Abstract
Children with conduct problems and callous unemotional traits (CPCU) seem to show a decreased response to behavioral treatment (Hawes, Price, & Dadds, 2014). It was hypothesized that children with CPCU may respond differently to behavior therapy when the target behavior criteria are fixed a priori versus when the target behavior criteria are randomly determined post hoc. A single-case study experiment was conducted as an initial step toward investigating this hypothesis. The study was conducted using a daily report card implemented in the context of an intensive behavioral summer treatment program. Results indicated that rates of negative behaviors were higher when rewards were delivered using randomly determined levels of target behaviors as compared to using fixed levels of target behaviors. Results suggest the importance of providing children with CPCU specific and predictable treatment goals when using contingency management procedures. Additional research that examines how children with CPCU react to components of behavioral treatment may help improve their response to behavior therapy.
Keywords: Oppositional defiant disorder, conduct disorder, callous-unemotional, behavioral treatment, child
Conduct problems (CP), including oppositional defiant disorder (ODD) or conduct disorder (CD), are estimated to affect 5% to 10% of children in community settings (Canino, Polanczyk, Bauermeister, Rohde, & Frick, 2010; Lahey, Miller, Gordon, & Riley, 1999). Children with CP are at risk for a host of negative outcomes, including serious antisocial behavior in adolescence and adulthood (Loeber, Farrington, Stouthamer-Loeber, & White, 2008). Of particular concern are children with CP who also evidence an interpersonal-affective style characterized by lack of guilt following misbehavior, lack of empathy for others in distress, and low investment in their own performance -- collectively referred to as callous and unemotional (CU) traits. Two decades of research suggests that children with CP and CU (CPCU) differ from children with CP without CU (CP-only) in many important ways, including showing antisocial behavior that is especially severe and persistent (see Frick, Ray, Thornton, & Kahn, 2014 for a review). Based on this research, CU traits were introduced as a specifier of CD (under the rubric “limited prosocial emotions”) in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013).
One of the most important questions about CU traits in children is whether they provide information relevant to understanding treatment response. This has been the focus of multiple recent studies, and at least some evidence from this research suggests that children with CPCU show a less positive response to behavioral treatment (BT) than do children with CP-only (see Hawes et al., 2014; Wilkinson, Waller, & Viding, 2016 for reviews), despite the fact that BT is an empirically supported intervention for CP (Eyberg, Nelson, & Boggs, 2008). This raises an important yet unanswered question: what accounts for the worse response to BT exhibited by children with CU traits? One strong possibility is that CU traits are associated with a differential response to reward and punishments. As briefly reviewed next, and as reviewed in more detail elsewhere (Byrd, Loeber, & Pardini, 2013), several lines of evidence support this possibility.
First, a handful of behavioral treatment studies suggest that children with CPCU do not show a uniformly poor response to treatment but instead differ in response to particular aspects of BT. Specifically, there is evidence that children with CPCU show an equally positive response to rewarding aspects of BT, but show a diminished or even negative response to punishing aspects of BT (Haas et al., 2011; Hawes & Dadds, 2005; Kimonis & Armstrong, 2012). Second, neuroimaging research suggests that children with CU traits have deficits in the amygdala and noradrenergic systems, and these deficits seem to negatively impact instrumental learning by impairing the ability to form stimulus-reinforcement associations (Blair, 2013; Blair, Leibenluft, & Pine, 2014). Third, neurocognitive research suggests children with CPCU respond differently than children with CP-only on tasks designed to measure contingency learning (Barry et al., 2000; Budhani & Blair, 2005; Finger et al., 2011; Fisher & Blair, 1998; Newman & Baskin-Sommers, 2012; O'Brien & Frick, 1996). Overall, these and other studies (Byrd et al., 2013) support the hypothesis that children with CU traits are less responsive to BT because they differ in how they learn from and respond to reward and punishment.
If, as hypothesized, children with CPCU show deficiencies in how they learn from and respond to contingencies, it is important to begin a more fine-grained analysis of this fact as a step toward improving response to BT in this seriously impaired group. There are, of course, many factors that determine how children respond to contingencies and by extension how they respond to contingency-based treatments, but one that may be relevant is the predictability of the criteria used to determine success or failure of a target behavior. That is, one aspect that influences how children respond to contingencies is whether or not they are aware of the criteria they need to achieve to earn reward and avoid punishment (hereafter referred to as target behavior criteria). In behavioral treatment programs there are at least two approaches for providing children information about target behavior criteria.
In fixed criteria approaches, the target behavior and the target behavior criteria are selected and communicated to the child a priori, whereas in randomized criteria approaches the target behavior is selected and communicated to the child a priori but the target behavior criteria is determined post hoc. Consider, for example, a behavioral program for a child who frequently interrupts others. In both fixed and random criteria programs, the child would be told that his/her goal is to reduce interruptions. In a fixed criteria approach, the child would also be provided specific goals, tied to earning rewards and/or avoiding punishment, that are tied to interruptions (e.g., “if you have four or fewer interruptions, you’ll earn free time”). In a random criteria approach, the number of acceptable interruptions would be determined randomly (e.g., by drawing a number out of a bag). In both approaches, children are then given the appropriate outcome (reward if they met the criteria and lack of reward or punishment if they do not) based on the target behavior criteria. A primary difference between these two approaches to determining target behavior criteria is predictability; in fixed-criteria the target behavior criteria are predictable ahead of time and in random-criteria they are not. In behavioral treatment contexts, predictability of treatment procedures has both advantages and disadvantages. On the one hand, providing children predictable treatment goals and criteria likely maximizes motivation to achieve the stated goal. On the other hand, motivation likely drops once the target behavior criteria is achieved or if it is clear that they will not achieve the targeted goal. In fact, there is evidence to suggest that fixed versus randomly determined target behavior criteria operate in this manner when treating disruptive behavior in youth (Kelshaw-Levering, Sterling-Turner, Henry, & Skinner, 2000; McKissick, Hawkins, Lentz, Hailley, & McGuire, 2010; Theodore, Bray, Kehle, & Jenson, 2001).
Of note, there are both theoretical and empirical reasons why fixed versus randomly determined target criteria may be especially relevant to the behavioral treatment of children with CPCU. Theoretically, this distinction may be important because one of hallmarks of CU traits is lack of caring about ones one performance, which suggests that lack of motivation is a central component of CU traits. To the extent that fixed and random approaches to determining target behavior criteria differentially influence motivation, it seems possible that children with CPCU may differentially respond to the two approaches. There is also indirect empirical evidence for this possibility from a pilot study that examined the effects of systematically varying reward and punishment during behavioral treatment of children with CPCU (Miller et al., 2014). In discussing the results, the investigators noted that children with CPCU appeared to show less positive and more negative behaviors as they became more familiar with the specific procedures used in each treatment condition. One explanation for this pattern is that as the children gained experience with each treatment condition they learned how to work just hard enough to achieve reward and avoid punishment, suggesting that having predictable treatment procedures and criteria negatively impacted their motivation during treatment. If so, then children with CPCU may show a more positive response to treatment when criteria for earning rewards and avoiding punishments are determined randomly post hoc (and are thus unpredictable) rather than fixed a priori (and are thus predictable).
To our knowledge, no research has examined this issue empirically. The purpose of this study was to take a first step toward doing so using a single-subject experiment. We conducted this study in the context of an intensive, behaviorally-based summer day treatment program (STP) for children with disruptive behavior disorders. It was hypothesized that the random-criteria approach to determining target behavior criteria would produce better results than the fixed-criteria approach because of decreased motivation sometimes associated with fixed-criteria approaches. Evaluating this hypothesis is important for both scientific and clinical reasons. Scientifically, this study represents a first step away from broad-brush conclusions and toward more fine-grained understanding about effects of behavior therapy on children with CPCU. Clinically, this study may lead to optimized behavioral interventions for patients with CPCU.
Method
Participant
Juan (pseudonym) is a Caucasian male of Hispanic ethnicity who was eight years 11 months at the time of intake. Juan was adopted at age 17 months and no information is available about his development prior to that age. From adoption through the time of the evaluation he resided with his adoptive parents who were middle class and resided in a southeastern part of the U.S. His medical history was unremarkable. Juan’s parents reported that they first became concerned about his behavior when he was about two years old due to high rates of noncompliant and disruptive behavior at home and in daycare. They also reported that he had been consistently disruptive in school starting from kindergarten. Juan had a history of treatment with psychoactive medications, including Focalin XR, Intuniv, Adderall, and Vyvanse, but these were discontinued prior to his enrollment in the treatment described here. He had previously received psychosocial treatment for behavioral and emotional control problems, which his parents described as moderately effective. Juan resided with his adoptive mother and adoptive father and had no siblings. Juan had recently completed third grade at his local public elementary school.
Juan was referred for treatment by his mother due to her concerns about his disruptive behavior at home and school. Primary concerns from his mother included defiance, tantrums, verbal abuse, aggression, poor impulse control, inattention, excessive silliness, and low-frustration tolerance. Juan's mother and teacher reported that he did not seem to care about his performance (e.g., school work), did not seem concerned about feelings of others, did not keep promises that he made, and lacked remorse following misbehavior. His teachers also described him as lacking warmth and kindness. At school, Juan also struggled with inattention, hyperactivity, and poor peer relationships. Given these presenting concerns, Juan’s mother sought to enroll him in a summer treatment program (STP) conducted at a university based mental health clinic. Juan’s parents provided written consent for participation in this treatment study and Juan provided verbal assent. All procedures followed American Psychological Association standards for ethical collection and use of patient information, including disguising relevant information to hide the identity of the participating child.
Procedures
Diagnoses
Diagnoses were determined using criteria specified in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994). Following recommended guidelines for evidence-based assessment of disruptive behavior (McMahon & Frick, 2005; Pelham, Fabiano, & Massetti, 2005), diagnoses were based on both symptom and impairment criteria as evaluated using multiple sources of information. Specifically, oppositional defiant disorder (ODD), conduct disorder (CD), and attention-deficit/hyperactivity disorder (ADHD) symptoms were evaluated using parent and teacher ratings on the Disruptive Behavior Disorders Rating Scale (DBDRS; Pelham, Gnagy, Greenslade, & Milich, 1992) and using parent responses to the computerized version of the Diagnostic Interview Schedule for Children for DSM-IV (NIMH-DISC Editorial Board, 1999). Impairment was evaluated using parent and teacher ratings on the Impairment Rating Scale (IRS; Fabiano et al., 2006). These data (see Table 1) were independently reviewed by two Ph.D. level clinicians who each assigned Juan diagnoses of ADHD and ODD.
Table 1.
Summary of ADHD, ODD, CD, impairment, and callous-unemotional traits as measured during the intake assessment
| Measure | Mother | Teacher |
|---|---|---|
| # of Symptoms Endorseda | ||
| ADHD-hyperactive/impulsive | 8 | 8 |
| ADHD-inattentive | 8 | 3 |
| Oppositional Defiant Disorder | 6 | 8 |
| Conduct Disorder Symptoms | 2 | 0 |
| Impairmentb | ||
| Peer relationships | 6 | 6 |
| Adult-child relationships | 6 | 3 |
| Overall adjustment | 6 | 6 |
| Callous Unemotional Traits | ||
| APSD CU-tscorec | 79 | 67 |
| ICU total scored | 37 | 31 |
Notes:
= Number of symptoms endorsed on the Disruptive Behavior Disorder Rating Scale (Pelham et al., 1992)
= Impairment Rating Scale scores (Fabiano et al., 2006), which range from 0 (no impairment) to 6 (serious impairment).
= Callous-Unemotional subscale t-scores from the Antisocial Process Screening Device (Frick & Hare, 2001)
= total raw score from the Inventory of Callous-Unemotional Traits (Frick, 2004), which range from 0 to 72.
The diagnostic evaluation also included an assessment of internalizing disorders. Anxiety, as measured by the Revised Children’s Manifest Anxiety Scale 2nd edition (Reynolds & Richmond, 2008), was in the normative range with a total anxiety T-score of 44. Depression, as measured by the Children’s Depression Inventory 2nd edition (Kovacs, 2011), was also in the normative range with a total depression T-score of 44.
Callous-Unemotional Traits
CU traits were evaluated using two measures: the Antisocial Process Screening Device (APSD; Frick & Hare, 2001) and the Inventory of Callous-Unemotional Traits (ICU; Frick, 2004). As shown on Table 1, Juan’s scores on these measures indicated very high levels of CU traits. His scores on the APSD place him in the top 1% (mother) to 5% (teacher) compared to other boys his same age. Likewise his scores on the ICU are substantially above recently proposed cutoffs on this measure (Kimonis, Fanti, & Singh, 2014).
Method
Treatment overview
Treatment was implemented in an STP, which is an evidenced based treatment program for youth with disruptive behavior problems that is delivered in the context of a summer camp setting (Pelham et al., 2010). The STP occurred five days a week (Monday through Friday) from 8:00 AM to 5:00PM for eight weeks. Juan was placed in a group with 17 other children ranging from six to twelve years of age, comprised of both boys (n=15) and girls (n=2). He attended 39 out of 39 days of the intervention (there was no treatment on the fourth of July).
The primary approach to treatment was behavior management with a focus on positive reinforcement, effective commands, and immediate consequences. Using token reinforcement and response cost methods, Juan received points for appropriate behavior and lost points for inappropriate behavior as he engaged in activities throughout the day. Of most relevance to this study is that treatment also included use of a daily report card (DRC). Three behavioral targets were included on Juan’s DRC: (1) interruptions, (2) rule violations during classroom activities, and (3) teasing peers. These goals were selected based on observations of his behavior during the first week of treatment, discussions with his parents, and inspecting information (ratings and written reports) from his classroom teacher in his regular school setting. Juan’s goals on his DRC did not change during treatment, but the criteria that defined success on the goals varied from week to week as described below. The DRC was always backed by a reward system that consisted of the chance to earn free time at noon and again at the end of the day, along with home-based rewards delivered by his parents, which consisted of access to screen time (TV, computer, video games). This reward was determined through discussion with Juan, his parents, his lead counselor, and the clinical supervisor. Delivery of home rewards was encouraged by informing Juan and his parents at the end of each day whether Juan earned his reward and if so reminding parents to deliver the reward to Juan. The DRC was also one part of determining whether Juan earned a weekly reward; to participate in a fun field trip on Friday, Juan was required to have achieved at least 75% of his treatment goals on the majority of days in a given week.
The majority of each day consisted of recreationally-based therapeutic group activities (i.e., basketball, soccer, baseball or kickball), an art period, lunch, and swimming. These were led by paraprofessional counselors that included one graduate student lead counselor and five undergraduate counselors. Behavioral treatment was delivered during these activities by using a token economy system and cognitive-emotional treatment was delivered between activities by using discussion, role playing, and problem solving. The remainder of each day (two hours) was spent in a classroom setting that was run by a teacher and teacher aide. Children completed individual seatwork (reading, math, writing) that was appropriate for their academic ability, followed by peer tutoring activities to foster reading skills. The behavior management used in the classroom was a response-cost system in that children began class with a set number of points and points were taken for each violation of a classroom rule, which included: be respectful of others, obey adults, work quietly, use materials and possessions appropriately, remain in your assigned seat or area, raise hand to speak or to ask for help, and stay on task. All activities were supervised by Ph.D. level clinicians.
Target behavior manipulation
The treatment manipulation of interest was whether Juan reacted differentially to fixed versus randomly determined target behavior criteria on his behavioral goals on his DRC. That is, Juan always had the same three goals on his DRC, but the criteria used to determine whether he was successful in achieving the goal (i.e., his target behavior criteria) were decided in different ways -- either fixed ahead of time or randomly determined after the fact. For example, reducing interruptions was always a goal on his DRC, but the number of interruptions he was allowed display and still achieve a reward for reducing interruptions goal was either fixed or random, with condition varying across weeks of treatment.
During the fixed-criteria weeks (weeks 2, 5, and 6), the target behavior criteria were determined a priori by his counselors who examined his past behavior and selected a number that represented about 20% improvement. This was done at the start the week and target behavior criteria remained constant throughout the week. Behavioral goals on his DRC, including the fixed criterion for achieving success at each goal, were reviewed with Juan at the start of each day (e.g., “you need to have four or fewer interruptions to meet your interruptions goal this morning”). If he met his criterion goal, a “yes” would be circled on his DRC. Throughout the day, Juan was prompted by staff to keep track of his behavior in relation to his criterion goals (e.g., “you have two interruptions and you can’t have more than four to make recess”). Juan was assigned a counselor who reviewed his DRC target behaviors and criterion goals each morning and after each reward period.
During the random-criteria weeks (weeks 3, 4, 7, and 8) the target behavior criteria were determined randomly and post hoc. Specifically, Juan was told that the number of behaviors on his DRC that he was allowed to display and still earn his reward was going to be a mystery that would be revealed just before the reward period. Behavioral goals were reviewed with Juan at the start of and throughout each day (“you need to work on reducing your interruptions today”) but no specific target behavior criteria were provided. Instead, just before the reward activity that reinforced the DRC, Juan chose a number out of a bag and this number became the target behavior criterion for earning his reward. The range of possible criterion goals (i.e., the numbers placed in the bag to draw from) were based on Juan’s behavior during the baseline week (i.e., first week of treatment) and ranged from one to 30.
The effect of fixed versus random criteria on the DRC was examined using an alternating treatments design in which the two treatment conditions were presented in an alternating manner. The first week of treatment was used to establish baseline rates of behavior without a DRC in place. The DRC was introduced the second week of treatment, with order of fixed versus random criteria determined by chance. Target behavior criteria procedures were changed weekly rather than daily to maximize Juan’s ability to discriminate the treatment conditions, thereby reducing carryover effects, and order of treatment was determined randomly to reduce sequential confounding (Barlow, Nock, & Hersen, 2009; Levin, Ferron, & Kratochwill, 2012).
Analytic Plan
Following recommendations, data were examined three ways (Barlow et al., 2009). First, data were examined visually to illustrate overall trends in the different treatment conditions. Second, alternation randomization tests were computed (Houle, 2009). This was done by comparing the observed mean difference between the treatment conditions to mean differences randomly generated from the data. Specifically, a difference score was computed for all 35 possible combinations of weeks (e.g., average of weeks 2, 3 and 4 minus average of weeks 5, 6, 7, and 8; average of weeks 2, 3 and 5 minus average of weeks 4, 6, 7, and 8; etc.), including the actual randomization used in the study (i.e., the observed treatment difference). The proportion of the 34 randomly generated mean differences that exceed the one observed treatment difference are reported. Third, three within-subject standardized mean difference effect sizes were computed: (a) fixed-criteria versus baseline; (b) random-criteria versus baseline; and (c) random criteria versus fixed criteria. Effect sizes were computed by subtracting the two conditions and dividing the result by the standard deviation averaged over all conditions.
Results
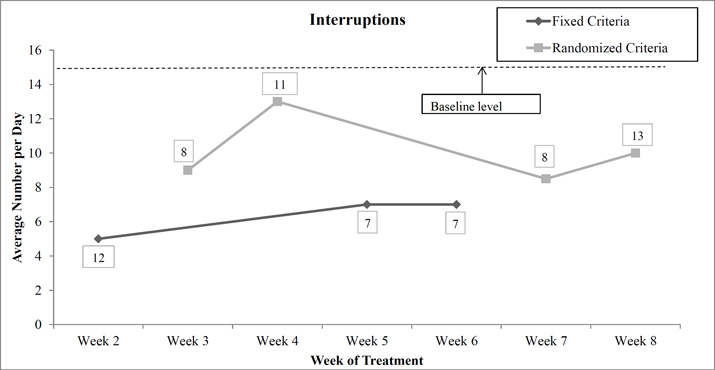
Interruption
As shown in Figure 1, Juan’s rate of interruption was higher in the baseline condition than in either DRC condition: (Effect sizes: fixed-criteria minus baseline = 1.60; random-criteria minus baseline = 0.90). Interruptions were also higher in the random-criteria condition than in the fixed-criteria condition (effect size = 0.70). The observed difference between the fixed and random condition means was greater than 100% of the 34 randomly generated mean differences.
Figure 1.
Interruptions over week of treatment as a function of fixed-criteria versus random-criteria on the daily report card. The baseline (week 1) level of interruptions before implementing a daily report card is shown by the dotted line. The number above or below each data point is the criterion used to define success, with success numbers during the Fixed Criteria weeks determined by counselors and held constant within each week and success numbers during the Randomized Criteria weeks determined by daily lottery and reported as within-week rounded averages.
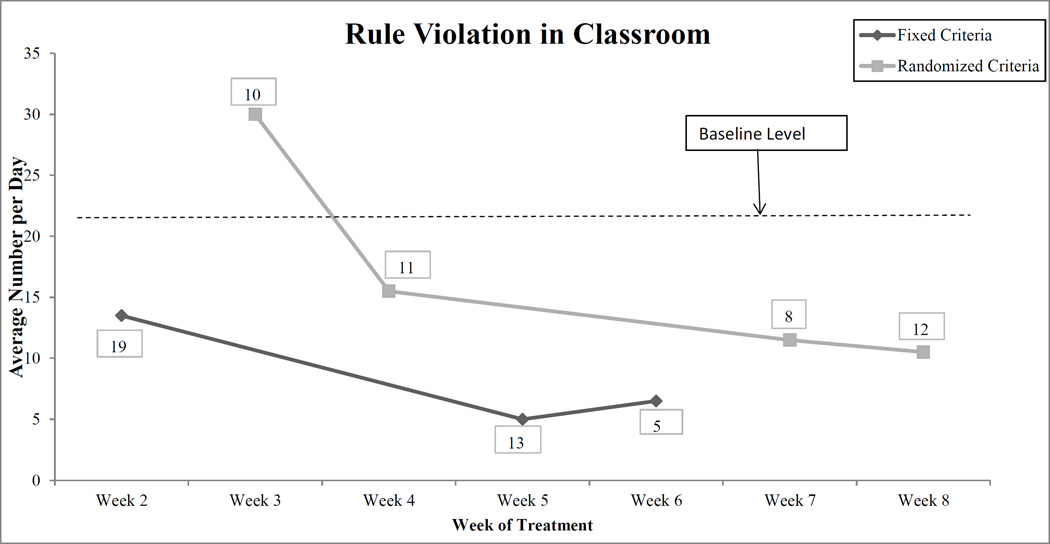
Rule Violations during Classroom
As shown in Figure 2, Juan’s rate of rule violations was higher in the baseline condition than in either DRC condition (Effect sizes: fixed criteria minus baseline = 2.40; random-criteria minus baseline = 0.90). Rule violations were also higher in the random-criteria condition than in the fixed-criteria condition (effect size = 1.50). The observed difference between the fixed and random condition means was greater than 94% (32 out of 34) of the randomly generated mean differences.
Figure 2.
Rule violations in the classroom over week of treatment as a function of fixed-criteria versus random-criteria on the daily report card. The baseline (week 1) level of rule violations before implementing a daily report card is shown by the dotted line. The number above or below each data point is the criterion used to define success, with success numbers during the Fixed Criteria weeks determined by counselors and held constant within each week and success numbers during the Randomized Criteria weeks determined by daily lottery and reported as within-week rounded averages.
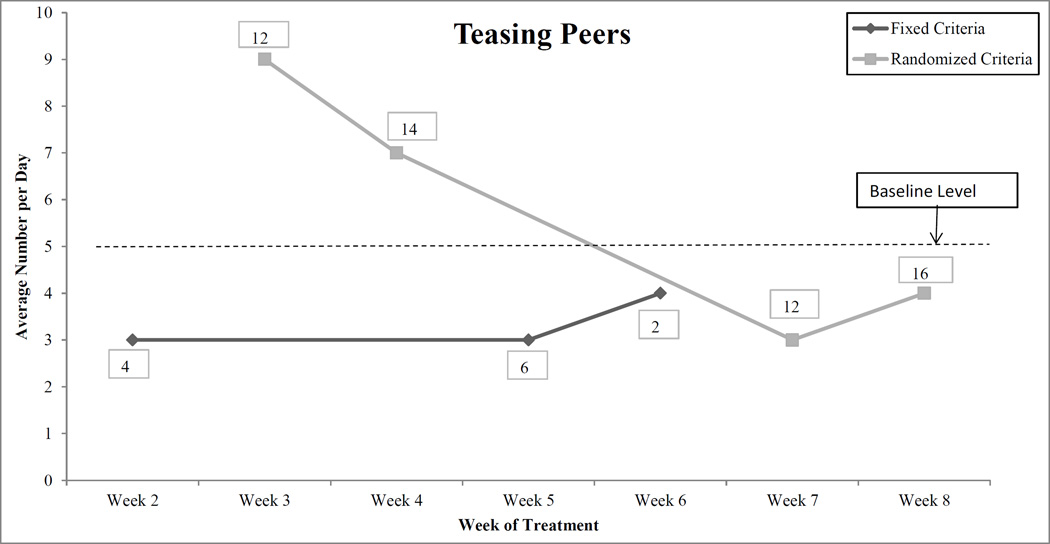
Teasing
As shown in Figure 3, Juan’s rate of teasing peers was somewhat higher in the baseline condition than in the fixed-criteria condition (effect size = 0.40). The baseline and random-criteria conditions did not differ overall (effect size = −0.05), but there is an apparent trend that suggests improvement over treatment in the random-criteria condition. Teasing was modestly lower in the fixed-criteria condition than in the random-criteria condition (effect size = 0.45). The observed difference between the fixed and random condition means was greater than 82% (28 out of 34) of the randomly generated mean differences.
Figure 3.
Teasing peers over week of treatment as a function of fixed-criteria versus random-criteria on the daily report card. The baseline (week 1) level of teasing before implementing a daily report card is shown by the dotted line. The number above or below each data point is the criterion used to define success, with success numbers during the Fixed Criteria weeks determined by counselors and held constant within each week and success numbers during the Randomized Criteria weeks determined by daily lottery and reported as within-week rounded averages.
Discussion
Behavior therapy (BT) has long been shown to be effective for the treatment of conduct problems in children (Eyberg et al., 2008). However, some evidence suggests that children with CPCU may show a less positive response to BT (Haas et al., 2011; Hawes et al., 2014; Waschbusch, Carrey, Willoughby, King, & Andrade, 2007), consistent with suggestions that this group of children may show an atypical response to contingencies (Blair, 2010; Dadds & Salmon, 2003). A key task is to begin unraveling the specific aspects of contingency response that account for this pattern, and researchers using experimental tasks have made significant progress in this area (e.g., Budhani & Blair, 2005). At the same time, almost no research has examined this topic in clinical contexts. This case study was a first step toward advancing this goal by examining whether knowledge of the criteria used to evaluate a behavioral goal has a significant impact on a child with CPCU. This aspect of contingency response was selected because previous theory and research suggests that providing specific behavioral goals to children with conduct problems can sometimes produce unwanted effects, such as working only has hard as needed to accomplish the goal and giving up when it is clear that the goal will not be accomplished (Kelshaw-Levering et al., 2000; Newman & Baskin-Sommers, 2012; Theodore et al., 2001). Of note, a pilot behavioral treatment study provided anecdotal evidence that this pattern may be apparent in children with CPCU (Miller et al., 2014).
Several interesting results emerged from this single subject experiment. At the most basic level, the results add to many others (e.g., Fabiano et al., 2010; Jurbergs & Kelley, 2008) in suggesting that DRCs are effective at reducing disruptive behavior in children. This is noteworthy because DRCs are relatively easy to implement, cost little, and in the present study apparently produced reductions in disruptive behavior (at least those that were measured) even after accounting for other behavioral interventions. The fact that this child, who had very high CU traits as well as significant conduct problems, responded well to this intervention suggests DRCs may be equally effective when treating children with CPCU as it is when used to treat children with CP in general.
More central to the focus of the study, the results showed that using the fixed-criteria approach for determining receipt of reward produced better behavioral performance than did the random-criteria approach. This finding was contrary to our hypothesis but is apparent from the data. Averaging across treatment conditions shows that Juan’s interruptions (see Figure 1), rule violations in the classroom (see Figure 2), and teasing (see Figure 3) were each lower when fixed-criteria were used than when random-criteria were used. Furthermore, the pattern of behavior across the figures is relatively consistent in showing large increases in negative behavior when going from fixed-criteria to random-criteria (i.e., week 2 to 3), followed by decreases when fixed criteria are re-introduced (week 4 to 5), and subsequent increases (for interruption and rule violations) when random-criteria are used again (weeks 6 to 7). Together these observations make a fairly compelling case that the fixed-criteria procedure resulted in less disruptive behavior than did the random-criteria procedure.
What might account for the increased effectiveness of fixed versus random criteria? Though speculative, predictability is one possible explanation. Experimental research demonstrates that children with CPCU respond similarly to children with CP-only when the association between behavior and response is clear, but differences emerge when this association becomes more ambiguous (Budhani & Blair, 2005). In the present study, the association between behavior and outcome was arguably clearer and less ambiguous -- that is, more predictable -- in the fixed-criteria condition than in the random-criteria condition because the same rate of behavior produced consistent outcomes in the fixed-criteria condition but could produce different outcomes in the random-criteria condition. For example, as shown in Figure 1, if Juan interrupted 10 times he would never have earned his reward in the fixed-criteria conditions, but 10 interruptions during the random-criteria conditions would have resulted in mixed outcomes (rewards some days but not others) depending on the criteria lottery at the end of the activity (i.e., if he randomly selected 10 or higher, he was rewarded, but if he randomly selected 9 or lower he was not rewarded). The results of this case study are thus consistent with results from experimental research in suggesting the importance of predictability in treating children with CPCU.
Related to this point, it is interesting to interpret these findings in light of evidence that inconsistent parenting is associated with later CPCU in children (McDonald, Dodson, Rosenfield, & Jouriles, 2011) and that children with CPCU seem to evoke inconsistent parenting (Hawes, Dadds, Frost, & Hasking, 2011). Experiencing inconsistent parenting may teach children with CPCU to place less value and trust in behavioral systems with unpredictable or unreliable contingencies and more value in trust in behavioral systems that are predictable and reliable. Given that the fixed criteria condition used more predictable contingency procedures than the random criteria condition, the relatively better response Juan showed in response to fixed versus random procedures may be associated with having experienced inconsistent parenting. This is a particularly interesting explanation in Juan’s case because he was adopted at 17 months old and may very well have experienced inconsistent caregiving as a result of or before his adoption.
These findings should be considered within the context of some limitations. First, the random-criteria procedure made it possible for Juan to randomly select high criterion goals. Our range of criterion goals were calculated by increasing Juan’s highest daily instance of negative behavior during the baseline phase (week one), by 25%, resulting in criterion goals that ranged from zero to 30. This data-driven procedure seems scientifically justified, but it limited the ecological validity of the manipulation by allowing Juan to randomly select criteria that were well-above what is typically considered acceptable behavior. Additionally, such high criterion goals meant that Juan was at times able to earn his reward despite demonstrating quite negative behavior. These observations suggest the random-criteria condition may have been strengthened by limiting the upper range of possible criterion goals thereby ensuring that the stringency of the random-criteria condition matched that of the fixed-criteria condition. We recommend that clinicians or researchers seeking to use the random criteria approach take this into account when developing an intervention strategy. Second, the treatment manipulations used with Juan were delivered in the context of group-based recreation therapy for children with disruptive and/or inattentive problems. Juan’s treatment response was likely influenced by the other children in his treatment, as well as the counselors who delivered the treatment. These influences cannot be disentangled from the effects of the DRC manipulations. Third, the DRC was not the only treatment used with Juan; as described, several other treatments were simultaneously in place while conducting this study. However, it should be noted that other treatments were held constant during the treatment, as were the peers and counselors who worked with Juan, suggesting they were not likely to account for the different pattern of findings that fixed versus random criteria seemed to produce. Fourth, Juan met criteria not only for CP and CU but also ADHD. This is to be expected because the majority of children with CP also meet criteria for ADHD, especially in treatment seeking samples (Waschbusch, 2002), However, because children with both CP and ADHD differ in some important ways from children with CP alone (Waschbusch, 2002) the results of this study may not generalize to children with CPCU who do not also have ADHD. Finally, the effects of time cannot be entirely eliminated. We attempted to reduce the influence of time by randomly assigning order of treatment manipulation to different treatment weeks, but it is nonetheless possible that time could influence the findings.
Practical Suggestions for Researchers
The results of this study suggest several additional lines of research. First, as apparent from the figures, there was considerable heterogeneity across the course of treatment for all outcomes. Statistically sophisticated yet easy to use methods for understanding this heterogeneity are sorely needed, and there are promising recent developments toward this goal (Ridenour, Pineo, Maldonado Molina, & Hassmiller Lich, 2013; Ridenour, Wittenborn, Raiff, Benedict, & Kane-Gill, 2016). Second, it would be interesting to extend the methods used in this study to examine whether children with CPCU differentially respond to fixed versus random punishment. It has been noted that the scientific examination of punishment procedures (also referred to as aversive control) has been seriously neglected in recent decades, despite the fact that punishment is a “partner of positive reinforcement”, is a prominent component of learning in the natural world, and when used judiciously has been shown to be an effective component of treating disruptive behavior in children (Critchfield & Rasmussen, 2007). Importantly, deterrence theory and research suggests that punishments are most effective when they are mild but consistent (Kleiman, 2010; Rosen, 2010), yet parents of children with CP often do the opposite -- ignore their child’s conduct problems until they get fed up, at which point they dole out a serious punisher, thereby delivering severe punishment unpredictably (Patterson, 1982). Given hypothesized and observed differences in how children with and without CU respond to punishment during treatment (Haas et al., 2011; Hawes & Dadds, 2005), it would be interesting to test whether predictable punishment (fixed) versus unpredictable punishment (random) differentially impacts CP children with and without CU traits. Third, the majority of research demonstrating that children with CPCU have differential response to reward and punishment has been conducted in controlled experimental settings. Much more work is needed translating these findings into clinical interventions and testing whether these translated interventions are effective. Conversely, additional controlled experimental research is needed to better understand how children with CPCU respond to reward and punishment. For example, most studies to date have operationalized punishment as the removal of a positive stimulus (e.g., loss of points which are in turn associated with toys, candy, or privileges). Relatively little research has operationalized punishment as the addition of an aversive. These two types of punishment can have different effects (Pear, 2001). It remains largely unknown how these different types of punishment effect children with CPCU differ relative to other children. Finally, at a broad level the results argue that future research on treatment response in children with CPCU would benefit from greater specificity. Paraphrasing Paul’s classic work on psychotherapy research (Paul, 1967), it is time to move beyond simple questions of whether children with CPCU respond to behavioral treatment and instead ask what specific aspects of BT are effective for which specific aspects of CPCU and under what conditions?
Practical Suggestions for Clinicians
The results of this single subject experiment also provide practical suggestions for clinicians. First, clinicians should establish clear and specific treatment goals for children with CPCU at the outset of behavior therapy rather than determining goal levels after treatment has begun. Concerns that children with CPCU may show low effort in response to knowing specific behavioral targets did not emerge in this study as judged by the more positive and less negative behavior in the fixed rather than random condition. Second, the results highlight the value to clinicians of using single-subject methods for understanding children in their care and for maximizing treatment response. Absent valid methods for accurately identifying and predicting which children will respond to which components of behavior therapy, clinicians should systematically manipulate the order and nature of treatment components, collect data to evaluate the impact of these manipulations, and use these data to make evidence-based decisions about treatment. A Daily Report Card incorporates many of these single-case methods (Jurbergs & Kelley, 2008) and research has demonstrated that it is a simple yet effective tool for treating disruptive behavior in children (Fabiano et al., 2010). Third, simple behavioral strategies may be preferred over complex strategies if simplifying results in greater consistency of implementation. Behavioral strategies, such as contingency management programs, are likely to be implemented by parents and teachers who have high demands on their time and attention and are thus likely to deliver contingencies in a somewhat variable or unpredictable manner. More unpredictable delivery of consequences is arguably more akin to the random rather than the fixed procedure used in this study, and it was the random procedure that produced less positive results. If so, then simpler behavioral strategies that increase consistency and predictability may be especially important when treating children with CPCU, even if the simplicity comes at a cost. For example, it may be more effective to limit the number of behaviors targeted or to reduce rates of reinforcement when treating children with CPCU if doing so increases the predictability of how contingencies and consequences are implemented. Given that these clinical suggestions are based on a single case study they should be viewed with caution. Even so, the results are promising and suggest that additional research investigating this topic with larger samples of children holds some potential to improve treatment of children with CPCU.
Acknowledgments
We thank the research assistants, clinical staff and participating family who made this study possible.
Funding
This study was partly supported by a grant from the National Institute of Mental Health (7R34MH085796) awarded to the first author.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- Barlow DH, Nock MK, Hersen M. Single case experimental designs: Strategies for studying behavior change. New York: Pearson Education Inc; 2009. [Google Scholar]
- Barry CT, Frick PJ, DeShazo TM, McCoy M, Ellis M, Loney BR. The importance of callous-unemotional traits for extending the concept of psychopathy to children. Journal of Abnormal Psychology. 2000;109(2):335–340. doi: 10.1037/0021-843X.109.2.335. [DOI] [PubMed] [Google Scholar]
- Blair RJR. A cognitive-neuroscience perspective on child and adolescent psychopathy. In: Salekin RT, Lynam DT, editors. Handbook of child and adolescent psychopathy. New York: Guilford Press; 2010. pp. 156–178. [Google Scholar]
- Blair RJR. The neurobiology of psychopathic traits in youths. Nature Reviews: Neuroscience. 2013;14(11):786–799. doi: 10.1038/nrn3577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair RJR, Leibenluft E, Pine DS. Conduct disorder and callous-unemotional traits in youth. New England Journal of Medicine. 2014;371(23):2207–2216. doi: 10.1056/NEJMra1315612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budhani S, Blair RJR. Response reversal and children with psychopathic tendencies: Success is a function of salience of contingency change. Journal of Child Psychology and Psychiatry. 2005;46(9):972–981. doi: 10.1111/j.1469-7610.2004.00398.x. [DOI] [PubMed] [Google Scholar]
- Byrd AL, Loeber R, Pardini DA. Antisocial behavior, psychopathic features and abnormalities in reward and punishment processing in youth. Clinical Child and Family Psychology Review. 2013;17(2):125–156. doi: 10.1007/s10567-013-0159-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G, Polanczyk G, Bauermeister JJ, Rohde LA, Frick PJ. Does the prevalence of CD and ODD vary across cultures? Social Psychiatry and Psychiatric Epidemiology. 2010;45(7):695–704. doi: 10.1007/s00127-010-0242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Critchfield TS, Rasmussen ER. It's aversive to have an incomplete science of behavior. Mexican Journal of Behavior Analysis. 2007;33(special issue):1–6. [Google Scholar]
- Dadds MR, Salmon K. Punishment insensitivity and parenting: Temperament and learning as interacting risks for antisocial behavior. Clinical Child and Family Psychology Review. 2003;6(2):69–86. doi: 10.1023/a:1023762009877. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Pelham WE, Waschbusch DA, Gnagy EM, Lahey BB, Chronis AM, Burrows-MacLean L. A practical impairment measure: Psychometric properties of the Impairment Rating Scale in samples of children with attention-deficit/hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology. 2006;35(3):369–385. doi: 10.1207/s15374424jccp3503_3. [DOI] [PubMed] [Google Scholar]
- Fabiano GA, Vujnovic R, Pelham WE, Waschbusch DA, Massetti GM, Pariseau ME, Volker M. Enhancing the effectiveness of special education programming for children with Attention-Deficit/Hyperactivity Disorder using a daily report card. School Psychology Review. 2010;39(2):219–239. [Google Scholar]
- Finger EC, Marsh AA, Blair KS, Reid ME, Sims C, Ng P, Blair RJR. Disrupted reinforcement signaling in the orbitofrontal cortex and caudate in youths with conduct disorder or oppositional defiant disorder and a high level of psychopathic traits. American Journal of Psychiatry. 2011;168(2):152–162. doi: 10.1176/appi.ajp.2010.10010129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher L, Blair RJR. Cognitive impairment and its relationship to psychopathic tendencies in children with emotional and behavioral difficulties. Journal of Abnormal Child Psychology. 1998;26(6):511–519. doi: 10.1023/a:1022655919743. [DOI] [PubMed] [Google Scholar]
- Frick PJ. Inventory of Callous-Unemotional Traits. 2004 Retrieved from http://labs.uno.edu/developmental-psychopathology/ICU.html. [Google Scholar]
- Frick PJ, Hare RD. Antisocial Processes Screening Device: Technical manual. Toronto: Multi-Health Systems; 2001. [Google Scholar]
- Frick PJ, Ray JV, Thornton LC, Kahn RE. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychological Bulletin. 2014;140(1):1–57. doi: 10.1037/a0033076. [DOI] [PubMed] [Google Scholar]
- Haas SM, Waschbusch DA, Pelham WE, King S, Andrade BF, Carrey NJ. Treatment response in CP/ADHD children with callous/unemotional traits. Journal of Abnormal Child Psychology. 2011;39(4):541–552. doi: 10.1007/s10802-010-9480-4. [DOI] [PubMed] [Google Scholar]
- Hawes DJ, Dadds MR. The treatment of conduct problems in children with callous-unemotional traits. Journal of Consulting and Clinical Psychology. 2005;73(4):737–741. doi: 10.1037/0022-006X.73.4.737. [DOI] [PubMed] [Google Scholar]
- Hawes DJ, Dadds MR, Frost ADJ, Hasking PA. Do childhood callous-unemotional traits drive change in parenting practices? Journal of Clinical Child and Adolescent Psychology. 2011;40(4):507–518. doi: 10.1080/15374416.2011.581624. [DOI] [PubMed] [Google Scholar]
- Hawes DJ, Price MJ, Dadds MR. Callous-unemotional traits and the treatment of conduct problems in childhood and adolescence: A comprehensive review. Clinical Child and Family Psychology Review. 2014 doi: 10.1007/s10567-014-0167-1. [DOI] [PubMed] [Google Scholar]
- Houle TT. Statistical analysis for single-case experimental designs. In: Barlow DH, Nock MK, Hersen M, editors. Single case experimental designs: Strategies for studying behavior change. New York: Pearson Education Inc; 2009. pp. 271–305. [Google Scholar]
- Jurbergs N, Kelley ML. Daily report cards. In: McBurnett K, Pfiffner LJ, editors. Attention-Deficit/Hyperactivity Disorder: Concepts, controversies, new directions. New York: Informa Healthcare; 2008. pp. 161–168. [Google Scholar]
- Kelshaw-Levering K, Sterling-Turner HE, Henry JR, Skinner CH. Randomized interdependent group contingencies: Group reinforcement with a twist. Psychology in the Schools. 2000;37(6):523–533. doi: [Google Scholar]
- Kimonis ER, Armstrong K. Adapting Parent Child Interaction Therapy to treat severe conduct problems with callous-unemotional traits: A case study. Clinical Case Studies. 2012;11(3):234–252. [Google Scholar]
- Kimonis ER, Fanti KA, Singh JP. Establishing cut-off scores for the Parent-Reported Inventory of Callous-Unemotional Traits. Archives of Forensic Psychology. 2014;1(1):27–48. [Google Scholar]
- Kleiman MAR. The outpatient prison: How to lower both the prison population and crime - at the same time. The American Interest. 2010;5(3) Retrieved from http://www.the-american-interest.com/2010/03/01/the-outpatient-prison/ [Google Scholar]
- Kovacs M. Children's Depression Inventory. 2nd. New York: Multi-Health Systems; 2011. [Google Scholar]
- Lahey BB, Miller TI, Gordon RA, Riley AW. Developmental epidemiology of the disruptive behavior disorders. In: Quay HC, Hogan AE, editors. Handbook of disruptive behavior disorders. New York: Kluwer Academic / Plenum Publishers; 1999. pp. 23–48. [Google Scholar]
- Levin JR, Ferron JM, Kratochwill TR. Nonparametric statistical tests for single-case systematic and randomized ABAB…AB and alternating treatment intervention designs: new developments, new directions. Journal of School Psychology. 2012;50(5):599–624. doi: 10.1016/j.jsp.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, White HR. Violence and serious theft: Development and prediction from childhood to adulthood. NY: Routledge; 2008. [Google Scholar]
- McDonald R, Dodson MC, Rosenfield D, Jouriles EN. Effects of a parenting intervention on features of psychopathy in children. Journal of Abnormal Child Psychology. 2011;39(7):1013–1023. doi: 10.1007/s10802-011-9512-8. [DOI] [PubMed] [Google Scholar]
- McKissick C, Hawkins RO, Lentz FE, Hailley J, McGuire S. Randomizing multiple contingency components to decrease disruptive behaviors and increase student engagement in an urban second-grade classroom. Psychology in the Schools. 2010;47(9):944–959. [Google Scholar]
- McMahon RJ, Frick PJ. Evidence-based assessment of conduct problems in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):477–505. doi: 10.1207/s15374424jccp3403_6. [DOI] [PubMed] [Google Scholar]
- Miller NV, Haas SM, Waschbusch DA, Willoughby MT, Helseth SA, Crum KI, Pelham WE. Behavior therapy and callous-unemotional traits: Effects of a pilot study examining modified behavioral contingencies on child behavior. Behavior Therapy. 2014;45(5):606–618. doi: 10.1016/j.beth.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman JP, Baskin-Sommers AR. Early selective attention abnormalities in psychopathy: Implications for self-regulation. In: Posner MI, editor. Cognitive neuroscience of attention. 2nd. New York, NY: Guilford Press; 2012. pp. 421–440. [Google Scholar]
- NIMH-DISC Editorial Board. The National Institute of Mental Health Diagnostic Interview Schedule for Children. New York: Columbia University; 1999. [Google Scholar]
- O'Brien BS, Frick PJ. Reward dominance: Associations with anxiety, conduct problems, and psychopathy in children. Journal of Abnormal Child Psychology. 1996;24(2):223–240. doi: 10.1007/BF01441486. [DOI] [PubMed] [Google Scholar]
- Patterson GR. Coercive family process. Eugene, OR: Castalia; 1982. [Google Scholar]
- Paul GL. Strategy of outcome research in psychotherapy. Journal of Consulting Psychology. 1967;31(2):109–118. doi: 10.1037/h0024436. [DOI] [PubMed] [Google Scholar]
- Pear J. The science of learning. New York: Psychology Press; 2001. [Google Scholar]
- Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment for Attention Deficit Hyperactivity Disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(3):449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(2):210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greiner AR, Waschbusch DA, Fabiano GA, Burrows-MacLean L. Summer treatment programs for Attention-Deficit/Hyperactivity Disorder. In: Weisz JR, Kazdin AE, editors. Evidence-based psychotherapies for children and adolescents. 2nd. New York: Guilford Press; 2010. pp. 277–292. [Google Scholar]
- Reynolds CR, Richmond BO. What I Think and Feel (RCMAS-2) Los Angeles, CA: Western Psychological Services; 2008. [Google Scholar]
- Ridenour TA, Pineo TZ, Maldonado Molina MM, Hassmiller Lich K. Toward rigorous idiographic research in prevention science: Comparison between three analytic strategies for testing preventive intervention in very small samples. Prev Sci. 2013;14(3):267–278. doi: 10.1007/s11121-012-0311-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridenour TA, Wittenborn AK, Raiff BR, Benedict N, Kane-Gill S. Illustrating idiographic methods for translational research: Moderation effects, natural clinical experiments, and complex treatment-by-subgroup interactions. Translational Behavioral Medicine. 2016;6(1):125–134. doi: 10.1007/s13142-015-0357-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen J. Prisoners of parole. New York Times. 2010 Jan 8; Retrieved from http://www.nytimes.com/2010/01/10/magazine/10prisons-t.html?_r=0. [Google Scholar]
- Theodore LA, Bray MA, Kehle TJ, Jenson WR. Randomization of group contingencies and reinforcers to reduce classroom disruptive behavior. Journal of School Psychology. 2001;39(3):267–277. [Google Scholar]
- Waschbusch DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;128(1):118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, Carrey NJ, Willoughby MT, King S, Andrade BF. Effects of methylphenidate and behavior modification on the social and academic behavior of children with disruptive behavior disorders: The moderating role of callous/unemotional traits. Journal of Clinical Child and Adolescent Psychology. 2007;36(4):629–644. doi: 10.1080/15374410701662766. [DOI] [PubMed] [Google Scholar]
- Wilkinson S, Waller R, Viding E. Practitioner Review: Involving young people with callous unemotional traits in treatment - does it work? A systematic review. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2016;57(5):552–565. doi: 10.1111/jcpp.12494. [DOI] [PubMed] [Google Scholar]