Abstract
Ebola virus is a highly pathogenic member of the family Filoviridae that causes a severe hemorrhagic disease in humans and NHP. The 2013–2016 West African outbreak has increased interest in the development and refinement of animal models of Ebola virus disease. These models are used to test countermeasures and vaccines, gain scientific insights into the mechanisms of disease progression and transmission, and study key correlates of immunology. Ebola virus is classified as a BSL4 pathogen and Category A agent, for which the United States government requires preparedness in case of bioterrorism. Rodents, such as Syrian golden hamsters (Mesocricetus auratus), mice (Mus musculus), and guinea pigs (Cavia porcellus), are the most common research species. However, NHP, especially macaques, are favored for Ebola virus disease research due to similarities with humans regarding the pathogenesis, clinical presentation, laboratory findings, and causes of fatality. To satisfy the regulatory requirements for approval of countermeasures against high-consequence pathogens, the FDA instituted the Animal Rule, which permits efficacy studies in animal models in place of human clinical data when such studies are not feasible or ethical. This review provides a comprehensive summary of various animal models and their use in Ebola virus disease research.
Abbreviations: AGM, African green monkeys; CC, collaborative cross; EBOV, Ebola virus; EVD, Ebola virus disease; ffu, focus-forming units; GPA, guinea-pig–adapted; MA, mouse-adapted; rVSV, recombinant vesicular stomatitis virus
The first outbreak of Ebola virus disease (EVD) occurred in Zaire (now Democratic Republic of the Congo) in 1976. In that outbreak of 318 cases, 280 patients (88%) died. The cases were due to close contact and the use of contaminated needles at the hospital where the patients were treated.41,86 Subsequent outbreaks were confined to equatorial Africa until the most recent epidemic. The 2013–2016 EVD outbreak in Western Africa originated in Guinea and spread to Liberia and Sierra Leone, resulting in approximately 11,310 fatalities among approximately 28,616 cases.108 No other filovirus has caused an epidemic on the same scale as observed in Western Africa.3,108 In the wake of this outbreak, interest in developing animal models for the study of pathogenesis, virus characterization, and vaccine and therapeutics research is increasing.
The family Filoviridae consists of nonsegmented, negative-sense RNA viruses subdivided into 3 genera: Ebolavirus, Marburgvirus, and Cuevavirus.15,56,57 The Ebolavirus genus has 5 species—Zaire ebolavirus, Sudan ebolavirus, Bundibugyo ebolavirus, Taï Forest ebolavirus, and Reston ebolavirus.15,41 The Ebola virus (EBOV) isolate responsible for the 2013–2016 outbreak is a member of the genus Zaire ebolavirus and was named ‘Makona’ (Ebola virus/H.sapiens-wt/GIN/2014/Makona-C15) after a river shared by the 3 most affected countries.56,108
All ebolaviruses, with the exception of Reston virus, cause infections exhibiting severe viral hemorrhagic fever, with lethality in humans averaging 40.3%.56 As such, filoviruses are considered Category A Bioterrorism Agents by the Centers for Disease Control and Prevention, Tier 1 Select Agents by the US Department of Health and Human Services, and priority pathogens needing urgent research by the World Health Organization. Accordingly, all work with filoviruses is performed under BSL4 conditions.3,5
Animal Models of Ebola Virus Infection
EBOV is a zoonotic pathogen that has been reported to infect several animal species, but exactly which animal species plays a role in transmission of EBOV infection to humans is still under investigation.108 Exhaustive efforts to find the natural host have resulted in the general agreement that fruit bats, which can be asymptomatically infected with EBOV, are likely to be a main reservoir species.41,60
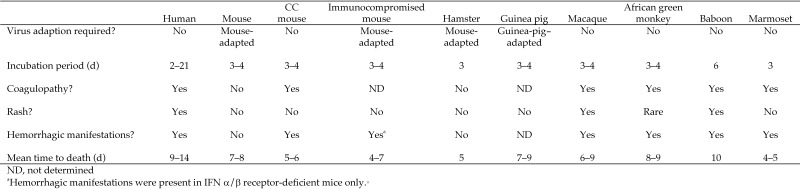
A variety of animal models (Figure 1) have been developed for basic research into the characterization of the virus, elucidation of pathogenesis, and development of countermeasures. Such models including immunocompetent mice, immunodeficient mice,6 hamsters,100 strain 13 guinea pigs, outbred guinea pigs, macaques, African green monkeys (Chlorocebus aethiops),78 marmosets (Callithrix jacchus), and baboons (Papio spp.).5,79 Among the many species used for EBOV research, the preferred models for studies on pathogenesis, treatment, and vaccines remain rhesus (Macaca mulatta) and cynomolgus (M. fascicularis) macaques.78,100
Figure 1.
Comparison of signs and symptoms of Ebola virus disease between humans and animal models.
Mouse Models
Although NHP are considered the most representative model of EVD,30,37 limited space in high-containment vivariums, financial considerations, and ethical issues regarding the use of NHP continue to fuel the development of small animal models for EBOV infection. Because of the availability of mice in large numbers and the existence of a wealth of reagents for biochemical and immunologic testing, these rodents are the preferred small animal model for filovirus research.9 Immunocompetent mice are resistant to WT EBOV.3,12,102 Immunocompromised mice are not well established as models of EBOV infection and are considered of limited use because of their immune status, but previously they were the only mice that could be infected with WT EBOV.80
WT EBOV is lethal to suckling mice and immunodeficient mice, such as SCID mice, which lack functional B and T cell responses. Suckling mice and knockout mice lacking a complete type I IFN response (for example, lack of expression of cytoplasmic signal transducer and activator of transcription 1 protein,23,84 IFN receptor α/β) uniformly die within a week of subcutaneous challenge with a variety of filovirus strains.9,11,12 After challenge with filoviruses, SCID mice remained healthy for approximately 14 d, but then developed gradual, progressive weight loss and slowing of activity and succumbed on 20 to 25 d after inoculation.5,12,102 Aerosol but not intraperitoneal challenge with the outbreak isolate, EBOV-Makona, in female A129 IFN α/β receptor–deficient mice is lethal.92 Signal transducer and activator of transcription 1 knockout mice developed severe disease from aerosol inoculation.62
Rodent models have been developed using EBOV-Makona and EBOV-Mayinga isolates through serial passage in both mice and guinea pigs.5 The 1976 Mayinga isolate of EBOV, Ebola virus H.sapiens-tc/COD/1976/Yambuku-Mayinga, was adapted to lethal virulence for adult, immunocompetent mice through serial passage in newborn, suckling, and progressively older weanling mice, by using intraperitoneal injections of liver homogenate.3,9,13 The resulting mouse-adapted EBOV (MA-EBOV), when administered intraperitoneally, caused lethal disease in adult C57Bl/6, BALB/c, and CD1 mice at approximately 5 to 6 d after inoculation and that resembled EVD in NHP.3 No adapted filoviruses cause disease in immunocompetent mice when administered intramuscularly or subcutaneously; only intraperitoneal injection produces uniform disease and lethality.3
Overall, mouse models of EBOV infection demonstrate rapid onset of viremia and high viral burden in the spleen, liver, and multiple organ tissues. Lymphopenia, thrombocytopenia, kidney dysfunction, and liver damage resulting in high serum concentrations of AST and ALT are observed.9,10,14,91 Liver and kidney function is diminished in mice, similar to that seen in rhesus macaques, and histopathologic findings include extensive necrosis of the liver, spleen, and other organs. Widespread lymphocyte apoptosis is observed in both species.9 A proinflammatory cytokine profile, including TNFα, IFNγ, IL8, macrophage inflammatory proteins 1α and 1β, and monocyte chemoattractant protein 1, resembles that seen in EBOV-infected rhesus macaques.9,13 Lymphoblast formation indicating lymphocyte activation, increased T-cell CD44 expression, and increased circulating lymphocytes late in infection have been found in mouse and macaque models. Commonly used mouse models (such as BALB/c and C57BL/6 mice) exhibit little to no coagulopathy or hemorrhagic manifestations (for example, tissue fibrin deposition, disseminated intravascular coagulation) or the characteristic maculopapular to petechial rash observed in patients with EVD.3,13,38
In 2004, a genetically diverse panel of recombinant inbred mice, collaborative cross (CC) mice, was obtained through a systematic cross of 8 inbred founder mouse strains. Five of these 8 strains are classic laboratory strains (C57BL/6J, A/J, 129S1/SvImJ, NOD/ShiLtJ, NZO/H1LtJ).83 The remaining 3 founders are from wild-derived strains selected to represent Mus musculus subspecies (M. m. musculus, M. m. domesticus, and M. m. castaneous).97 Genetic analysis reveals that the 8 strains capture almost 90% of the known genetic variation present in laboratory mice and that the captured variation is randomly distributed across the genome.87,97 Currently, CC mice consist of hundreds of independently bred, octo-parental recombinant inbred lines.97
The use of CC mice substantially expands the number of EBOV-related disease manifestations observed. Exposure of these strains to MA-EBOV yielded a wide variety of outcomes.83 The CC mouse line 13140 × 3015 (susceptible to lethal EVD) exhibited typical lesions as seen in humans. By day 5 after inoculation with MA-EBOV, CC mice presented with prolonged blood coagulation, internal hemorrhage, coffee-colored blood, splenomegaly, and hepatic discoloration and softened texture. However, the mice did not show these signs after infection with WT EBOV. Susceptible CC mice also had significantly prolonged thrombin time, PTT, and APTT compared with C57BL/6J mice, suggesting that host genetic background plays a role in disease development.83
A humanized mouse model on a NOD/ShiLtJ background, NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ, shows promise for the study of WT EBOV infections in mice.6,80 These mice are highly immunodeficient, because they lack functional murine macrophages, dendritic cells, T cells, B cells, and natural killer cells. These cells are nonfunctional because of mutations in multiple genes, including those encoding protein kinase, DNA-activated catalytic polypeptide, and X-linked IL2 receptor γ chain (gene-targeted mutation 1), which results in SCID.6 When humanized through transplantation of bone marrow cells and liver and thymus tissue, these mice typically have high levels of engraftment of functional human macrophages, dendritic cells, T cells, B cells, and natural killer cells.6,48,80
Challenge with 1 × 104 focus-forming units (ffu) of Mayinga WT EBOV isolate caused uniformly lethal EVD in these humanized mice, with histologic changes in the liver and upregulation of cytokines and chemokines corresponding closely to those seen in human patients with EVD.6,80 With lower-dose challenges of 10 ffu of either Mayinga or Makona EBOV isolate, the severity of EVD in such mice was lower; thus, the severity of infection is dose-dependent.6 Unlike the situation with most prior mouse models, WT EBOV was able to cause disease in these humanized mice, suggesting that interactions between the virus and the model's immune system is similar to that observed in humans.6,80 With the humanized bone marrow, liver, and thymus mouse model, researchers can examine the activity of filovirus-specific therapeutic agents and vaccines that directly target cells derived from hematopoietic stem cells.65,80 One drawback of using humanized bone marrow, liver, and thymus mice is the variability of immune characteristics among human donors. However, the possibility of using donors with immune characteristics associated with EVD susceptibility could increase the value of the model. Prior to the development of this model, only NHP infected with WT EBOV could be studied for the development of vaccines and therapeutics, given that rodent models require MA- or guinea-pig–adapted (GPA) EBOV to produce EBOV infection.
Hamster Models
Because of their short life cycle and the ease with which they are bred in captivity, Syrian golden hamsters (Mesocricetus auratus) are a readily available rodent candidate for use in infectious disease research. When experimentally infected with MA-EBOV, Syrian hamsters have disease manifestations similar to those of humans and NHP, including the severity of coagulopathy, which does not occur in mouse and guinea pig models.27 Although Syrian hamsters have been thoroughly characterized for use in EVD studies,1 their ability to develop coagulopathies makes them a valuable animal model for studying other viral hemorrhagic fevers.27 As in the mouse model, WT EBOV does not cause clinical signs in hamsters, although a low level of replication can occur.3,100 MA-EBOV replicates to high titers in hamsters, causing significant organ damage, especially in the liver and spleen. When hamsters are challenged intraperitoneally or subcutaneously with MA-EBOV or WT EBOV, only MA-EBOV administered intraperitoneally mimics human disease.
Manifestations of MA-EBOV infection in Syrian hamsters include cytokine dysregulation (suppression of early type I IFN responses), severe coagulopathy, lymphocyte apoptosis, target organ necrosis or apoptosis (lymph nodes, spleen, liver), and lethal outcome.27,73,100 Suppression or noninduction of type I IFN responses and aberrant proinflammatory responses in infected hamsters, which are also seen in the signal transducer and activator of transcription 1 mice, are suggested as critical pathogenic processes leading to lethal outcomes.4,23,27,84,100 In terminally ill Syrian hamsters, all cytokines tested (IL1β, IL2, IL4, IL6, and IL12p35; TNFβ, IFNγ-induced protein 10, IFNγ, and TNFα) are upregulated in the spleen, liver, and blood, indicating potentially uncontrolled immune responses. The severe coagulopathy seen in hamsters is similarto that seen in macaques infected with WT EBOV. MA-EBOV–infected hamsters have significantly prolonged PTT, APTT, and thrombin times during late stages of infection.27 Coagulopathy was preceded by an initial abnormal increase in fibrinogen concentrations, representing the acute-phase response to EBOV infection.27
The spleens, livers, and lymph nodes of EBOV-infected hamsters have degenerative changes similar to those seen in macaques. Multifocal acute splenitis is characterized by lymphocyte depletion and tissue destruction.27,100 Hepatic changes include diffuse hepatocellular degeneration and necrosis, with infiltration of moderate numbers of neutrophils, decreased numbers of macrophages, and the presence of intracytoplasmic inclusion bodies.27,73,100 Fibrin deposition in the liver is reported to be similar to that seen in macaques and humans.27,73 In addition, lymph nodes from EBOV-infected hamsters display diffuse lymphocytic necrosis and loss, along with acute lymphadenitis and draining hemorrhage.
Recently a new Syrian hamster strain has been developed that does not express the cytoplasmic signal transducer and activator of transcription 2 protein (signal transducer and activator of transcription 2 knockout hamsters). As in signal transducer and activator of transcription 1 mice, the type I IFN pathway in these hamsters is disrupted, which is an important part of the innate immune response to virus infection.98 This strain is the first genetically modified Syrian hamster strain ever reported, although it has yet to be used as an animal model of EVD.
Unlike mice, whose genome has been fully sequenced, a limited number of Syrian hamster genes involved in the spectrum of fundamental biologic processes have been identified.28 The limited genomic information is a significant downside to using Syrian hamsters as an EBOV model and, more broadly, as a model for infectious disease research. However, the recent elevation of Syrian hamsters in the sequencing priorities of the Human Genome Research Institute ultimately will expand their use as a valuable infectious disease animal model.63
Guinea Pig Models
Both outbred Duncan–Hartley and inbred strain 13 guinea pigs have been used as models of EVD for the evaluation of pathogenesis, vaccines, and therapeutic agents. Compared with most other rodent models, the larger size of guinea pigs is reflected in a greater circulating blood volume. With greater blood volume, the increased blood sampling and dosing adjustments necessary for optimizing therapeutic agent and vaccine development are possible.21 Guinea pigs inoculated with WT EBOV develop only a short-lived, nonlethal febrile illness.5,91 Like NHP, guinea pigs can be infected by peripheral routes in addition to intraperitoneal inoculation. Several different GPA filoviruses were generated over the last few decades, most of which required only 8 or fewer passages of the original WT EBOV in adult guinea pigs before a lethal phenotype was achieved.3,5,19 The animals showed few signs of EBOV infection until day 5, at which time they developed a fever and became anorexic and dehydrated. A maculopapular rash did not develop in these animals. Hemorrhage was not seen in this model, but a drop in platelet counts, increased fibrin deposition (more than mice), and prolonged PT and APTT occurred.5,9,100
Guinea pigs exhibit histopathologic lesions and serum chemistry changes during filovirus infection similar to those of mice, NHP, and humans. After GPA-EBOV challenge, the virus was first detected in lymph node macrophages as early as 24 hours after inoculation, spread to the spleen and liver on day 2 after inoculation, and subsequently to the other organs and tissues.19 The disease course of GPA-EBOV–infected guinea pigs includes splenic and hepatic pathology, lymphocyte apoptosis, neutrophilia, thrombocytopenia, and marked granulocytosis. In outbred Hartley guinea pigs, changes in the serum biochemistry profile include marked increases in liver-associated enzyme concentrations and significant hypoalbuminemia.21
In contrast to similarities to the serum biochemistry profiles of other rodents and humans, strain 13 guinea pigs demonstrate altered immune responsiveness.21 Thus, these guinea pigs may not be representative of the heterogeneous immune responses of outbred hosts such as NHP and humans. Compared with older models of GPA-EBOV in inbred strain 13 guinea pigs, recently developed models in outbred Hartley guinea pigs infected with GPA-EBOV show evidence of bystander lymphocyte apoptosis and a marked proinflammatory response. However, the proinflammatory response observed may simply be a function of the increased availability of guinea pig reagents used to characterize proinflammatory responses.3,21
In addition the use of the guinea pig model to explore the natural history of EVD, these animals have been used to test therapeutic agents against EVD. Antibody therapy against filoviruses with equine IgG containing high concentrations of antiEBOV antibodies protected guinea pigs after GPA-EBOV infection.51,55 In another GPA-EBOV challenge study, guinea pigs were protected from lethal infection in a dose-dependent manner by a monoclonal antibody, KZ52, which was derived from a human survivor of EVD.77
Nonhuman Primate Models
NHP are the preferred animal model for human filovirus infection, because they can be fatally infected by various routes with human virulent, nonadapted strains of EBOV.29 NHP recapitulate human disease quite accurately in terms of clinical symptoms (fever, anorexia, and rash), clinical chemistry profile (increase in liver enzymes, disruption of coagulation), and pathologic changes. As in humans, monocytes, macrophages, and dendritic cells are primary sites of filovirus replication in NHP. A few published studies detail EBOV infection in marmosets and baboons, but the majority of research studies describe the pathogenesis of EBOV infections in cynomolgus or rhesus macaques (favored NHP models) or African green monkeys (AGM).91 Currently, only macaques recapitulate many clinical hallmarks of fatal filovirus disease observed in humans, including high viremia, coagulation abnormalities, and an aberrant proinflammatory cytokine response.3
Macaque models.
Cynomolgus macaques have been the species most often used for vaccine studies, whereas rhesus macaques have been more frequently used for evaluating therapeutics.37 This difference in species usage results from the slightly shorter disease course in cynomolgus macaques as compared with that observed in rhesus macaques.37 Results of multiple studies have shown that filovirus infection in macaques closely reproduces what is known about the disease in humans.30,34,37 The macaque incubation period of ebolavirus infections is similar to that seen in humans, although the route of inoculation, the ebolavirus isolate used, and challenge dose affect disease progression.34,73 Results of studies in macaques have shown that EBOV doses as low as 2 to 15 pfu, administered by a variety of challenge routes, can produce a lethal filovirus infection.85,94,95
The initial onset of EVD signs in macaques occurs by approximately 3 to 5 d after exposure and includes fever and malaise, followed by anorexia, depression, lethargy, diarrhea, vomiting, and development of a maculopapular rash. Hemorrhagic manifestations can be seen, including petechiae, ecchymosis, and bruising; hemorrhage at venipuncture sites; epistaxis; hematochezia; and hematuria. CBC abnormalities include neutrophilia, lymphopenia, thrombocytopenia, decreased Hct, and early monocytosis. Clinical chemistry results are typical of that seen in severe dehydration and kidney impairment, including high BUN and creatinine concentrations and hypocalcemia.26,67,94 Increases in the liver enzymes AST and ALT can occur as early as 3 to 5 d after challenge.94 Coagulation panels reveal increased prothrombin time and PTT, and elevations in fibrin degradation products and D-dimers.34,85
Monocytes, macrophages, and dendritic cells are primary sites of filovirus replication in macaques, and some researchers consider that high levels of tissue factor expression by filovirus-infected monocytes and macrophages trigger disseminated intravascular coagulation.37,67 Infection with EBOV leads to early and robust IFN-like responses that occur before the appearance of circulating virus. This response occurs not only from circulating immune cells but also throughout the majority of infected tissues.16,67 Prior to succumbing to infection, macaques exhibit characteristic inflammatory cytokine, chemokine, and growth factor profiles, such as increased production of eotaxin, IFNγ-induced protein 10, monocyte chemoattractant protein 1, and IL6, similar to what is seen in EVD patients.67 Macaques are often euthanized at 7 to 9 d after exposure, due to multiorgan failure, hypovolemic shock, and severe dehydration.30,37
A number of administration routes have been used to mimic different transmission routes of EBOV infection in macaques. The most commonly used route of EBOV infection in macaques is intramuscular injection (1000 pfu), mimicking a needle-stick injury in a laboratory setting. Although airborne transmission is not thought to be a significant route of human infection,76 aerosolized virus causes a rapidly lethal disease in experimentally infected NHP. In the research setting, aerosol inoculation mimics either large droplets or small particles circulating near human patients. Several NHP studies have attempted to show transmission through aerosol, fomites, and indirect exposure to body fluids of experimentally inoculated animals to other animals housed in the same room. In one study, control rhesus macaques, which were located 3 m from the experimental rhesus macaques challenged intramuscularly with EBOV, became infected.49 In that study, the pattern of pulmonary antigen staining on pathology specimens suggested aerosol infection. Alternatively, transmission might have occurred through various behavioral activities or through routine animal husbandry practices.2,76
Another study showed transmission between 6 EBOV-infected piglets (swine) and 4 cynomolgus macaques; the animals were separated by a wire barrier 20 cm in front of the NHP cages.106 Transmission could have resulted from inhalation of aerosols, inoculation of mucous membranes by droplets, or by fomite transmission. Although animal caretakers were trained to avoid cross-contamination of the cages during husbandry practices, inadvertent transfer during husbandry procedures could not be ruled out. In a contrasting study, 2 rhesus macaques infected intramuscularly with EBOV were housed in open barred cages adjacent to 2 uninfected rhesus macaques, that did not become infected.2 The infected macaques had high titers of circulating virus, but oral, nasal, and rectal swabs did not produce infectious virus.
In several studies examining mucosal exposure, investigators found that rhesus macaques were successfully infected through the conjunctival and oral routes, as in humans,50 but required higher doses (5.2 log10 of EBOV Mayinga isolate) than for parenteral routes.50,70 Doses of 10 pfu by oral or conjunctival routes did not result in clinical disease in cynomolgus macaques.70
In addition to the use of macaques to study the natural history of EBOV infection and transmission of the virus, these species have been used to evaluate therapeutic interventions. Vaccines against EBOV have typically been screened initially in guinea pigs, mice, and hamsters.11,14,96 Unfortunately, because filovirus isolates from humans or NHP do not cause severe disease in rodents, candidate vaccines must ultimately be tested in NHP. Several vaccine platforms, including replicating and nonreplicating viral vector approaches (for example, rabies virus, adenovirus, vesicular stomatitis virus [VSV], paramyxoviruses), subunit vaccines, and DNA vaccines have shown promise in macaque models. However, safety and manufacturing concerns with these vaccines still exist.
A replication-competent recombinant VSV (rVSV)-vectored EBOV (rVSV–EBOV), also known as rVSV-ZEBOV, candidate vaccine protected rhesus macaques from lethal EBOV challenge after single-dose vaccination, even when given a week prior to EBOV exposure.68 WT VSV infection is an exotic disease of livestock in the United States, causing vesicles and ulceration of the mucous membranes, hooves, and teats. Disease due to VSV is clinically indistinguishable from foot and mouth disease.88 Replication-competent viral vector vaccines in general are a concern due to issues such as this one. Human infections are rare and asymptomatic or cause very mild influenza-type illness, although more severe disease has been described.1
Therefore, rVSV appears to be a good candidate as a vaccine platform for EBOV. In addition, the rVSV–EBOV vaccine has been shown to be somewhat protective in rhesus macaques when given 1 and 24 h after EBOV exposure.68 All animals became clinically ill, including the survivors. The rVSV–EBOV vaccine is currently in phase I–III clinical trials in Europe and Africa.1,53
In evaluating the other vectors of EBOV vaccines in macaques, a live rabies virus replication-competent vaccine provided 100% protection without significant morbidity after EBOV challenge, whereas the inactivated candidates (no adjuvant) provided 50% or less protection in infected rhesus macaques, and all animals became ill.7,52 The replication-incompetent rabies virus vaccine showed increased efficacy when paired with an adjuvant.52
An additional vaccine approach in macaques uses replication-defective adenoviruses, such as recombinant adenovirus serotype 5.39,95 Although multiple vaccinations of recombinant adenovirus vector with multiple EBOV glycoprotein and nucleoprotein virus-like particles have been used, one study using a single dose of a recombinant, replication-deficient, adenovirus-vectored vaccine showed equal efficacy to multiple vaccinations.94 The biggest drawback to using adenoviral vectors in humans is that many people have preexisting immunity to adenovirus serotype 5, thus decreasing the immunogenicity of the vaccine.94 In the United States, Western Europe, and Kenya, the adult prevalence of neutralizing antibodies to human adenovirus 5 has been 30%, 50%, and as high as 98%, respectively.24,39 Adenovirus vectors that are less common or those found in chimpanzee populations have been tested, but protection against lethal challenge in EBOV- challenged macaques is variable.39 Recently, a chimpanzee adenovirus type 3 vectored EBOV vaccine phase II-III trial is ongoing to evaluate the safety and efficacy of the vaccine.53
An alternative to virus-vectored EBOV vaccines, nonreplicating protein subunit-based vaccine platforms using virus-like particles protected macaques. Virus-like particles are composed of as many as 4 filovirus proteins: nucleoprotein, VP24, VP40, and glycoprotein. Virus-like particles are highly immunogenic, and vaccination induces innate, humoral, and cellular immune responses in macaques and chimpanzees.101,104 Compared with replication-competent platforms, virus-like particles are considered a safer approach.101,104 In one study, all EBOV-challenged cynomolgus macaques (n = 5) survived after a 3-dose virus-like particle vaccine protocol using RIBI (trehalose dimycolate, monophosphoryl-lipid A, cell wall skeleton) adjuvant.59,105 Results from a second study in which NHP were pretreated with 2 doses of virus-like particles and QS21 adjuvant indicated that all cynomolgus macaques (n = 3) were protected from morbidity after subsequent EBOV challenge.103
DNA vaccines have been developed against a number of viruses including EBOV. DNA vaccines are noninfectious, can be rapidly developed in large quantities, and can used in multiple-boost regimens; all of these qualities are important when working with emerging infectious pathogens.39 DNA vaccines are administered intramuscularly through electroporation using a gene gun.40,45 The vaccines require several boosts but induce both humoral and cellular immunity in cynomolgus macaques.
Several studies have evaluated the efficacy of EBOV DNA vaccines in macaques. One study using EBOV glycoprotein DNA vaccine protected 5 of 6 cynomolgus macaques against lethal EBOV challenge.40 In another study, DNA combination vaccines expressing glycoprotein from 3 ebolaviruses (that is, EBOV, Sudan, and Ivory Coast) were used in combination in cynomolgus macaques, followed by challenge with EBOV Mayinga isolate.95 Antibody responses to adenovirus vector expressing EBOV glycoprotein were not reduced compared with administration of the single DNA vaccine, and the combination was protective against EBOV lethal challenge.95 Another strategy included DNA vaccination followed by a boost with recombinant adenoviral vectors encoding Ebola viral proteins.93-95 Cynomolgus macaques subsequently challenged by a lethal EBOV dose were uniformly protected, and 3 of 4 animals had sterilizing immunity; the remaining animal had mild viremia.89
Macaques are frequently used for studying therapeutic agents and countermeasures. The majority of those examined since the 2013–2016 West African outbreak represent antivirals and antimicrobials, many of which are FDA approved for treatment of other virus infections such as influenza, cytomegalovirus infections, HIV, and adenovirus infections. Other interventions include passive transfer of hyperimmune IgG from horses to NHP, monoclonal antibodies,43 and small-protein therapeutics. The administration of hyperimmune horse serum IgG to cynomolgus and rhesus macaques failed to produce significant reductions in morbidity and fatalities.54,74
The most famous monoclonal antibody therapy is ZMapp, a combination of 3 monoclonal antibodies that bind to the glycoprotein of EBOV.71 When ZMapp was given to rhesus macaques 24 or 48 h after EBOV exposure, 4 of 6 animals survived with little viremia and only a few clinical signs.75 In another rhesus macaque study, ZMapp given as late as 5 d after inoculation, when rhesus macaques became viremic, was 100% protective (n = 6).82 In a small, randomized phase I–II clinical trial in West African patients with EVD, ZMapp plus current standard of care (for example, replacement IV fluids, antiemetics, gastric acid inhibitors, antibiotics, antimalarials, antipyretics) were beneficial, but results did not meet the threshold of superiority over supportive care alone.81
Small proteins have also been used as therapeutic interventions in macaques. Recombinant nematode anticoagulant protein c294 and recombinant human activated protein C44—typically used to treat coagulopathy and sepsis, respectively—can be used to treat viral hemorrhagic fevers. Coagulopathy and sepsis occur in EBOV-infected human patients and people with other types of viral hemorrhagic fevers, although these manifestations are not specific for viral hemorrhagic fevers. Approximately 33% of NHP that were treated with nematode anticoagulant protein C (10 min or 24 h after EBOV challenge) were protected from EVD after EBOV challenge.5 Similarly, 18% of NHP that received recombinant human activated protein C 30 to 60 min after EBOV challenge survived.44 Survival in treated animals that succumbed to disease was approximately 4 d longer compared with that observed in control animals.
Lipid nanoparticle-encapsulated short interfering RNAs were adapted to target the new Makona outbreak isolate of EBOV. In one rhesus macaque study, 2 compounds together were efficacious (66% to 100% survival), with milder clinical signs than those observed in control animals.96 The drug consists of 3 distinct short interfering RNA sequences formulated in self-assembling nucleic acid–lipid nanoparticles. These nucleic acids were chemically modified to eliminate any immune-related toxicities associated with the short interfering RNAs. The drugs caused the destruction of mRNA, resulting in the downregulation of EBOV proteins VP24, VP35 and L, which are required for virus assembly, transcription, and replication, and the evasion of host IFN response.36,42,46,99 The therapy was 100% protective against lethal challenge, and clinical signs were diminished but present in rhesus macaques,96 but studies in human patients in West Africa did not confirm the efficacy seen in macaque studies.25
African green monkey model.
Marburg virus, a filovirus closely related to EBOV, was first recognized in 1967, when outbreaks of hemorrhagic fever occurred simultaneously in laboratories in Marburg and Frankfurt, Germany, and in Belgrade, Yugoslavia (now Serbia). Laboratory research workers exposed to imported AGM or their tissues18,66 spread the disease to medical personnel and family members.
In addition to Marburg virus susceptibility, AGM have been studied as models of EBOV infection. The EVD progression in AGM is similar to that seen in rhesus macaques.8,22 Unlike macaques, maculopapular rash does not occur, and no behavioral changes, such as anorexia or depression, are reported.22,85 In one study, EBOV aerosol exposure resulted in greater fever severity and platelet loss in AGM than in macaque species. Both the extrinsic and intrinsic coagulation pathways were more affected in AGM than in similarly infected macaque species.85 In an AGM study, EBOV-induced coagulopathies, with fibrin thrombosis, were observed in all abdominal organs.73 By using AGM, fibroblastic reticular cells in lymph nodes were first identified as EBOV targets.22 Despite these findings, AGM have a higher survival rate after filovirus infections than do macaques, with the exception of infection with EBOV-Mayinga isolate, which is uniformly fatal.31
Marmoset model.
Marmosets (small [less than 500 g] New World callitrichid primates), have been used as a model of EVD.17,92 Like other NHP species, common marmosets are susceptible to WT, nonadapted EBOV. Like AGM, filovirus-infected marmosets do not develop a petechial rash.5,17,22 Marmosets can be infected by the intramuscular or aerosol route.92 Animals exhibit anorexia, weight loss, and fever, but unlike humans and macaques, marmosets succumb early, by day 4 to 5 after exposure.91 Similarities to human disease include clinical signs, hepatocellular necrosis, and extensive fibrin deposition. Marmosets demonstrate coagulation abnormalities, including thrombocytopenia, hemorrhage and bleeding from venipuncture sites.91 In addition, marmosets develop high viral titers, which exceed 105 or 106 genomic viral RNA equivalents per milliliter of tissue homogenate in most tissues and higher titers in the adrenal glands, lymph nodes, spleen, and liver.17,91 Although one group17 has identified several reagents for tagging and tracking marmoset cells in studies, fewer immunologic tools are available for marmosets than macaques. The very small size of marmosets limits blood collection.107
Baboon model.
Since 1994, Russian researchers have studied EBOV infection in baboons (Papio hamadryas).79 Baboons are somewhat more resistant to infection from all ebolavirus species, compared with macaques.5,31,32,89,90 The baboon DNA sequence is more similar to human DNA than macaque DNA, differing by only 4%; whereas DNA from humans and macaque species differ by 6.5%.58,72,79 In a seroprevalence survey of NHP, wild baboons were positive for antiEBOV IgG, suggesting that baboons may be a natural reservoir.61 Despite their susceptibility to natural EBOV infection in the wild, the use of baboons as a model of human infection has been limited in the United States.61,79 The disease course in baboons is similar to that seen in infected humans. Baboons and humans both have a 4- to 5-d prodromal period, followed by sudden onset of fever, anorexia, and depression and progression to widespread hemorrhagic manifestations. Petechial rash did not occur until day 7 after inoculation in baboons as compared with day 4 to 5 after inoculation in macaques.73 Results from one study found hemorrhage in all visceral organs, most notably the liver and spleen.73 In several studies, peripheral lymphadenopathy occurred at 3 to 4 d after inoculation, and cutaneous maculopapular rash appeared on days 6 to 8 after inoculation—several days later than the onset of rash in macaques.47,64,79,89
Baboons have been used for EBOV vaccine research and for the evaluation of therapeutic interventions. Results from a study on an early vaccine, using inactivated EBOV, showed complete protection against lethal challenge in 4 of 5 hamadryad baboons.35,69 However, results from other studies suggested that inactivated EBOV vaccine did not induce sufficient immunity to reliably protect hamadryad baboons against lethal challenge.20,35 One therapeutic study involving hyperimmune horse serum IgG showed partial protection of hamadryad baboons, but the challenge dose (10 to 30 pfu) was lower than the standard 1000 pfu.55
The large size of adult baboons and the disparity in size between adult and juvenile baboons favor macaques over baboons for research. Most baboons used in biomedical research are 1 to 3 y old and weigh 3 to 12 kg. Young baboons require a smaller cage (that is, group 4) when singly housed. Because adult male baboons can exceed 25 kg and adult females range in weight from 12 to 18 kg, both sexes must be housed in group 5 or 6 primate cages.46
Conclusions
Since the first appearance of EVD 40 y ago, progress in the development of animal models for EVD has been considerable. The 2013–2016 outbreak underscores the critical importance of animal models in the search for vaccines and therapeutics. Although rodent models, with the possible exception of humanized mice, require serial passage of EBOV to acquire lethal infectious capacity, mice, hamsters, and guinea pigs remain the model of choice for preliminary studies on countermeasures and vaccines. The advantages of the small animal models include ease of handling, relative affordability, ability to perform experiments with many subjects, and defined genetic backgrounds. In particular, Syrian golden hamsters and some strains of CC mice have clinical courses and severity of coagulopathy seen otherwise only in humans and NHP. Whereas guinea pigs and hamsters may provide models with higher fidelity to EVD than do mice, the current lack of species-specific immunologic tools limits their use.
Macaques remain the model of choice for EBOV research because they can be infected with WT EBOV, and they exhibit disease progression that is similar to that seen in humans, including coagulopathy, multiorgan failure, and proinflammatory cytokine profiles. Macaques do not exactly mirror human disease. EBOV causes 100% lethality in untreated macaques, whereas the human fatality rate in the West African outbreak was approximately 40%.108 However, all of the current animal models have their place in research. To obtain licensing under the FDA Animal Rule, 2 animal models must be used to show efficacy of treatments and vaccines, unless a single animal model adequately recapitulates human disease.33 Since 2013, the interest in and use of animals in EBOV basic research and the development of countermeasures have greatly increased and will further the refinement of animal models.
Acknowledgments
The content of this publication does not necessarily reflect the views or policies of the US Department of Health and Human Services (DHHS) or of the institutions and companies affiliated with the authors. This work was funded in part through Battelle Memorial Institute's prime contract with the US National Institute of Allergy and Infectious Diseases (NIAID) under contract no. HHSN272200700016I. Dan Ragland, a coparticipant in this work, is an employee of Charles River Laboratories.
References
- 1.Agnandji ST, Huttner A, Zinser ME, Njuguna P, Dahlke C, Fernandes JF, Yerly S, Dayer JA, Kraehling V, Kasonta R, Adegnika AA, Altfeld M, Auderset F, Bache EB, Biedenkopf N, Borregaard S, Brosnahan JS, Burrow R, Combescure C, Desmeules J, Eickmann M, Fehling SK, Finckh A, Goncalves AR, Grobusch MP, Hooper J, Jambrecina A, Kabwende AL, Kaya G, Kimani D, Lell B, Lemaitre B, Lohse AW, Massinga-Loembe M, Matthey A, Mordmuller B, Nolting A, Ogwang C, Ramharter M, Schmidt-Chanasit J, Schmiedel S, Silvera P, Stahl FR, Staines HM, Strecker T, Stubbe HC, Tsofa B, Zaki S, Fast P, Moorthy V, Kaiser L, Krishna S, Becker S, Kieny MP, Bejon P, Kremsner PG, Addo MM, Siegrist CA. 2016. Phase 1 trials of rVSV Ebola vaccine in Africa and Europe. N Engl J Med 374:1647–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alimonti J, Leung A, Jones S, Gren J, Qiu X, Fernando L, Balcewich B, Wong G, Stroher U, Grolla A, Strong J, Kobinger G. 2014. Evaluation of transmission risks associated with in vivo replication of several high containment pathogens in a biosafety level 4 laboratory. Sci Rep 4:5824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Banadyga L, Dolan MA, Ebihara H. 2016. Rodent-adapted filoviruses and the molecular basis of pathogenesis. J Mol Biol 428:3449–3466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basler CF, Amarasinghe GK. 2009. Evasion of interferon responses by Ebola and Marburg viruses. J Interferon Cytokine Res 29:511–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bente D, Gren J, Strong JE, Feldmann H. 2009. Disease modeling for Ebola and Marburg viruses. Dis Model Mech 2:12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bird BH, Spengler JR, Chakrabarti AK, Khristova ML, Sealy TK, Coleman-McCray JD, Martin BE, Dodd KA, Goldsmith CS, Sanders J, Zaki SR, Nichol ST, Spiropoulou CF. 2016. Humanized mouse model of Ebola virus disease mimics the immune responses in human disease. J Infect Dis 213:703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blaney JE, Marzi A, Willet M, Papaneri AB, Wirblich C, Feldmann F, Holbrook M, Jahrling P, Feldmann H, Schnell MJ. 2013. Antibody quality and protection from lethal Ebola virus challenge in nonhuman primates immunized with rabies virus–based bivalent vaccine. PLoS Pathog 9:e1003389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bowen ET, Platt GS, Simpson DI, McArdell LB, Raymond RT. 1978. Ebola haemorrhagic fever: experimental infection of monkeys. Trans R Soc Trop Med Hyg 72:188–191. [DOI] [PubMed] [Google Scholar]
- 9.Bradfute SB, Braun DR, Shamblin JD, Geisbert JB, Paragas J, Garrison A, Hensley LE, Geisbert TW. 2007. Lymphocyte death in a mouse model of Ebola virus infection. J Infect Dis 196 Suppl 2:S296–S304. [DOI] [PubMed] [Google Scholar]
- 10.Bradfute SB, Swanson PE, Smith MA, Watanabe E, McDunn JE, Hotchkiss RS, Bavari S. 2010. Mechanisms and consequences of ebolavirus-induced lymphocyte apoptosis. J Immunol 184:327–335. [DOI] [PubMed] [Google Scholar]
- 11.Brannan JM, Froude JW, Prugar LI, Bakken RR, Zak SE, Daye SP, Wilhelmsen CE, Dye JM. 2015. Interferon α/β receptor-deficient mice as a model for Ebola virus disease. J Infect Dis 212 Suppl 2:S282–S294. [DOI] [PubMed] [Google Scholar]
- 12.Bray M. 2001. The role of the type I interferon response in the resistance of mice to filovirus infection. J Gen Virol 82:1365–1373. [DOI] [PubMed] [Google Scholar]
- 13.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. 1998. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis 178:651–661. [DOI] [PubMed] [Google Scholar]
- 14.Bray M, Hatfill S, Hensley L, Huggins JW. 2001. Haematological, biochemical, and coagulation changes in mice, guinea pigs, and monkeys infected with a mouse-adapted variant of Ebola Zaire virus. J Comp Pathol 125:243–253. [DOI] [PubMed] [Google Scholar]
- 15.Bukreyev AA, Chandran K, Dolnik O, Dye JM, Ebihara H, Leroy EM, Muhlberger E, Netesov SV, Patterson JL, Paweska JT, Saphire EO, Smither SJ, Takada A, Towner JS, Volchkov VE, Warren TK, Kuhn JH. 2014. Discussions and decisions of the 2012 to 2014 International Committee on Taxonomy of Viruses (ICTV) Filoviridae Study Group, January 2012 to June 2013. Arch Virol 159:821–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caballero IS, Honko AN, Gire SK, Winnicki SM, Mele M, Gerhardinger C, Lin AE, Rinn JL, Sabeti PC, Hensley LE, Connor JH. 2016. In vivo Ebola virus infection leads to a strong innate response in circulating immune cells. BMC Genomics 17:707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carrion R, Jr, Ro Y, Hoosien K, Ticer A, Brasky K, de la Garza M, Mansfield K, Patterson JL. 2011. A small nonhuman primate model for filovirus-induced disease. Virology 420:117–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. [Internet]. 2014. Marburg hemorrhagic fever. [Cited 5 October 2016]. Available at: http://www.cdc.gov/vhf/marburg/about.html.
- 19.Cheresiz SV, Semenova EA, Chepurnov AA. 2016. Adapted lethality: what we can learn from guinea pig–adapted Ebola virus infection model. Adv Virol 2016:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chupurnov AA, Chernukhin IV, Ternovoi VA, Kudoiarova NM, Makhova NM, Azaev MSh, Smolina MP. 1995. [Attempts to develop a vaccine against Ebola fever] Vopr Virusol 40:257–260.[Article in Russian]. [PubMed] [Google Scholar]
- 21.Cross RW, Fenton KA, Geisbert JB, Mire CE, Geisbert TW. 2015. Modeling the disease course of Zaire ebolavirus infection in the outbred guinea pig. J Infect Dis 212 Suppl 2:S305–S315. [DOI] [PubMed] [Google Scholar]
- 22.Davis KJ, Anderson AO, Geisbert TW, Steele KE, Geisbert JB, Vogel P, Connolly BM, Huggins JW, Jahrling PB, Jaax NK. 1997. Pathology of experimental Ebola virus infection in African green monkeys. Involvement of fibroblastic reticular cells. Arch Pathol Lab Med 121:805–819. [PubMed] [Google Scholar]
- 23.de Wit E, Munster VJ, Metwally SA, Feldmann H. 2011. Assessment of rodents as animal models for Reston ebolavirus. J Infect Dis 204 Suppl 3:S968–S972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dudareva M, Andrews L, Gilbert SC, Bejon P, Marsh K, Mwacharo J, Kai O, Nicosia A, Hill AV. 2009. Prevalence of serum neutralizing antibodies against chimpanzee adenovirus 63 and human adenovirus 5 in Kenyan children, in the context of vaccine vector efficacy. Vaccine 27:3501–3504. [DOI] [PubMed] [Google Scholar]
- 25.Dunning J, Sahr F, Rojek A, Gannon F, Carson G, Idriss B, Massaquoi T, Gandi R, Joseph S, Osman HK, Brooks TJ, Simpson AJ, Goodfellow I, Thorne L, Arias A, Merson L, Castle L, Howell-Jones R, Pardinaz-Solis R, Hope-Gill B, Ferri M, Grove J, Kowalski M, Stepniewska K, Lang T, Whitehead J, Olliaro P, Samai M, Horby PW. 2016. Experimental treatment of Ebola virus disease with TKM-130803: a single-arm phase 2 clinical trial. PLoS Med 13:e1001997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ebihara H, Rockx B, Marzi A, Feldmann F, Haddock E, Brining D, LaCasse RA, Gardner D, Feldmann H. 2011. Host response dynamics following lethal infection of rhesus macaques with Zaire ebolavirus. J Infect Dis 204 Suppl 3:S991–S999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ebihara H, Zivcec M, Gardner D, Falzarano D, LaCasse R, Rosenke R, Long D, Haddock E, Fischer E, Kawaoka Y, Feldmann H. 2013. A Syrian golden hamster model recapitulating Ebola hemorrhagic fever. J Infect Dis 207:306–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fan Z, Li W, Lee SR, Meng Q, Shi B, Bunch TD, White KL, Kong IK, Wang Z. 2014. Efficient gene targeting in golden Syrian hamsters by the CRISPR/Cas9 system. PLoS One 9:e109755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Feldmann H, Jones S, Klenk HD, Schnittler HJ. 2003. Ebola virus: from discovery to vaccine. Nat Rev Immunol 3:677–685. [DOI] [PubMed] [Google Scholar]
- 30.Feldmann H, Sanchez A, Geisbert T. 2007. Filoviridae: Marburg and Ebola viruses, p 923–956. In: Knipe D, Howley P, editors. Field's virology. Philadelphia (PA): Lippincott, Williams, and Wilkins. [Google Scholar]
- 31.Fisher-Hoch SP, Brammer TL, Trappier SG, Hutwagner LC, Farrar BB, Ruo SL, Brown BG, Hermann LM, Perez-Oronoz GI, Goldsmith CS, Hanes MA, McCormick JB. 1992. Pathogenic potential of filoviruses: role of geographic origin of primate host and virus strain. J Infect Dis 166:753–763. [DOI] [PubMed] [Google Scholar]
- 32.Fisher-Hoch SP, McCormick JB. 1999. Experimental filovirus infections. Curr Top Microbiol Immunol 235:117–143. [DOI] [PubMed] [Google Scholar]
- 33.Food and Drug Administration. [Internet]. 2015. Product development under the animal rule: guidance for industry. [Cited 18 October 2016]. Available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM399217.pdf.
- 34.Geisbert TW, Hensley LE, Jahrling PB, Larsen T, Geisbert JB, Paragas J, Young HA, Fredeking TM, Rote WE, Vlasuk GP. 2003. Treatment of Ebola virus infection with a recombinant inhibitor of factor VIIa/tissue factor: a study in rhesus monkeys. Lancet 362:1953–1958. [DOI] [PubMed] [Google Scholar]
- 35.Geisbert TW, Jahrling PB, Larsen T, Davis KJ, Hensley LE. 2004. Filovirus pathogenesis in nonhuman primates, p 203–238. In: Klenk HD, Feldmann H, editors. Ebola and Marburg viruses: molecular and cellular biology. Norfolk (United Kingdom): Horizon Bioscience. [Google Scholar]
- 36.Geisbert TW, Lee AC, Robbins M, Geisbert JB, Honko AN, Sood V, Johnson JC, de Jong S, Tavakoli I, Judge A, Hensley LE, Maclachlan I. 2010. Postexposure protection of nonhuman primates against a lethal Ebola virus challenge with RNA interference: a proof-of-concept study. Lancet 375:1896–1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Geisbert TW, Strong JE, Feldmann H. 2015. Considerations in the use of nonhuman primate models of Ebola virus and Marburg virus infection. J Infect Dis 212 Suppl 2:S91–S97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gibb TR, Bray M, Geisbert TW, Steele KE, Kell WM, Davis KJ, Jaax NK. 2001. Pathogenesis of experimental Ebola Zaire virus infection in BALB/c mice. J Comp Pathol 125:233–242. [DOI] [PubMed] [Google Scholar]
- 39.Gilbert SC. 2015. Adenovirus-vectored Ebola vaccines. Expert Rev Vaccines 14:1347–1357. [DOI] [PubMed] [Google Scholar]
- 40.Grant-Klein RJ, Altamura LA, Badger CV, Bounds CE, Van Deusen NM, Kwilas SA, Vu HA, Warfield KL, Hooper JW, Hannaman D, Dupuy LC, Schmaljohn CS. 2015. Codon-optimized filovirus DNA vaccines delivered by intramuscular electroporation protect cynomolgus macaques from lethal Ebola and Marburg virus challenges. Hum Vaccin Immunother 11:1991–2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gumusova S, Sunbul M, Leblebicioglu H. 2015. Ebola virus disease and the veterinary perspective. Ann Clin Microbiol Antimicrob 14:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haasnoot J, de Vries W, Geutjes EJ, Prins M, de Haan P, Berkhout B. 2007. The Ebola virus VP35 protein is a suppressor of RNA silencing. PLoS Pathog 3:e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haque A, Hober D, Blondiaux J. 2015. Addressing therapeutic options for Ebola virus infection in current and future outbreaks. Antimicrob Agents Chemother 59:5892–5902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hensley LE, Stevens EL, Yan SB, Geisbert JB, Macias WL, Larsen T, Daddario-DiCaprio KM, Cassell GH, Jahrling PB, Geisbert TW. 2007. Recombinant human activated protein C for the postexposure treatment of Ebola hemorrhagic fever. J Infect Dis 196 Suppl 2:S390–S399. [DOI] [PubMed] [Google Scholar]
- 45.Herbert AS, Kuehne AI, Barth JF, Ortiz RA, Nichols DK, Zak SE, Stonier SW, Muhammad MA, Bakken RR, Prugar LI, Olinger GG, Groebner JL, Lee JS, Pratt WD, Custer M, Kamrud KI, Smith JF, Hart MK, Dye JM. 2013. Venezuelan equine encephalitis virus replicon particle vaccine protects nonhuman primates from intramuscular and aerosol challenge with ebolavirus. J Virol 87:4952–4964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hoenen T, Jung S, Herwig A, Groseth A, Becker S. 2010. Both matrix proteins of Ebola virus contribute to the regulation of viral genome replication and transcription. Virology 403:56–66. [DOI] [PubMed] [Google Scholar]
- 47.Ignatiev GM, Dadaeva AA, Luchko SV, Chepurnov AA. 2000. Immune and pathophysiological processes in baboons experimentally infected with Ebola virus adapted to guinea pigs. Immunol Lett 71:131–140. [DOI] [PubMed] [Google Scholar]
- 48.Ishikawa F, Yasukawa M, Lyons B, Yoshida S, Miyamoto T, Yoshimoto G, Watanabe T, Akashi K, Shultz LD, Harada M. 2005. Development of functional human blood and immune systems in NOD/SCID/IL2 receptor γ chainnull mice. Blood 106:1565–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jaax N, Jahrling P, Geisbert T, Geisbert J, Steele K, McKee K, Nagley D, Johnson E, Jaax G, Peters C. 1995. Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory. Lancet 346:1669–1671. [DOI] [PubMed] [Google Scholar]
- 50.Jaax NK, Davis KJ, Geisbert TJ, Vogel P, Jaax GP, Topper M, Jahrling PB. 1996. Lethal experimental infection of rhesus monkeys with Ebola–Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch Pathol Lab Med 120:140–155. [PubMed] [Google Scholar]
- 51.Jahrling PB, Geisbert TW, Geisbert JB, Swearengen JR, Bray M, Jaax NK, Huggins JW, LeDuc JW, Peters CJ. 1999. Evaluation of immune globulin and recombinant interferon α2b for treatment of experimental Ebola virus infections. J Infect Dis 179 Suppl 1:S224–S234. [DOI] [PubMed] [Google Scholar]
- 52.Johnson RF, Kurup D, Hagen KR, Fisher C, Keshwara R, Papaneri A, Perry DL, Cooper K, Jahrling PB, Wang JT, Ter Meulen J, Wirblich C, Schnell MJ. 2016. An inactivated rabies virus-based Ebola vaccine, FILORAB1, adjuvanted with glucopyranosyl lipid A in stable emulsion confers complete protection in nonhuman primate challenge models. J Infect Dis. 214 Suppl 3: S342–S354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kennedy SB, Neaton JD, Lane HC, Kieh MW, Massaquoi MB, Touchette NA, Nason MC, Follmann DA, Boley FK, Johnson MP, Larson G, Kateh FN, Nyenswah TG. 2016. Implementation of an Ebola virus disease vaccine clinical trial during the Ebola epidemic in Liberia: design, procedures, and challenges. Clin Trials 13:49–56. [DOI] [PubMed] [Google Scholar]
- 54.Krasnianskii BP, Mikhailov VV, Borisevich IV, Gradoboev VN, Evseev AA, Pshenichnov VA. 1995. [Preparation of hyperimmune horse serum against Ebola virus] Vopr Virusol 40:138–140.[Article in Russian]. [PubMed] [Google Scholar]
- 55.Kudoyarova-Zubavichene NM, Sergeyev NN, Chepurnov AA, Netesov SV. 1999. Preparation and use of hyperimmune serum for prophylaxis and therapy of Ebola virus infections. J Infect Dis 179 Suppl 1:S218–S223. [DOI] [PubMed] [Google Scholar]
- 56.Kuhn JH. 2015. Ebolavirus and Marburg virus infections.p 1323–1329. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson JL, Loscalzo J.editors. Harrison's principles of internal medicine. New York (NY): McGraw–Hill Education. [Google Scholar]
- 57.Kuhn JH, Becker S, Ebihara H, Geisbert TW, Jahrling PB, Kawaoka Y, Netesov SV, Nichol ST, Peters CJ, Volchkov VE, Ksiazek TB. 2011. Family filoviridae. p 665–671. In: King AMQ, Adams MJ, Carstens EB, Lefkowitz EJ, editors. Virus taxonomy—9th report of the International Committee on Taxonomy of Viruses. London (United Kingdom): Elsevier–Academic Press. [Google Scholar]
- 58.Langergraber KE, Prufer K, Rowney C, Boesch C, Crockford C, Fawcett K, Inoue E, Inoue-Muruyama M, Mitani JC, Muller MN, Robbins MM, Schubert G, Stoinski TS, Viola B, Watts D, Wittig RM, Wrangham RW, Zuberbuhler K, Paabo S, Vigilant L. 2012. Generation times in wild chimpanzees and gorillas suggest earlier divergence times in great ape and human evolution. Proc Natl Acad Sci USA 109:15716–15721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leenaars PP, Hendriksen CF, Angulo AF, Koedam MA, Claassen E. 1994. Evaluation of several adjuvants as alternatives to the use of Freund's adjuvant in rabbits. Vet Immunol Immunopathol 40:225–241. [DOI] [PubMed] [Google Scholar]
- 60.Leroy EM, Epelboin A, Mondonge V, Pourrut X, Gonzalez JP, Muyembe-Tamfum JJ, Formenty P. 2009. Human Ebola outbreak resulting from direct exposure to fruit bats in Luebo, Democratic Republic of Congo, 2007. Vector Borne Zoonotic Dis 9:723–728. [DOI] [PubMed] [Google Scholar]
- 61.Leroy EM, Telfer P, Kumulungui B, Yaba P, Rouquet P, Roques P, Gonzalez JP, Ksiazek TG, Rollin PE, Nerrienet E. 2004. A serological survey of Ebola virus infection in central African nonhuman primates. J Infect Dis 190:1895–1899. [DOI] [PubMed] [Google Scholar]
- 62.Lever MS, Piercy TJ, Steward JA, Eastaugh L, Smither SJ, Taylor C, Salguero FJ, Phillpotts RJ. 2012. Lethality and pathogenesis of airborne infection with filoviruses in A129 α/β−/− interferon receptor-deficient mice. J Med Microbiol 61:8–15. [DOI] [PubMed] [Google Scholar]
- 63.Lindblad-Toh K, Lander E. G10K Mammalian Community. [Internet]. 2014. Center initiated proposal: sequencing and analysis of 200 additional mammals to identify functional constraint in the human genome at roughly single base resolution. Cambridge (MA): Broad Institute of MIT and Harvard; [Cited 11 October 2016]. Available at: https://www.genome.gov/pages/research/sequencing/seqproposals/200mammals_cip_%20final.pdf. [Google Scholar]
- 64.Luchko SV, Dadaeva AA, Ustinova EN, Sizikova LP, Riabchikova EI, Sandakhchiev LS. 1995. [Experimental study of Ebola hemorrhagic fever in baboon models] Biull Eksp Biol Med 120:302–304.[Article in Russian]. [PubMed] [Google Scholar]
- 65.Ludtke A, Oestereich L, Ruibal P, Wurr S, Pallasch E, Bockholt S, Ip WH, Rieger T, Gomez-Medina S, Stocking C, Rodriguez E, Gunther S, Munoz-Fontela C. 2015. Ebola virus disease in mice with transplanted human hematopoietic stem cells. J Virol 89:4700–4704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Martini GA. 1971. Marburg virus disease, clinical syndrome. In: Martini GA, Siegert R, editors. Marburg virus disease. Berlin (GER): Springer-Verlag. [Google Scholar]
- 67.Martins K, Cooper C, Warren T, Wells J, Bell T, Raymond J, Stuthman K, Benko J, Garza N, van Tongeren S, Donnelly G, Retterer C, Dong L, Bavari S. 2015. Characterization of clinical and immunologic parameters during Ebola virus infection of rhesus macaques. Viral Immunol 28:32–41. [DOI] [PubMed] [Google Scholar]
- 68.Marzi A, Hanley PW, Haddock E, Martellaro C, Kobinger G, Feldmann H. 2016. Efficacy of vesicular stomatitis virus–Ebola virus postexposure treatment in rhesus macaques infected with Ebola virus Makona. J Infect Dis. 214 Suppl 3:S360–S366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mikhailov VV, Borisevich IV, Chernikova NK, Potryvaeva NV, Krasnianskii VP. 1994. [The evaluation in hamadryas baboons of the possibility for the specific prevention of Ebola fever] Vopr Virusol 39:82–84.[Article in Russian]. [PubMed] [Google Scholar]
- 70.Mire CE, Geisbert JB, Agans KN, Deer DJ, Fenton KA, Geisbert TW. 2016. Oral and conjunctival exposure of nonhuman primates to low doses of Ebola Makona virus. J Infect Dis.214 Suppl 3:S263–S267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Murin CD, Fusco ML, Bornholdt ZA, Qiu X, Olinger GG, Zeitlin L, Kobinger GP, Ward AB, Saphire EO. 2014. Structures of protective antibodies reveal sites of vulnerability on Ebola virus. Proc Natl Acad Sci USA 111:17182–17187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Murthy KK, Salas MT, Carey KD, Patterson JL. 2006. Baboon as a nonhuman primate model for vaccine studies. Vaccine 24:4622–4624. [DOI] [PubMed] [Google Scholar]
- 73.Nakayama E, Saijo M. 2013. Animal models for Ebola and Marburg virus infections. Front Microbiol 4:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Olinger GG, Biggins JE, Melanson VR, Wahl-Jensen V, Geisbert T, Hensley LE. 2009. Drug targets in infections with Ebola and Marburg viruses. Infect Disord Drug Targets 9:191–200. [DOI] [PubMed] [Google Scholar]
- 75.Olinger GG, Jr, Pettitt J, Kim D, Working C, Bohorov O, Bratcher B, Hiatt E, Hume SD, Johnson AK, Morton J, Pauly M, Whaley KJ, Lear CM, Biggins JE, Scully C, Hensley L, Zeitlin L. 2012. Delayed treatment of Ebola virus infection with plant-derived monoclonal antibodies provides protection in rhesus macaques. Proc Natl Acad Sci USA 109:18030–18035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Osterholm MT, Moore KA, Kelley NS, Brosseau LM, Wong G, Murphy FA, Peters CJ, LeDuc JW, Russell PK, Van Herp M, Kapetshi J, Muyembe JJ, Ilunga BK, Strong JE, Grolla A, Wolz A, Kargbo B, Kargbo DK, Sanders DA, Kobinger GP. 2015. Transmission of Ebola viruses: what we know and what we do not know. MBio 6:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Parren PW, Geisbert TW, Maruyama T, Jahrling PB, Burton DR. 2002. Pre- and postexposure prophylaxis of Ebola virus infection in an animal model by passive transfer of a neutralizing human antibody. J Virol 76:6408–6412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Patterson JL, Carrion R., Jr 2005. Demand for nonhuman primate resources in the age of biodefense. ILAR J 46:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Perry DL, Bollinger L, White GL. 2012. The baboon (Papio spp.) as a model of human Ebola virus infection. Viruses 4:2400–2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Prescott J, Feldmann H. 2016. Humanized mice—a neoteric animal disease model for Ebola virus? J Infect Dis 213:691–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.PREVAIL II Writing Group; Multinational PREVAIL II Study Team. Davey RT, Jr, Dodd L, Proschan MA, Neaton J, Neuhaus Nordwall J, Koopmeiners JS, Beigel J, Tierney J, Lane HC, Fauci AS, Massaquoi MBF, Sahr F, Malvy D. 2016. A randomized, controlled trial of ZMapp for Ebola virus fnfection. N Engl J Med 375:1448–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, Fausther-Bovendo H, Wei H, Aviles J, Hiatt E, Johnson A, Morton J, Swope K, Bohorov O, Bohorova N, Goodman C, Kim D, Pauly MH, Velasco J, Pettitt J, Olinger GG, Whaley K, Xu B, Strong JE, Zeitlin L, Kobinger GP. 2014. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 514:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rasmussen AL, Okumura A, Ferris MT, Green R, Feldmann F, Kelly SM, Scott DP, Safronetz D, Haddock E, LaCasse R, Thomas MJ, Sova P, Carter VS, Weiss JM, Miller DR, Shaw GD, Korth MJ, Heise MT, Baric RS, de Villena FP, Feldmann H, Katze MG. 2014. Host genetic diversity enables Ebola hemorrhagic fever pathogenesis and resistance. Science 346:987–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Raymond J, Bradfute S, Bray M. 2011. Filovirus infection of STAT1 knockout mice. J Infect Dis 204 Suppl 3:S986–S990. [DOI] [PubMed] [Google Scholar]
- 85.Reed DS, Lackemeyer MG, Garza NL, Sullivan LJ, Nichols DK. 2011. Aerosol exposure to Zaire ebolavirus in 3 nonhuman primate species: differences in disease course and clinical pathology. Microbes Infect 13:930–936. [DOI] [PubMed] [Google Scholar]
- 86.Report of an International Commission 1978. Ebola haemorrhagic fever in Zaire, 1976. Bull World Health Organ 56:271–293. [PMC free article] [PubMed] [Google Scholar]
- 87.Roberts A, Pardo-Manuel de Villena F, Wang W, McMillan L, Threadgill DW. 2007. The polymorphism architecture of mouse genetic resources elucidated using genome-wide resequencing data: implications for QTL discovery and systems genetics. Mamm Genome 18:473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rodríguez LL. 2002. Emergence and re-emergence of vesicular stomatitis in the United States. Virus Res 85:211–219. [DOI] [PubMed] [Google Scholar]
- 89.Ryabchikova EI, Kolesnikova LV, Luchko SV. 1999. An analysis of features of pathogenesis in 2 animal models of Ebola virus infection. J Infect Dis 179 Suppl 1:S199–S202. [DOI] [PubMed] [Google Scholar]
- 90.Ryabchikova EI, Kolesnikova LV, Netesov SV. 1999. Animal pathology of filoviral infections. Curr Top Microbiol Immunol 235:145–173. [DOI] [PubMed] [Google Scholar]
- 91.Shurtleff AC, Bavari S. 2015. Animal models for ebolavirus countermeasures discovery: what defines a useful model? Expert Opin Drug Discov 10:685–702. [DOI] [PubMed] [Google Scholar]
- 92.Smither SJ, Nelson M, Eastaugh L, Nunez A, Salguero FJ, Lever MS. 2015. Experimental respiratory infection of marmosets (Callithrix jacchus) with Ebola virus Kikwit. J Infect Dis 212 Suppl 2:S336–S345. [DOI] [PubMed] [Google Scholar]
- 93.Sullivan N, Yang ZY, Nabel GJ. 2003. Ebola virus pathogenesis: implications for vaccines and therapies. J Virol 77:9733–9737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sullivan NJ, Geisbert TW, Geisbert JB, Xu L, Yang ZY, Roederer M, Koup RA, Jahrling PB, Nabel GJ. 2003. Accelerated vaccination for Ebola virus haemorrhagic fever in nonhuman primates. Nature 424:681–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sullivan NJ, Sanchez A, Rollin PE, Yang ZY, Nabel GJ. 2000. Development of a preventive vaccine for Ebola virus infection in primates. Nature 408:605–609. [DOI] [PubMed] [Google Scholar]
- 96.Thi EP, Mire CE, Lee AC, Geisbert JB, Zhou JZ, Agans KN, Snead NM, Deer DJ, Barnard TR, Fenton KA, MacLachlan I, Geisbert TW. 2015. Lipid nanoparticle siRNA treatment of Ebola virus Makona-infected nonhuman primates. Nature 521:362–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Threadgill DW, Churchill GA. 2012. Ten years of the collaborative cross. G3 (Bethesda) 2:153–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Toth K, Lee SR, Ying B, Spencer JF, Tollefson AE, Sagartz JE, Kong IK, Wang Z, Wold WS. 2015. STAT2 knockout Syrian hamsters support enhanced replication and pathogenicity of human adenovirus, revealing an important role of type I interferon response in viral control. PLoS Pathog 11:e1005084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Volchkov VE, Volchkova VA, Chepurnov AA, Blinov VM, Dolnik O, Netesov SV, Feldmann H. 1999. Characterization of the L gene and 5‘ trailer region of Ebola virus. J Gen Virol 80:355–362. [DOI] [PubMed] [Google Scholar]
- 100.Wahl-Jensen V, Bollinger L, Safronetz D, de Kok-Mercado F, Scott DP, Ebihara H. 2012. Use of the Syrian hamster as a new model of Ebola virus disease and other viral hemorrhagic fevers. Viruses 4:3754–3784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Warfield KL, Aman MJ. 2011. Advances in virus-like particle vaccines for filoviruses. J Infect Dis 204 Suppl 3:S1053–S1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Warfield KL, Bradfute SB, Wells J, Lofts L, Cooper MT, Alves DA, Reed DK, VanTongeren SA, Mech CA, Bavari S. 2009. Development and characterization of a mouse model for Marburg hemorrhagic fever. J Virol 83:6404–6415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Warfield KL, Dye JM, Wells JB, Unfer RC, Holtsberg FW, Shulenin S, Vu H, Swenson DL, Bavari S, Aman MJ. 2015. Homologous and heterologous protection of nonhuman primates by Ebola and Sudan virus-like particles. PLoS One 10:e0118881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Warfield KL, Goetzmann JE, Biggins JE, Kasda MB, Unfer RC, Vu H, Aman MJ, Olinger GG, Jr, Walsh PD. 2014. Vaccinating captive chimpanzees to save wild chimpanzees. Proc Natl Acad Sci USA 111:8873–8876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S. 2007. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J Infect Dis 196 Suppl 2:S430–S437. [DOI] [PubMed] [Google Scholar]
- 106.Weingartl HM, Embury-Hyatt C, Nfon C, Leung A, Smith G, Kobinger G. 2012. Transmission of Ebola virus from pigs to nonhuman primates. Sci Rep 2:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Willyard C. 2014. Advances in marmoset and mouse models buoy Ebola research. Nat Med 20:1356–1357. [DOI] [PubMed] [Google Scholar]
- 108.World Health Organization. [Internet]. 2015. Ebola virus disease situation report. [Cited 10 June 2016]. Geneva, CH: World Health Organization. Available at: http://apps.who.int/iris/ bitstream/10665/208883/1/ebolasitrep_10Jun2016_eng.pdf?ua=1.