all circumstances. It is nevertheless worthwhile for clinicians to keep the findings of this review in mind, as it can draw their attention to those environmental factors that are often experienced as facilitators or barriers in reengagement in general, as well as in more specific types of valued activities. Apart from this, clinicians should be aware that what stroke-survivors perceive as optimal with regard to reengagement does not always mirror existing clinical measures. Depending on the aim of treatment, clinicians should consider using both objective and subjective measures to examine stroke-survivors’ ability to reengage in their valued activities.
Strengths and limitations
To our knowledge, this is the first mixed-method systematic review of environmental determinants of valued activities post-stroke. The strength of this study was the broad search; by using a comprehensive combination of keywords related to common activities and contexts, we were able to collect a relevant data set that can inform clinical practice and research. Since we chose not to include studies about professional services, the data about services, systems and policies are incomplete.
Another strength was the integrative approach we used to combine qualitative and quantitative findings, which resulted in a detailed picture of knowledge available on environmental factors and reengagement post-stroke. However, the original studies used different terminology, measurements and methods of analysis. The quantitative studies analysed a set of pre-set environmental factors, while most of the qualitative studies let the environmental factors emerge from the data. The methods used in the qualitative studies furthermore varied in the extent to which they interpreted or just described the data. We therefore had to be cautious about which findings could be compared or combined, and what final conclusions could be drawn.
Because of the diversity of the included studies and the low levels of evidence found, the conclusions of this review may be considered global or preliminary by nature. Nevertheless, in the absence of more precise research findings, our results provide a good first indication of environmental factors that play a role in stroke-survivors’ valued activities.
Clinical messages.
There is inconsistency between what stroke-survivors see as ‘optimal’ with regard to their reengagement in valued activities and what is measured by commonly used participation measures.
Others’ positive attitudes and behaviours seem to be especially crucial for stroke-survivors to enable them to become reengaged in social, community and work-related activities.
Supplementary Material
Acknowledgments
We thank Dr Yvonne Heerkens for her advice on the application of the ICF.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by a HAN University of Applied Sciences PhD scholarship.
References
- 1. Singam A, Ytterberg C, Tham K, von Koch L. Participation in complex and social everyday activities six years after stroke: Predictors for return to pre-stroke level. PLoS ONE 2015; 10: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Salter K, Hellings C, Foley N, Teasell R. The experience of living with stroke: a qualitative meta-synthesis. Journal of rehabilitation medicine 2008; 40: 595–602. [DOI] [PubMed] [Google Scholar]
- 3. Boosman H, Schepers VP, Post MW, Visser-Meily JM. Social activity contributes independently to life satisfaction three years post stroke. Clinical rehabilitation 2011; 25: 460–467. [DOI] [PubMed] [Google Scholar]
- 4. Bergstrom AL, von Koch L, Andersson M, Tham K, Eriksson G. Participation in everyday life and life satisfaction in persons with stroke and their caregivers 3-6 months after onset. Journal of rehabilitation medicine 2015; 47: 508–515. [DOI] [PubMed] [Google Scholar]
- 5. Egan M, Davis CG, Dubouloz CJ, Kessler D, Kubina LA. Participation and well-being poststroke: evidence of reciprocal effects. Archives of physical medicine and rehabilitation 2014; 95: 262–268. [DOI] [PubMed] [Google Scholar]
- 6. Cott CA, Wiles R, Devitt R. Continuity, transition and participation: preparing clients for life in the community post-stroke. Disability and rehabilitation 2007; 29: 1566–1574. [DOI] [PubMed] [Google Scholar]
- 7. de Weerd L, Rutgers WA, Groenier KH, van der Meer K. Perceived wellbeing of patients one year post stroke in general practice–recommendations for quality aftercare. BMC Neurology 2011; 11: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Desrosiers J, Rochette A, Noreau L. Long-term changes in participation after stroke. Topics in stroke rehabilitation 2006; 13: 86–96. [DOI] [PubMed] [Google Scholar]
- 9. Vik K, Lilja M, Nygard L. The influence of the environment on participation subsequent to rehabilitation as experienced by elderly people in Norway. Scandinavian journal of occupational therapy 2007; 14: 86–95. [DOI] [PubMed] [Google Scholar]
- 10. Whiteneck G, Dijkers MP. Difficult to measure constructs: conceptual and methodological issues concerning participation and environmental factors. Archives of physical medicine and rehabilitation 2009; 90: S22–S35. [DOI] [PubMed] [Google Scholar]
- 11. Hoyle M, Gustafsson L, Meredith P, Ownsworth T. Participation after stroke: Do we understand all the components and relationships as categorised in the ICF? Brain impairment 2012; 13: 4–15. [Google Scholar]
- 12. CASP checklists. Critical Appraisal Skills Programme (CASP) Oxford. Available at: http://www.casp-uk.net. 2013. (accessed 20 January 2014).
- 13. Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Research in the schools 2006; 13: 29. [PMC free article] [PubMed] [Google Scholar]
- 14. International Classification of Functioning, Disability and Health: ICF. World Health Organization Geneva, 2001. [Google Scholar]
- 15. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–1288. [DOI] [PubMed] [Google Scholar]
- 16. Cieza A, Geyh S, Chatterji S, Kostanjsek N, Ustun B, Stucki G. ICF linking rules: an update based on lessons learned. Journal of rehabilitation medicine 2005; 37: 212–218. [DOI] [PubMed] [Google Scholar]
- 17. Melnyk M, Fineout-Overholt E. Evidence-based practice in nursing and healthcare. A guide to best practice. Philadelphia: Lippincott, Williams & Wilkins, 2011. [Google Scholar]
- 18. Burns PB, Rohrich RJ, Chung KC. The levels of evidence and their role in evidence-based medicine. Plastic and reconstructive surgery 2011; 128: 305–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guest G, MacQueen KM, Namey EE. Applied thematic analysis. Thousand Oaks, California: SAGE Publications, 2012. [Google Scholar]
- 20. Noblit GW, Hare RD. Meta-ethnography: synthesizing qualitative studies. London: Sage Publications, 1988. [Google Scholar]
- 21. Barker DJ, Reid D, Cott C. The experience of senior stroke survivors: Factors in community participation among wheelchair users. Canadian Journal of Occupational Therapy / Revue Canadienne D’Ergotherapie 2006; 73: 18–25. [DOI] [PubMed] [Google Scholar]
- 22. Lindqvist E, Borell L. Computer-based assistive technology and changes in daily living after stroke. Disability and Rehabilitation: Assistive Technology 2012; 7: 364–371. [DOI] [PubMed] [Google Scholar]
- 23. Egbert N, Koch L, Coeling H, Ayers D. The role of social support in the family and community integration of right-hemisphere stroke survivors. Health communication 2006; 20: 45–55. [DOI] [PubMed] [Google Scholar]
- 24. Corr S, Wilmer S. Returning to work after a stroke: an important but neglected area. British journal of occupational therapy 2003; 66: 186–192. [Google Scholar]
- 25. Reid D. Impact of the environment on role performance in older stroke survivors living at home. International journal of therapy and rehabilitation 2004; 11: 567–573. [Google Scholar]
- 26. Anderson S, Whitfield K. Social identity and stroke: ’they don’t make me feel like, there’s something wrong with me’. Scandinavian journal of caring sciences 2013; 27: 820–830. [DOI] [PubMed] [Google Scholar]
- 27. Walsh ME, Galvin R, Loughnane C, Macey C, Horgan NF. Factors associated with community reintegration in the first year after stroke: a qualitative meta-synthesis. Disability and rehabilitation 2015; 37: 1599–1608. [DOI] [PubMed] [Google Scholar]
- 28. Fotiadou D, Northcott S, Chatzidaki A, Hilari K. Aphasia blog talk: How does stroke and aphasia affect a person’s social relationships? Aphasiology 2014; 28: 1281–1300. [Google Scholar]
- 29. Tan KM, O’Driscoll A, O’Neill D. Factors affecting return to driving post-stroke. Irish journal of medical science 2011; 180: 41–45. [DOI] [PubMed] [Google Scholar]
- 30. Rimmer JH, Wang E, Smith D. Barriers associated with exercise and community access for individuals with stroke. Journal of rehabilitation research & development 2008; 45: 315–322. [DOI] [PubMed] [Google Scholar]
- 31. Giaquinto S, Buzzelli S, Di Francesco L, Nolfe G. Evaluation of sexual changes after stroke. Journal of Clinical Psychiatry 2003; 64: 302–307. [DOI] [PubMed] [Google Scholar]
- 32. Kalra L, Evans A, Perez I. Training carers of stroke patients: Randomised controlled trial. BMJ: British Medical Journal 2004; 328: 1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Carlijn H Z A, Lindeman E, Kappelle LJ. Participation in the chronic phase of stroke. Topics in stroke rehabilitation 2013; 20: 52–61. [DOI] [PubMed] [Google Scholar]
- 34. Dalemans RJ, De Witte LP, Beurskens AJ, Van Den Heuvel WJ, Wade DT. An investigation into the social participation of stroke survivors with aphasia. Disability and dehabilitation 2010; 32: 1678–1685. [DOI] [PubMed] [Google Scholar]
- 35. Forster A, Dickerson J, Young J. A structured training programme for caregivers of inpatients after stroke (TRACS): A cluster randomised controlled trial and cost-effectiveness analysis. The Lancet 2013; 382: 2069–2076. [DOI] [PubMed] [Google Scholar]
- 36. Mudzi W, Stewart A, Musenge E. Effect of carer education on functional abilities of patients with stroke. International journal of therapy & rehabilitation 2012; 19: 380–385. [Google Scholar]
- 37. Bui Q, Markides K, Ottenbacher K, Ostir GV. Predictors of disability post stroke: Findings from the H-EPESE. Journal of mental health and aging 2004; 10: 221–230. [Google Scholar]
- 38. Gottlieb A, Golander H, Bar-Tal Y, Gottlieb D. The influence of social support and perceived control on handicap and quality of life after stroke. Aging 2001; 13: 11–15. [DOI] [PubMed] [Google Scholar]
- 39. Lin JH, Hsiao SF, Chang CM, Huang MH, Liu CK, Lin YT. Factors influencing functional independence outcome in stroke patients after rehabilitation. The Kaohsiung journal of medical sciences 2000; 16: 351–359. [PubMed] [Google Scholar]
- 40. Rochette A, Desrosiers J, Noreau L. Association between personal and environmental factors and the occurrence of handicap situations following a stroke. Disability and Rehabilitation 2001; 23: 559–569. [DOI] [PubMed] [Google Scholar]
- 41. Pettersson I, Tornquist K, Ahlstrom G. The effect of an outdoor powered wheelchair on activity and participation in users with stroke. Disability and Rehabilitation: Assistive Technology 2006; 1: 235–243. [DOI] [PubMed] [Google Scholar]
- 42. Perrin PB, Heesacker M, Stidham BS, Rittman MR, Gonzalez-Rothi LJ. Structural equation modeling of the relationship between caregiver psychosocial variables and functioning of individuals with stroke. Rehabilitation psychology 2008; 53: 54–62. [Google Scholar]
- 43. Klinedinst NJ, Gebhardt MC, Aycock DM. Caregiver characteristics predict stroke survivor quality of life at 4 months and 1 year. Research in nursing & health 2009; 32: 592–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chang K-H, Lin Y-N, Liao H-F. Environmental effects on WHODAS 2.0 among patients with stroke with a focus on ICF category e120. Quality of life Research 2014; 23: 1823–1831. [DOI] [PubMed] [Google Scholar]
- 45. Zhang L, Yan T, You L, Li K. Barriers to activity and participation for stroke survivors in rural China. Archives of physical medicine & rehabilitation 2015; 96: 1222–1228. [DOI] [PubMed] [Google Scholar]
- 46. Fallahpour M, Tham K, Joghataei MT, Jonsson H. Perceived participation and autonomy: aspects of functioning and contextual factors predicting participation after stroke. Journal of rehabilitation medicine 2011; 43: 388–397. [DOI] [PubMed] [Google Scholar]
- 47. Griffen JA, Rapport LJ, Bryer RC, Scott CA. Driving status and community integration after stroke. Topics in stroke rehabilitation 2009; 16: 212–221. [DOI] [PubMed] [Google Scholar]
- 48. Beckley MN. Community participation following cerebrovascular accident: Impact of the buffering model of social support. American journal of occupational therapy 2006; 60: 129–135. [DOI] [PubMed] [Google Scholar]
- 49. Vestling M, Ramel E, Iwarsson S. Thoughts and experiences from returning to work after stroke. Work 2013; 45: 201–211. [DOI] [PubMed] [Google Scholar]
- 50. Dalemans RJ, de Witte L, Wade D, van den Heuvel W. Social participation through the eyes of people with aphasia. International journal of language & communication disorders / Royal College of Speech & Language Therapists 2010; 45: 537–550. [DOI] [PubMed] [Google Scholar]
- 51. Corrigan R, McBurney H. Community ambulation: perceptions of rehabilitation physiotherapists in rural and regional communities. Physiotherapy theory and practice 2012; 28: 10–17. [DOI] [PubMed] [Google Scholar]
- 52. Northcott S, Hilari K. Why do people lose their friends after a stroke? International journal of language & communication disorders / Royal College of Speech & Language Therapists 2011; 46: 524–534. [DOI] [PubMed] [Google Scholar]
- 53. Barnsley L, McCluskey A, Middleton S. What people say about travelling outdoors after their stroke: a qualitative study. Australian occupational therapy journal 2012; 59: 71–78. [DOI] [PubMed] [Google Scholar]
- 54. Risser R, Iwarsson S, Stahl A. How do people with cognitive functional limitations post-stroke manage the use of buses in local public transport? Transportation research part F: Traffic psychology and behaviour 2012; 15: 111–118. [Google Scholar]
- 55. Chimatiro G, Rhoda A. Environmental barriers to reintegration experienced by stroke clients post discharge from a rehabilitation centre in Malawi. The South African journal of physiotherapy 2014; 70: 18–23. [Google Scholar]
- 56. White JH, Miller B, Magin P, Attia J, Sturm J, Pollack M. Access and participation in the community: a prospective qualitative study of driving post-stroke. Disability and Rehabilitation 2012; 34: 831–838. [DOI] [PubMed] [Google Scholar]
- 57. Logan PA, Dyas J, Gladman JRF. Using an interview study of transport use by people who have had a stroke to inform rehabilitation. Clinical rehabilitation 2004; 18: 703–708. [DOI] [PubMed] [Google Scholar]
- 58. Walsh ME, Galvin R, Loughnane C, Macey C, Horgan NF. Factors associated with community reintegration in the first year after stroke: a qualitative meta-synthesis. Disability and rehabilitation 2015; 37: 1599–1608. [DOI] [PubMed] [Google Scholar]
- 59. Liddle J, Turpin M, McKenna K, Kubus T, Lambley S, McCaffrey K. The experiences and needs of people who cease driving after stroke. Brain impairment 2009; 10: 271–281. [Google Scholar]
- 60. Vincent C, Deaudelin I, Robichaud L. Rehabilitation needs for older adults with stroke living at home: perceptions of four populations. BMC geriatrics 2007; 7: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Le Dorze G, Salois-Bellerose E, Alepins M, Croteau C, Halle M-C. A description of the personal and environmental determinants of participation several years post-stroke according to the views of people who have aphasia. Aphasiology 2014; 28: 421–439. [Google Scholar]
- 62. Casey D, Murphy K, Cooney A, O’Shea E. Patient perceptions having suffered a stroke in Galway. British journal of community nursing 2008; 13: 384–390. [DOI] [PubMed] [Google Scholar]
- 63. McKevitt C, Luse A, Wolfe C. The unfortunate generation: stroke survivors in Riga, Latvia. Social science & medicine (1982) 2003; 56: 2097–3108. [DOI] [PubMed] [Google Scholar]
- 64. Wallace GL. Profile of life participation after stroke and aphasia. Topics in stroke rehabilitation 2010; 17: 432–450. [DOI] [PubMed] [Google Scholar]
- 65. Saeki S, Toyonaga T. Determinants of early return to work after first stroke in Japan. Journal of rehabilitation medicine 2010; 42: 254–258. [DOI] [PubMed] [Google Scholar]
- 66. Won Hyuk C, Min Kyun S, Jongmin L. Return to work after stroke: the KOSCO study. Journal of rehabilitation medicine 2016; 48: 273–279. [DOI] [PubMed] [Google Scholar]
- 67. Schepers VP, Visser-Meily AM, Ketelaar M, Lindeman E. Prediction of social activity 1 year poststroke. Archives of physical medicine & rehabilitation 2005; 86: 1472. [DOI] [PubMed] [Google Scholar]
- 68. Robison J, Wiles R, Ellis-Hill C, McPherson K, Hyndman D, Ashburn A. Resuming previously valued activities post-stroke: who or what helps? Disability and rehabilitation 2009; 31: 1555–1566. [DOI] [PubMed] [Google Scholar]
- 69. Atler KE, Gliner JA. Post stroke activity and psychosocial factors. Physical & occupational therapy in geriatrics 1989; 7: 13–27. [Google Scholar]
- 70. Kubina L-A, Dubouloz C-J, Davis CG, Kessler D, Egan MY. The process of re-engagement in personally valued activities during the two years following stroke. Disability and rehabilitation 2013; 35: 236–243. [DOI] [PubMed] [Google Scholar]
- 71. Anderson S, Whitfield K. An ecological approach to activity after stroke: It takes a community. Topics in stroke rehabilitation 2011; 18: 509–524. [DOI] [PubMed] [Google Scholar]
- 72. Jongbloed L, Stanton S, Fousek B. Family adaptation to altered roles following a stroke. Canadian journal of occupational therapy 1993; 60: 70–77. [Google Scholar]
- 73. Hammel J, Jones R, Gossett A, Morgan E. Examining barriers and supports to community living and participation after a stroke from a participatory action research approach. Topics in stroke rehabilitation 2006; 13: 43–58. [DOI] [PubMed] [Google Scholar]
- 74. Lund A, Mangset M, Wyller TB, Sveen U. Occupational transaction after stroke constructed as threat and balance. Journal of occupational science 2015; 22: 146–159. [Google Scholar]
- 75. Tanaka H, Toyonaga T, Hashimoto H. Functional and occupational characteristics associated with very early return to work after stroke in Japan. Archives of physical medicine & rehabilitation 2011; 92: 743–748. [DOI] [PubMed] [Google Scholar]
- 76. Tanaka H, Toyonaga T, Hashimoto H. Functional and occupational characteristics predictive of a return to work within 18 months after stroke in Japan: implications for rehabilitation. International archives of occupational and environmental health 2014; 87: 445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Howard G, Till JS, Toole JF, Matthews C, Truscott BL. Factors influencing return to work following cerebral infarction. JAMA : the journal of the American Medical Association 1985; 253: 226–232. [PubMed] [Google Scholar]
- 78. Culler KH, Wang Y-C, Byers K, Trierweiler R. Barriers and facilitators of return to work for individuals with strokes: Perspectives of the stroke survivor, vocational specialist, and employer. Topics in stroke rehabilitation 2011; 18: 325–340. [DOI] [PubMed] [Google Scholar]
- 79. Lock S, Jordan L, Bryan K, Maxim J. Work after stroke: Focusing on barriers and enablers. Disability & society 2005; 20: 33–47. [Google Scholar]
- 80. Hartke RJ, Trierweiler R, Bode R. Critical factors related to return to work after stroke: A qualitative study. Topics in stroke rehabilitation 2011; 18: 341–351. [DOI] [PubMed] [Google Scholar]
- 81. Alaszewski A, Alaszewski H, Potter J, Penhale B. Working after a stroke: Survivors’ experiences and perceptions of barriers to and facilitators of the return to paid employment. Disability and rehabilitation 2007; 29: 1858–1869. [DOI] [PubMed] [Google Scholar]
- 82. Lindström B, Röding J, Sundelin G. Positive attitudes and preserved high level of motor performance are important factors for return to work in younger persons after stroke: a national survey. Journal of rehabilitation medicine 2009; 41: 714–718. [DOI] [PubMed] [Google Scholar]
- 83. Medin J, Barajas J, Ekberg K. Stroke patients’ experiences of return to work. Disability and rehabilitation. 2006; 28: 1051–1060. [DOI] [PubMed] [Google Scholar]
- 84. Koch L, Egbert N, Coeling H, Ayers D. Returning to work after the onset of illness: Experiences of right hemisphere stroke survivors. Rehabilitation counseling bulletin 2005; 48: 209–218. [Google Scholar]
- 85. Bonner B, Pillai R, Sarma P, Lipska K, Pandian J, Sylaja P. Factors predictive of return to work after stroke in patients with mild-Moderate disability in India. European journal of neurology 2016; 23: 548–553. [DOI] [PubMed] [Google Scholar]
- 86. Vestling M, Tufvesson B, Iwarsson S. Indicators for return to work after stroke and the importance of work for subjective well-being and life satisfaction. Journal of rehabilitation medicine 2003; 35: 127–131. [DOI] [PubMed] [Google Scholar]
- 87. Damush TM, Plue L, Bakas T, Schmid A, Williams LS. Barriers and facilitators to exercise among stroke survivors. Rehabilitation nursing 2007; 32: 253–60. [DOI] [PubMed] [Google Scholar]
- 88. Klinke ME, Hafsteinsdóttir TB, Thorsteinsson B, Jónsdóttir H. Living at home with eating difficulties following stroke: a phenomenological study of younger people’s experiences. Journal of clinical nursing 2014; 23: 250–360. [DOI] [PubMed] [Google Scholar]
- 89. Medin J, Larson J, von Arbin M, Wredling R, Tham K. Elderly persons’ experience and management of eating situations 6 months after stroke. Disability and rehabilitation: An International, Multidisciplinary Journal 2010; 32: 1346–1353. [DOI] [PubMed] [Google Scholar]
- 90. O’Sullivan C, Chard G. An exploration of participation in leisure activities post-stroke. Australian occupational therapy journal 2010; 57: 159–166. [DOI] [PubMed] [Google Scholar]
- 91. Garcia SF, Hahn EA, Magasi S. Development of self-report measures of social attitudes that act as environmental barriers and facilitators for people with disabilities. Archives of physical medicine and rehabilitation 2015; 96: 596–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Glassel A, Coenen M, Kollerits B, Cieza A. Validation of the extended ICF core set for stroke from the patient perspective using focus groups. Disability and rehabilitation 2012; 34: 157–166. [DOI] [PubMed] [Google Scholar]
- 93. Heinemann AW, Magasi S, Hammel J. Environmental factors item development for persons with stroke, traumatic brain injury, and spinal cord injury. Archives of physical medicine and rehabilitation 2015; 96: 589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Noreau L, Boschen K. Intersection of participation and environmental factors: a complex interactive process. Archives of physical medicine and rehabilitation 2010; 91: S44–S53. [DOI] [PubMed] [Google Scholar]
- 95. Hammel J, Magasi S, Heinemann A, Whiteneck G, Bogner J, Rodriguez E. What does participation mean? An insider perspective from people with disabilities. Disability and Rehabilitation 2008; 30: 1445–1460. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.