Abstract
Floating thrombus in the aortic arch is an unusual source of systemic embolism. Surgical removal of the thrombus is a therapeutic option, because thrombolytic therapy carries the risk of partial lysis and repeat embolization. We report a case involving a large floating thrombus that originated in the proximal aortic arch and extended into the left subclavian artery and the descending aorta, and we discuss the surgical management.
Key words: Aorta, thoracic/surgery; aortic arch syndromes/complications; thrombectomy/methods; thrombosis/surgery
Mural aortic thrombi can occur anywhere in the aorta and are important causes of distal embolization. A review of the English-language medical literature shows that there are few reported cases of floating thrombus in the aortic arch.1,2 Formation of friable floating thrombus, especially in the proximal aortic arch, creates a life-threatening risk of stroke, as well as peripheral embolization. Treatment is mandatory, once the diagnosis is established. When the floating thrombus is near the branches of the aortic arch, special thought must be given to therapeutic strategy. We discuss the surgical management of a large, floating thrombus that originated in the proximal aortic arch and extended into the left subclavian artery.
Case Report
In August 2003, a 59-year-old woman presented with numbness in the left arm and hand, which had been continuous for the past 3 days. The onset of this numbness had been followed by mild epigastric pain, vomiting, diarrhea, and chills. She had been taking medication for hypertension for about 10 years. There was no history of arrhythmia, ischemic heart disease, diabetes mellitus, or stroke. At admission, the blood pressure was 110/70 mmHg in the right arm and 90/60 mmHg in the left arm; the pulse rate was 78 beats/min.
The patient had been evaluated at another center by means of transthoracic echocardiography and was reported to have a mobile mass with an irregular margin, in the aortic arch. At our center, further investigation by transesophageal echocardiography showed a large free-floating thrombus in the aortic arch (Fig. 1). It appeared to attach to the posterior wall of the proximal aortic arch and to extend into the left subclavian artery and the descending aorta (Fig. 2). There was no evidence of coagulopathies.

Fig. 1 Transesophageal echocardiographic images of a long, floating thrombus (T) in the aortic arch. The stalk can be seen in the proximal aortic arch (A), and the floating end can be seen in the distal aortic arch and the descending aorta (B). The adjacent aortic wall was thickened with diffuse atherosclerosis and focal calcific plaque.
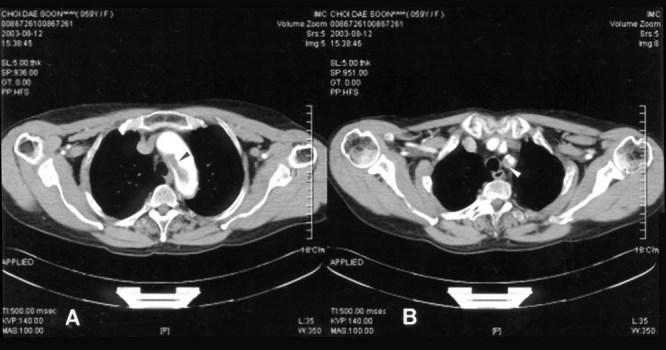
Fig. 2 Computed tomographic images of the floating thrombus A) in the aortic arch (black arrowhead) and B) in the left subclavian artery (white arrowhead).
Anticoagulation therapy was not considered because of the risk of repeat embolization that could result from partial lysis of the thrombus. Instead, we thought it necessary to remove the clot surgically.
At surgery, the aorta was approached via a median sternotomy. For extracorporeal circulation, we placed an arterial perfusion cannula in the proximal ascending aorta about 4.0 cm below the proximal aortic arch (with the cannula tip at some remove from the thrombus), and a venous cannula was placed in the right atrium. After the patient was core-cooled to 17 °C, we induced circulatory arrest and began retrograde cerebral perfusion at a rate of about 400 mL per minute, through the right-angled venous cannula in the superior vena cava. We incised the aortic arch longitudinally, avoiding injury to the phrenic and vagus nerves. With cardiotomy suckers in place, we removed a large thrombus of about 8.5 cm in length (Fig. 3) from the aortic arch, the left subclavian artery, and the descending aorta. A small amount of residual superficial material was removed piecemeal from the roughened base of the thrombus, at the posterior wall of the proximal aortic arch. This base was dimpled like an atheromatous lesion. The lesion was curetted and reinforced with a 2.0-cm round patch of collagen-impregnated woven Dacron aortic graft (Hemashield, Meadox Medicals, Inc.; Oakland, NJ), secured with 4-0 polypropylene running suture. After the aortic arch was closed, the aortic cannula was moved to the usual site on the distal ascending aorta, and retrograde cerebral perfusion was stopped. After de-airing, cardiopulmonary bypass was reinstituted and the patient was rewarmed. The duration of circulatory arrest was 43 minutes.
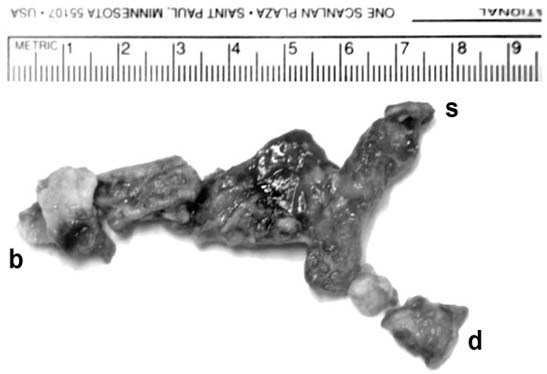
Fig. 3 Organized thrombus. The base of the thrombus (b), the arm that extended into the left subclavian artery (s), and the end that floated within the descending aorta (d) are shown.
The organized thrombus did not show evidence of malignancy on histopathologic examination, but there was a focal aggregation of many neutrophils in the tissue that had been curetted from the dimpled atheromatous base of the thrombus. Two weeks later, after an uneventful recovery, the patient was discharged from the hospital on a regimen of warfarin. At her 1-year follow-up, the patient was doing well and transthoracic echocardiography showed an intact contour wall in the aortic arch.
Discussion
Many factors, such as atherosclerosis, dissection, trauma, malignancy, and coagulopathies, have been associated with aortic mural thrombi. Even though some collected cases of mural thrombus in the ascending aorta and the proximal aortic arch have been reported,3 there have been only a few reported cases of friable floating thrombus in the aortic arch, and in those the base of the thrombus was the aortic isthmus or the ligamentum arteriosum.1,2 In our patient, the origin of the aortic thrombus was an atheromatous lesion in the proximal aortic arch, and the remaining part of the aortic arch was intact. The base of the thrombus was grossly dimpled with ulceration, and histopathologic examination showed focal vascularization and many neutrophils in the curetted tissue. However, this was not evidence of granulomatous aortitis, nor were we able to confirm a diagnosis, due to an inadequate quantity of specimen. It is possible that the main cause of aortic thrombus is aortitis, rather than simple atheromatous lesion.4,5 In our patient, we reinforced the presumed atheromatous lesion with a round patch of collagen-impregnated woven Dacron graft. Prosthetic grafts can be thrombogenic, but we were more concerned about delayed perforation or dissection through the dimpled aortic lesion.
Thrombolysis has been suggested as a promising therapy for aortic thrombus,6,7 and in some cases heparin and warfarin have led to complete resolution in 3 months.8 However, long-term anticoagulation for the complete resolution of a floating, friable thrombus carries unacceptable risk of partial lysis and distal embolization.
A thrombus in the distal aortic arch can be removed under extracorporeal circulation while the heart is beating,2 but a more conservative surgical option is necessary for the excision of thrombi in the proximal or middle aortic arch. In the latter case, it is dangerous to place the arterial perfusion cannula in the distal ascending aorta, which is the usual cannulation site. Walther and colleagues1 removed a thrombus from the aortic arch under hypothermic circulatory arrest, using retrograde perfusion through the femoral artery during extracorporeal circulation. The prospect of retrograde femoral perfusion concerned us, however, for fear of retrograde coronary or cerebral embolization of distal floating thrombus. In our judgment, aortic flow from the arterial perfusion cannula has to be antegrade, like natural aortic flow, in order to prevent retrograde embolization at the beginning of cardiopulmonary bypass. Kalangos and coworkers9 described successful removal of a thrombus in the aortic arch without hypothermic circulatory arrest, by means of selective cerebral perfusion in combination with retrograde femoral artery perfusion. However, hypothermic circulatory arrest with subsequent retrograde cerebral perfusion seems to be simpler than the selective cerebral perfusion technique, because the operation can be completed within the safe limits of circulatory arrest time. Therefore, we placed the arterial perfusion cannula in the proximal ascending aorta so that the cannula tip was well away from the thrombus. After the thrombus had been excised and the base of the lesion repaired, we moved the cannula to the distal ascending aorta in order to evacuate air from the aortic arch and the ascending aorta through a vent at the aortic root (upon re-establishing extracorporeal circulation).
When friable floating thrombus is close to the cerebral branches of the aortic arch, alternative antegrade perfusion techniques and hypothermic circulatory arrest with subsequent retrograde cerebral perfusion enable safe removal of the thrombus and accurate repair of the base of the lesion.
Footnotes
Address for reprints: Jong Bum Choi, MD, Department of Thoracic and Cardiovascular Surgery, Wonkwang University School of Medicine, 344-2 Sinyong-dong, Iksan, Jeonbuk 570-711, South Korea
E-mail: jobchoi@wonkwang.ac.kr
References
- 1.Walther T, Mochalski M, Falk V, Mohr FW. Resection of a thrombus floating in the aortic arch. Ann Thorac Surg 1996;62:899–901. [PubMed]
- 2.Kolvekar SK, Chaubey S, Firmin R. Floating thrombus in the aorta. Ann Thorac Surg 2001;72:925–7. [DOI] [PubMed]
- 3.Goueffic Y, Chaillou P, Pillet JC, Duveau D, Patra P. Surgical treatment of nonaneurysmal aortic arch lesions in patients with systemic embolization. J Vasc Surg 2002;36:1186–93. [DOI] [PubMed]
- 4.Goldman MH, Akl B, Mafi S, Pastore L. Granulomatous aortitis presenting as an acute myocardial infarction in Crohn's disease. Circulation 2000;102:3023–4. [DOI] [PubMed]
- 5.Goldman MH, Akl B, Mafi S, Pastore L. Causes of “idiopathic” aortic thrombus [letter]. Ann Thorac Surg 2003;75: 2009. [DOI] [PubMed]
- 6.Hausmann D, Gulba D, Bargheer K, Niedermeyer J, Comess KA, Daniel WG. Successful thrombolysis of an aortic-arch thrombus in a patient after mesenteric embolism [letter]. N Engl J Med 1992;327:500–1. [DOI] [PubMed]
- 7.Alaeddini J, Ilercil A, Shirani J. Thoraco-abdominal aortic thrombosis and superior mesenteric artery embolism. Tex Heart Inst J 2000;27:318–9. [PMC free article] [PubMed]
- 8.Blackshear JL, Jahangir A, Oldenburg WA, Safford RE. Digital embolization from plaque-related thrombus in the thoracic aorta: identification with transesophageal echocardiography and resolution with warfarin therapy. Mayo Clin Proc 1993;68:268–72. [DOI] [PubMed]
- 9.Kalangos A, Vala D, Bednarkiewicz M, Faidutti B. Technical implications regarding surgical removal of a floating thrombus located in the ascending aorta or aortic arch. Ann Vasc Surg 1999;13:115–20. [DOI] [PubMed]


