Abstract
Purpose
Why do orphans have higher rates of HIV infection than non-orphaned peers? Research consistently assumes that orphans acquire HIV primarily through sexual behavior, but infections may instead be due to maternal transmission. Although these two pathways have very different implications for HIV programs and policies, their relative contribution has not been previously examined. In this research, we compare the contribution of maternal and sexual transmission to HIV infection among orphans in Africa.
Methods
We use Demographic and Health Surveys data for 21,463 women and 18,359 men from 17 countries. We propose a conceptual framework linking orphanhood to HIV, and use mediation analysis and structural equation modeling to compare the potential contribution of maternal transmission (measured through direct pathways from orphanhood to HIV) and sexual transmission (measured through reports of risky sexual behavior) to orphan HIV infection.
Results
Our results suggest that maternal transmission is the predominant pathway of HIV infection among orphaned adolescents: there is strong evidence for a direct pathway from maternal (odds ratio 2.45; 95% confidence interval 1.72–3.51 for females and 2.45; 1.53–3.90 for males) and double orphanhood (odds ratio 2.69; 1.97–3.66 and 2.53; 1.68–3.82 respectively) to HIV; greater excess HIV risk in maternal versus paternal orphans. The contribution of sexual behavior is largely not significant. We do not observe correspondingly high orphan disparities in other STDs.
Conclusion
Maternal transmission is a more likely explanation than sexual transmission for heightened HIV infection among orphans. These results suggest that programs designed to address HIV infection among adolescents should focus on reducing maternal transmission and identifying and testing undiagnosed HIV among orphans.
Keywords: orphans, HIV infection, Africa, maternal transmission
HIV infection among adolescents and young adults remains a critical issue: despite steep declines among every other age group, AIDS mortality has tripled among adolescents (aged 10–19 years) since 2000, and AIDS is now the leading cause of death among this age group in sub-Saharan Africa (SSA).1 Another quarter million adolescents are newly infected every year.2
Throughout the HIV/AIDS epidemic, research in SSA has consistently assumed that HIV transmission for adolescents and young adults occurred primarily through sexual behavior.3–5 As a result, programs for this population have been primarily aimed at sexual transmission, focusing on increasing condom use and male circumcision, reducing multiple sexual partners and transactional sex, and delaying age at sexual debut.3
Among adolescents and young adults, there is particular concern for orphans. A growing number of studies have identified adolescent orphans as a high-risk group for HIV; several have found that orphans are two to three times more likely to have acquired HIV by the time they reach adolescence than non-orphaned peers.6,7 Humanitarian groups, governments, and donors have specifically targeted orphans in HIV prevention initiatives.8,9
Whether such investments have the intended impact on HIV incidence, however, depends on when and how orphans acquire HIV. As with other populations, it is widely assumed that orphaned adolescents acquire HIV primarily through behavioral transmission.10,11 There is evidence that orphans experience greater economic hardship, mental distress, and sexual victimization,12 and such extreme social vulnerability may predispose orphans to greater sexual risk taking. However, the empirical evidence on this is not definitive.7 Despite the ambiguity, the implicit assumption that orphans acquire HIV sexually appears frequently in research, policies and programs.
But what if this basic assumption is wrong? For much of the epidemic, ART was largely unavailable or inaccessible, and the chance of an infected infant surviving to adolescence was thought to be very low. However, recent research has found that HIV infection progresses slowly among some infants and a substantial proportion of HIV positive survive to adolescence and beyond.13,14 Moreover, recent research in Kenya15 and Ethiopia16 has found substantial HIV prevalence for older children (under age 15), the majority of whom were presumably not infected through sexual transmission due to low rates of sexual activity for these age groups. In addition, an intervention to reduce HIV among Zimbabwean adolescents had no impact on orphan HIV disparities, leading the authors to suggest that excess risk among orphans is likely due to maternal transmission.17 These studies challenge long-held assumptions about the predominant mode of transmission, although this has not been explicitly tested.
Compared to sexual transmission, maternal transmission has important implications for HIV and orphanhood programming, including a shift towards greater surveillance to identify undiagnosed HIV and related morbidity among orphans. Due to the predominant focus on sexual transmission, HIV testing efforts are typically not directed towards this population.16 As a result, many of these HIV positive children are undiagnosed and not linked to treatment.15,16 As these “missing children” mature into adolescents, they may alter the future course of the HIV epidemic. The goal of this study is to clarify the etiology of orphan HIV disparities, and in doing so provide essential guidance for our response.
Methods
Sample
Data are derived from Demographics and Health Surveys (DHS) in 17 Sub-Saharan African countries (Table 1). DHS are nationally-representative and have high response rates. For more detail on DHS methods and scope see18. For this study, surveys were included if they were publicly-available at the time of analyses, collected parental survival information, conducted HIV testing, and had at least one HIV-positive adolescent (see Table 1). For females, secondary analyses are further restricted to surveys in which sexual violence data were also collected. Data are pooled across all eligible surveys. Secondary research on this data source was exempted from the need for human subjects review by Stony Brook University.
Table 1.
DHS sample size included in analyses, by country and survey year
| Country (year) | Females 15–17 with HIV data | Females 15–17 with HIV and sexual violence data | Males 15–17 with HIV data |
|---|---|---|---|
| Burkina Faso (2010) | * | – | 959 |
| Cameroon (2011) | 1,020 | – | 938 |
| Congo (2009) | 767 | – | 640 |
| Cote d’Ivoire (2005) | 591 | 432 | 528 |
| Cote d’Ivoire (2011) | 547 | – | 474 |
| DRC (2007) | 550 | – | 507 |
| Ethiopia (2011) | 2,191 | – | 1,582 |
| Gabon (2012) | 732 | 356 | 725 |
| Lesotho (2004) | 464 | – | 407 |
| Lesotho (2009) | 562 | – | 490 |
| Liberia (2007) | 734 | 330 | 606 |
| Malawi (2004) | 298 | – | 262 |
| Malawi (2010) | 1,115 | 616 | 1,037 |
| Mozambique (2009) | 525 | – | 541 |
| Rwanda (2005) | 830 | 826 | – |
| Rwanda (2010) | 988 | 509 | 919 |
| Sierra Leone | 311 | – | – |
| Swaziland (2006) | 739 | – | 778 |
| Tanzania (2003) | 750 | – | 687 |
| Tanzania (2007) | 1,335 | – | 1,174 |
| Tanzania (2011) | 1,369 | – | 1,174 |
| Uganda (2011) | 1,403 | 303 | 1,312 |
| Zambia (2007) | 780 | 397 | 679 |
| Zimbabwe (2005 – 6) | 1,062 | 566 | 1,017 |
| Zimbabwe (2010 – 11) | 1,005 | 516 | 923 |
|
| |||
| Total | 21,070 | 4,851 | 18,359 |
Burkino Faso was not included as there were no HIV-positive female adolescents.
Measures
Independent variable: We define orphans as children below age 18 who have lost one or both parents. We further classify orphans by whether they have lost their mother (maternal orphan), father (paternal orphan), or both parents (double orphan).
Dependent variables: The primary dependent variable in our analysis is HIV status. The DHS has been conducting anonymous, informed, and voluntary HIV testing since 2001. Blood spots are taken from individuals aged 15–49 and HIV status is assessed with an ELISA test; positive results (and a subsample of negative results) are confirmed with a second test.19 Secondary analyses use a binary variable capturing any self-reported sexually transmitted disease (STD) symptomology, abnormal genital discharge, or genital ulcers/sores in the past 12 months; these questions were asked only of sexually active respondents.
Potential mediating variables: Adolescents are coded as engaging in risky sexual behavior if they did not use a condom with any of their last three partners in the past year, or had two or more partners in the past year – behaviors that are empirically linked to HIV acquisition in Africa.20,21 The reference group is adolescents who were abstinent or had protected sex with only one partner in the past year. We also examine the possibility that sexual victimization contributes to HIV infection among orphans through a binary indicator of reported lifetime sexual violence experience. Questions related to sexual violence generally came from a modified version of the conflict tactics scale.22 Men were not asked these questions, and only a subset of DHS surveys included this scale for women. There was variation between countries in how sexual violence was measured (more information on this measure is available in23).
Analyses
Descriptive data are presented using the DHS sample weights; unadjusted differences in outcome variables (HIV infection and STD infection) and potential mediators (sexual violence and HIV risk behavior) by orphan categories are assessed with chi-square tests.
To guide pathway analyses, we created the conceptual model in Figure 1. We test the role of different pathways by simultaneously examining the relationship between orphanhood and intermediate outcomes (risky behaviors in the primary sample, with the addition of lifetime sexual violence in secondary sample) and the main outcome (HIV status). We repeat such models using STD status as the outcome. OLS regression cannot capture simultaneous mediation, and thus we use structural equation modelling.24 Models are fit using the gsem command in Stata 13, are adjusted for age, and include country-level fixed effects.
Figure 1.
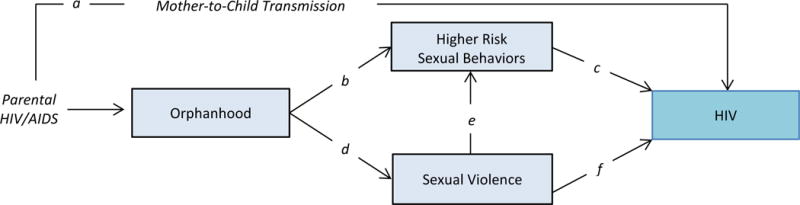
Conceptual pathways from orphanhood to HIV
Hypotheses
According to Figure 1, if sexual transmission is a key pathway to HIV, we expect corresponding pathways b and c to be significant. Sexual violence may also contribute to sexual transmission (through pathway d plus e and/or f). Further support for a sexual transmission hypothesis would come from correspondingly high orphan disparities in other STDs, which would likewise result from risky sexual behavior.
If mother-to-child transmission plays an important role, we expect substantial unexplained variance in HIV disparities (represented by path a) after controlling for sexual risk and violence. We do not have a measure of parental HIV status, and thus use the direct pathway as a proxy. We adapt the approach taken by Eaton et al.25 to further assess the likelihood of mother-to-child transmission: if orphans were primarily infected around birth, we further expect 1) greater excess HIV risk in maternal versus paternal orphans, 2) greater HIV disparities among those most likely to be sexually naïve (e.g., those aged 15).
Results
There were 21,463 females aged 15–17 who were tested for HIV, 4,851 of whom were also surveyed about sexual violence. Just over a quarter of the sample had a deceased parent. Almost half (46%) of the 393 HIV-positive test results occurred among orphans. HIV prevalence among non-orphans was 1% (see Table 2), and was elevated among maternal (4%), paternal (3%) and double orphans (4%). Approximately a third of the sample (n = 6,512) reported being sexually active and were asked about STD symptoms. Among this subsample, 15% reported an STD with no significant difference by orphan status. Similarly, there were no differences in the prevalence of mediators by orphanhood: overall, 23% reported engaging in at least one risky sexual behavior in the past year. In the subsample with sexual violence data, 12% of females reported ever experiencing sexual violence, with no crude difference by orphan status.
Table 2.
Descriptive statistics on orphanhood and sexual health, by gender
| Outcome Variables | Potential Mediators | |||
|---|---|---|---|---|
| HIV - positive | Past year STD among sexually active | Lifetime sexual violence | Past year risky sexual behavior | |
| Females (N = 21,463) | % | % | % | % |
| Maternal Orphans (n =1,079) | 3.69 | 14.82 | na | 24.93 |
| Paternal Orphans (n = 3,252) | 2.53 | 12.54 | na | 23.32 |
| Double Orphans (n = 1,162) | 4.43 | 15.02 | na | 22.06 |
| Non - Orphans (n =15,970) | 1.35 | 16.00 | na | 23.53 |
| χ2 p - value | 0.00 | 0.23 | na | 0.65 |
|
| ||||
| Females (N = 4, 851) | % | % | % | % |
| Maternal Orphans (n = 284) | 6.14 | 12.72 | 14.47 | 19.14 |
| Paternal Orphans (n = 856) | 2.78 | 12.22 | 10.13 | 18.44 |
| Double Orphans (n = 362) | 4.10 | 12.67 | 13.42 | 17.59 |
| Non - Orphans (n = 3,349) | 1.42 | 17.67 | 11.97 | 21.45 |
| χ2 p - value | 0.00 | 0.31 | 0.38 | 0.23 |
|
| ||||
| Males (N = 18,359) | % | % | % | % |
| Maternal Orphans (n = 938) | 2.70 | 9.11 | na | 17.51 |
| Paternal Orphans (n = 2,674) | 1.44 | 9.25 | na | 19.56 |
| Double Orphans (n = 1,015) | 3.72 | 8.61 | na | 18.62 |
| Non - Orphans (n = 13,732) | 0.90 | 7.67 | na | 19.71 |
| χ2 p - value | 0.00 | 0.59 | na | 0.55 |
There were 18,359 males in our sample, and they followed a similar pattern: 25% had a deceased parent and 90 of the 208 HIV-positive test results occurred among orphans. Only HIV infection differed significantly by orphanhood (<1% in non-orphans versus 4% in double orphans). No orphan disparities emerged for either reported STDs (8% among the 5011 males who reported sexual activity) or risky sexual behavior (20%).
Pathways between orphanhood and HIV
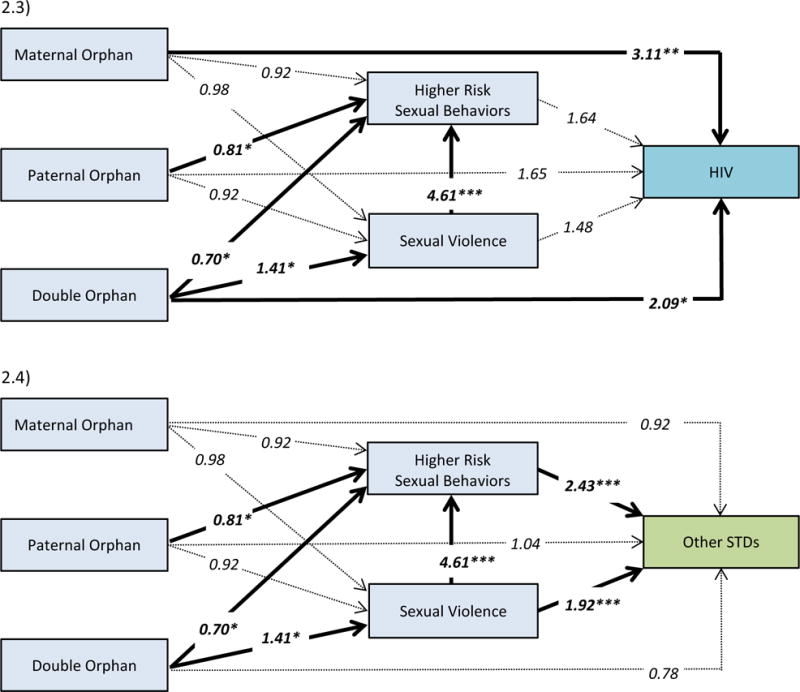
Each pathway diagram in Figure 2 (for females) and Figure 3 (for males) illustrates the empirical results from a structural equation model. Consistent with the conceptual model, the diagram contains both direct and indirect pathways from orphanhood to sexual health. Each segment of the pathway represents a relationship between the two connected variables. The strength of the relationship is captured in the embedded odds ratio. We further use bolded lines to highlight significant relationships; dotted lines represent hypothesized relationships that are not supported by the data.
Figure 2.
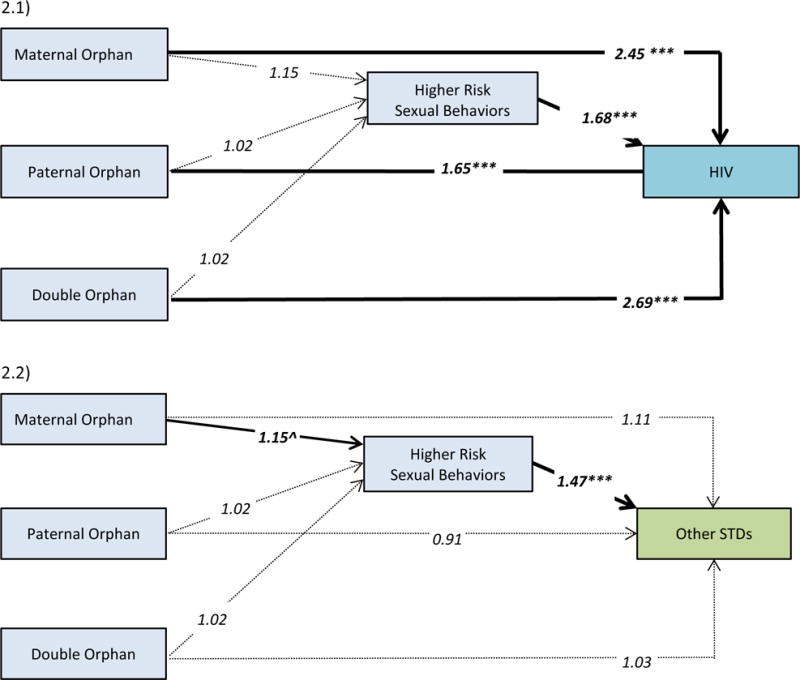
Pathway analysis from orphanhood to HIV and other STDs for the full sample of female adolescents (2.1 & 2.2) and for those with both HIV and SV data (2.3 & 2.4). Embedded values are odds ratios (*p<.05, **p<.01, ***p<.001); bolded lines indicate significant relationships. ORs are adjusted for age and country-level fixed effects.
Figure 3.
Pathway analysis from orphanhood to HIV and other STDs for male adolescents with HIV data. Embedded values are odds ratios (*p<.05, **p<.01, ***p<.001); bolded lines indicate significant relationships. ORs are adjusted for age and country-level fixed effects.
Evidence for mother-to-child transmission: There is strong and consistent evidence for a direct pathway from maternal orphanhood (odds ratio (OR) 2.45; 95% confidence interval (CI) 1.72–3.51 for females (Figure 2.1) and 2.44; 1.53–3.90 for males (Figure 3.1)) and double orphanhood (OR 2.69; 95% CI 1.97–3.66 and 2.53; 1.68–3.82 respectively) to HIV, regardless of gender. This is tempered for paternal orphans in whom we would expect a weaker relationship: for females, the odds ratio is 1.65 (95% CI 1.26–2.15) and for males it is 1.37 (95% CI 0.94–2.02).
Moreover, the direct pathway from maternal orphanhood to HIV is more pronounced when the sample is limited to 15 year olds, in whom we’d expect less contribution from sexual activity (e.g., for double orphans, OR 3.07; 95% CI 1.75–5.40 for females and OR 3.46; 95% CI 1.79–6.71 for males; results not shown).
Further support for mother-to-child transmission comes from modeling other sexual outcomes. Sexually active respondents reported on STD symptomology. There are no statistically significant direct pathways from orphanhood to other STDs for either boys or girls (Figures 2.2 and 3.2). Again, there is one moderately significant indirect pathway from maternal orphaning to STDs in females. Risky sexual behavior follows the expected pattern in relation to STDs for both genders (OR 1.47; 95% CI 1.21–1.78 for females, OR 2.19; 95% CI 1.61–2.97 for males).
Evidence for sexual transmission: In contrast, there is no evidence that orphans take greater sexual risks. For both females (Figure 2.1) and males (Figure 3.1), the odds ratios between orphan status and sexual risk taking range from 0.87–1.15, and all 95% confidence intervals include the null. There is an inconsistent relationship between risk behavior and HIV positive status by gender: there is a positive association in females (OR 1.68; 95% CI 1.33–2.13), and a negative association in males (OR 0.53; 95% CI 0.34–0.52).
In secondary analyses, we find weak evidence for an indirect pathway to HIV mediated by sexual violence (Figure 2.3): double orphaning is associated with a higher likelihood of sexual violence (OR=1.41; 95% CI 1.04–1.93); this in turn increases sexual risk taking (OR 4.61; 95% CI 3.80–5.59). When all pathways between double orphaning and sexual risk are considered simultaneously, however, the net impact on HIV is not significant (OR 1.25; 95% CI 0.81–1.92; not explicitly shown in Figure 2.3).
Discussion
We find strong support that mother-to-child transmission is the primary explanation for higher HIV infection among adolescent orphans. Our results show that orphanhood is associated with HIV infection for both boys and girls, but is not strongly associated with sexual risk behavior or STDs for either. We also find greater excess HIV risk in maternal versus paternal orphans. Orphan disparities are more pronounced at younger ages, when sexual activity is less prevalent. The results are remarkably consistent for boys and girls. While sexual transmission undeniably contributed to HIV prevalence in the general adolescent population, mother-to-child transmission appears to be a stronger explanation for the higher HIV rates among orphaned adolescents.
The above results are consistent with both emerging clinical evidence that HIV progresses very slowly in some children,13,14 as well as the substantial burden of HIV among older children found in population surveys.15,16 Moreover, our study found little evidence that sexual risk behaviors were elevated among orphans. This is in contrast to select studies showing that female orphans have more multiple partnerships and transactional sex.5,26,27 More commonly, however, studies have failed to show any difference between orphans and non-orphans in sexual behavior4,5,28–31 or other STDs.29,32 We also tested other possible mediators in the relationship between orphanhood and HIV infection, such as STD infection and number of year sexually active. Analysis including these measures did not affect our conclusions or add substantively to our framework, and we therefore do not include in the final analysis in this research. Thus, our results are consistent with the picture emerging from this wider evidentiary base.
These results have important implications for policies and programs in Africa on HIV infection, and on orphanhood. For example, a dominant focus of adolescent HIV programs in Africa is on preventing infection by reducing sexual risk behavior.3 However, our results imply that a substantial percentage of a key adolescent risk group, the 13 million orphans in Africa,33 may already be infected. Reducing risk behaviors among these already-infected adolescents is still crucial to prevent the spread of HIV to their partners, but it will not help those already infected. In order to achieve “An AIDS-free generation”1, programs will need to identify and target the relevant at-risk groups. This research adds to the growing body of evidence that vertical transmission is of increasing importance, despite being under-recognized. Provision of ART while pregnant and breastfeeding may reduce vertical transmission, thereby reducing the proportion of HIV positive adolescents (and orphans). Such ART coverage is still limited and in need of expansion.34
Our results also reinforce the importance of promoting HIV testing for all adolescents. Studies have repeatedly shown that testing rates are low among adolescents.1 Many HIV positive adolescents may not believe they have any risk of infection: adolescents may be unaware of their parents’ status, even if they have passed away from an AIDS-related illness. Current testing campaigns primarily focus on sexual behavior and rarely address the possibility of undiagnosed maternal infection. The narrow focus on sexual risk behavior may give the mistaken impression that adolescents who are not sexually active are not HIV positive. All HIV-positive adolescents need timely diagnosis and treatment, and our results suggest that HIV testing programs should promote testing for all adolescents regardless of sexual behavior, and make efforts to ensure they are reaching orphans.
In part because they cannot be reached through HIV positive parents, it is particularly challenging to connect orphans to HIV testing and treatment programs.35 In a South African study, maternal orphans were diagnosed and initiated ARVs later than other HIV-infected children.35 Three quarters of the caregivers knew the child’s mother had died of an AIDS-related illness, yet most waited until the child was chronically ill to bring them in for HIV testing. The authors speculate that orphan caregivers – many of whom are grandparents and have little formal education – may be less aware of the need for early diagnosis. Orphans can also face another barrier to testing: the lack of a legal guardian to consent. For adolescent orphans specifically, laws that allow minors to self-consent to HIV testing could engender greater equity.34
The high burden of undiagnosed HIV among orphans specifically suggests greater challenges, but also a potential entry point. Many humanitarian and government programs are already serving orphaned adolescents, can play a pivotal role linking them to HIV testing, and can do so in a sensitive manner. Such organizations have often earned the trust of the adolescents and families that they serve, and can motivate all beneficiaries – regardless of orphan status - to make appointments with local clinics. They are well placed to recognize additional barriers (e.g., parental consent, secondary stigma) specific to orphans, and to help providers create more accessible testing programs. Working with local clinics, they can also help ensure that testing strategies are tailored specifically to the needs of children and adolescents. For instance, family-based and/or self-administered HIV testing may offer effective alternatives.10 Finally, while organizations that support orphans represent an excellent starting place, their reach remains limited. This highlights the importance of routine provider testing for all adolescents – again, regardless of sexual debut.
We call for more research on this emerging and important issue. While DHS data confers many benefits, its use for secondary analyses has limitations. Most notably, temporal ordering is a feature in our conceptual pathway, but cannot be fully evaluated with the available cross-sectional data. As mentioned above, we organized variables into the most probably causal pathway based on previous theoretical and empirical evidence. While it is unlikely that the sexual outcomes (sexual violence, risky behavior and HIV) cause orphanhood, there is far less certainty around the ordering of the sexual outcomes themselves. This may underlie one unexpected finding: sexual risk behavior appears to lower HIV risk among male adolescents. Risk behavior is positively correlated with other STDs, so misreporting of sexual activity is an unlikely explanation. Another possible explanation is recursive causation. The assumed pathway in our conceptual model is that risk behavior causes HIV infection. But the relationship between risk behavior and HIV positive status is likely more complicated. With testing increasingly available, male adolescents who know their positive status may take steps to reduce risk behavior. This is a new area of research, and a clear picture of how growing up HIV-positive affects sexual risk taking is yet to emerge. Longitudinal or population-based studies of early adolescence (prior to sexual debut) would provide more definitive evidence, but are generally lacking.
The reliance on self-reported measures of sensitive behaviors, such as sexual behavior and STD symptomology, may have implications for our research. Many studies have documented the lack of reliability or validity of self-reported sexual behavior, particularly among adolescents and young adults.36–39 This research has typically shown that women tend to under-report of sexual behavior, while men may either under-report or over-report sexual behavior. In general, misreporting of sexual behavior would likely make it more difficult to detect a relationship between sexual behavior and HIV infection, or could mean that a detected relationship is not estimated accurately. Differences in the patterns of misreporting may also explain differences in our results by men and women: although the relationship between risk behavior and HIV positive status is as expected for women, systematic misreporting may explain the negative association among men. Of greater concern would be systematic misreporting associated with HIV infection and orphanhood: if HIV infected orphans were systematically less likely report sexual risk behavior, this would lead to potentially biased results. That said, we have no reason to think this is the case: misreporting sexual behavior is likely to be similar between orphans and non-orphans, and between maternal and paternal orphans. There is, however, limited research on patterns of reporting sexual behavior among orphans specifically, and such research could potentially provide more insight into the extent that misreporting of sexual behavior affects our results. The data on sexual violence may also be particularly prone to reporting bias. Still, we demonstrate strong pathways from victimization to sexual risk taking and to HIV. There is little rigorous evidence on what works to prevent childhood sexual abuse, though we refer interested readers to a new WHO report on strategies that show promise.40 Another measurement limitation is our use of proxies - orphan status and sexual behavior - to measure maternal and sexual transmission respectively. While we build a circumstantial case for maternal transmission, it is only as strong as these proxies.
Finally, although our sample is limited to adolescents aged 15–17 due to data availability, this research is highly relevant for other age groups. As recent research has shown, HIV prevalence among older children younger than age 15 is not negligible and vertical transmission is likely the primary mode of infection. Yet data on HIV infection, testing, and associated behaviors is severely lacking for this population.3 This research joins calls from elsewhere for more HIV testing to be made available to adolescents before sexual debut.15,16
Implications and Contribution.
Adolescent orphans are a high-risk group for HIV in Africa, and explanations focus on heightened sexual risk taking during adolescence. However, these results show that maternal transmission is a more likely explanation. New efforts to identify and test undiagnosed HIV among orphans are key to reducing adolescent AIDS mortality.
Acknowledgments
This research was funded by the Eunice Kennedy Shriver National Institute Of Child Health & Human Development of the National Institutes of Health under Award Number R03HD082475. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.UNICEF. Children, Adolescents and AIDS: 2015 Statistical Update. 2015 [Google Scholar]
- 2.United Nations Children’s Fund (UNICEF) UNICEF Analysis of UNAIDS 2012 HIV and AIDS Estimates. New York, NY: UNICEF; 2013. [Google Scholar]
- 3.Idele P, Gillespie A, Porth T, et al. Epidemiology of HIV and AIDS Among Adolescents: Current Status, Inequities, and Data Gaps. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2014;66:S144–S53. doi: 10.1097/QAI.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 4.Nyirenda M, McGrath N, Newell M-L. Gender differentials in the impact of parental death: Adolescent’s sexual behaviour and risk of HIV infection in rural South Africa. Vulnerable Children and Youth Studies. 2010;5(3):284–96. doi: 10.1080/17450128.2010.507804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Operario D, Pettifor A, Cluver L, MacPhail C, Rees H. Prevalence of parental death among young people in South Africa and risk for HIV infection. Journal of Acquired Immune Deficiency Syndromes. 2007;44:93–8. doi: 10.1097/01.qai.0000243126.75153.3c. [DOI] [PubMed] [Google Scholar]
- 6.Kidman R, Anglewicz P. Are adolescent orphans more likely to be HIV-positive? A pooled data analyses across 19 countries in sub-Saharan Africa. Journal of epidemiology and community health. 2016 doi: 10.1136/jech-2015-206744. jech-2015-206744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Operario D, Underhill K, Chuong C, Cluver L. HIV infection and sexual risk behaviour among youth who have experienced orphanhood: systematic review and meta-analysis. Journal of the International AIDS Society. 2011;14(1):1–11. doi: 10.1186/1758-2652-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunbar MS, Maternowska MC, Kang M-SJ, Laver SM, Mudekunye-Mahaka I, Padian NS. Findings from SHAZ!: a feasibility study of a microcredit and life-skills HIV prevention intervention to reduce risk among adolescent female orphans in Zimbabwe. Journal of Prevention & Intervention in the Community. 2010;38(2):147–61. doi: 10.1080/10852351003640849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nyberg BJ, Yates DD, Lovich R, et al. Saving Lives for a Lifetime: Supporting Orphans and Vulnerable Children Impacted by HIV/AIDS. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2012;60:S127–S35. doi: 10.1097/QAI.0b013e31825da836. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. HIV and adolescents: Guidance for HIV testing and counselling and care for adolescents living with HIV: recommendations for a public health approach and considerations for policy-makers and managers. 2013 [PubMed] [Google Scholar]
- 11.Nyberg BJ, Yates DD, Lovich R, et al. Saving lives for a lifetime: supporting orphans and vulnerable children impacted by HIV/AIDS. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2012;60:S127–S35. doi: 10.1097/QAI.0b013e31825da836. [DOI] [PubMed] [Google Scholar]
- 12.Sherr L, Cluver L, Betancourt T, Kellerman S, Richter L, Desmond C. Evidence of impact: health, psychological and social effects of adult HIV on children. AIDS. 2014;28:S251–S9. doi: 10.1097/QAD.0000000000000327. [DOI] [PubMed] [Google Scholar]
- 13.Stover J, Walker N, Grassly NC, Marston M. Projecting the demographic impact of AIDS and the number of people in need of treatment: updates to the Spectrum projection package. Sexually Transmitted Infections. 2006;82(Suppl 3):iii45–iii50. doi: 10.1136/sti.2006.020172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marston M, Becquet R, Zaba B, et al. Net survival of perinatally and postnatally HIV-infected children: a pooled analysis of individual data from sub-Saharan Africa. International Journal of Epidemiology. 2011 doi: 10.1093/ije/dyq255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng’eno B, Mwangi A. Burden of HIV Infection Among Children Aged 18 Months to 14 Years in Kenya: Results From a Nationally Representative Population-Based Cross-sectional Survey. Journal of acquired immune deficiency syndromes (1999) 2014;66(Suppl 1):S82. doi: 10.1097/QAI.0000000000000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pegurri E, Konings E, Crandall B, et al. The missed HIV-positive children of Ethiopia. PloS one. 2015;10(4):e0124041. doi: 10.1371/journal.pone.0124041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luseno W, Zhang L, Rusakaniko S, Cho H, Hallfors D. HIV infection and related risk behaviors: does school support level the playing field between orphans and nonorphans in Zimbabwe? AIDS Care. 2015;27(9):1191–5. doi: 10.1080/09540121.2015.1036726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corsi DJ, Neuman M, Finlay JE, Subramanian S. Demographic and health surveys: a profile. International Journal of Epidemiology. 2012;41(6):1602–13. doi: 10.1093/ije/dys184. [DOI] [PubMed] [Google Scholar]
- 19.Mishra V, Vaessen M, Boerma J, et al. HIV testing in national population-based surveys: experience from the Demographic and Health Surveys. Bulletin of the World Health Organization. 2006;84(7):537–45. doi: 10.2471/blt.05.029520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen L, Jha P, Stirling B, et al. Sexual Risk Factors for HIV Infection in Early and Advanced HIV Epidemics in Sub-Saharan Africa: Systematic Overview of 68 Epidemiological Studies. PLoS ONE. 2007;2(10):e1001. doi: 10.1371/journal.pone.0001001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weller S, Davis-Beaty K. Condom effectiveness in reducing heterosexual HIV transmission (Review) The Cochrane Library. 2007;4:1–24. doi: 10.1002/14651858.CD003255. [DOI] [PubMed] [Google Scholar]
- 22.Kishor S. Domestic violence measurement in the demographic and health surveys: The history and the challenges: UN Division for the Advancement of Women. 2005 [Google Scholar]
- 23.Kidman R, Palermo T. The relationship between parental presence and child sexual violence: evidence from thirteen countries in sub-Saharan Africa. Child abuse & neglect. 2016;51:172–80. doi: 10.1016/j.chiabu.2015.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bryan A, Schmiege SJ, Broaddus MR. Mediational analysis in HIV/AIDS research: Estimating multivariate path analytic models in a structural equation modeling framework. AIDS Behav. 2007;11(3):365–83. doi: 10.1007/s10461-006-9150-2. [DOI] [PubMed] [Google Scholar]
- 25.Eaton JW, Garnett GP, Takavarasha FR, et al. Increasing Adolescent HIV Prevalence in Eastern Zimbabwe – Evidence of Long-Term Survivors of Mother-to-Child Transmission? PLoS ONE. 2013;8(8):e70447. doi: 10.1371/journal.pone.0070447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cluver L, Orkin M, Boyes M, Gardner F, Meinck F. Transactional Sex Amongst AIDS-Orphaned and AIDS-Affected Adolescents Predicted by Abuse and Extreme Poverty. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2011;58(3):336–43. doi: 10.1097/QAI.0b013e31822f0d82. [DOI] [PubMed] [Google Scholar]
- 27.Nyamukapa CA, Gregson S, Lopman B, et al. HIV-associated orphanhood and children’s psychosocial distress: Theoretical framework tested with data from Zimbabwe. American Journal of Public Health. 2008;98(1):133–41. doi: 10.2105/AJPH.2007.116038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Juma M, Alaii J, Bartholomew LK, Askew I, den Borne B. Risky Sexual Behavior Among Orphan and Non-orphan Adolescents in Nyanza Province, Western Kenya. AIDS Behav. 2013;17(3):951–60. doi: 10.1007/s10461-012-0336-5. [DOI] [PubMed] [Google Scholar]
- 29.Gregson S, Nyamukapa C, Garnett G, et al. HIV infection and reproductive health in teenage women orphaned and made vulnerable by AIDS in Zimbabwe. AIDS Care. 2005;17(7):785–94. doi: 10.1080/09540120500258029. [DOI] [PubMed] [Google Scholar]
- 30.Chae S. Timing of Orphanhood, Early Sexual Debut, and Early Marriage in Four Sub-Saharan African Countries. Studies in Family Planning. 2013;44(2):123–46. doi: 10.1111/j.1728-4465.2013.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kidman R, Anglewicz P. Fertility Among Orphans in Rural Malawi: Challenging Common Assumptions About Risk and Mechanisms. International Perspectives on Sexual and Reproductive Health. 2014;40(4):164–75. doi: 10.1363/4016414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kang M, Dunbar M, Laver S, Padian N. Maternal versus paternal orphans and HIV/STI risk among adolescent girls in Zimbabwe. AIDS Care. 2008;20(2):214–7. doi: 10.1080/09540120701534715. [DOI] [PubMed] [Google Scholar]
- 33.UNICEF. Towards an AIDS-Free Generation–Children and AIDS: Sixth Stocktaking Report. New York: UNICEF; 2013. [Google Scholar]
- 34.Sam-Agudu NA, Folayan MO, Ezeanolue EE. Seeking wider access to HIV testing for adolescents in sub-Saharan Africa. Pediatric research. 2016;79(6):838–45. doi: 10.1038/pr.2016.28. [DOI] [PubMed] [Google Scholar]
- 35.Mokgatle MM, Madiba S. The burden of disease on HIV-infected orphaned and non-orphaned children accessing primary health facilities in a rural district with poor resources in South Africa: a cross-sectional survey of primary caregivers of HIV-infected children aged 5–18 years. Infectious diseases of poverty. 2015;4(1):1. doi: 10.1186/s40249-015-0049-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mensch BS, Hewett PC, Erulkar AS. The reporting of sensitive behavior by adolescents: a methodological experiment in Kenya. Demography. 2003;40(2):247–68. doi: 10.1353/dem.2003.0017. [DOI] [PubMed] [Google Scholar]
- 37.Curtis SL, Sutherland EG. Measuring sexual behaviour in the era of HIV/AIDS: the experience of Demographic and Health Surveys and similar enquiries. Sexually Transmitted Infections. 2004;80(suppl 2):ii22–ii7. doi: 10.1136/sti.2004.011650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maughan-Brown B, Venkataramani AS. Measuring concurrent partnerships: potential for underestimation in UNAIDS recommended method. Aids. 2011;25(12):1549–51. doi: 10.1097/QAD.0b013e32834905c4. [DOI] [PubMed] [Google Scholar]
- 39.Nnko S, Boerma JT, Urassa M, Mwaluko G, Zaba B. Secretive females or swaggering males?: An assessment of the quality of sexual partnership reporting in rural Tanzania. Social science & medicine. 2004;59(2):299–310. doi: 10.1016/j.socscimed.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization. INSPIRE: seven strategies for ending violence against children. Geneva: 2016. [Google Scholar]


