Abstract
Background:
Timely coordinated diagnostic assessment following an abnormal screening mammogram reduces patient anxiety and may optimise breast cancer prognosis. Since 1998, the Ontario Breast Screening Program (OBSP) has offered organised assessment through Breast Assessment Centres (BACs). For OBSP women seen at a BAC, an abnormal mammogram is followed by coordinated referrals through the use of navigators for further imaging, biopsy, and surgical consultation as indicated. For OBSP women seen through usual care (UC), further diagnostic imaging is arranged directly from the screening centre and/or through their physician; results must be communicated to the physician who is then responsible for arranging any necessary biopsy and/or surgical consultation. This study aims to evaluate factors associated with diagnostic wait times for women undergoing assessment through BAC and UC.
Methods:
Of the 2 147 257 women aged 50–69 years screened in the OBSP between 1 January 2002 and 31 December 2009, 155 866 (7.3%) had an abnormal mammogram. A retrospective design identified two concurrent cohorts of women diagnosed with screen-detected breast cancer at a BAC (n=4217; 47%) and UC (n=4827; 53%). Multivariable logistic regression analyses examined associations between wait times and assessment and prognostic characteristics by pathway. A two-sided 5% significance level was used.
Results:
Screened women with breast cancer were two times more likely to be diagnosed within 7 weeks when assessed through a BAC vs UC (OR=1.91, 95% CI=1.73–2.10). In addition, compared with UC, women assessed through a BAC were significantly more likely to have their first assessment procedure within 3 weeks of their abnormal mammogram (OR=1.25, 95% CI=1.12–1.39), ⩽3 assessment procedures (OR=1.54, 95% CI=1.41–1.69), ⩽2 assessment visits (OR=1.86, 95% CI=1.70–2.05), and ⩾2 procedures per visit (OR=1.41, 95% CI=1.28–1.55). Women diagnosed through a BAC were also more likely than those in UC to have imaging (OR=1.99, 95% CI=1.44–2.75) or a biopsy (OR=3.69, 95% CI=2.64–5.15) vs consultation only at their first assessment visit, and two times more likely to have a core or FNA biopsy than a surgical biopsy (OR=2.08, 95% CI=1.81–2.40). Having ⩽2 assessment visits was more likely to reduce time to diagnosis for women assessed through a BAC compared with UC (BAC OR=10.58, 95% CI=8.96–12.50; UC OR=4.47, 95% CI=3.94–5.07), as was having ⩽3 assessment procedures (BAC OR=4.97, 95% CI=4.26–5.79; UC OR=2.95, 95% CI=2.61–3.33). Income quintile affected wait times only in women diagnosed in UC, with those in the two highest quintiles more likely to receive a diagnosis in 7 weeks.
Conclusions:
Women with screen-detected breast cancer in OBSP were more likely to have shorter wait times if they were diagnosed through organised assessment. This might be as a result of women diagnosed through a BAC having more procedures per visit, procedures scheduled in shorter intervals, and imaging or biopsy on their first visit. Given the significant improvement in timeliness to diagnosis, women with abnormal mammograms should be managed through organised assessment.
Keywords: breast cancer, breast screening, breast assessment, wait times to diagnosis, breast assessment procedures, early detection
To ensure the benefits of early detection by mammography (The Canadian Task Force on Preventive Health Care, 2011; Nelson et al, 2016) women with abnormal screening results must have access to timely and accurate diagnostic assessment. One of the essential components of screening centres is appropriate follow-up of women with abnormal findings with an effective referral system (The Workshop Group, 1989). The time required for assessment of an abnormal mammogram is associated with patient stress and anxiety (Sutton et al, 1995; Rimer and Bluman, 1997; Brett et al, 1998) and delays in diagnostic times have a negative impact on the prognosis of screen-detected breast cancers (Olivotto et al, 2002; Ganry et al, 2004).
A study of Canadian screening programs found that age at screen, family history of breast cancer, and screening history were not associated with delays in breast cancer diagnosis (Olivotto et al, 2002). However, this study as well as several others found that diagnostic intervals actually decreased for screened women with high-suspicion mammograms (Caplan et al, 2000; Olivotto et al, 2002; Ganry et al, 2004; Bairati et al, 2007; Borugian et al, 2008). Shorter diagnostic times were also seen for women with higher income (Bairati et al, 2007), larger tumour size (Bairati et al, 2007), more advanced stage (Jiang et al, 2015), and for women who attended screening programs that used core biopsies more often than open biopsies (Olivotto et al, 2001a).
The Ontario Breast Assessment Collaborative Group was established in 1998 to guide development of coordinated multidisciplinary approaches for facilities to provide organised breast assessment (Ontario Breast Screening Program, 2001). Within the Ontario Breast Screening Program (OBSP), facilities that qualify as a Breast Assessment Centre (BAC) have a patient navigation system that coordinates referrals through a defined pathway and have access to diagnostic imaging, image-guided biopsies, pathology, and surgical services. Canadian breast screening programs have reported shorter diagnostic intervals for women who had coordinated referrals from screening centres to diagnostic facilities (Olivotto et al, 2001b; Decker et al, 2004; Psooy et al, 2004; Borugian et al, 2008; Baliski et al, 2014). For women screened in the OBSP, a previous study showed that women receiving work-up through organised assessment had shorter diagnostic wait times with a biopsy than for those evaluated through usual care (UC) (Quan et al, 2012). However, this study only utilised 1 year of data, and did not explore the effect of various assessment and prognostic characteristics on diagnostic intervals. A more recent Ontario study of screened women had similar findings; however, a large proportion (20.5%) underwent opportunistic screening and only invasive cancers were included (Jiang et al, 2015).
After 15 years of implementation of BACs in the OBSP, this study aims to evaluate the effectiveness of organised breast assessment. Wait times from an abnormal mammogram to breast cancer diagnosis will be compared between concurrent cohorts of women aged 50–69 years screened in the OBSP undergoing assessment through BAC and UC. The association of assessment and prognostic characteristics with wait times will be examined separately in BAC and UC cohorts.
Materials and methods
Study population
The OBSP has operated since 1990 to deliver a population-based breast screening program to eligible women (Chiarelli et al, 2013). Women are not eligible if they have had a prior history of breast cancer, an augmentation mammoplasty, or if they currently have acute breast symptoms. This study identified women aged 50–69 years screened through the OBSP with an abnormal mammogram between 1 January 2002 and 31 December 2009. Mammography consisted of standard craniocaudal and mediolateral oblique views performed by certified mammography technologists on equipment that meets or exceeds that specified by Canadian Association of Radiologists’ Mammography Accreditation Program (CAR-MAP). Of those with an abnormal mammogram, one cohort underwent diagnostic assessment through a BAC and the other through UC. Although all women in the study were screened at an OBSP centre, referral to a BAC was dependent on whether the screening centre was affiliated with a BAC. Women were then followed prospectively to determine whether there was a breast cancer diagnosis within a year of the abnormal screening mammogram. During the time period of this study, women were screened at 150 OBSP centres and assessed at 35 BACs. The study was approved by the University of Toronto Research Ethics Board and informed consent was not required.
Ontario facilities that provide organised assessment must meet established criteria in order to qualify as a BAC. Criteria include: having certified mammography technologists and equipment that meets or exceeds that specified by CAR-MAP; providing all abnormal mammographic work-up including special mammographic views and image-guided core biopsy; providing radiological, surgical, and pathologic consultation with experts in breast evaluation; and providing a navigator for patient support and coordination of referrals. The BACs may either perform all the required services for abnormal mammographic work-up or establish networks with facilities to provide the services (Quan et al, 2012). For OBSP women seen through UC, further diagnostic imaging after an abnormal mammogram is arranged directly from the screening centre and/or through their physician; results must be communicated to the physician who is then responsible for arranging any necessary biopsy and/or surgical consultation.
Selection of breast cancer cases
There were 2 147 257 women aged 50–69 years screened at an OBSP centre between 1 January 2002 and 31 December 2009. To allow for learning curves for new BACs, only women with an abnormal mammogram assessed after the first 6 months of operation were selected. All women diagnosed with unilateral, primary ductal carcinoma in situ (DCIS), or invasive breast cancer of any histological type were identified through record linkage with the Ontario Cancer Registry (OCR) (Jaro, 1995). Breast cancers detected within 12 months of the abnormal screening episode and classified as screen-detected by the program during follow-up were included. For these women, the last OBSP abnormal screening mammogram before diagnosis was included. Information for all women screened within the OBSP was obtained from data routinely collected by the Integrated Client Management System (ICMS) and OCR.
Demographics and breast cancer risk factors
Information on demographics and breast cancer risk factors comprises self-reported data in the ICMS, collected at the screening appointment. Age and year at screen were based on the date of abnormal mammogram before diagnosis. Women with a first-degree relative with breast or ovarian cancer or personal history of ovarian cancer were classified as having a positive family history. Menopausal status (premenopausal, postmenopausal), age at menarche (⩽11 years, >11 years), and parity (nulliparous; first full-term pregnancy (FFTP) <30 years; FTTP ⩾30) were also measured. Women’s postal code of residence at screening was linked to the 2006 Canadian Census (Wilkins, 1998) to determine socioeconomic status (SES) and community status. The SES was defined by five income quintiles (Q1 (low)–Q5 (high)). Community status included urban (population 10 000+), rural (<10 000 and a strong metropolitan influenced zone (MIZ)), rural remote (<10 000 and a moderate MIZ), and rural very remote (<10 000 and a weak/no MIZ) (Statistics Canada, 1997).
Screening characteristics
Information on screening visit for each woman was obtained through the ICMS. An abnormal mammogram was defined as an initial screen for women who had only one OBSP mammogram, or a rescreen for women who had more than one mammogram. The type of mammography was recorded as screen film or digital. Mammographic density was recorded by the radiologist as <75% or ⩾75%.
Assessment characteristics
Assessment procedures and dates were obtained through ICMS. Time (days) to a woman’s first assessment procedure following an abnormal screening mammogram was calculated. Assessment procedures from abnormal screening mammogram to final diagnosis date included breast imaging (diagnostic mammogram, ultrasound, MRI), breast biopsy (fine-needle aspiration (FNA), core biopsy, open/surgical), and consultation (radiological, surgical, oncology, primary care). Procedures at first visit were categorised hierarchically as consultation only; imaging±consultation (i.e., imaging only, imaging with consultation); and biopsy±consultation or imaging (i.e., biopsy only; biopsy and consultation, biopsy and imaging, biopsy with imaging and consultation). First diagnostic assessment delay was defined as having a first assessment >3 weeks following an abnormal mammogram (Canadian Breast Cancer Screening Initiative Working Group, 2000). Number of assessment procedures, number of assessment visits, and average number of procedures per visit were calculated and categorised according to the median. Type of biopsy was defined as the woman’s first biopsy procedure after abnormal mammogram and was either percutaneous (FNA, core biopsies) or surgical (open surgical, nodal/axillary, nodal/sentinel, or treatment surgery).
Diagnosis age refers to the age at screen-detected breast cancer diagnosis. Time (days) to breast cancer diagnosis was calculated from the date of the abnormal screening mammogram to the date of the first biopsy indicating malignancy. Diagnostic delay was defined as having a breast cancer diagnosis >7 weeks after an abnormal screening mammogram, a national timeliness target based on expert opinion and evidence review (Canadian Breast Cancer Screening Initiative Working Group, 2000; Canadian Partnership against Cancer, 2013).
Prognostic characteristics
Histological classification (invasive, DCIS) for breast cancers was obtained from the ICMS and OCR. Tumour morphology was coded using the International Classification of Diseases for Oncology (ICD-O), Second Edition, 1990 (World Health Organization, 1990). Data on tumour size (⩽0.5; >0.5 to ⩽1.0; >1.0 to ⩽2.0; >2.0), nodal status (positive, negative), and stage (I, II, III) were collected for invasive cases. The TNM classification scheme (American Joint Committee on Cancer, 2002) was used for staging of breast cancer. Tumour size was defined as the largest diameter of the invasive carcinoma. Lymph node status was defined by TNM criteria for women who had axillary assessment.
Statistical analysis
Risk factors and screening characteristics were compared between BAC and UC using multivariable logistic regression analyses, adjusted for age and/or year of screening. Similarly, the association of pathway (BAC/UC) with assessment and prognostic characteristics was examined using multivariable logistic regression to estimate adjusted odds ratios (ORs) and corresponding 95% confidence intervals (CIs) (Diggle et al, 2002). The association of risk, screening, assessment, and prognostic characteristics with delay in diagnosis (⩽7 weeks vs >7 weeks) was examined separately for women assessed through BAC and UC to identify possible effect modification. Additional analyses examined stage and tumour size as quantitative exposure variables to assess trend effects. Wilcoxon rank-sum tests were used to test for differences in median time to diagnosis between pathways, overall and stratified by ⩽3 and >3 procedures (Haynes, 2013). Finally, sensitivity analyses were performed on a subset of the cohort screened between 2006 and 2009 to examine whether differences between pathways persisted over time. All analyses were performed using SAS version 9.4 (SAS Institute Inc., 2008). Statistical tests were two sided and evaluated at a 5% significance level.
Results
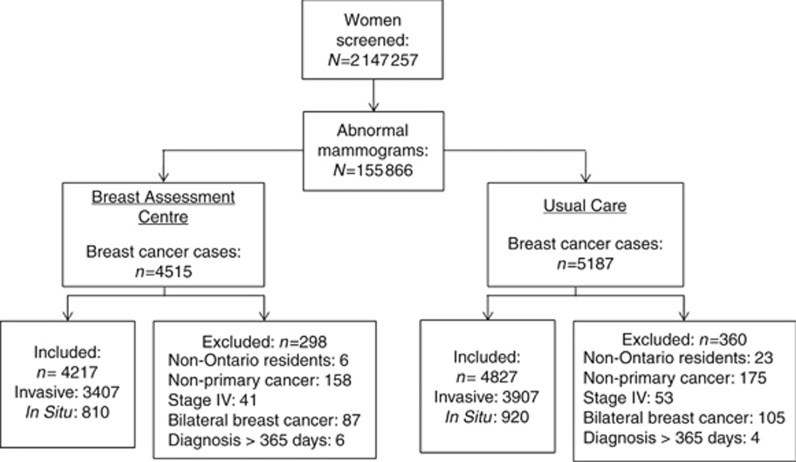
Of the 155 866 women with an abnormal mammogram, 9702 (6.2%) were diagnosed with breast cancer. Women were excluded if they resided outside Ontario (n=29), had stage IV (n=94), bilateral (n=192) or non-primary (n=333) breast cancer, or had a breast cancer diagnosis >1 year following an abnormal mammogram (n=10). The final sample included 9044 (93.2%) eligible women, of whom 4217 (47%) were assessed through a BAC and 4827 (53%) through UC (Figure 1).
Figure 1.
Cohorts of women screened between 1 January 2002 and 31 December 2009 and diagnosed with breast cancer within the Ontario Breast Screening Program.
The mean age at screening was 59.7 years, with no significant differences in age group distribution between pathways (Table 1). Women evaluated in a BAC compared with UC were more likely to have their abnormal mammogram be a rescreen than an initial screen, have their abnormal mammogram after 2006 than before, and be assessed with digital rather than screen-film mammography. Family history of breast or ovarian cancer, menopausal status, and age at menarche did not differ between pathways. Women assessed through a BAC were less likely to be parous vs nulliparous regardless of age, and were significantly more likely to have less mammographically dense breasts (<75% vs ⩾75%) compared with UC. In addition, women assessed through a BAC were twice as likely to live in rural remote compared with urban regions, and less likely to be in the highest compared with lowest income quintile.
Table 1. Adjusted ORs and 95% CIs for the association of risk factors and screening characteristics among women diagnosed with screen-detected breast cancers through a Breast Assessment Centre compared with Usual Care.
| Breast assessment type | |||||
|---|---|---|---|---|---|
| Characteristics | Usual Care, N=4827, n (%) | Breast Assessment Centre, N=4217, n (%) | Overall, N=9044, n (%) | Adjusted OR (95% CI) | P-value |
|
Age at screening (years)a | |||||
| 50–59 | 2335 (48.4) | 2045 (48.5) | 4380 (48.4) | 1.00 (reference) | |
| 60–69 | 2492 (51.6) | 2172 (51.5) | 4664 (51.6) | 0.98 (0.90–1.06) | 0.6170 |
|
Screen typeb | |||||
| Initial | 1859 (38.5) | 1230 (29.2) | 3089 (34.2) | 1.00 (reference) | |
| Rescreen | 2968 (61.5) | 2987 (70.8) | 5955 (65.8) | 1.55 (1.41–1.70) | <0.0001 |
|
Period of screeningc | |||||
| 2002–2005 | 2060 (42.7) | 1364 (32.3) | 3424 (37.9) | 1.00 (reference) | |
| 2006–2009 | 2767 (57.3) | 2853 (67.7) | 5620 (62.1) | 1.56 (1.43–1.70) | <0.0001 |
|
Mammography typeb | |||||
| Screen film | 4315 (89.4) | 3325 (78.9) | 7640 (84.5) | 1.00 (reference) | |
| Digital | 512 (10.6) | 892 (21.1) | 1404 (15.5) | 1.89 (1.66–2.15) | <0.0001 |
|
Family history of breast or ovarian cancerb | |||||
| No | 3799 (78.7) | 3251 (77.1) | 7050 (78.0) | 1.00 (reference) | |
| Yes | 1028 (21.3) | 966 (22.9) | 1994 (22.0) | 1.09 (0.98–1.20) | 0.1002 |
|
Menopausal statusb | |||||
| Premenopausal | 709 (14.7) | 608 (14.4) | 1317 (14.6) | 1.00 (reference) | |
| Postmenopausal | 4117 (85.3) | 3609 (85.6) | 7726 (85.4) | 1.00 (0.88–1.14) | 0.9949 |
| Missing | 1 | 0 | 1 | – | |
|
Age at menarche (years) b | |||||
| ⩽11 | 874 (18.8) | 814 (20.0) | 1688 (19.3) | 1.00 (reference) | |
| >11 | 3786 (81.2) | 3261 (80.0) | 7047 (80.7) | 0.92 (0.82–1.02) | 0.1170 |
| Missing | 167 | 142 | 309 | – | |
|
Parityb | |||||
| Nulliparous | 70 (1.7) | 91 (2.5) | 161 (2.1) | 1.00 (reference) | |
| Age at FFTP <30 | 3481 (83.5) | 3056 (83.7) | 6537 (83.6) | 0.70 (0.51–0.96) | 0.0270 |
| Age at FFTP ⩾30 | 617 (14.8) | 503 (13.8) | 1120 (14.3) | 0.63 (0.45–0.88) | 0.0066 |
| Missing | 659 | 567 | 1226 | – | |
|
Mammographic density (%)b | |||||
| ⩾75% | 456 (9.4) | 311 (7.4) | 767 (8.5) | 1.00 (reference) | |
| <75% | 4371 (90.6) | 3906 (92.6) | 8277 (91.5) | 1.34 (1.15–1.56) | 0.0002 |
|
Community statusb | |||||
| Urban | 4117 (85.3) | 3477 (82.5) | 7594 (84.0) | 1.00 (reference) | |
| Rural | 297 (6.2) | 214 (5.1) | 511 (5.6) | 0.87 (0.73–1.05) | 0.1491 |
| Rural remote | 234 (4.8) | 406 (9.6) | 640 (7.1) | 2.13 (1.80–2.52) | <0.0001 |
| Rural very remote | 177 (3.7) | 119 (2.8) | 296 (3.3) | 0.80 (0.63–1.02) | 0.0711 |
| Missing | 2 | 1 | 3 | ||
|
Income quintileb | |||||
| 1, Lowest | 771 (16.1) | 735 (17.5) | 1506 (16.7) | 1.00 (reference) | |
| 2 | 912 (19.0) | 842 (20.1) | 1754 (19.5) | 0.96 (0.84–1.10) | 0.5626 |
| 3 | 934 (19.4) | 804 (19.1) | 1738 (19.3) | 0.90 (0.78–1.03) | 0.1216 |
| 4 | 988 (20.6) | 848 (20.2) | 1836 (20.4) | 0.88 (0.77–1.01) | 0.0691 |
| 5, Highest | 1195 (24.9) | 970 (23.1) | 2165 (24.1) | 0.85 (0.74–0.97) | 0.0132 |
| Missing | 27 | 18 | 45 | – | |
Abbreviations: CI=confidence interval; FTTP=first full-term pregnancy; OR=odds ratio.
Adjusted by year of screen.
Adjusted by year of screen and age at screening.
Adjusted by age at screening.
Compared with women assessed through UC, those assessed through a BAC were significantly more likely to have their first assessment procedure within 3 weeks of their abnormal mammogram (vs >3; OR=1.25, 95% CI=1.12–1.39), ⩽3 assessment procedures (vs >3; OR=1.54, 95% CI=1.41–1.69), ⩽2 assessment visits (vs >2; OR=1.86, 95% CI=1.70–2.05), and ⩾2 procedures per visit (vs <2; OR=1.41, 95% CI=1.28–1.55) (Table 2). In addition, women assessed through a BAC were more likely than those in UC to have imaging (OR=1.99, 95% CI=1.44–2.75) or a biopsy (OR=3.69, 95% CI=2.64–5.15) vs consultation only at their first assessment visit. Women diagnosed at a BAC were two times more likely to have a core or FNA biopsy than a surgical biopsy (OR=2.08, 95% CI=1.81–2.40), and almost twice as likely to receive a diagnosis within 7 weeks of their abnormal mammogram (vs >7 weeks; OR=1.91, 95% CI=1.73–2.10) compared with those in UC. Sensitivity analyses on a subset of the cohort screened between 2006 and 2009 found similar results (Supplementary Table 1). Prognostic characteristics did not significantly differ between pathways.
Table 2. Adjusted ORs and 95% CIs for association of assessment and prognostic characteristics among women diagnosed with screen-detected breast cancers through a Breast Assessment Centre compared with Usual Care.
|
Breast assessment type |
|||||
|---|---|---|---|---|---|
| Characteristics | Usual Care, N=4827, n (%) | Breast Assessment Centre, N=4217, n (%) | Overall, N=9044, n (%) | Adjusted ORa (95% CI) | P-value |
|
Time to first assessment procedure | |||||
| >3 Weeks | 1056 (21.9) | 794 (18.8) | 1850 (20.5) | 1.00 (reference) | |
| ⩽3 Weeks | 3771 (78.1) | 3423 (81.2) | 7194 (79.5) | 1.25 (1.12–1.39) | <0.0001 |
|
Total assessment procedures | |||||
| >3 Procedures | 2034 (42.1) | 1336 (31.7) | 3370 (37.3) | 1.00 (reference) | |
| ⩽3 Procedures | 2793 (57.9) | 2881 (68.3) | 5674 (62.7) | 1.54 (1.41–1.69) | <0.0001 |
|
Total assessment visits | |||||
| >2 Visits | 1918 (39.7) | 1089 (25.8) | 3007 (33.2) | 1.00 (reference) | |
| ⩽2 Visits | 2909 (60.3) | 3128 (74.2) | 6037 (66.8) | 1.86 (1.70–2.05) | <0.0001 |
|
Procedures per visit (average) | |||||
| <2 Procedures per visit | 3617 (74.9) | 2895 (68.6) | 6512 (72.0) | 1.00 (reference) | |
| ⩾2 Procedures per visit | 1210 (25.1) | 1322 (31.4) | 2532 (28.0) | 1.41 (1.28–1.55) | <0.0001 |
|
Procedure(s) at first visit | |||||
| Consultation only | 148 (3.1) | 54 (1.3) | 202 (2.2) | 1.00 (reference) | |
| Imaging (±consultation) | 3944 (81.7) | 3129 (74.2) | 7073 (78.2) | 1.99 (1.44–2.75) | <0.0001 |
| Biopsy (±imaging or consultation) | 735 (15.2) | 1034 (24.5) | 1769 (19.6) | 3.69 (2.64–5.15) | <0.0001 |
|
First biopsy procedure (any visit) | |||||
| Open/surgical | 787 (16.3) | 346 (8.2) | 1133 (12.5) | 1.00 (reference) | |
| Core/FNA | 4038 (83.7) | 3870 (91.8) | 7908 (87.5) | 2.08 (1.81–2.40) | <0.0001 |
| Missing | 2 | 1 | 3 | – | |
|
Time to diagnosis | |||||
| >7 weeks | 1776 (36.8) | 1004 (23.8) | 2780 (30.7) | 1.00 (reference) | |
| ⩽7 weeks | 3051 (63.2) | 3213 (76.2) | 6264 (69.3) | 1.91 (1.73–2.10) | <0.0001 |
|
Age at diagnosis (years) | |||||
| 50–59 | 2299 (47.6) | 2025 (48.0) | 4324 (47.8) | 1.00 (reference) | |
| 60–70 | 2528 (52.4) | 2192 (52.0) | 4720 (52.2) | 0.89 (0.75–1.05) | 0.1552 |
|
Breast cancer classification | |||||
| DCIS | 920 (19.1) | 810 (19.2) | 1730 (19.1) | 1.00 (reference) | |
| Invasive | 3907 (80.9) | 3407 (80.8) | 7314 (80.9) | 1.00 (0.90–1.11) | 0.9669 |
|
Invasive stage at diagnosis | |||||
| Stage I | 2301 (63.4) | 2030 (62.7) | 4331 (63.1) | 1.00 (reference) | |
| Stage II | 1135 (31.2) | 1018 (31.5) | 2153 (31.3) | 1.03 (0.92–1.14) | 0.6375 |
| Stage III | 195 (5.4) | 189 (5.8) | 384 (5.6) | 1.02 (0.82–1.26) | 0.8898 |
| Missing | 276 | 170 | 446 | – | |
|
Invasive tumour size | |||||
| ⩽0.5 cm (T1mic, T1a) | 345 (9.5) | 279 (9.0) | 624 (9.3) | 1.00 (reference) | |
| >0.5–⩽1.0 (T1b) | 853 (23.6) | 782 (25.2) | 1635 (24.3) | 1.11 (0.92–1.34) | 0.2862 |
| >1.0–⩽2.0 (T1c) | 1538 (42.5) | 1295 (41.7) | 2833 (42.2) | 1.01 (0.85–1.21) | 0.9076 |
| >2.0 (T2, T3, T4) | 879 (24.3) | 748 (24.1) | 1627 (24.2) | 1.02 (0.84–1.23) | 0.8795 |
| Missing | 292 | 303 | 595 | ||
|
Invasive nodal status | |||||
| Negative | 2682 (76.3) | 2404 (75.2) | 5086 (75.8) | 1.00 (reference) | |
| Positive | 835 (23.7) | 791 (24.8) | 1626 (24.2) | 1.05 (0.94–1.18) | 0.3938 |
| Missing | 390 | 212 | 602 | – | |
Abbreviations: CI=confidence interval; DCIS=ductal carcinoma in situ; FNA=fine-needle aspiration; OR=odds ratio.
Adjusted by year of screen, age at screening, screen type (initial vs rescreen), mammography type (film vs digital), mammographic density, income quintile, and community status.
Irrespective of pathway, women with breast cancer were more likely to be diagnosed within 7 weeks if they had their first procedure within 3 weeks, ⩾2 assessment procedures per visit, a biopsy during their first assessment visit compared with a consultation only, and a core/FNA compared with surgical biopsy at any visit (Table 3). In addition, women having an invasive breast cancer vs DCIS, stage II or III vs stage I, a larger tumour size (>0.5 vs ⩽0.5 cm), and positive vs negative nodal status were more likely to be diagnosed within 7 weeks, regardless of pathway. More advanced stage and larger tumour size increased the odds of being diagnosed within 7 weeks (test for trend P<0.0001). Rurality decreased the likelihood of receiving a diagnosis within 7 weeks for both BAC and UC. Income quintile did not affect time to diagnosis in a BAC; however, women in the two highest quintiles (vs the lowest) were more likely to receive a diagnosis in 7 weeks (vs >7) when assessed through UC. Having ⩽2 assessment visits was more likely to reduce time to diagnosis for women assessed through a BAC (OR=10.58, 95% CI=8.96–12.50) compared with UC (OR=4.47, 95% CI=3.94–5.07), as was having ⩽3 assessment procedures (vs >3) (BAC OR=4.97, 95% CI=4.26–5.79; UC OR=2.95, 95% CI=2.61–3.73) (Table 3). Sensitivity analyses on a subset of the cohort screened between 2006 and 2009 found similar results (Supplementary Table 2).
Table 3. Adjusted ORs and 95% CIs for the association of breast cancer risk factors, screening, assessment, and prognostic characteristics by time to diagnosis (⩽7 vs >7 weeks) among women diagnosed with screen-detected breast cancers through a Breast Assessment Centre and Usual Care.
|
Breast Assessment Centre (n=4217) |
Usual Care (n=4827) |
|||||
|---|---|---|---|---|---|---|
| Characteristic | >7 Weeks, N=1004, n (%) | ⩽7 Weeks, N=3213, n (%) | Adjusted OR (95% CI) | >7 Weeks, N=1776, n (%) | ⩽7 Weeks, N=3051, n (%) | Adjusted OR (95% CI) |
|
Screen typea | ||||||
| Initial | 289 (28.8) | 941 (29.3) | 1.00 (reference) | 673 (37.9) | 1186 (38.9) | 1.00 (reference) |
| Rescreen | 715 (71.2) | 2272 (70.7) | 0.97 (0.82–1.15) | 1103 (62.1) | 1865 (61.1) | 0.96 (0.85–1.09) |
|
Mammography typea | ||||||
| Screen film | 782 (77.9) | 2543 (79.1) | 1.00 (reference) | 1604 (90.3) | 2711 (88.9) | 1.00 (reference) |
| Digital | 222 (22.1) | 670 (20.9) | 1.12 (0.92–1.36) | 172 (9.7) | 340 (11.1) | 1.12 (0.91–1.38) |
|
Mammographic densitya | ||||||
| <75% | 915 (91.1) | 2991 (93.1) | 1.00 (reference) | 1600 (90.1) | 2771 (90.8) | 1.00 (reference) |
| ⩾75% | 89 (8.9) | 222 (6.9) | 0.78 (0.60–1.01) | 176 (9.9) | 280 (9.2) | 0.91 (0.74–1.11) |
|
Community statusa | ||||||
| Urban | 756 (75.3) | 2721 (84.7) | 1.00 (reference) | 1500 (84.5) | 2617 (85.8) | 1.00 (reference) |
| Rural | 58 (5.8) | 156 (4.9) | 0.75 (0.55–1.03) | 93 (5.2) | 204 (6.7) | 1.27 (0.98–1.63) |
| Rural remote | 128 (12.7) | 278 (8.7) | 0.60 (0.48–0.75)d | 102 (5.8) | 132 (4.3) | 0.75 (0.58–0.98)e |
| Rural very remote | 62 (6.2) | 57 (1.8) | 0.26 (0.18–0.37)d | 80 (4.5) | 97 (3.2) | 0.70 (0.52–0.95)f |
| Missing | 0 | 1 | – | 1 | 1 | – |
|
Income quintilea | ||||||
| 1, Lowest | 176 (17.6) | 559 (17.5) | 1.00 (reference) | 309 (17.5) | 462 (15.2) | 1.00 (reference) |
| 2 | 235 (23.6) | 607 (19.0) | 0.83 (0.66–1.04) | 330 (18.7) | 582 (19.2) | 1.18 (0.97–1.44) |
| 3 | 169 (17.0) | 635 (19.8) | 1.19 (0.94–1.52) | 361 (20.5) | 573 (18.9) | 1.06 (0.87–1.29) |
| 4 | 195 (19.6) | 653 (20.4) | 1.07 (0.84–1.35) | 347 (19.7) | 641 (21.1) | 1.23 (1.01–1.49)g |
| 5, Highest | 222 (22.3) | 748 (23.4) | 1.07 (0.85–1.34) | 418 (23.7) | 777 (25.6) | 1.24 (1.03–1.50)h |
| Missing | 7 | 11 | – | 11 | 16 | – |
|
Time to first assessment procedureb | ||||||
| >3 Weeks | 387 (38.5) | 407 (12.7) | 1.00 (reference) | 706 (39.8) | 350 (11.5) | 1.00 (reference) |
| ⩽3 Weeks | 617 (61.5) | 2806 (87.3) | 4.18 (3.53–4.94)d | 1070 (60.3) | 2701 (88.5) | 5.12 (4.41–5.93)d |
|
Total assessment proceduresb | ||||||
| >3 Procedures | 595 (59.3) | 741 (23.1) | 1.00 (reference) | 1039 (58.5) | 995 (32.6) | 1.00 (reference) |
| ⩽3 Procedures | 409 (40.7) | 2472 (76.9) | 4.97 (4.26–5.79)d | 737 (41.5) | 2056 (67.4) | 2.95 (2.61–3.33)d |
|
Total assessment visitsb | ||||||
| >2 Visits | 632 (62.9) | 457 (14.2) | 1.00 (reference) | 1098 (61.8) | 820 (26.9) | 1.00 (reference) |
| ⩽2 Visits | 372 (37.1) | 2756 (85.8) | 10.58 (8.96–12.50)d | 678 (38.2) | 2231 (73.1) | 4.47 (3.94–5.07)d |
| Average number of procedures per visitb | ||||||
| <2 Procedures per visit | 883 (88.0) | 2012 (62.6) | 1.00 (reference) | 1546 (87.1) | 2071 (6.9) | 1.00 (reference) |
| ⩾2 Procedures per visit | 121 (12.1) | 1201 (37.4) | 4.31 (3.51–5.29)d | 230 (13.0) | 980 (32.1) | 3.18 (2.71–3.73)d |
|
Procedure(s) at first visitb | ||||||
| Consultation only | 17 (1.7) | 37 (1.2) | 1.00 (reference) | 57 (3.2) | 91 (3.0) | 1.00 (reference) |
| Imaging (±consultation) | 917 (91.3) | 2212 (68.8) | 1.12 (0.62–2.02) | 1651 (93.0) | 2293 (75.2) | 0.84 (0.60–1.18) |
| Biopsy (±imaging or consultation) | 70 (7.0) | 964 (30.0) | 6.00 (3.18–11.33)d | 68 (3.8) | 667 (21.9) | 6.05 (3.99–9.18)d |
|
First biopsy procedure (any visit)b | ||||||
| Open/surgical | 150 (14.9) | 196 (6.1) | 1.00 (reference) | 429 (24.2) | 358 (11.7) | 1.00 (reference) |
| Core/FNA | 854 (85.1) | 3016 (93.9) | 2.85 (2.25–3.61)d | 1346 (75.8) | 2692 (88.3) | 2.43 (2.06–2.86)d |
| Missing | 0 | 1 | – | 1 | 1 | – |
|
Age at diagnosis (years)c | ||||||
| 50–59 | 475 (47.3) | 1550 (48.2) | 1.00 (reference) | 833 (46.9) | 1466 (48.0) | 1.00 (reference) |
| 60–70 | 529 (52.7) | 1663 (51.8) | 0.98 (0.85–1.13) | 943 (53.1) | 1585 (52.0) | 0.95 (0.85–1.07) |
|
Breast cancer classificationb | ||||||
| DCIS | 305 (30.4) | 505 (15.7) | 1.00 (reference) | 482 (27.1) | 438 (14.4) | 1.00 (reference) |
| Invasive | 699 (69.6) | 2708 (84.3) | 2.41 (2.03–2.85)d | 1294 (72.9) | 2613 (85.6) | 2.26 (1.95–2.62)d |
|
Invasive stage at diagnosisb | ||||||
| Stage I | 451 (70.8) | 1579 (60.7) | 1.00 (reference) | 836 (70.7) | 1465 (59.8) | 1.00 (reference) |
| Stage II | 158 (24.8) | 860 (33.1) | 1.58 (1.29–1.93)d | 307 (26.0) | 828 (33.8) | 1.55 (1.32–1.81)d |
| Stage III | 28 (4.4) | 161 (6.2) | 1.82 (1.19–2.79)i | 40 (3.4) | 155 (6.3) | 2.14 (1.49–3.08)d |
| Missing | 62 | 108 | – | 111 | 165 | – |
|
Invasive tumour sizeb | ||||||
| ⩽0.5 cm (T1mic, T1a) | 87 (14.2) | 192 (7.7) | 1.00 (reference) | 167 (14.0) | 178 (7.3) | 1.00 (reference) |
| >0.5–⩽1.0 (T1b) | 190 (31.1) | 592 (23.8) | 1.47 (1.09–2.00)j | 347 (29.1) | 506 (20.9) | 1.36 (1.06–1.75)k |
| >1.0–⩽2.0 (T1c) | 235 (38.5) | 1060 (42.5) | 2.17 (1.62–2.91)d | 460 (38.6) | 1078 (44.5) | 2.19 (1.73–2.79)d |
| >2.0 (T2, T3, T4) | 99 (16.2) | 649 (26.0) | 3.18 (2.28–4.45)d | 217 (18.2) | 662 (27.3) | 2.84 (2.18–3.69)d |
| Missing | 88 | 215 | – | 103 | 189 | – |
|
Invasive nodal statusb | ||||||
| Negative | 502 (79.2) | 1902 (74.3) | 1.00 (reference) | 930 (81.7) | 1752 (73.7) | 1.00 (reference) |
| Positive | 132 (20.8) | 659 (25.7) | 1.38 (1.11–1.71)l | 209 (18.3) | 626 (26.3) | 1.59 (1.33–1.89)d |
| Missing | 65 | 147 | – | 155 | 235 | – |
Abbreviations: CI=confidence interval; DCIS=ductal carcinoma in situ; FNA=fine-needle aspiration; OR=odds ratio.
Adjusted by year of screen and age at screening.
Adjusted by year of screen, age at screening, income quintile, and community status.
Adjusted by year of screen, income quintile, and community status.
P<0.0001; eP=0.0362; fP=0.0211; gP=0.0386; hP=0.0231; i P=0.0058; jP=0.0131; kP=0.0175; lP=0.0105.
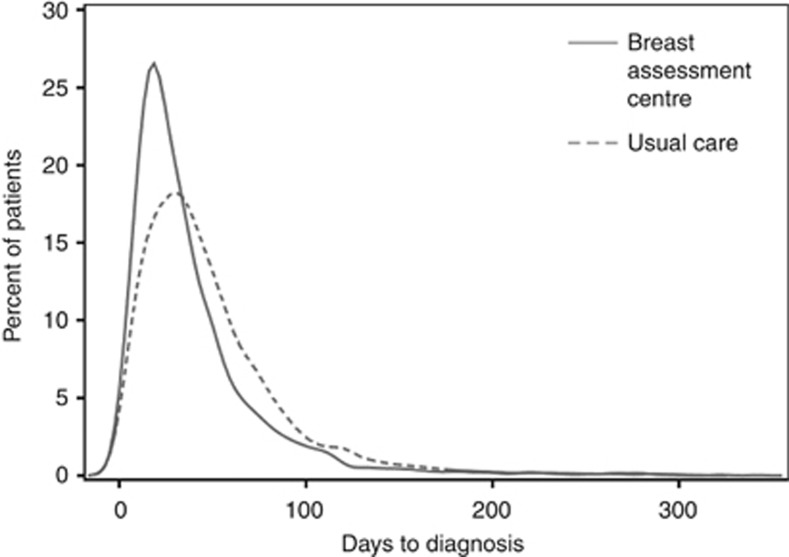
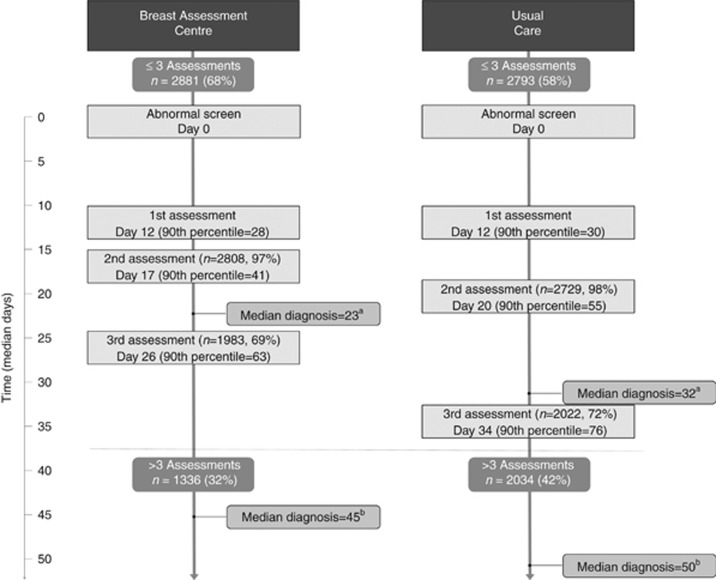
Overall median wait times from abnormal screen to diagnosis were 28 days for women assessed through BACs and 39 days for UC (P<0.0001; Figure 2). For women with ⩽3 assessment procedures, the median time to diagnosis was 9 days shorter in a BAC compared with UC (BAC: 23 median days IQR=15–39; UC: 32 median days IQR=18–51; P<0.0001) (Figure 3). Among women with >3 procedures, this difference still persisted (BAC: 45 median days IQR=26–75; UC: 50 median days IQR=34–79; P<0.0001).
Figure 2.
Distributions of time to diagnosis (in days) for women diagnosed through Breast Assessment Centres and Usual Care.
Figure 3.
Median time and 90th percentile (in days) from abnormal mammogram to diagnosis for women diagnosed with screen-detected breast cancers, stratified by assessment centre type and number of assessment procedures (⩽3 assessments (top) vs >3 assessments (bottom)). Sample size within the assessment boxes represent the proportion of women who have had that assessment (i.e., who have not yet obtained a diagnosis). aWilcoxon rank-sum test for differences in median days to diagnosis (23 days vs 31 days) for ⩽3 assessment procedures, p<0.0001. bWilcoxon rank-sum test for differences in median days to diagnosis (45 days vs 50 days) for > 3 assessment procedures, p<0.0001.
Discussion
This study found that women with breast cancer were almost two times more likely to be diagnosed within 7 weeks when assessed through a BAC vs UC. Irrespective of assessment pathway, women were significantly more likely to be diagnosed within 7 weeks if they had their first assessment procedure within 3 weeks (vs >3 weeks), ⩾2 procedures per visit (vs <2), a biopsy at first visit compared with consultation only, and a core/FNA compared with open biopsy at any visit. Having ⩽2 assessment visits and ⩽3 assessment procedures was more likely to reduce time to diagnosis for women assessed through a BAC compared with UC. However, diagnostic wait time was significantly shorter in a BAC, regardless of the number of procedures.
Another Ontario study found that women undergoing organised assessment had 1.7 times greater odds of receiving a diagnosis within 7 weeks (Jiang et al, 2015), a result very similar to this study. Although the previous study included only 1 year of data, a large proportion of opportunistic screens, and only invasive cancers, this study and ours suggests that organised assessment is beneficial to women. Shorter diagnostic intervals were also seen among women with screen-detected breast cancer in Manitoba who received diagnostic work up through direct referral compared with UC (Decker et al, 2004). Women in British Columbia’s direct referral program, ‘‘Fast Track’’, experienced similar improvement (Borugian et al, 2008), as did those receiving patient navigation in Nova Scotia (Psooy et al, 2004). Given our study, and others (Olivotto et al, 2001b; Decker et al, 2004; Psooy et al, 2004; Borugian et al, 2008; Baliski et al, 2014; Jiang et al, 2015), it appears that patient navigation and coordinated referral results in equitable expedited access to services, having a consistent benefit over UC.
Having ⩽2 assessment visits and ⩽3 assessment procedures was more likely to reduce time to diagnosis for women assessed through a BAC vs UC. For women with ⩽ 3 assessment procedures, this difference could not be explained by time to first assessment procedure, which was similar between pathways. However, those in a BAC did have more procedures per visit than UC, resulting in more efficient visits. Women assessed through BACs also had assessment procedures scheduled in shorter intervals. In addition, type of procedure is important in shortening diagnostic wait times, as women assessed through BAC were more likely to have imaging or biopsy on their first assessment visit.
We found that open biopsy was uncommon overall, possibly because of the recommendation that tissue diagnosis of breast abnormalities be obtained before surgery (McCready et al, 2005; Bevers et al, 2009). Irrespective of pathway, those who underwent open biopsy were more likely to experience longer wait times to diagnosis than those having percutaneous FNA or core biopsy. This finding is consistent with research conducted in British Columbia (Olivotto et al, 2000) and across screening programs in Canada, including Ontario (Olivotto et al, 2001a). Wait times for operating rooms and the need for surgical consultations may be the most likely explanation for the delay. Recent findings have shown that women in rural areas have higher rates of open biopsy at diagnosis (Holloway et al, 2007). Although women attending BACs were more likely to live in rural areas, they had a lower proportion of open biopsies as a result of the standardisation of care pathways and improving access to guideline-based care. This in turn is likely to influence time to diagnosis (Olivotto et al, 2000, 2001a). In addition, although those in UC were more likely to be diagnosed within 7 weeks if they were of higher income, income had no effect for women assessed within a BAC. This result might indicate an important benefit of organised assessment on social disparities.
Irrespective of pathway, women with invasive breast cancers of more advanced stage and larger tumour size were more likely to be diagnosed within 7 weeks as compared with those diagnosed at earlier stages with smaller tumours. This finding is consistent with literature demonstrating an expedited evaluation process for more overtly worrisome cases, where suspicious (Caplan et al, 2000; Olivotto et al, 2002; Ganry et al, 2004) and larger tumours (Bairati et al, 2007) were associated with decreased likelihood of diagnostic delay, and smaller tumours associated with increased delay (Molinié et al, 2013). Our results also align with research showing that women with less advanced stage were more likely to experience diagnostic delay compared with those with more advanced stage (Jiang et al, 2015), although their population also included symptomatic breast cancers.
Overall, women assessed through a BAC had more timely diagnoses and received fewer, more appropriate procedures. However, there are important considerations to facilitate the establishment of organised breast assessment centres. In Ontario, BACs require additional practitioners, access to diagnostic specialists, and adequate imaging, biopsy, and pathological assessment capacity (Quan et al, 2012; Jiang et al, 2015). These requirements may be more challenging in remote settings, in addition to being more costly.
The strengths of this study include its use of existing data collected on a large population-based cohort of screened women during an 8-year period. All eligible women were identified from a centralised screening database, and follow-up was identical. Women diagnosed through BACs were similar to women diagnosed through UC by age at screen and at diagnosis and on breast cancer risk factors and prognostic characteristics. However, the two cohorts did differ significantly by year of screen and region of screening centre as this would reflect when and where the BACs were implemented. To ensure comparability, any differences in year of screen, screen type, mammography type, mammographic density, income quintile, and community status were adjusted for in analyses.
There were several limitations to the study. First, it was not possible to distinguish between system-level and certain patient-level factors associated with diagnostic delay. Patient-level factors that can influence diagnostic times include poorer health (Yabroff et al, 2004), patient beliefs and attitudes (Yabroff et al, 2004; Allen et al, 2008), and logistical barriers to accessing services (Allen et al, 2008). However, recent reviews have not been able to estimate the proportion of diagnostic delay that might be due to patient vs system-level factors (Wujcik and Fair, 2008; Zapka et al, 2010). In addition, compared with UC, a greater proportion of women in the BAC cohort were seen in a more recent time period, when percutaneous biopsy has become standardised and more accessible. Lastly, this study focussed solely on patients with cancer diagnoses. We are not able to determine how diagnostic wait times would compare for patients with a benign outcome who often undergo less prompt assessment than those with overtly suspicious findings.
The benefits of early detection by mammography are dependent on women with abnormal screening results having access to timely and accurate diagnostic assessment. This study examined the impact of procedures and visits on diagnostic delays and found that women with screen-detected breast cancer in OBSP were more likely to have shorter wait times if they were seen through organised assessment. This was likely because of fewer, timelier, more appropriate assessment procedures for women diagnosed through BACs vs UC. Given the significant improvement in timeliness to diagnosis, women with abnormal mammograms should be managed through organised assessment. Future work will address the impact of diagnostic and treatment intervals on breast cancer survival by assessment pathway.
Acknowledgments
We thank the study staff: Leanne Lindsay, Lucy Leon, and Anjali Pandya. We also thank Cancer Care Ontario for use of its data. This work was supported by the Canadian Institutes of Health Research (Grant Number 130400). This agency had no involvement in the study design, data collection, analysis, interpretation, manuscript preparation, or the decision to submit the manuscript for publication.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
The authors declare no conflict of interest.
Supplementary Material
References
- Allen JD, Shelton RC, Harden E, Goldman RE (2008) Follow-up of abnormal screening mammograms among low-income ethnically diverse women: findings from a qualitative study. Patient Educ Couns 72: 283–292. [DOI] [PubMed] [Google Scholar]
- American Joint Committee on Cancer (2002) Cancer Staging Manual 6th edn Springer-Verlag: New York. [Google Scholar]
- Bairati I, Jobin E, Fillion L, Larochelle M, Vincent L (2007) Determinants of delay for breast cancer diagnosis. Cancer Detect Prev 31: 323–331. [DOI] [PubMed] [Google Scholar]
- Baliski C, Mcgahan CE, Liberto CM, Broughton S, Ellard S, Taylor M, Bates J, Lai A (2014) Influence of nurse navigation on wait times for breast cancer care in a Canadian regional cancer center. Am J Surg 207: 686–692. [DOI] [PubMed] [Google Scholar]
- Bevers TB, Anderson BO, Bonaccio E, Buys S, Daly MB, Dempsey PJ, Farrar WB, Fleming I, Garber JE, Harris RE, Heerdt AS, Helvie M, Huff JG, Khakpour N, Khan SA, Krontiras H, Lyman G, Rafferty E, Shaw S, Smith ML, Tsangaris TN, Williams C, Yankeelov T National Comprehensive Cancer Network (2009) NCCN clinical practice guidelines in oncology: breast cancer screening and diagnosis. J Natl Compr Canc Netw 7: 1060–1096. [DOI] [PubMed] [Google Scholar]
- Borugian MJ, Kan L, Chu CC, Ceballos K, Gelmon KA, Gordon PB, Poole B, Tyldesley S, Olivotto IA (2008) Facilitated ‘‘Fast Track’’ referral reduces time from abnormal screening mammogram to diagnosis. Can J Public Health 99: 252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett J, Austoker J, Ong G (1998) Do women who undergo further investigation for breast screening suffer adverse psychological consequences? A multi-centre follow-up study comparing different breast screening result groups five months after their last breast screening appointment. J Public Health Med 20: 396–403. [DOI] [PubMed] [Google Scholar]
- Canadian Breast Cancer Screening Initiative Working Group (2000) Canadian Breast Cancer Screening Initiative Working Group on the Integration of Screening and Diagnosis: Waiting for a diagnosis after an abnormal breast cancer screen in Canada. Minister of Public Works and Government Services: Ottawa. [Google Scholar]
- Canadian Partnership against Cancer (2013) Report from the Evaluation Indicators Working Group: Guidelines for Monitoring Breast Cancer Screening Program Performance 3rd edn, Canadian Partnership Against Cancer Toronto. [Google Scholar]
- Caplan LS, May DS, Richardson LC (2000) Time to diagnosis and treatment of breast cancer: results from the National Breast and Cervical Cancer Early Detection Program, 1991–1995. Am J Public Health 90: 130–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiarelli AM, Edwards SA, Prummel MV, Muradali D, Majpruz V, Done SJ, Brown P, Shumak RS, Yaffe MJ (2013) Digital compared with screen-film mammography: performance measures in concurrent cohorts within an organized breast screening program. Radiology 268: 684–693. [DOI] [PubMed] [Google Scholar]
- Decker KM, Harrison M, Chateau D (2004) Influence of direct referrals on time to diagnosis after an abnormal breast screening result. Cancer Detect Prev 28: 361–367. [DOI] [PubMed] [Google Scholar]
- Diggle PJ, Heagerty P, Liang K, Zeger SL (2002) Analysis of Longitudinal Data. Oxford University Press: Oxford. [Google Scholar]
- Ganry O, Peng J, Dubreuil A (2004) Influence of abnormal screens on delays and prognostic indicators of screen-detected breast carcinoma. J Med Screen 11: 28–31. [DOI] [PubMed] [Google Scholar]
- Haynes W (2013) Wilcoxon Rank Sum Test. Encyclopedia of Systems Biology. Springer: New York, NY, USA. [Google Scholar]
- Holloway CM, Saskin R, Brackstone M, Paszat L (2007) Variation in the use of percutaneous biopsy for diagnosis of breast abnormalities in Ontario. Ann Surg Oncol 14: 2932–2939. [DOI] [PubMed] [Google Scholar]
- Jaro MA (1995) Probabilistic linkage of large public health data files. Stat Med 14: 491–498. [DOI] [PubMed] [Google Scholar]
- Jiang L, Gilbert J, Langley H, Moineddin R, Groome P (2015) Effect of specialized diagnostic assessment units on the time to diagnosis in screen-detected breast cancer patients. Br J Cancer 112: 1744–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCready D, Holloway C, Shelley W, Down N, Robinson P, Sinclair S, Mirsky D Breast Cancer Disease Site Group of Cancer Care, Ontario’s Program in Evidence-Based Care (2005) Surgical management of early stage invasive breast cancer: a practice guideline. Can J Surg 48: 185–194. [PMC free article] [PubMed] [Google Scholar]
- Molinié F, Leux C, Delafosse P, Ayrault-Piault S, Arveux P, Woronoff A, Guizard A, Velten M, Ganry O, Bara S (2013) Waiting time disparities in breast cancer diagnosis and treatment: a population-based study in France. Breast 22: 810–816. [DOI] [PubMed] [Google Scholar]
- Nelson HD, Fu R, Cantor A, Pappas M, Daeges M, Humphrey L (2016) Effectiveness of breast cancer screening: systematic review and meta-analysis to update the 2009 US Preventive Services Task Force recommendation. Ann Intern Med 164: 244–255. [DOI] [PubMed] [Google Scholar]
- Olivotto IA, Bancej C, Goel V, Snider J, Mcauley RG, Irvine B, Kan L, Mirsky D, Sabine MJ, Mcgilly R, Caines JS (2001. a) Waiting times from abnormal breast screen to diagnosis in 7 Canadian provinces. CanJ 165: 277–283. [PMC free article] [PubMed] [Google Scholar]
- Olivotto IA, Borugian MJ, Kan L, Harris SR, Rousseau EJ, Thorne SE, Vestrup JA, Wright CJ, Coldman AJ, Hislop TG (2001. b) Improving the time to diagnosis after an abnormal screening mammogram. Can J Public Health 92: 366–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivotto IA, Gomi A, Bancej C, Brisson J, Tonita J, Kan L, Mah Z, Harrison M, Shumak R (2002) Influence of delay to diagnosis on prognostic indicators of screen-detected breast carcinoma. Cancer 94: 2143–2150. [DOI] [PubMed] [Google Scholar]
- Olivotto IA, Kan L, King S (2000) Waiting for a diagnosis after an abnormal screening mammogram. Can J Public Health 91: 113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ontario Breast Screening Program (2001) Multidisciplinary Roles and Expectations for Breast Assessment in Ontario. The Breast Assessment Collaborative Group: Toronto. [Google Scholar]
- Psooy BJ, Schreuer D, Borgaonkar J, Caines JS (2004) Patient navigation: improving timeliness in the diagnosis of breast abnormalities. Can Assoc Radiol J 55: 145–150. [PubMed] [Google Scholar]
- Quan ML, Shumak RS, Majpruz V, Holloway CM, O’Malley FP, Chiarelli AM (2012) Improving work-up of the abnormal mammogram through organized assessment: Results from the ontario breast screening program. J Oncol Pract 8: 107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimer BK, Bluman LG (1997) The psychosocial consequences of mammography. J Natl Cancer Inst Monogr 22: 131–138. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc (2008) Statistical Analysis Software. 9.4 edn. SAS Institute: Cary. [Google Scholar]
- Statistics Canada (1997) 1996 Census dictionary. Report No.: 92-325-UIE. Statistics Canada: Ottawa. [Google Scholar]
- Sutton S, Saidi G, Bickler G, Hunter J (1995) Does routine screening for breast cancer raise anxiety? Results from a three wave prospective study in England. J Epidemiol Community Health 49: 413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Canadian Task Force on Preventive Health Care (2011) Recommendations on screening for breast cancer in average-risk women aged 40–74 years. CMAJ 183: 1991–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Workshop Group (1989) Reducing deaths from breast cancer in Canada. Can Med Assoc J 141: 199–201. [PMC free article] [PubMed] [Google Scholar]
- Wilkins R (1998) Geocodes/PCCF Version 3 User’s Guide: Automated Geographic Coding based on the Statistics Canada Postal Code Conversion Files. Health Statistics Division, Statistics Canada: Ottawa. [Google Scholar]
- World Health Organization (1990) International Classification of Diseases for Oncology (ICD-O). WHO: Geneva. [Google Scholar]
- Wujcik D, Fair AM (2008) Barriers to diagnostic resolution after abnormal mammography: a review of the literature. Cancer Nurs 31: E16–E30. [DOI] [PubMed] [Google Scholar]
- Yabroff KR, Breen N, Vernon SW, Meissner HI, Freedman AN, Ballard-Barbash R (2004) What factors are associated with diagnostic follow-up after abnormal mammograms? Findings from a US National Survey. Cancer Epidemiol Biomarkers Prev 13: 723–732. [PubMed] [Google Scholar]
- Zapka J, Taplin SH, Price RA, Cranos C, Yabroff R (2010) Factors in quality care—the case of follow-up to abnormal cancer screening tests—problems in the steps and interfaces of care. J Natl Cancer Inst Monogr 2010: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.