Abstract
Study Objectives:
This study aimed to determine the associations between the self-reported sleep duration and self-rated health in young adults.
Methods:
In this cross-sectional study, participants were 689 young adults (mean age 20 ± 1.35 years, 49.8% female). Sleep duration and self-rated health, as the main outcome of interest, were measured as self-reported. As potential covariates, we included sex, age, smoking status, alcohol consumption, physical activity, sedentary behavior, psychological distress, and body mass index.
Results:
Approximately 30% of participants slept 7–8 hours, 17.4% were short sleepers (categories < 6 hours and 6–7 hours), and 53.9% were long sleepers (categories 8–10 hours and > 10 hours of sleep). In an unadjusted model, compared with the reference category (7–8 hours of sleep), those who slept < 6 hours (odds ratio 0.20; 95% confidence interval 0.08 to 0.48) and between 6–7 hours (odds ratio 0.43; 95% confidence interval 0.26 to 0.69) were less likely to have good self-rated health. In an adjusted model, short (< 7 hours) and long sleep (> 10 hours) were both associated with poor self-rated health.
Conclusions:
Our results suggest that both short (< 7 hours) and long (> 10 hours) sleepers have lower odds of having good self-rated health after adjusting for potential covariates. Health professionals should pay more attention to young adults, who have both short and long period of sleep, in order to prevent health problems and potential acute or chronic diseases.
Citation:
Štefan L, Juranko D, Prosoli R, Barić R, Sporiš G. Self-reported sleep duration and self-rated health in young adults. J Clin Sleep Med. 2017;13(7):899–904.
Keywords: gender, logistic regression, self-rated health, sleep duration, young adults
INTRODUCTION
Recently, sleep duration has become an important predictor for individuals' overall health.1 Several studies have shown that persons who sleep fewer than 7 hours or more than 8 hours have higher mortality rates than those who sleep 7–8 hours.2,3 Also, both short and long sleep are associated with metabolic4,5 and cardiovascular diseases.6–8
The associations between sleep duration and health status in adults (older than 18 years) and older adults (older than 65 years) has been investigated.9–15 In both populations, results have shown that both short and long sleep duration were associated with poor self-rated health independent of potential covariates. It is worthwhile to note that most of the aforementioned studies included a heterogeneous group of participants with a wide age range. However, little is known of how sleep duration influences on self-rated health in adolescents and young adults. To the best of our knowledge, only one study has analyzed the associations between the sleep duration and self-rated health in the sample of young adults. A retrospective observational study from Steptoe et al. showed that young adults, who slept < 6 hours and 6–7 hours were more likely to report poor self-rated health compared with those reporting 7–8 hours of sleep.16 Also, the authors found no significant association between self-rated health and long sleep duration.16 As highlighted in the study by Steptoe et al., it is not known whether similar patterns of short and long sleep duration may affect poor self-rated health in young adults.16
Thus, the main purpose of the current study was to investigate the associations between the sleep duration and self-rated health in a sample of young adults aged 17–24 years. We hypothesized that both short and long sleep duration would be associated with poor self-rated health after controlling for potential covariates.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep duration represents a key factor for physical and mental health, especially in young adults. Evidence suggests that only short sleep is known to affect poor self-rated health in young adults.
Study Impact: Our study shows that young adults reporting both short (< 7 hours) and long (> 10 hours) sleep duration have higher odds of having poor self-rated health. Special interventions and policies that leverage sleep duration might serve as an avenue for health promotion in young adults.
METHODS
Study Sample
In this cross-sectional study, a sample of 750 young adults were selected. Participants were recruited via flyers handed out in two faculties (Faculty of Kinesiology and Faculty of Economics and Business) from the urban area of the city of Zagreb, Croatia. This city is home to the University of Zagreb which is composed of 33 departments, and approximately 70,000 students attend the university. A recruitment announcement was also circulated by email and e-newsletter to university staff with a request to pass the study information to students. At the time the study was conducted, all participants resided in the urban part of the city of Zagreb, and no participants had any type of medical problems. Also, all participants were instructed that the study was voluntary and participants could withdraw at any time. A testing procedure was conducted from December 2016 to February 2017. Each participant was given specific instructions on how to complete the questionnaire. Questionnaires were administered in medium-sized groups of 25–30 people. Before the study began, parents or legal guardians had given their written informed consent for examinations and data collection for their children, whereas participants expressed oral consent. At the end, 50 participants did not want to participate in the study and 11 of them did not express their oral consent. The final sample consisted of 689 young adults (mean age 20 ± 1.35 years, 49.8% female, response rate 91.9%). There were no significant differences between the participants included in the study and those excluded from it. Basic descriptive statistics are presented in Table 1. All the procedures performed in this study were anonymous and in accordance with the Declaration of Helsinki, and also approved by the Institution Review Board of the first author.
Table 1.
Descriptive statistics of the study participants (n = 689).

Dependent Variable
To assess health status, we used one question: “How would you perceive your health status?” Responses were arranged along a five-point Likert-type scale: (1) very poor, (2) poor, (3) fair, (4) very good, and (5) excellent.17 We explained that health status referred to both physical and psychological health. For the purposes of this study, the responses “very poor” and “poor” represented poor self-rated health. “Fair,” “good,” and “excellent” represented good self-rated health. The question was translated from English to Croatian by two experienced and independent experts who were familiar with the question. Potential disagreements and differences in the process of translation were removed, and a third independent expert translated the question from Croatian back into English to determine the accuracy and quality of translation. Perceived health is an easily administrated and widely used outcome measure, especially in epidemiological studies, and serves as a valid predictor of mortality. This measure has been used in both adult18 and adolescent populations.19,20
Independent Variable
Sleep duration was assessed by one question: “On average, how many hours of sleep do you get in a 24-hour period?”16 The result was expressed as numerical value. For the purposes of this study, we categorized the results in 5 categories: (1) < 6 hours, (2) 6–7 hours, (3) 7–8 hours, (4) 8–10 hours and (5) > 10 hours, as proposed by one previous study.16 Previous studies have shown that self-reported sleep duration is moderately associated with actigraphy-assessed sleep duration,21,22 and this measure has often been used as a valid instrument to assess sleep duration in young adults.16,23
Covariates
Previous findings have shown that age, cigarette and alcohol consumption, body mass index, physical activity, and psychological distress are known factors that might influence both self-rated health and sleep duration.24–27 To assess physical activity, we used the International Physical Activity Questionnaire-short form. Previous findings have shown acceptable reliability and validity properties of the questionnaire.28 For the purposes of this study, we used World Health Organization recommendations, where (1) adults aged 18–64 years should do at least 150 minutes of moderate-intensity aerobic physical activity throughout the week, or (2) 75 minutes of vigorous-intensity aerobic physical activity throughout the week, or (3) an equivalent combination of moderate- and vigorous-intensity activity. Where participants did not satisfy the recommendations, we classified them as “insufficiently active.” Those who satisfied recommended guidelines were classified as “sufficiently active.”29
Body mass index was derived from the self-reported height and weight of the participants by using the formula: weight (kg) / height (m)2. The result was expressed as a continuous variable.
Smoking status was used as a potential covariate and assessed with two questions: “Do you currently smoke?” with “yes” and “no” answers and “On average, how many cigarettes do you usually smoke in one day?” expressed as a continuous variable. Also, alcohol consumption was used as a covariate and was assessed by two questions: “In the past week, did you consume an alcoholic drink?” with “yes” and “no” answers. The second question referred to the average number of alcoholic drinks consumed in the past week and was expressed as a continuous variable.
Sedentary behavior was assessed by using one question taken from the International Physical Activity Questionnaire: “In the last 7 days, how much time did you spend sitting on a weekday?”28 The responses were expressed in minutes per day. For the purposes of this study, we categorized the responses into 2 categories: (1) ≤ 4 hours and (2) > 4 hours.
We used the Kessler questionnaire to assess psychological distress in the past 30 days.30 The questionnaire is composed of 6 questions: (1) “How often did you feel nervous in the last 30 days?” (2) “How often did you feel hopeless in the last 30 days?” (3) “During the past 30 days, how often did you feel restless or fidgety?” (4) “During the last 30 days, how often did you feel so depressed that nothing could cheer you up?” (5) “During the last 30 days, how often did you feel that everything was an effort?” and (6) “During the last 30 days, how often did you feel worthless?”30 Each question is scored on a 5-point scale from 0 (none of the time) to 4 (all of the time). At the end, responses are summed up on a scale from 0–24, where a higher score indicates a higher level of psychological distress. Previous studies have shown that the categorization of responses in the range of 0–12 versus ≥ 13 identifies participants without and with psychological distress, respectively.30
Age was expressed as a continuous variable. For the purposes of this study, we entered body mass index, cigarette and alcohol consumption, and age as continuous variables into the multivariate model.
Data Analysis
Descriptive results are presented as frequencies (n) and percentages. Differences between men and women in all variables were calculated by using chi-square test. The associations between sleep duration and self-rated health were analyzed by using logistic regression analysis. We calculated odds ratio (OR) with 95% confidence intervals (CI) for each association. In model 1, we calculated the association between the sleep duration categories and self-rated health. In model 2, we calculated the associations between the sleep duration categories and self-rated health while adjusting for physical activity, smoking and alcohol consumption, sedentary behavior, body mass index, psychological distress, sex, and age. In both models, our referent value for sleep duration category was 7–8 hours of sleep.16 All the analysis performed in this study were analyzed in SPSS version 23 (Statistical Package for Social Sciences, Chicago, Illinois, United States). Significance was set at α < 0.05 (two-sided).
RESULTS
Basic descriptive statistics of the study participants are presented in Table 1. Approximately 17% of all participants slept fewer than 7 hours per night, whereas most of the participants (74%) slept between 7–10 hours. A lower percentage of women than men slept fewer than 7 hours. Also, almost 73% of the participants had good self-rated health. A lower number of men than women perceived their health status as good (65% versus 80.3%). More than 30% of all participants are current smokers, with an average number of 2.20 cigarettes smoked per day. Approximately 70% of participants consumed alcohol in the past week, with an average number of 3.78 alcoholic drinks. A higher percentage of women than men smoked or consumed alcohol.
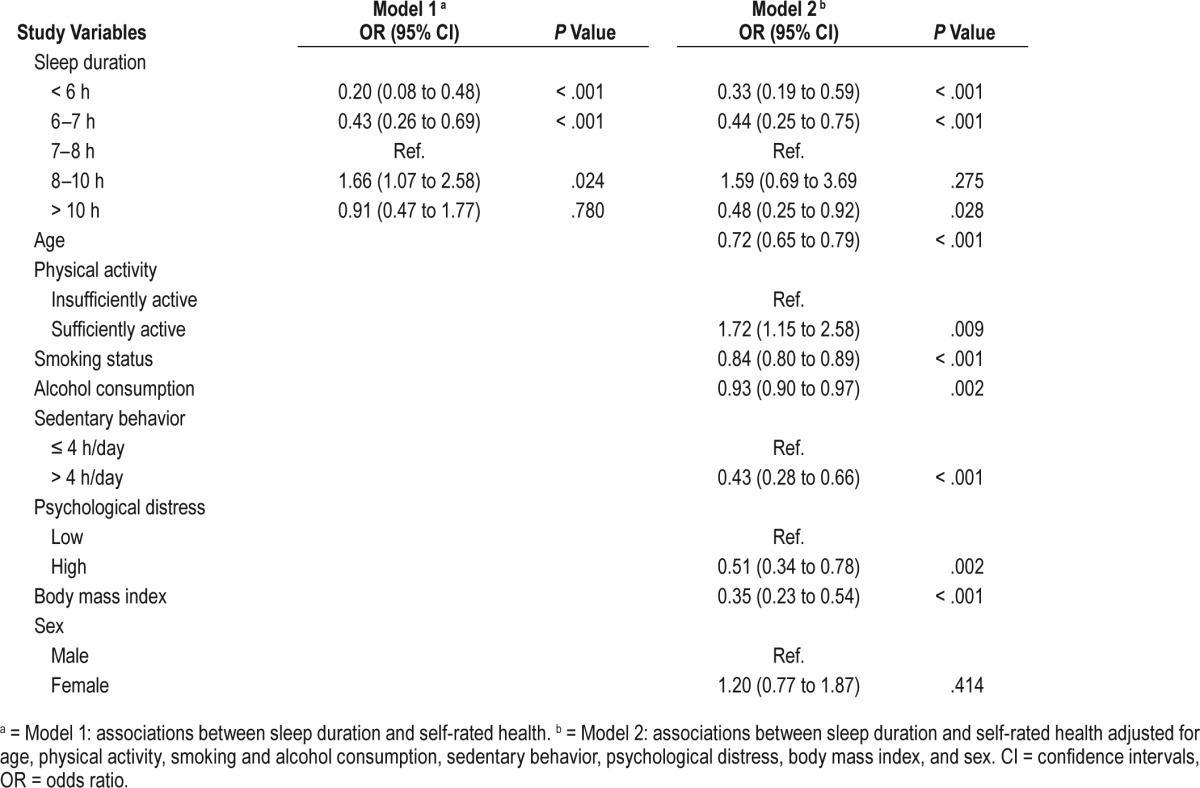
The associations between the self-reported sleep duration categories and self-rated health are presented in Table 2. Overall, sleeping < 6 hours (OR 0.20; 95% CI 0.08 to 0.48) and 6–7 hours (OR 0.43; 95% CI 0.26 to 0.69) were both associated with poor self-rated health. Interestingly, sleeping 8–10 hours was associated with good self-rated health (OR 1.66; 95% CI 1.07 to 2.58). However, no association was found between sleeping ≥ 10 hours and self-rated health (OR 0.91; 95% CI 0.47 to 1.77). In the second model adjusted for age, physical activity, smoking and alcohol consumption, sedentary behavior, body mass index, psychological distress, and sex, sleeping < 6 hours (OR 0.33; 95% CI 0.19 to 0.59), between 6–7 hours (OR 0.44; 95% CI 0.25 to 0.75), and > 10 hours (OR 0.48; 95% CI 0.25 to 0.92) were associated with poor self-rated health. Sleep duration between 8–10 hours was not significantly associated with good self-rated health in the multivariate model (OR 1.59; 95% CI 0.69 to 3.69).
Table 2.
Odds ratios for good self-rated health of the study participants (n = 689).
DISCUSSION
The main purpose of the current study was to determine the associations between sleep duration and self-rated health in young adults adjusted for potential covariates.
Our results showed that short sleep duration (< 7 hours) was associated with poor self-rated health. Previous findings have shown the same associations in the population of adults9,12,14 and older adults.10 It has been previously established that short sleep duration is associated with increased rates of mortality,2,3 diabetes,4,5 and cardiovascular diseases.6–8 A study from Step-toe et al. showed the same results, where sleeping < 6 hours and 6–7 hours was associated with poor self-rated health.16 Short sleep duration is associated with increased daytime fatigue,31 impaired mood and cognitive functioning,10 and adverse physiological changes.2–8 Also, individuals with poorer self-rated health could be more likely to experience disturbed and short sleep or are less accurate in estimating their sleep duration.10 Findings from one recent study conducted with United States adolescents have shown that sleep duration has decreased over the past 20 years,32 which may be attributed to increased demands of school, faculty obligations, extracurricular activities,33 and social media.34
Next, results from the univariate model showed positive association between self-rated health and sleeping 8–10 hours. The National Sleep Foundation recommends 8–10 hours of sleep per night for adolescents and young adults in order to maximize overall health and well-being.35 Also, both longitudinal and cross-sectional studies conducted with children and adolescents have reported that longer sleep duration is associated with better emotional regulation.36–38 Moreover, one previous study has shown that increased levels of total sleep predict a lower likelihood of past-month cigarette and marijuana use at 2-year follow-up.37 The authors concluded that developing good sleeping habits in childhood and adolescence may keep youth away from engaging in substance use and misuse. In clinical practice, more detailed information on sleep behavior may serve as a screening tool for substance use among youth.37 In general, long sleep duration cannot be assessed as a risk factor or independent factor without taking into account other potential covariates, such as mental or sleeping problems.39 Positive association between sleeping 8–10 hours and self-rated health may be explained by the fact that children and youth often sleep longer than other age groups.16 This is an indicator that sleeping more than the recommended 7–8 hours is not a sign of pathology.40
Results from our study showed that long sleep duration (> 10 hours of sleep) was associated with poor self-rated health. Studies conducted on adults and older adults have shown the same associations.9–15 However, a study from Step-toe et al. showed no significant association between self-rated health and long sleep duration (> 10 hours).16 The authors explained that the absence of association was not a consequence of using self-rated health as the dependent variable, because their findings showed clear associations between short sleep duration and poor self-rated health. The presence of the association in our study might be explained by the fact that we used a more homogenous sample (aged between 17–24 years). Also, we included a sample of participants from 2 departments and our results cannot be generated in other young adults attending different departments and studying for professions that are probably more stressful, such as a medical doctor. Moreover, we obtained the data from December 2016 to February 2017. In Croatia the schedule of midterm examinations starts in January/February. Previous findings have reported that potential covariates that might influence poor mental health are academic overload, stressful way of life, pressure to succeed, competition, and uncertainty about the future.41,42 It is possible that because of the examinations and studying period, students in our study experienced more emotional and behavioral problems and were dealing with a large amount of stress. Because psychological distress is associated with long sleep duration,23 a midterm examination schedule might serve as a stressful mediator between long sleep duration and mental health problems. Studies from Kim et al. and Shankar et al. showed a U-shaped association between the sleep duration and self-rated health; that is, both short and long sleep duration were associated with poor self-rated health in general population.9,13 As stated before, long sleep duration may be a marker of undiag-nosed medical conditions that may affect subjective health,13 such as sleep apnea.43
Our study has several limitations. First, because of a cross-sectional design, we cannot exclude the possibility of reverse causality; that is, poor self-rated health led to a short sleep duration in our sample. However, we adjusted for psychological distress, where participants with higher psychological distress would report short sleep duration and psychological distress could affect their self-rated health. Second, we used a subjective measure to assess sleep duration and self-rated health. Future studies should include objective measures for assessing sleep.44 Third, we selected a sample of students from 2 departments. Unfortunately, we cannot generalize our results to the entire population of young adults, because we did not take into account students from other departments and studying for different professions. Fourth, we did not adjust for potential sleeping problems (eg, sleep apnea), because one previous study showed that long sleep duration cannot be assessed as a risk factor or independent factor without taking into account other potential covariates such as mental or sleeping problems.39
In conclusion, we found that both short (< 7 hours) and long (> 10 hours) sleep duration were associated with poor self-rated health after adjusting for numerous covariates compared to 7–8 hours of sleep (referent value). To the best of our knowledge, this is the first study that shows the association between the both short and long sleep duration and self-rated health in young adults. Health professionals should pay more attention to young adults who have both short and long periods of sleep in order to prevent health problems and potential acute or chronic diseases. Also, special interventions and policies that leverage sleep duration might serve as an avenue for health promotion in young adults.
DISCLOSURE STATEMENT
Work for this study was performed at the Faculty of Kinesiology, University of Zagreb, Croatia. All authors have approved the final version of the manuscript. This work was self-funded and the authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- CI
confidence intervals
- OR
odds ratio
REFERENCES
- 1.Frange C, Souza de Queiroz S, Martuscelli da Silva Prado J, Tufik S, Túlio de Mello M. The impact of sleep duration on self-rated health. Sleep Sci. 2014;7(2):107–113. doi: 10.1016/j.slsci.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tamakoshi A, Ohno Y JACC Study Group. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27(1):51–54. [PubMed] [Google Scholar]
- 3.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marier MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(4):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 4.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29(3):657–661. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 5.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes. Diabetes Care. 2010;33(2):414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep. 2010;33(8):1037–1042. doi: 10.1093/sleep/33.8.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 8.Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: the effect of short and long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3(4):305–314. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 9.Kim JH, Ran Kim K, Hee Cho K, Yo KB, Kwon JA, Park EC. The association between sleep duration and self-rated health in the Korean general population. J Clin Sleep Med. 2013;9(10):1057–1064. doi: 10.5664/jcsm.3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged elderly Australians. Sleep Med. 2011;12(4):346–350. doi: 10.1016/j.sleep.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Kakizaki M, Kuriyama S, Nakaya N, et al. Long sleep duration and cause-specific mortality according to physical function and self-rated heath: the Ohsaki Cohort Study. J Sleep Res. 2013;22(2):209–216. doi: 10.1111/j.1365-2869.2012.01053.x. [DOI] [PubMed] [Google Scholar]
- 12.Silva-Costa A, Härter Griep R, Rotemberg L. Associations of a short sleep duration, insufficient sleep, and insomnia with self-rated health among nurses. Plos One. 2015;10(5):e0126844. doi: 10.1371/journal.pone.0126844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shankar A, Charumathi S, Kalidindi S. Sleep duration and self-rated health: the National Health Interview Survey 2008. Sleep. 2011;34(9):1173–1177. doi: 10.5665/SLEEP.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geiger SD, Sabanayagam C, Shankar A. The relationship between insufficient sleep and self-rated health in a nationally representative sample. J Environ Public Health. 2012;2012:518263. doi: 10.1155/2012/518263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Segovia J, Bartlett RF, Edwards AC. The association between self-assessed health status and individual health practices. Can J Public Health. 1989;80(1):32–37. [PubMed] [Google Scholar]
- 16.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166(16):1689–1692. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 17.Eriksson I, Undén AL, Elofsson S. Self-rated health. Comparisons between three different measures. Results from a population study. Int J Epidemiol. 2001;30(2):326–333. doi: 10.1093/ije/30.2.326. [DOI] [PubMed] [Google Scholar]
- 18.Idler ED, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 19.Johnson PB, Richter L. The relationship between smoking, drinking, and adolescents' self-perceived health and frequency of hospitalization: analyses from the 1997 National Household Survey on Drug Abuse. J Adolesc Health. 2002;30(3):175–183. doi: 10.1016/s1054-139x(01)00317-2. [DOI] [PubMed] [Google Scholar]
- 20.Larsson D, Hemmingsson T, Allebeck P, Lundberg I. Self-rated health and mortality among young men: what is the relation and how may it be explained? Scand J Public Health. 2002;30(4):259–266. doi: 10.1080/14034940210133997. [DOI] [PubMed] [Google Scholar]
- 21.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Sleep duration: how well do self-reports reflect objective measures? The CARDIA Sleep Study. Epidemiology. 2008;19(6):838–845. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biddle DJ, Robillard R, Hermens DF, Hickie IB, Glozier N. Accuracy of self-reported sleep parameters compared with actigraphy in young people with mental ill-health. Sleep Health. 2015;1(3):214–220. doi: 10.1016/j.sleh.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Glozier N, Martiniuk A, Patton G, et al. Short sleep duration in prevalent and persistent psychological distress in young adults: the DRIVE study. Sleep. 2010;33(9):1139–1145. doi: 10.1093/sleep/33.9.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hale L. Who has time to sleep? J Public Health (Oxf) 2005;27(2):205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- 25.Strine TW, Okoro CA, Chapman DP, et al. Health-related quality of life and health risk behaviors among smokers. Am J Prev Med. 2005;28(2):182–187. doi: 10.1016/j.amepre.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analysis of the NHANES I. Sleep. 2005;28(10):1289–1296. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 27.Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A. Excessive day-time sleppiness in a general population sample: the role of sleep apnea, age, obesity, diabetes and depression. J Clin Endocrinol Metab. 2005;90(8):4510–4515. doi: 10.1210/jc.2005-0035. [DOI] [PubMed] [Google Scholar]
- 28.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization. Global Recommendations on Physical Activity for Health. Geneva, Switzerland: WHO Press; 2010. [PubMed] [Google Scholar]
- 30.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 31.Van Dongen HP, Vitellaro KM, Dinges DF. Individual differences in adult human sleep and wakefulness: leitmotif for a research agenda. Sleep. 2005;28(4):479–496. doi: 10.1093/sleep/28.4.479. [DOI] [PubMed] [Google Scholar]
- 32.Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. Pediatrics. 2015;135(3):460–468. doi: 10.1542/peds.2014-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med. 2010;11(8):735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 34.Peiró-Velert C, Valencia-Peris A, González LM, García-Massó X, Serra-Añó P, Devís-Devís J. Screen media usage, sleep time and academic performance in adolescents: clustering a self-organizing maps analysis. Plos One. 2014;9(6):e99478. doi: 10.1371/journal.pone.0099478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 36.Barlett ND, Gentile DA, Barlett CP, Eisenmann JC, Walsh DA. Sleep as a mediator of screen time effects on US children's health outcomes: a prospective study. J Child Media. 2012;6(1):37–50. [Google Scholar]
- 37.Pasch KE, Latimer KA, Cance JD, Moe SG, Lytle LA. Longitudinal bi-directional relationships between sleep and youth substance use. J Youth Adolesc. 2012;41(9):1184–1196. doi: 10.1007/s10964-012-9784-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnes JC, Meldrum RC. The impact of sleep duration on adolescent development: a genetically informed analysis of identical twin pairs. J Youth Adolesc. 2015;44(2):489–506. doi: 10.1007/s10964-014-0137-4. [DOI] [PubMed] [Google Scholar]
- 39.Stamatakis KA, Punjabi NM. Long sleep duration: a risk to health or a marker of risk? Sleep Med Rev. 2007;11(5):337–339. doi: 10.1016/j.smrv.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Floyd JA, Medier SM, Ager JW, Janisse JJ. Age-related changes in initiation and maintenance of sleep: a meta-analysis. Res Nurs Health. 2000;23(2):106–117. doi: 10.1002/(sici)1098-240x(200004)23:2<106::aid-nur3>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 41.Tosevski D, Milovancevic M, Gajic S. Personality and psychopathology of university students. Curr Opin Psychiatry. 2010;23(1):48–52. doi: 10.1097/YCO.0b013e328333d625. [DOI] [PubMed] [Google Scholar]
- 42.Li H, Lin CD, Bray MA, Kehle TJ. The measurement of stressful events in chinese college students. Psychol Sch. 2005;42(3):315–323. [Google Scholar]
- 43.Al Lawati NM, Patel SR, Ayas NT. Epidemiology, risk factors, and consequences of obstructive sleep apnea and short sleep duration. Prog Cardiovasc Dis. 2009;51(4):285–293. doi: 10.1016/j.pcad.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 44.Sorić M, Turkalj M, Kučić D, Marušić I, Plavec D, Mišigoj-Duraković M. Validation of a multi-sensor activity monitor for assessing sleep in children and adolescents. Sleep Med. 2013;14(2):201–205. doi: 10.1016/j.sleep.2012.11.003. [DOI] [PubMed] [Google Scholar]


