Abstract
GENERAL PURPOSE:
To provide information from a review of literature about economic evaluations of preventive strategies for pressure injuries (PIs).
TARGET AUDIENCE:
This continuing education activity is intended for physicians, physician assistants, nurse practitioners, and nurses with an interest in skin and wound care.
LEARNING OBJECTIVES/OUTCOMES:
After participating in this educational activity, the participant should be better able to:
1. Identify the purpose and methods used for this study.
2. Compare costs and effectiveness related to preventative strategies for PIs.
ABSTRACT
BACKGROUND: Pressure injuries (PIs) are a common and resource-intensive challenge for acute care hospitals worldwide. While a number of preventive strategies have the potential to reduce the cost of hospital-acquired PIs, it is unclear what approach is the most effective.
OBJECTIVE: The authors performed a narrative review of the literature on economic evaluations of preventive strategies to survey current findings and identify important factors in economic assessments.
DATA SOURCES: Ovid, MEDLINE, NHS Economic Evaluation Databases, and the Cochrane Database of Systematic Reviews
SELECTION CRITERIA: Potentially relevant original research articles and systematic reviews were considered.
DATA EXTRACTION: Selection criteria included articles that were written in English, provided data on cost or economic evaluations of preventive strategies of PIs in acute care, and published between January 2004 and September 2015. Data were abstracted from the articles using a standardized approach to evaluate how the items on the Consolidated Health Economic Evaluation Reporting Standards checklist were addressed.
DATA SYNTHESIS: The searches identified 192 references. Thirty-three original articles were chosen for full-text reviews. Nineteen of these articles provided clear descriptions of interventions, study methods, and outcomes considered.
CONCLUSIONS: Limitations in the available literature prevent firm conclusions from being reached about the relative economic merits of the various approaches to the prevention of PIs. The authors’ review revealed a need for additional high-quality studies that adhere to commonly used standards of both currently utilized and emerging ways to prevent hospital-acquired PIs.
KEYWORDS: economic evaluation, hospital-acquired pressure injuries, prevention strategies, treatment costs
INTRODUCTION
Hospital-acquired pressure injuries (HAPIs) are globally common, often preventable, costly, and associated with significant morbidity and mortality.1 The point prevalence estimate for pressure injuries (PIs) in Canadian acute care facilities was 25.1% (95% confidence interval, 23.8%–26.3%) in a systematic review published in 2004.2 The total net per-person adjusted cost of hospitalization for a HAPI was reported to be Can $40,000 for a Stage II ulcer and Can $90,000 for a Stage IV ulcer, based on data from the Ontario Case Costing Initiative database in 2013 using the European Pressure Ulcer Advisory Panel (EPUAP) staging system.3 The cost of dealing with PIs is increasing over time. For example, in the United Kingdom, the estimated annual total cost of managing PIs increased approximately 7-fold from 180 million to 321 million in 1993 to 1.4 billion to 2.1 billion in 2000.4 The financial burden of PIs on the United States healthcare system was estimated between $6 and $15 billion (USD) per year in 2012.5
There are many preventive strategies that have been implemented over the years for PIs. Frequent repositioning of patients and pressure redistribution surfaces (either alone or in combination) have attracted the most interest as preventive strategies.6 These approaches, though, appear to be only partially effective and can be costly to implement. It is unclear if any strategy offers financial advantages compared with others. The ability to gauge the likely benefits of the available preventive strategies and compare their cost-effectiveness is essential to making evidence-based decisions about the selection and implementation of preferred methods.4
The authors performed a narrative review of the literature published between 2004 and 2015 that reported on the costs of PIs and economic evaluations of prevention strategies in acute care. Their goals were to identify what prevention strategies had an economic evaluation, assess the relative strengths and weaknesses of the evaluations performed to date, and determine what future economic evaluations should incorporate.
METHODS
Search Strategy
In September 2015, the authors conducted searches on Ovid, MEDLINE, NHS Economic Evaluation Databases, and the Cochrane Database of Systematic Reviews to identify potentially relevant original research articles and systematic reviews on the topic. The search terms “pressure ulcer,” “pressure sore,” “bedsore,” “bed sore,” “decubitus ulcer,” and “decubitus sore” were combined with “cost-benefit analysis,” “cost-effective analysis,” “financial,” “dollar,” “expenditure,” “models,” “economic,” and “health care costs” to identify potentially relevant publications.
Selection Criteria
Two reviewers independently examined the titles and abstracts of identified articles to classify potentially eligible articles for inclusion in the review. These citations were selected for full-text reviews. Selection criteria included the following: written in English, provision of data on cost or economic evaluations of preventive strategies for PIs in acute care/primary healthcare centers, and publication between January 2004 and September 2015. Studies that provided both the original data and systematic reviews were considered.
A single individual performed the full-text reviews. Reviewed articles were selected for inclusion in the narrative review if they provided clear descriptions of interventions, methods used, and outcomes. Data were abstracted from the articles using a standardized approach to evaluate how the items on the CHEERS (Consolidated Health Economic Evaluation Reporting Standards) checklist were addressed.7 All prices were converted and adjusted to 2015 Canadian dollars.
RESULTS
The searches identified 192 citations. Review of titles and abstracts eliminated 149 of them. Thirty-three were chosen for full-text reviews. Nineteen of these articles provided original data with clear descriptions of interventions, study methods, and the economic outcomes considered and were included in the narrative review.3,4,8–24 They are summarized in Tables 1 and 2. Two systematic reviews were also identified.25,26 The remaining 12 articles were not retained because they did not provide either the original data/analyses or an explicit description of the methods used.
Table 1.
STUDIES ON COST OF HOSPITAL-ACQUIRED PRESSURE INJURIES
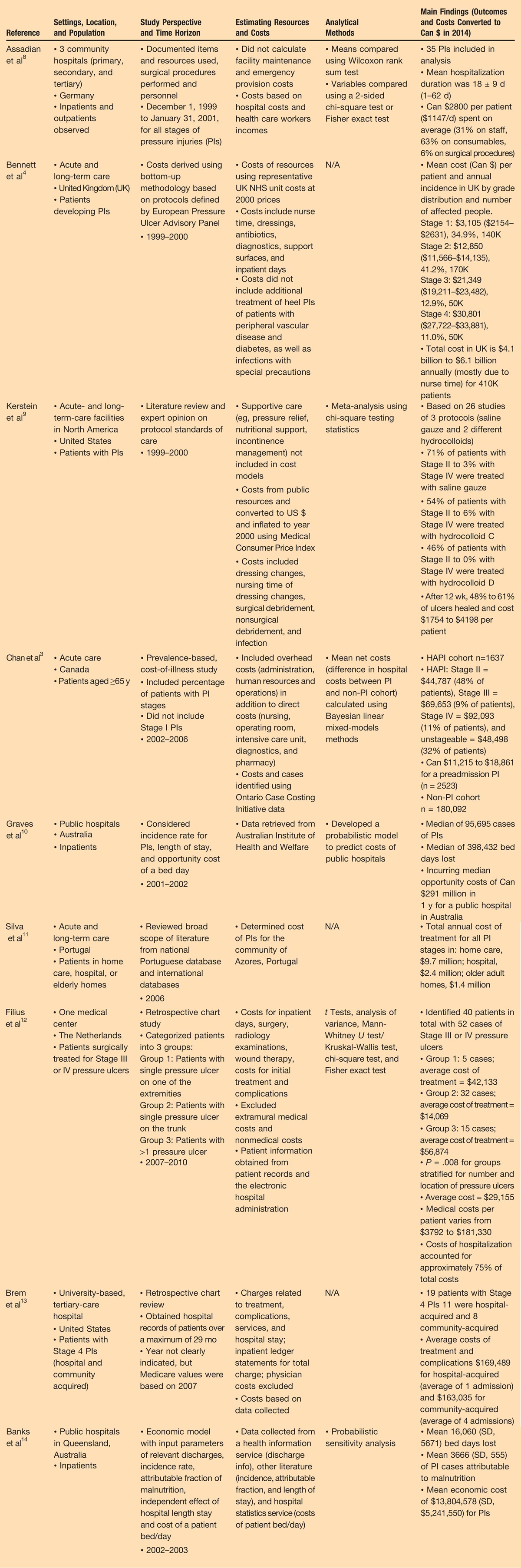
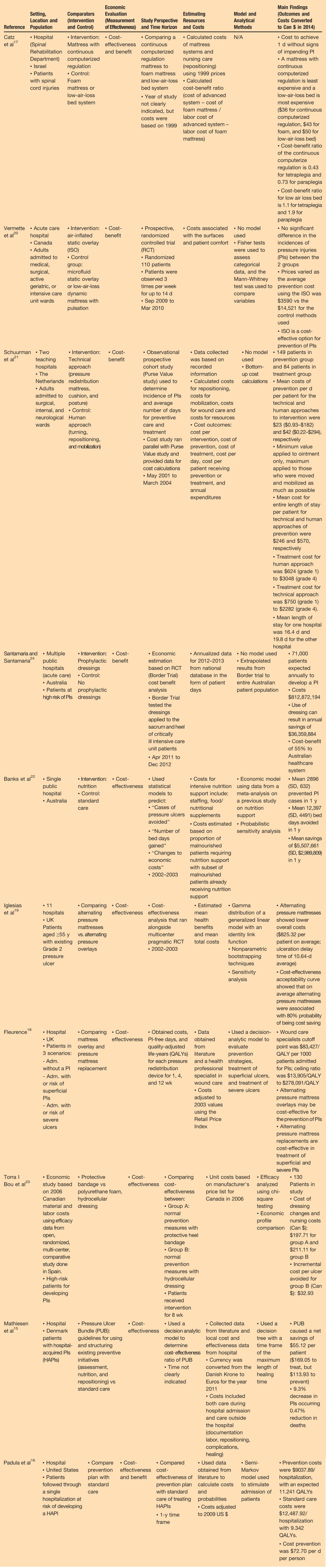
Table 2.
STUDIES ON ECONOMIC EVALUATIONS OF PRESSURE INJURY PREVENTION STRATEGIES
Nine studies reported on the cost of HAPIs.3,4,8–14 All of those studies originated from economically developed regions (Europe,4,8,11,12 North America,3,9,13 Australia10,14), but heterogeneous approaches were taken to estimate and report costs. Notwithstanding these limitations, it was clear that the costs of HAPIs reported were stage-dependent (ie, higher with increasing grade) and high in total.3,4 As indicated by Chan et al,3 the net cost of a Stage II HAPI was Can $44,000 and Can $90,000 for a Stage IV HAPI from 2002 to 2006.
Ten studies provided economic evaluations (5 cost-effectiveness, 3 cost-benefit, 2 both) of approaches to the prevention of PIs.15–24 Favorable outcomes from a bundle of PI prevention strategies were found in 2 studies that based cost estimates on statistical modeling using data from the literature.15,16 A combination of risk assessment, nutritional support, and repositioning resulted in an estimated net savings of Can $55.12 per patient per day, a 9.3% decrease in PI incidence, and a 0.47% reduction in deaths in 2013.15 In the second study, pressure redistribution surfaces, nutritional support, repositioning, and moisture/incontinence control resulted in estimated net savings of Can $3450.03 per hospitalization and a 1.90 increase in quality-adjusted life-years.16
Economic evaluations of single approaches also concluded that implementation of the intervention would result in cost savings. Pressure redistribution surfaces were the modality most commonly studied. These studies typically compared various types of pressure redistribution surfaces with an active control.17–20 In patients with spinal cord injuries requiring assistance with repositioning, a continuous computer-regulated mattress was found to be cost-effective if nurses were not able to frequently reposition patients.17
Mattress overlays were reported to be a cost-effective intervention compared with replacing mattresses,17 whereas another study indicated that alternating pressure mattresses offered an economic advantage compared with alternating pressure overlays.19 An inflated static overlay was found to be less costly and as effective as either a microfluid static overlay or a low-air-loss dynamic mattress with pulsation.19 Pressure redistribution surfaces may be less costly than frequent repositioning programs (Can $23 vs $42 mean cost of prevention per day per patient, respectively).21 Other single approaches to prevent PIs (ie, dressings and nutritional support) also showed apparent financial benefits.22–24 Some of these studies used statistical modeling for their economic evaluations,18,19 whereas others were at least partially based on collected data.17,20,21 The different methods used and the lack of a standard comparator made it impossible to compare across studies.
One of the identified systematic reviews examined the cost of preventing and treating PIs,25 whereas the other assessed economic evaluations embedded in randomized controlled trials (RCTs) of interventions to prevent or treat PIs.26 Both concluded that the cost of treating PIs was substantially higher than preventing them, but noted marked heterogeneity in the methods used in the published studies. For example, Demarre et al25 commented on the differences in study design, perspective taken, cost components considered, and outcomes examined in the available studies. Both suggested standardizing PI economic studies to improve both quality and usability. A number of recommendations, such as enhancing quality of data collection and reporting, were suggested by Demarre et al25 to improve study design and methods.
DISCUSSION
The available evidence validates that PIs are costly and prevention is preferable to treating them once they occur. Beyond that observation, few conclusions can be made. Ideally, economic evaluations should be done concurrently with efficacy trials,3 but unfortunately there are few high-quality RCTs of interventions to either prevent or manage PIs.27 A common challenge to conducting high-quality RCTs as indicated by Palfreyman and Stone26 is the cost of these studies, noting that medical devices, unlike pharmaceuticals, do not require RCTs before they are approved for marketing. In addition, the relevance of results and internal validity of the economic evaluations being done need improvement.28,29 The costs collected and used in studies to date have been inconsistent.25,26 Although direct costs associated with the intervention and the care of patients, such as nursing care and consumables, are commonly included,15–18,20–23 some studies did not specifically identify cost components19 or included only the costs of the intervention.24 One included the cost of care outside the hospital,15 and another study incorporated unforeseen costs but did not specify them.16 Cost components of the intervention, such as cleaning and maintenance costs, were not consistently collected.18 What costs are included affects the outcomes of economic evaluations.25 This variability makes it impossible to accurately compare the cost-effectiveness of different PI prevention approaches.
Another challenge is that a number of the interventions for prevention are complex in nature and involve multiple components, such as training, nursing care, nutritional support, and/or use of technology. This complexity, especially if interventions are individually tailored to deal with identified risk factors, will raise challenges in their economic evaluation.
The authors acknowledge a number of limitations to their narrative review. Their focus was limited to economic evaluations performed to date on the prevention of PI in acute care, not on what approach should be taken to prevent PIs. The authors acknowledge that multicomponent interventions implemented by interdisciplinary teams are viewed as the standard of practice in the prevention in PIs.30,31 Comparing different preventive strategies, especially in isolation, across settings in various patient populations would be counter to the concept of customizing PI prevention interventions. Nearly all of the economic evaluations of PI prevention strategies come from more economically developed nations. One of the few available reports dealing with economically developing nations was a literature review of the prevalence, risks, costs, and solutions to PIs among spinal cord injury patients that did not meet the authors’ inclusion criteria.32 Although the prevalence was high, the authors had difficulty obtaining accurate information, especially economic data. One of few published studies from a less economically developed region dealt with a cardiac hospital in Bangalore, India.33 A quality improvement strategy that included raising awareness, educating staff, improving documentation and communication, and implementing preventive practices, including those in operating rooms, led to a reduction in prevalence from 6% to zero over a 5-month period.33 No economic evaluation was done. Differences in patient populations (and inherent risk for PIs), available resources, labor costs, and other factors emphasize the need for caution in extrapolating results from one setting or country to another.
There are emerging approaches to the prevention of PIs that have not been studied from a cost perspective and may offer advantages. An example of this was continuous monitoring with feedback of interface pressure distribution. This type of technology monitors the interface pressure of patients and could alert caregivers on the need for repositioning a patient and guide how it is done.34–36
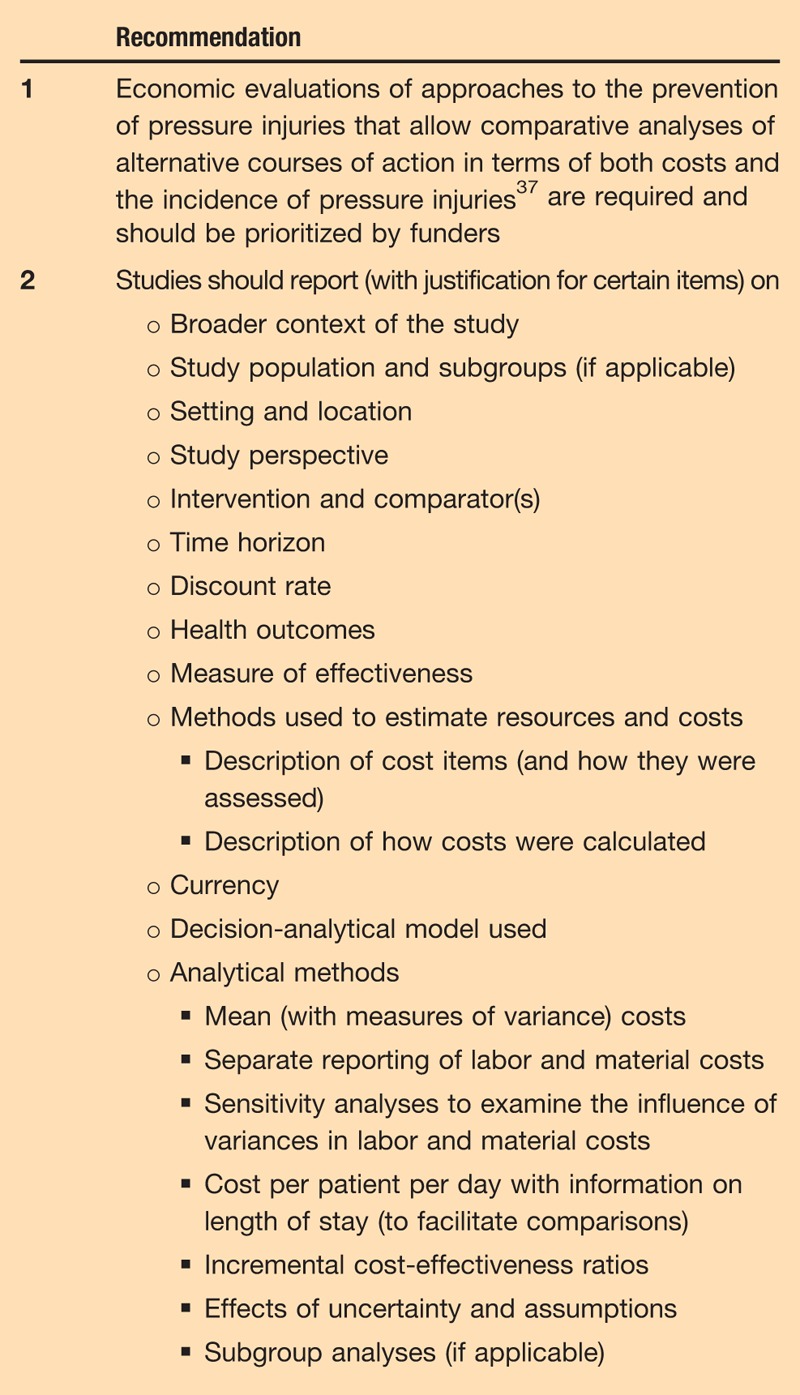
Based on the authors’ review of the literature, a number of recommendations (Table 3)7,25,26,37 to improve on the economic evaluations of approaches to prevent HAPIs were made. The authors believe this information is needed to support rational decisions about PI prevention.
Table 3.
RECOMMENDATIONS FOR FUTURE ECONOMIC EVALUATIONS OF APPROACHES TO THE PREVENTION OF HOSPITAL-ACQUIRED PRESSURE INJURIES7,25,26
CONCLUSIONS
In summary, HAPIs are a common and costly challenge for healthcare systems. Various PI prevention approaches, including pressure redistribution mattresses or overlays, specialized bandages, and nutrition, whether used as single interventions or in a combined manner, have been reported to be cost-effective in at least some studies. However, methodologic limitations including study design heterogeneity, differences in cost components, and intervention complexity undermine our ability to make firm conclusions about the extent of their cost-effectiveness. In addition, the lack of a common methodology prevents the confirmation of promising results found in 1 study or comparing approaches and/or results across studies. The authors suggest that economic evaluation of strategies to prevent HAPIs should be done concurrently with RCTs and conducted in less, as well as more, economically developed nations.
In addition, future economic evaluations of approaches to the prevention of PIs should use explicit, standardized, and appropriate methodology that will allow comparisons of the consequences of alternative courses of action.38
PRACTICE PEARLS
To date, the economic evaluations of PI prevention strategies used as a single or combined intervention are methodologically limited.
A lack of an explicit and standardized approach in conducting economic evaluations makes it difficult to compare approaches and results across studies. Few evidence-based conclusions can be made from the current literature.
Standardized and methodologically sound economic evaluations of strategies to prevent HAPIs should be conducted concurrently with efficacy trials.
Future economic evaluations of PI prevention strategies should allow for comparisons of alternative courses of action in terms of the cost of preventing PIs.
Figure.

No caption available.
Figure.
No caption available.
Footnotes
All authors, faculty, staff, and planners, including spouses/partners (if any), in any position to control the content of this CME activity have disclosed that they have no financial relationships with, or financial interests in, any commercial companies pertaining to this educational activity.
To earn CME or CNE credit, you must read the CME article and complete the quiz online, answering at least 13 of the 18 questions correctly.
This continuing educational activity will expire for physicians on July 31, 2018, and for nurses on July 31, 2019.
All tests are now online only; take the test at http://cme.lww.com for physicians and www.nursingcenter.com for nurses. Complete CE/CME information is on the last page of this article.
Acknowledgment: The authors thank the Alberta Innovates Health Solutions Collaborative Research and Innovation Opportunities team grant (no. 20130152) for funding and supporting this report.
REFERENCES
- 1.Sullivan N, Schoelles KM. Preventing in-facility pressure ulcers as a patient safety strategy: a systematic review. Ann Intern Med 2013;158(5 Pt 2):410-6. [DOI] [PubMed] [Google Scholar]
- 2.Woodbury MG, Houghton PE. Prevalence of pressure ulcers in Canadian healthcare settings. Ostomy Wound Manage 2004;50(10):17. [PubMed] [Google Scholar]
- 3.Chan B, Ieraci L, Mitsakakis N, Pham B, Krahn M. Net costs of hospital-acquired and pre-admission PUs among older people hospitalised in Ontario. J Wound Care 2013;22:341-6. [DOI] [PubMed] [Google Scholar]
- 4.Bennett G, Dealey C, Posnett J. The cost of pressure ulcers in the UK. Age Ageing 2004;33:230-5. [DOI] [PubMed] [Google Scholar]
- 5.Markova A, Mostow EN. US skin disease assessment: ulcer and wound care. Dermatol Clin 2012;30(1):107-11. [DOI] [PubMed] [Google Scholar]
- 6.McInnes E, Jammali-Blasi A, Bell-Syer SE, Dumville JC, Cullum N. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev 2011;(4):CD001735. [DOI] [PubMed] [Google Scholar]
- 7.Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013;346:f1049. [DOI] [PubMed] [Google Scholar]
- 8.Assadian O, Oswald JS, Leisten R, Hinz P, Daeschlein G, Kramer A. Management of leg and pressure ulcer in hospitalized patients: direct costs are lower than expected. GMS Krankenhhyq Interdiszip 2011;6(1):1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kerstein M, Gemmen E, van Rijswijk L, Lyder CH, Philips T, Xakellis G, et al. Cost and cost effectiveness of venous and pressure ulcer protocols of care. Dis Management and Health Outcomes 2001;9:651-63. [Google Scholar]
- 10.Graves N, Birrell F, Whitby M. Modeling the economic losses from pressure ulcers among hospitalized patients in Australia. Wound Repair Regen 2005;13:462-7. [DOI] [PubMed] [Google Scholar]
- 11.Silva AJ, Pereira SM, Rodrigues A, et al. Economic cost of treating pressure ulcers: a theoretical approach. Rev Esc Enferm USP 2013;47:967-72. [DOI] [PubMed] [Google Scholar]
- 12.Filius A, Damen THC, Schuiger-Maaskant KP, Polinder S, Hovius SER, Walbeehm ET. Cost analysis of surgically treated pressure sores Stage III and IV. J Plast Reconstr Aesthet Surg 2013;66:1580-6. [DOI] [PubMed] [Google Scholar]
- 13.Brem H, Maggi J, Nierman D, et al. High cost of Stage IV pressure ulcers. Am J Surg 2010;200:473-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Banks MD, Graves N, Bauer JD, Ash S. The costs arising from pressure ulcers attributable to malnutrition. Clin Nutr 2010;29:180-6. [DOI] [PubMed] [Google Scholar]
- 15.Mathiesen AS, Nørgaard K, Andersen MF, Møller KM, Ehlers LH. Are labour-intensive efforts to prevent pressure ulcers cost-effective? J Med Econ 2013;16:1238-45. [DOI] [PubMed] [Google Scholar]
- 16.Padula WV, Mishra MK, Makic MB, Sullivan PW. Improving the quality of pressure ulcer care with prevention: a cost-effectiveness analysis. Medical Care 2011;49:385-92. [DOI] [PubMed] [Google Scholar]
- 17.Catz A, Zifroni A, Philo O. Economic assessment of pressure sore prevention using a computerized mattress system in patients with spinal cord injury. Disabil Rehabil 2005;27:1315-9. [DOI] [PubMed] [Google Scholar]
- 18.Fleurence RL. Cost-effectiveness of pressure-relieving devices for the prevention and treatment of pressure ulcers. Int J Technol Assess Health Care 2005;21:334-41. [DOI] [PubMed] [Google Scholar]
- 19.Iglesias C, Nixon J, Cranny G, et al. Pressure relieving support surfaces (PRESSURE) trial: cost effectiveness analysis. BMJ 2006;332:1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vermette S, Reeves I, Lemaire J. Cost effectiveness of an air-inflated static overlay for pressure ulcer prevention: a randomized, controlled trial [provisional abstract]. Wounds 2012;24:207-14. [PubMed] [Google Scholar]
- 21.Schuurman JP, Schoonhoven L, Defloor T, van Engelshoven I, van Ramshorst B, Buskens E. Economic evaluation of pressure ulcer care: a cost minimization analysis of preventive strategies. Nurs Econ 2009;27:390-400, 415. [PubMed] [Google Scholar]
- 22.Banks MD, Graves N, Bauer JD, Ash S. Cost effectiveness of nutrition support in the prevention of pressure ulcer in hospitals. Eur J Clin Nutr 2013;67(1):42-6. [DOI] [PubMed] [Google Scholar]
- 23.Torra I Bou J-E, Herrero E, Hernández E, et al. Preventing pressure ulcers on the heel: a Canadian cost study. Dermatol Nurs 2009;21:268-72. [PubMed] [Google Scholar]
- 24.Santamaria N, Santamaria H. An estimate of the potential budget impact of using prophylactic dressings to prevent hospital-acquired PUs in Australia. J Wound Care 2014;23:583-9. [DOI] [PubMed] [Google Scholar]
- 25.Demarre L, van Lancker A, van Hecke A, et al. The cost of prevention and treatment of pressure ulcers: a systematic review. Int J Nurs Stud 2015; 52:1754-74. [DOI] [PubMed] [Google Scholar]
- 26.Palfreyman SJ, Stone PW. A systematic review of economic evaluations assessing interventions aimed at preventing or treating pressure ulcers. Int J Nurs Stud 2015;52:769-88. [DOI] [PubMed] [Google Scholar]
- 27.Clancy MJ. Pressure redistribution devices: what works, at what cost and what’s next? J Tissue Viability 2013;22(3):57-62. [DOI] [PubMed] [Google Scholar]
- 28.Baltussen R, Ament A, Leidl R. Making cost assessments based on RCTs more useful to decision-makers. Health Policy 1996;37:163-83. [DOI] [PubMed] [Google Scholar]
- 29.Ramsey S, Willke R, Briggs A, Brown R, Buxton M, Chawla A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health 2005;8:521-33. [DOI] [PubMed] [Google Scholar]
- 30.National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Washington, DC: National Pressure Ulcer Advisory Panel; 2014. [Google Scholar]
- 31.Qaseem A, Mir TP, Starkey M, Denberg TD; Clinical Guidelines Committee of the American College of Physicians. Risk assessment and prevention of pressure ulcers: a clinical practice guideline from the American College of Physicians. Ann Intern Med 2015;162:359-69. [DOI] [PubMed] [Google Scholar]
- 32.Zakrasek EC, Creasey G, Crew JD. Pressure ulcers in people with spinal cord injury in developing nations. Spinal Cord 2015;53(1):7-13. [DOI] [PubMed] [Google Scholar]
- 33.Paul R, McCutcheon SP, Tregarthen JP, Denend LT, Zenios SA. Sustaining pressure ulcer best practices in a high-volume cardiac care environment. Am J Nurs 2014;114(8):11. [DOI] [PubMed] [Google Scholar]
- 34.Du H, Cork R. XSENSOR technology. A pressure imaging overview. Sensor Rev 2007;27(1):24-8. [Google Scholar]
- 35.Sakai K, Sanada H, Matsui N, Nakagami G, Sugama J, Komiyama C, et al. Continuous monitoring of interface pressure distribution in intensive care patients for pressure ulcer prevention. J Adv Nurs 2009;65:809-17. [DOI] [PubMed] [Google Scholar]
- 36.Yip M HD, Winokur E, Balderrama AG, Sheridan R, Ma H. A flexible pressure monitoring system for pressure ulcer prevention. Presented at the 31st Annual International Conference of the IEEE EMBS; Minneapolis, Minnesota; September 2-6, 2009. [DOI] [PubMed]
- 37.Cano A, Anglade D, Stamp H, et al. Improving outcomes by implementing a pressure ulcer prevention program (PUPP): going beyond the basics. Healthcare (Basel) 2015;3:574-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. 3rd ed Oxford, UK: Oxford University Press; 2005. [Google Scholar]


