Abstract
Study Objectives:
To investigate parental knowledge about adolescent sleep needs, and other beliefs that may inform their support for or objection to later school start times.
Methods:
In 2014, we conducted a cross-sectional, Internet-based survey of a nationally representative sample of parents as part of the C.S. Mott Children's Hospital National Poll on Children's Health. Parents with teens aged 13–17 years reported their children's sleep patterns and school schedules, and whether the parents supported later school start times (8:30 am or later). Responses associated with parental support of later school start times were examined with logistic regression analysis.
Results:
Overall, 88% of parents reported school start times before 8:30 am, and served as the analysis sample (n = 554). In this group, 51% expressed support for later school start times. Support was associated with current school start times before 7:30 am (odds ratio [OR] = 3.1 [95% confidence interval (CI) 1.2, 8.4]); parental opinion that their teen's current school start time was “too early” (OR = 3.8 [1.8, 7.8]); and agreement with American Academy of Pediatrics recommendations about school start times (OR = 4.7 [2.2, 10.1]). Support also was associated with anticipation of improved school performance (OR = 3.0 [1.5, 5.9]) or increased sleep duration (OR = 4.0 [1.8, 8.9]) with later school start times. Conversely, parents who anticipated too little time for after-school activities (OR = 0.5 [0.3, 0.9]) and need for different transportation plans (OR = 0.5 [0.2, 0.9]) were often less supportive.
Conclusions:
Parental education about healthy sleep needs and anticipated health benefits may increase their support for later school start times. Educational efforts should also publicize the positive experiences of communities that have made this transition, with regard to limited adverse effect on after-school activity schedules and transportation.
Citation:
Dunietz GL, Matos-Moreno A, Singer DC, Davis MM, O'Brien LM, Chervin RD. Later school start times: what informs parent support or opposition? J Clin Sleep Med. 2017;13(7):889–897.
Keywords: adolescents, circadian rhythms, high school, insufficient sleep, parental opinion, poll, school start times, sleep deprivation, survey
INTRODUCTION
Adequate sleep is a major determinant of healthier, longer life and well-being across the lifespan.1 Sufficient sleep is particularly important during human development and growth.2,3
Short sleep has been linked to several adverse outcomes, including reduced learning capacity and poor academic performance4,5; impaired metabolism that may lead to weight gain, obesity and type 2 diabetes6–8; drowsy driving and motor vehicle accidents9,10; dysregulation of behavior, emotions and mood11,12; and substance use, anxiety, and depression.13,14
The average adolescent needs about 9 hours of sleep per night for optimal daytime function.15,16 However, at the onset of puberty, physiological changes tend to include a longer circa-dian cycle and an approximate 2-hour delay in timing of sleep and wake. As a result, teens' natural sleep preferences evolve toward 11:00 pm bedtimes and 8:00 am wake times.15,17 In addition to biological mechanisms, social and lifestyle factors such as heavy academic load, after-school activities or jobs, screen time, and caffeine consumption also contribute to adolescents' later bedtimes.18–20 Because most adolescents in the United States start school before 8:30 am,21,22 it is not surprising that the average teen experiences a chronic sleep debt.23,24
BRIEF SUMMARY
Current Knowledge/Study Rationale: Despite recent evidence that links later school start times with improved sleep health among adolescents, most middle and high schools have current start times before 8:30 am. This study identifies potential facilitators and barriers to parental support for school start times at 8:30 am or later.
Study Impact: Results from this nationally representative survey of United States parents of adolescents suggest that education about medical recommendations in support of later school start times, anticipated effect on health, and performance benefits might improve support for adoption of recommended school start times. Efforts to publicize the positive experiences of communities that have made this transition, with regard to previously feared family scheduling and transportation challenges, may also prove helpful.
Numerous reports suggest that delaying school start time (SST) improves sleep patterns.25,26 Thus, in an effort to promote adolescent health, safety, and quality of life, in 2014 the American Academy of Pediatrics (AAP) published a policy statement that expressed full support for SSTs at 8:30 am or later.27 The American Academy of Sleep Medicine (AASM) also published a position statement that recommends later SSTs for high school students to improve their sleep health.28
To shift SSTs later in the morning will likely require support from parents, whose teens experience the negative consequences of sleep deprivation. Published literature has not reported well-characterized parental attitudes, opinions, perceptions, or experiences that may impede institution of later SSTs. Therefore, we aimed to (1) identify potential facilitators of, and barriers to, parental support for later SSTs, and (2) compare published recommendations for teens' sleep duration with parents' opinions on sufficient sleep duration for their adolescents. Our hypotheses were that parental perception of adolescents' sleep needs, as well as other identifiable and potentially modifiable factors, would show associations with failure to support later SSTs.
METHODS
Study Design
In November and December of 2014, we conducted a cross-sectional, internet-based survey of a nationally representative sample of the United States population. The multipart survey included questions regarding medical marijuana, parental use of social media, health behavior, hospital satisfaction, and SSTs. This survey was conducted as part of the C.S. Mott Children's Hospital National Poll on Children's Health (NPCH), a recurring online survey of parents and nonparents about issues related to children's health in the United States.29 The NPCH has served as the data source for other national peer-reviewed studies about health-related issues for more than 9 years.29–31
The NPCH is designed by investigators at the University of Michigan and fielded by GfK Custom Research, LLC Group (GfK). Funding for the NPCH is provided by the University of Michigan Health System. The study was approved by the University of Michigan Medical School Institutional Review Board.
Study Population
The sample used for this study was drawn from GfK's web-enabled KnowledgePanel, which is composed of more than 50,000 potential respondents in all 50 states and the District of Columbia. For individuals who agree to participate but do not have a computer or internet access, GfK supplies these items free of charge. Participants are assigned personal log-in information to access surveys online and receive invitations to participate in surveys via email. Incentive points (per survey and redeemable for cash, merchandise, gift cards, or game entries), are provided to respondents for survey completion. On average, panel members complete 2 to 3 surveys per month, with typical durations of 10 to 15 minutes per survey.
Probability-based sampling was used to recruit members into the KnowledgePanel to achieve representativeness. Panel members were initially contacted using a random-digit dialing and address-based sampling method following the United States Postal Service's Delivery Sequence files. Census blocks with high-density minority communities were oversampled and remaining census blocks were relatively undersampled. A unique random sample of participants was drawn from the larger panel of candidates for this study, with an oversample of KnowledgePanel households that had at least one child younger than 18 years. The survey was fielded by GfK during November 28, 2014–December 31, 2014, to 3,812 panel members via email. The email notification contained a link that sent sampled individuals to the survey, without any cues about the specific content regarding SSTs. Reminders were sent after 3 days to remaining nonresponding members of the sample. Only one adult per household was selected.
The resulting study sample in the NPCH is nationally representative of adults in the United States. Only parents or legal guardians of teens 13 to 17 years old were asked questions about their adolescents' sleep habits and SSTs. The survey included questions about parental concerns regarding changes in SSTs, support of the AAP guidelines related to SSTs, and benefits of later SSTs. At the end of the data collection, GfK sent deidentified survey and demographic data to the research team as an electronic file. Adjustments were applied to sampling weights to account for selection probability, nonresponse probability, and poststratification. Poststratification weights were calculated to adjust for undersampling and oversampling populations in the United States by comparing respondents' demographic information (sex, race/ ethnicity, age, education, census region, and household income) with the United States Current Population Survey data.
Outcome and Predictor Variables
Data for all variables were collected through survey responses of the participants (see poll sleep questions in the supplemental material). Parental support for later SSTs, collected with a three-category outcome, (“yes, regardless of the impact on school budget”; “yes, if does not impact the school budget”; “no”) was recoded to a binary (“yes/no”) outcome to ensure adequate power for comparisons. Three types of candidate predictor variables were used in the analyses: (1) demographic factors (parent age, adolescent age, race/ethnicity, education, household income, household size, geographic region, school type); (2) sleep-related predictors (current SSTs, parental opinion about SSTs of their teen, parental awareness of and agreement with AAP recommendation on later SSTs, adolescent sleep duration, parental opinion about sleep duration, teen adherence to bedtime schedule, bedtime, and clock time their teen leaves for school); and (3) parental opinion about potential positive and negative effect of later SSTs. Assessed positive predictors of support for later SSTs included anticipated benefits such as: improved school performance, ability to obtain more sleep, improved health, and reduced stress. Assessed negative predictors included: lack of time for after-school activities, inability to find a job, interference with mealtime, and effect on school transportation.
Statistical Analysis
Inferential methods for survey data (chi-square and linear regression) were first used to compare demographic and adolescent sleep characteristics for parents who supported versus opposed later SSTs. We then examined parental opinions about the expected effect of delayed SSTs on their teen.
The associations among demographic and adolescent sleep characteristics, parental opinions about the impact of delayed SSTs, and parental support for later SSTs were examined using bivariate and multivariate logistic regression models for survey data. We first fit bivariate models with each predictor to assess their associations with support of later SSTs. Predictors with P < .15 in bivariate analyses were selected for inclusion in the first multivariate model. As a second step, we removed all nonsignificant predictors (P > .05) in the initial multivariate model and fit the final model with the set of most influential predictors of support for later SSTs. Odds ratios (OR) with 95% confidence intervals (CI) were computed for bivariate and final models to evaluate parental support for delaying SSTs (yes/no).
Finally, the National Sleep Foundation standards and AASM recommendations for adolescent sleep needs were used to evaluate parental opinions about what constitutes sufficient sleep.32,33 We used SAS software, version 9.4 (SAS Institute, Cary, North Carolina, United States) for all statistical analyses.
RESULTS
Study Sample
Of the 3,812 adults invited to participate, 3,061 were parents of children 17 years or younger, and 1,563 completed the survey (response rate = 51%, as determined using RR1 of the American Association for Public Opinion Research).34 Of these, 636 adults identified themselves as parents or legal guardians of teens 13 to 17 years of age, living in the same household and attending public/charter or private school. Among this subgroup, 554 parents whose teens had SSTs before 8:30 am were eligible for inclusion in the current analysis. Demographic characteristics of these parents are presented in Table 1.
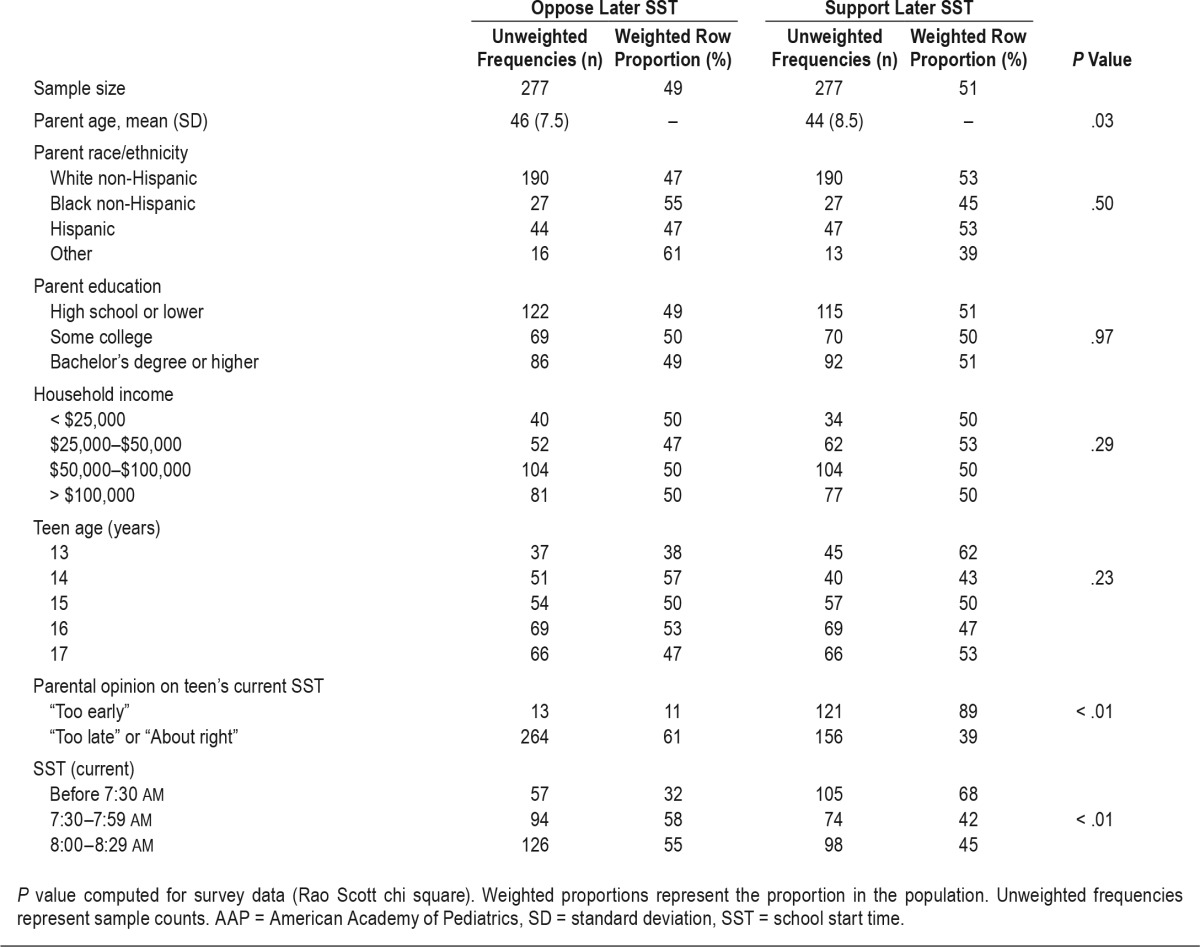
Table 1.
Demographic characteristics of parents and perceptions of their teens' sleep, by parental support of later SST.
Beliefs and Opinions That May Inform Support or Opposition in Regard to Later School Start Times
Among parents with teens who have an SST earlier than 8:30 am, similar numbers supported versus opposed later SSTs (Table 1). Teens' SSTs, parental opinions about SSTs, agreement with the AAP recommendations for later SSTs, and the time a teen leaves for school in the morning were significantly different (all P < .05) among supporters versus nonsupporters. Conversely, parent demographic characteristics (except for age), adolescent sleep patterns (bedtime, sleep duration), adherence to bedtime routine, and parental opinion about sufficiency of their teen's sleep all were comparable among parents supporting versus opposing later SSTs.
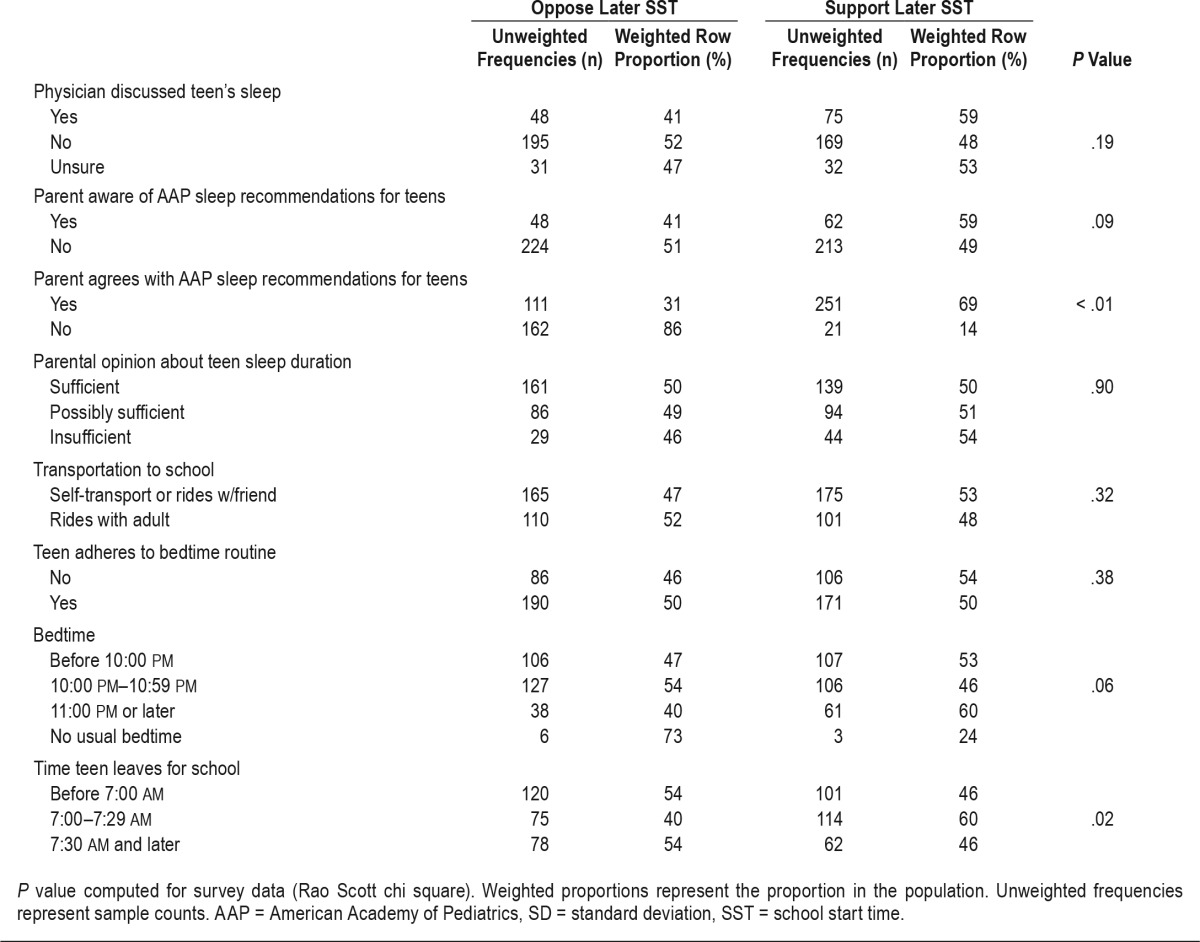
Parents anticipating a positive effect for their teens following later SSTs (eg, improved school performance and health, reduced stress, or ability to get more sleep) were more likely to support later SST (Figure 1, P < .01). Parents expecting a negative effect resulting from later SSTs (eg, interference with after-school activities, transportation plans, or mealtime) were more likely to oppose later SSTs (P < .01). However, teens' inability to find a job was not significantly associated with parental support for later SSTs.
Figure 1. Distribution of opinions about the effect of a later SST on teens, among parents supporting versus opposing a later SST.
Proportions are weighted to represent parents of teens 13–17 years old in the United States. * = P < .01. SST = school start time.
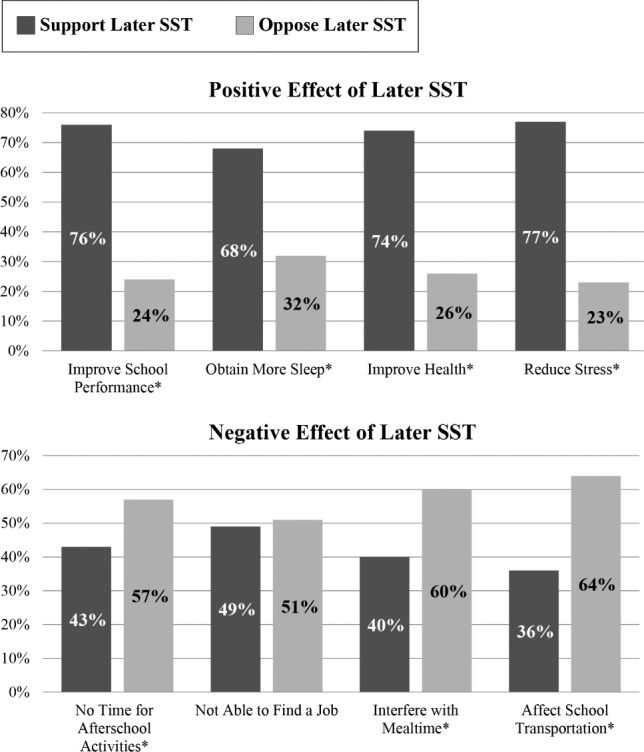
In adjusted logistic regression models, no demographic characteristics or current teen sleep patterns (eg, sleep duration, bedtime, adherence to bedtime routine) were associated with parental support of later SSTs. In contrast, parental support for later SSTs was associated with parental opinions about current SSTs as “too early” compared to “too late or about right,” and with agreement on AAP recommendations about later SSTs (Table 2). Similarly, parental support of later SSTs was significantly associated with perceived positive effect of later SSTs, namely, better academic performance in school and increased sleep duration. Conversely, parents expecting disruptions of school day schedules and transportation were significantly less likely to support later SSTs. Compared with SSTs of 8:00 am–8:29 am, SSTs before 7:30 am were associated with threefold higher parental support for later SSTs. However, parents whose teens' SSTs were at 7:30 am–7:59 am were not more likely than those of teens with SSTs at 8:00 am–8:29 am to support later SSTs.
Table 2.
Crude and adjusted odds ratios for support of later school start time among parents of adolescents.
In exploratory analyses, we separated unconditional supporters of later SSTs from parents who supported later SSTs only if that would entail no budget changes. However, the results for each group of supporters were similar to those obtained when their data were pooled (data not shown).
Parental Beliefs About Their Teens' Sleep Needs
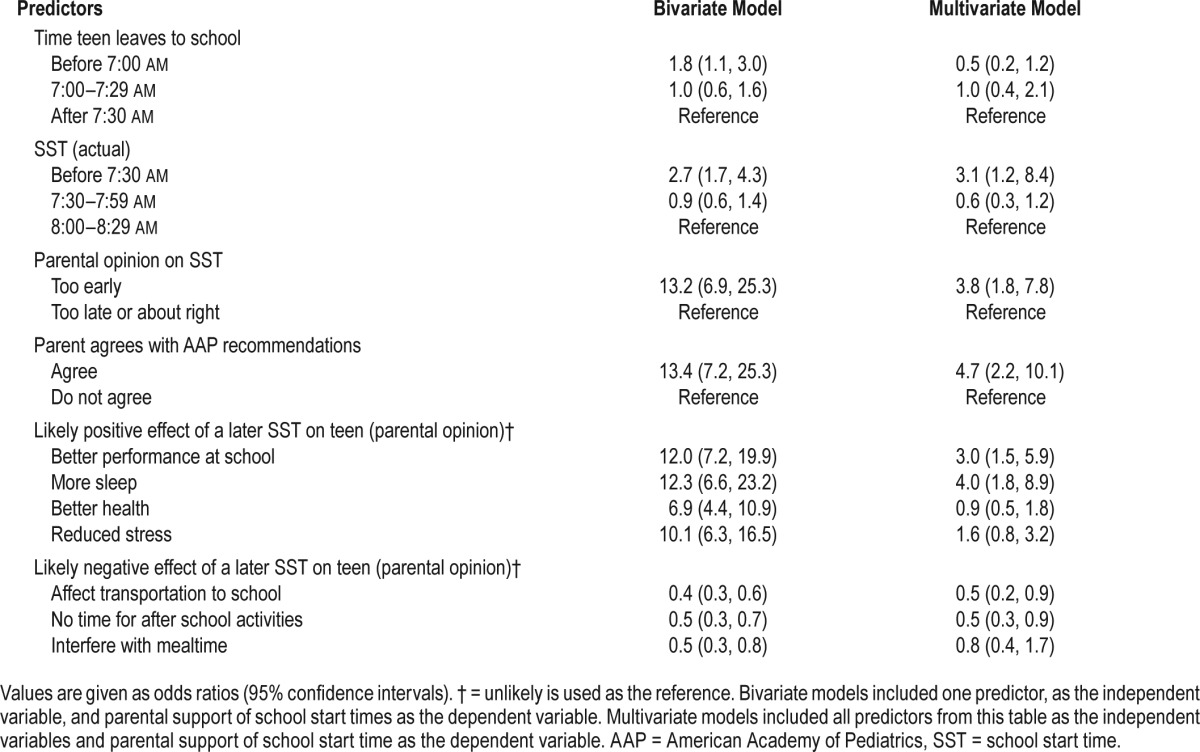
Almost 50% of the parents reported deficient sleep (fewer than 7 hours) as sufficient or possibly sufficient for their adolescents (Table 3). Further, most parents (86% to 100% depending on teen's age) perceived just a little more sleep, 7–7.5 hours, as sufficient or possibly sufficient sleep duration for teens, in contrast with published recommendations that 7–8 hours “may be appropriate.”32 Finally, in alignment with recommendations for sufficient sleep for teens, more than 90% of parents report that 8 or more hours of sleep is a sufficient or possibly sufficient sleep duration.
Table 3.
Parental opinions on sufficient sleep duration of their adolescents.
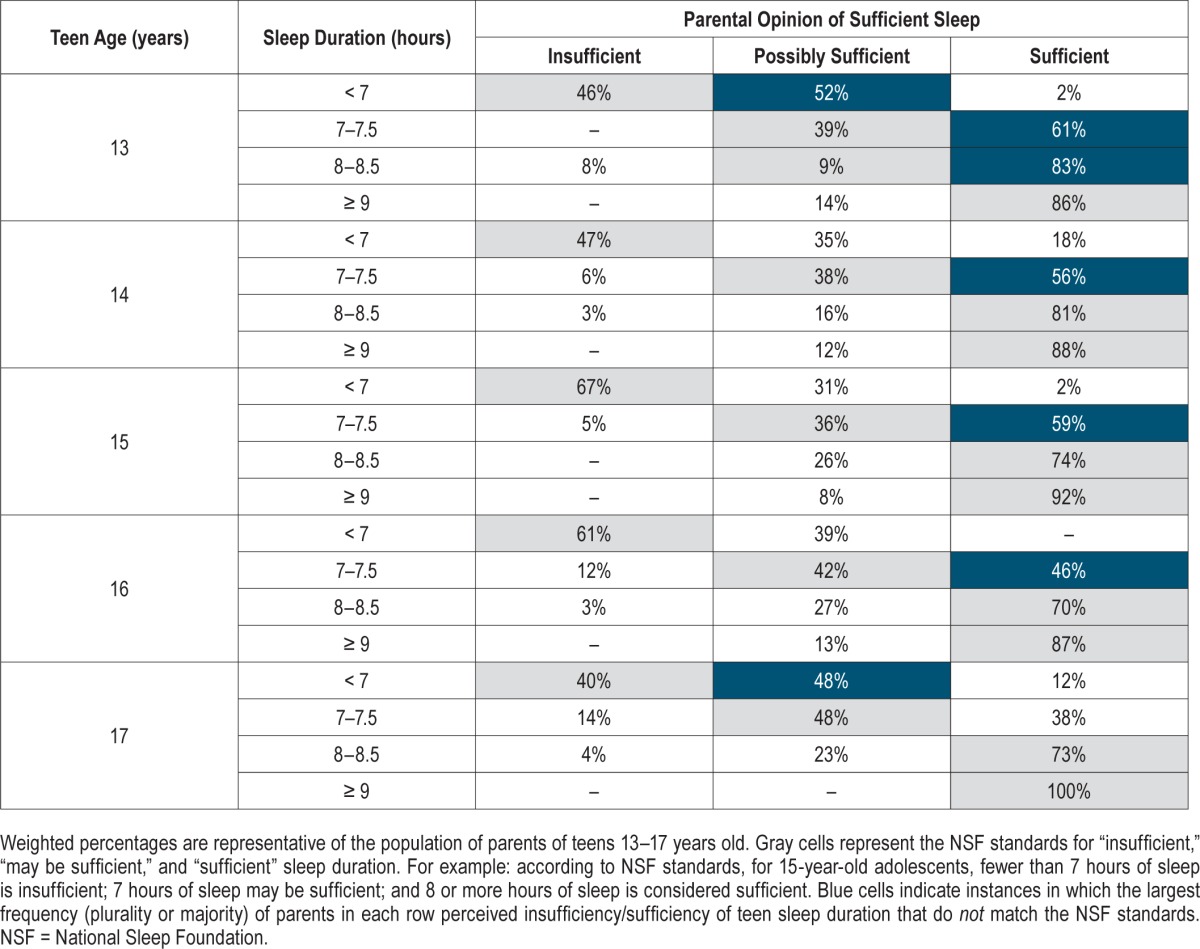
DISCUSSION
Data from this nationally representative survey of parents of teens suggest that public support for delayed SSTs is linked to parental challenges, expectations, and opinions about their teens' current SST or its prospective delay. Parents who did support later SSTs tended to be those who reported an early SST for their teens (before 7:30 am), viewed their teens' SSTs as “too early,” agreed with AAP recommendations on later SSTs, and expected positive effect on their teen's academic performance and sleep, following delayed SSTs. Conversely, parents who anticipated negative effect on school-related transportation plans or after-school activities were significantly more likely than their peers to oppose later SSTs. Additional results showed that parents often had misconceptions about how much sleep teens need, with nearly half indicating that fewer than 7 hours of sleep was sufficient or possibly sufficient and approximately 90% of parents perceiving 7–7.5 hours of sleep as sufficient or possibly sufficient for their teens. These data are some of the first to explore potential reasons for resistance among parents to medical recommendations for later SSTs.
Increased Support for Later School Start Times May Require Education About Teen Sleep Needs
Despite recommendations from the AAP that specifically highlight the importance of later SSTs,27 delay of SSTs to 8:30 am or later remains controversial among parents, schoolteachers, and administrators. In our survey, the extent of parental support for later SSTs corresponded to agreement with AAP recommendations for teen sleep. This strong association provides rationale for invigorated efforts to educate parents about sleep health of teens.
The opposition of many parents—about half of those surveyed—to later SSTs may reflect, at least in part, the high prevalence of adolescent sleep-need beliefs that underestimate AASM and National Sleep Foundation consensus panel recommendations.32,33 To achieve the AAP-recommended later SSTs in the 85% of public middle and high schools that have not implemented them, broader parental education about AAP recommendations and academic benefits of SSTs may be necessary. Such educational efforts and publicity could conceivably be conducted by professional societies or foundations that promote child health. However, the individual pediatrician may also have an important role to play. Most parents in our study (77%) did not recall discussing sleep with their pediatrician. Discussion about sleep health and sleep hygiene should be a concise part of a child's well-visit care.
Sufficient sleep is key for physical and mental health, improved cognition, learning, neurobehavioral function, and safety.4–11,13,14 Chronic sleep deprivation, commonly observed among adolescents, arises in large part from the combination of late bedtimes and early SSTs. Several studies have linked later SSTs with longer sleep duration, improved daytime cognition and function, and decreased sleep problems.4,18 A study within the Minneapolis school district examined the associations of SSTs and sleep patterns among high school students. Students with an 8:40 am SST reported an additional hour of sleep compared to students with a 7:15 am SST.35 A recent systematic review associated delaying SSTs to 8:30 am or later with longer sleep duration, increased daytime alertness and function, improved health and behavior, and reduced incidence of car accidents.36 Specifically, 25- to 60-minute delays in SSTs increased sleep duration 25 to 77 minutes, suggesting favorable effect on sleep duration even after modest SST change. Indeed, a 30-minute change in the SST at a Rhode Island high school was associated with longer sleep as well as improved daytime alertness, motivation, and mental health.26 Further support for a positive effect of later SSTs on sleep duration, as well as reduced car accidents and daytime sleepiness, was provided in a recent evidence-based review.37 However, this study found only weak evidence overall for the association of later SSTs and improved academic performance and behavioral health.
Bedtimes are generally similar among high schoolers, independent of their SST.35,36 The latter finding of adolescents' regular bedtimes has been reported elsewhere as well38,39 and is consistent with natural sleep preferences and circadian rhythms during adolescence.17 Thus, later SSTs, rather than efforts to institute earlier bedtimes, may be more influential to improve sleep health among adolescents.
Educational Efforts Will Be Needed Across All Demographic Groups
In this nationally representative survey, we found similar demographic characteristics, including household income, parental education, race, and teen's age, among parents who support or oppose later SSTs. These findings suggest identical support patterns across socioeconomic classes and racial groups. These data do not suggest that efforts to educate parents about adolescent sleep health should be directed more at any one demographic group than another.
Barriers to Later School Start Times: Perception Versus Reality
Our data identified scheduling and transportation challenges as likely barriers to broader public support of delayed SSTs. These barriers may explain the reluctance among stakeholders to adopt recommended changes. Indeed, in a survey about high school start times, 345 high school administrators described athletic practices as the major barrier (55% of the respondents) to implementation of later SSTs, followed by teachers' concerns (32%), expected costs of SST changes (30%), parental concerns (28%), after-school activities (26%), and childcare logistics (20%).22 In contrast to potential negative effects sometimes anticipated with later SSTs, communities that have delayed their SSTs have reported positive effect on their students. In the same survey, high school administrators were also asked whether their district has changed or considered a change in SSTs, or if no change has been contemplated. High school administrators whose district had implemented or considered delays in SSTs, about 40% of the respondents, associated the change with positive effects such as reduced tardiness, increased attendance, better academic performance, and increased satisfaction among students and teachers alike.22 Of note, negative effects of delayed SSTs were negligible: only 4% of respondents reported negative effect on athletic achievements, 3% indicated decreased school attendance, and 2% associated the change in SSTs with student moodiness.22
Positive effects of later SSTs were also observed in a 2014 survey of high school students, who reported after a 25-minute delay in SST that they spent similar time in athletic and academic after-school activities, and were less tired after school.25 Sufficient time for after-school activities with later SSTs has been confirmed elsewhere.36 A recent longitudinal study associated a 45-minute delay in high school start time with reduced tardiness and disciplinary violations at 6-month and 12-month follow-up. However, longer sleep duration was evident only at 6 months.40 Furthermore, a pilot study that examined the effect of a 30-minute delay to a high school start time reported that faculty and athletic coaches strongly opposed the SST change, and planned to reintroduce an 8:00 am SST once the study was completed.26 However, during the study, students and faculty recognized significant improvements to their quality of life following the SST delay, and subsequently agreed to retain 8:30 am as the SST. Published real-world experiences such as these provide an opportunity for education of administrators and parents opposed to later SSTs, who, like our respondents, may be surprised to learn that their fears about the assumed negative effects of later SSTs may not be well justified.
Financial costs related to changes in transportation schedules are also often cited as a barrier to delaying SSTs.38,41 However, evidence suggests that transportation rescheduling costs following delayed SSTs are district specific and may increase, decrease, or remain unchanged.41 Fewer than 34% of K-12 students use school buses42 as high school districts transition to public buses.41 Correspondingly, in our study we found that only 37% of adolescents arrived to school on a bus or via public transportation.
In summary, available evidence in the literature, combined with our findings, indicate a gap between anticipated and actual adverse effect of delayed SSTs. Although anticipated negative effect of later SSTs on schedules and transportation is a primary barrier to implementation of later SSTs, such negative effect does not appear to be realized in practice.
Study Limitations
Limitations of this study include the potential for nonresponse bias, although we attempted to mitigate this possibility by inviting individuals to participate without disclosing the topics. Another limitation is that we sampled parents of teens in school districts that already have later SSTs, as well as parents in districts with earlier SSTs. If there were a data source that permitted targeted sampling based on SSTs, we could have implemented a more efficient study design. However, such a sampling approach would not have been generalizable to the full United States population of parents of teens aged 13–17 years. Finally, the implications of our study could have been further investigated by testing messages about later SSTs and whether they would potentially change the opinions and knowledge of parents who initially expressed opposition to later SSTs. However, the current set of survey questions was fielded as one element of a multipart survey and we did not want to overly burden respondents. Such testing of messages about later SSTs merits future research.
CONCLUSIONS
This nationally representative survey illuminates potential explanations for why approximately half of parents in United States households with teen children do not support AAP and AASM recommendations for SSTs at 8:30 am or later. Parents often did not understand the sleep needs of their adolescents. When they were aware of AAP recommendations for later SSTs and related health benefits, parents did tend to support later SSTs. Parental education about healthy sleep during adolescents' well-care visits may be key, to broaden awareness that significant benefits are likely and harms less likely in practice after adoption of later SSTs.
DISCLOSURE STATEMENT
Work for this study was performed at the University of Michigan's Medical School. This work was partially supported by a T32 Grant from the National Institute of Neurological Disorders and Stroke (NIH/NINDS T32 NS007222). The C.S. Mott National Poll on Children's Health is supported by the University of Michigan Health System. Dr. Chervin is named in or has developed patented and copyrighted materials owned by the University of Michigan and designed to assist with assessment or treatment of sleep disorders; these materials include the Pediatric Sleep Questionnaire Sleep-Related Breathing Disorder Scale. This questionnaire is licensed online by the University of Michigan to appropriate users at no charge, and (for electronic use) to Zansors. Dr. Chervin serves on the boards of the American Academy of Sleep Medicine (currently as President); the International Pediatric Sleep Society; and the nonprofit Sweet Dreamzzz. He is an editor for UpToDate, has edited a book for Cambridge University Press, and has consulted for Zansors. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Dr. Brady T. West.
ABBREVIATIONS
- AASM
American Academy of Sleep Medicine
- AAP
Academy of Pediatrics
- CI
confidence interval
- NPCH
National Poll on Children's Health
- NSF
National Sleep Foundation
- OR
odds ratio
- SST
school start time
REFERENCES
- 1.Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC: National Academies Press (US) National Academy of Sciences; 2006. [PubMed] [Google Scholar]
- 2.Dahl RE. Sleep and the developing brain. Sleep. 2007;30(9):1079–1080. doi: 10.1093/sleep/30.9.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frank MG, Issa NP, Stryker MP. Sleep enhances plasticity in the developing visual cortex. Neuron. 2001;30(1):275–287. doi: 10.1016/s0896-6273(01)00279-3. [DOI] [PubMed] [Google Scholar]
- 4.Wolfson AR, Carskadon MA. Understanding adolescents' sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7(6):491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 5.Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bogels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14(3):179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 6.Chaput JP, Despres JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31(4):517–523. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol. 2005;99(5):2008–2019. doi: 10.1152/japplphysiol.00660.2005. [DOI] [PubMed] [Google Scholar]
- 8.Copinschi G, Leproult R, Spiegel K. The important role of sleep in metabolism. Front Horm Res. 2014;42:59–72. doi: 10.1159/000358858. [DOI] [PubMed] [Google Scholar]
- 9.Gander PH, Marshall NS, Harris RB, Reid P. Sleep, sleepiness and motor vehicle accidents: a national survey. Aust N Z J Public Health. 2005;29(1):16–21. doi: 10.1111/j.1467-842x.2005.tb00742.x. [DOI] [PubMed] [Google Scholar]
- 10.Taylor DJ, Bramoweth AD. Patterns and consequences of inadequate sleep in college students: substance use and motor vehicle accidents. J Adolesc Health. 2010;46(6):610–612. doi: 10.1016/j.jadohealth.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–291. doi: 10.1196/annals.1308.032. [DOI] [PubMed] [Google Scholar]
- 12.Shochat T, Cohen-Zion M, Tzischinsky O. Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18(1):75–87. doi: 10.1016/j.smrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: are they linked? Am J Health Behav. 2010;34(2):237–248. doi: 10.5993/ajhb.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behav Sleep Med. 2005;3(3):113–133. doi: 10.1207/s15402010bsm0303_1. [DOI] [PubMed] [Google Scholar]
- 15.Carskadon MA, Harvey K, Duke P, Anders TF, Litt IF, Dement WC. Pubertal changes in daytime sleepiness. Sleep. 1980;2(4):453–460. doi: 10.1093/sleep/2.4.453. [DOI] [PubMed] [Google Scholar]
- 16.Mercer PW, Merritt SL, Cowell JM. Differences in reported sleep need among adolescents. J Adolesc Health. 1998;23(5):259–263. doi: 10.1016/s1054-139x(98)00037-8. [DOI] [PubMed] [Google Scholar]
- 17.Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8(6):602–612. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69(4):875–887. [PubMed] [Google Scholar]
- 19.Teixeira LR, Fischer FM, Nagai R, Turte SL. Teen at work: the burden of a double shift on daily activities. Chronobiol Int. 2004;21(6):845–858. doi: 10.1081/cbi-200036878. [DOI] [PubMed] [Google Scholar]
- 20.Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123(6):e1005–e1010. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 21.Wheaton AG, Ferro GA, Croft JB. School start times for middle school and high school students - United States, 2011-12 school year. MMWR Morb Mortal Wkly Rep. 2015;64(30):809–813. doi: 10.15585/mmwr.mm6430a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolfson AR, Carskadon MA. A survey of factors influencing high school start times. NASSP Bulletin. 2005;89(642):47–66. [Google Scholar]
- 23.Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-Cantrell L, Croft JB. Prevalence of insufficient, borderline, and optimal hours of sleep among high school students - United States, 2007. J Adolesc Health. 2010;46(4):399–401. doi: 10.1016/j.jadohealth.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 24.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21(8):871–881. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 25.Boergers J, Gable CJ, Owens JA. Later school start time is associated with improved sleep and daytime functioning in adolescents. J Dev Behav Pediatr. 2014;35(1):11–17. doi: 10.1097/DBP.0000000000000018. [DOI] [PubMed] [Google Scholar]
- 26.Owens JA, Belon K, Moss P. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch Pediatr Adolesc Med. 2010;164(7):608–614. doi: 10.1001/archpediatrics.2010.96. [DOI] [PubMed] [Google Scholar]
- 27.Adolescent Sleep Working Group; Committee on Adolescence; Council on School Health. School start times for adolescents. Pediatrics. 2014;134(3):642–649. doi: 10.1542/peds.2014-1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Watson NF, Martin JL, Wise MS, et al. Delaying middle school and high school start times promotes student health and performance: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2017;13(4):623–625. doi: 10.5664/jcsm.6558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.C.S. Mott Children's Hospital National Poll on Children's Health website. [Accessed October 2015]. http://mottnpch.org.
- 30.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Sources and perceived credibility of vaccine-safety information for parents. Pediatrics. 2011;127(Suppl 1):S107–S112. doi: 10.1542/peds.2010-1722P. [DOI] [PubMed] [Google Scholar]
- 31.Tarini BA, Singer D, Clark SJ, Davis MM. Parents' concern about their own and their children's genetic disease risk: potential effects of family history vs genetic test results. Arch Pediatr Adolesc Med. 2008;162(11):1079–1083. doi: 10.1001/archpedi.162.11.1079. [DOI] [PubMed] [Google Scholar]
- 32.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health. 2015;1(4):233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 33.Paruthi S, Brooks L, D'Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786. doi: 10.5664/jcsm.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Response Rates - An Overview. American Association for Public Opinion Research website. [Accessed May 8, 2017]. http://www.aapor.org/Education-Resources/For-Researchers/Poll-Survey-FAQ/Response-Rates-An-Overview.aspx.
- 35.Wahlstrom K, Wrobel G, Kubow P. Minneapolis Public Schools Start Time Study Executive Summary 1998. University of Minnesota Libraries Digital Conservancy website. [Accessed May 8, 2017]. https://conservancy.umn.edu/handle/11299/3902.
- 36.Minges KE, Redeker NS. Delayed school start times and adolescent sleep: a systematic review of the experimental evidence. Sleep Med Rev. 2015;28:86–95. doi: 10.1016/j.smrv.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Morgenthaler TI, Hashmi S, Croft JB, Dort L, Heald JL, Mullington J. High school start times and the impact on high school students: what we know, and what we hope to learn. J Clin Sleep Med. 2016;12(12):1681–1689. doi: 10.5664/jcsm.6358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wahistrom K. Changing times: findings from the first longitudinal study of later high school start times. NASSP Bulletin. 2002;86(633):3–21. [Google Scholar]
- 39.Wolfson AR, Spaulding NL, Dandrow C, Baroni EM. Middle school start times: the importance of a good night's sleep for young adolescents. Behav Sleep Med. 2007;5(3):194–209. doi: 10.1080/15402000701263809. [DOI] [PubMed] [Google Scholar]
- 40.Thacher PV, Onyper SV. Longitudinal outcomes of start time delay on sleep, behavior, and achievement in high school. Sleep. 2016;39(2):271–281. doi: 10.5665/sleep.5426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kirby M, Maggi S, D'Angiulli A. School start times and the sleep-wake cycle of adolescents: a review and critical evaluation of available evidence. Educ Res. 2011;40(2):56–61. [Google Scholar]
- 42.McDonald NC, Brown AL, Marchetti LM, Pedroso MS. U.S. school travel, 2009 an assessment of trends. Am J Prev Med. 2011;41(2):146–151. doi: 10.1016/j.amepre.2011.04.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.