Abstract
Purpose
To assess the relationship of binocular visual function tests with binocular approximations, using data from the Collaborative Initial Glaucoma Treatment Study (CIGTS).
Design
Case series based on existing data from a clinical trial
Subjects
607 subjects with newly diagnosed open-angle glaucoma from the CIGTS.
Methods
Monocular visual field (VF) and visual acuity (VA) tests were taken at baseline and every 6 months thereafter. Binocular tests of visual function (Esterman VF score; binocular VA) were added to the CIGTS protocol 3 years into study. The binocular approximations of binocular visual function were better/worse eye, average eye, better/worse location, and binocular summation/pointwise binocular summation. Associations between binocular tests and binocular approximations to represent binocular visual function were assessed with Pearson’s correlations (r), as was the relationship between vision-related quality of life [VR-QOL; Visual Activities Questionnaire (VAQ) and the National Eye Institute Visual Function Questionnaire (NEI-VFQ25)] and binocular tests or binocular approximations of visual function.
Main Outcome Measures
Binocular visual function (VF and VA), and VR-QOL
Results
575 subjects had at least one binocular visual function test. The Esterman score was significantly correlated with all binocular approximations of VF, with r-values ranging from 0.31 (worse eye mean deviation, MD) to 0.42 (better eye MD, all p<0.0001). Binocular VA showed stronger correlations with binocular approximations, with r-values ranging from 0.65 (worse eye VA) to 0.80 (binocular summation, all p<0.0001). Correlations between the VAQ and Esterman score were stronger in 7 of 9 subscales (r =−0.14 to −0.25, all p<0.05) than correlations with all 7 binocular approximations. In contrast, correlations between the VAQ and binocular VA (r=−0.07 to −0.21) were weaker in all subscales than those with better eye, average eye, and binocular summation of VA (r=−0.12 to −0.25), but not different from worse eye. These trends were also found in relevant subscales of the NEI-VFQ25.
Conclusions
We found limited benefit in binocular testing of VA in the clinical setting as a means of approximating a patient’s reported visual functioning. In contrast, we found some benefit in performing binocular VF testing, as the results correlated more closely with reported functioning than binocular approximations.
In the clinical assessment of glaucoma, common clinical tests are performed on each eye (monocularly) in typical eye care settings. Likewise, most major clinical trials of glaucoma treatment, as well as population-based epidemiological studies that assessed glaucoma incidence or prevalence, have relied on monocular testing of visual function, including visual field (VF), visual acuity (VA), and less frequently contrast sensitivity. These tests do not always relate closely to how well the patient is functioning in daily life. Therefore, patient-reported outcome (PRO) questionnaires were developed to assess vision-related quality of life (VR-QOL). Many of these questionnaires, such as the Visual Activities Questionnaire (VAQ)1 and the more commonly-used 25-item National Eye Institute Visual Function Questionnaire (NEI-VFQ25),2 include a domain or a set of questions relating to how the respondent is functioning in common activities of daily life that require good vision.
The collection of monocular and binocular tests of visual function used in the Collaborative Initial Glaucoma Treatment Study (CIGTS) permitted a unique opportunity to investigate the value of binocular measures. Mills et al.3 evaluated the association between better or worse eye VF measures and the VAQ, using baseline information collected on CIGTS participants. We expanded upon this work by exploring the extent to which various ways of combining vision tests conducted on each eye approximate binocular function. We also investigated the associations of binocular tests and binocular approximations with VR-QOL.
Methods
Six hundred seven subjects with newly diagnosed open-angle glaucoma (OAG) were enrolled in the CIGTS at 14 clinical centers from 1993 to 1997. After providing informed consent, subjects were randomized to receive either topical medication or surgery as the initial treatment of their OAG and were followed every 6 months through 2004. Although a study eye was designated at baseline, both eyes received the same, carefully standardized testing throughout follow-up. All testing was conducted by CIGTS personnel who were certified for the specific test conducted, and the CIGTS protocol dictated the testing conditions (e.g., lane length & ambient lighting) and procedures.4
Monocular measures of visual function collected at baseline and over follow-up included the mean deviation (MD) from the Humphrey 24-2 full-threshold VF test and best-corrected VA from Early Treatment Diabetic Retinopathy Study (ETDRS) VA testing.5,6 The MD is a measure of overall VF depression calculated by averaging the differences at each test location between the patient’s measure and the corresponding age-corrected normal value.7 MD values range from −30.0 to +5 dB, with more positive measurements indicating better visual function. The ETDRS VA measures the number of letters correctly identified on an ETDRS VA chart. As used in the CIGTS, its values range from 0 to 100 letters, with higher values indicating better visual function (e.g., a score of 85 is equivalent to 20/20 VA). Binocular tests of visual function were added to the CIGTS protocol 3 years into the study and included the Esterman binocular VF test8 and binocular testing of VA. The Esterman VF test is a suprathreshold test (a size III white stimulus is used with an intensity of 10 dB) in which a grid of 120 test points is presented. More than 130 degrees of the VF are examined. A score is generated from the Humphrey software, ranging from 0 to 100%, based on the percentage of the 120 VF test points that were correctly detected during binocular VF testing (in which the patient uses both eyes). Binocular VA was measured using the same method as monocular measures and scaled accordingly, excepting the lack of binocular testing at 1 meter, which was done only for a monocular VA test result that yielded less than 20 letters read correctly at four meters (<20/100). To account for this difference in measurements, we deleted from comparative use any VA test result (monocular or binocular) that was <20/100.
Methods to approximate binocular VA and binocular VF (“binocular approximations”) included the better eye, worse eye, and average eye measures, calculated using the maximum, minimum, and mean of measures (MD or VA) between eyes of a subject, respectively. Better eye and worse eye status were defined by baseline measures of visual function and held constant over time even when follow-up measures would otherwise redefine the status. Binocular summation measures were calculated as the square root of the summed squares of the two monocular measures (for either MD or VA).9 Better eye and worse eye location measures were calculated only for MD, using data from each of the 52 points of the total deviation probability plot. Each point of the plot was scored based on the VF output that provides significance of the deviation from the Humphrey software’s data on normal subjects as follows: 0=p≥5%, 1=p<5%, 2=p<2%, 3=p<1%, 4=p<0.5%. Points between eyes were compared by superimposing along the central axis to mimic binocular vision, rather than flipping over the axis to line up points based on corresponding quadrants. This created 56 unique locations due to points that did not overlap in the periphery. Corresponding locations in each eye were compared to determine the better location score (minimum) and the worse location score (maximum) for each of the 56 points. The average better (worse) location score was then calculated as the mean of the 56 better (worst) pointwise scores. Lastly, pointwise binocular summation measures were calculated for each of the 56 locations using the total deviation probability scores. The mean of these 56 measures was taken as the average pointwise binocular summation.9
In addition to clinical measures, the CIGTS obtained VR-QOL information via telephone-administered interviews conducted at baseline and every 6 months throughout follow-up. The interview included administering the VAQ1 and the NEI-VFQ25,2 which assess patients’ perceptions of their visual functioning and the impact of visual problems on their daily activities. When the trial was planned, the VAQ was selected as the most relevant condition-specific measure of visual function status available. After enrollment was complete and CIGTS participants were being followed, the NEI-VFQ25 became available, which was first administered at the 54-month follow-up and annually thereafter.
The 33-item VAQ1 obtains the person’s report of their ability to perform everyday tasks and activities of daily living involving vision. Each item describes a potential vision problem and asks how often this problem occurs on a five-point scale from 1 (never) to 5 (always), or “not applicable.” The VAQ includes eight subscales: color discrimination, glare disability, light-dark adaptation, acuity/spatial vision, depth perception, peripheral vision, visual search, and visual processing speed. The VAQ total score and subscale scores were calculated as a mean of all items, or the items in that subscale, respectively. Scores ranged from 1 to 5 with higher scores indicate worse visual functioning.
The NEI-VFQ252 is a reduced 25-item version of a 51-item questionnaire developed based on focus groups conducted with patients who had cataract, macular degeneration, diabetic retinopathy, primary open-angle glaucoma, cytomegalovirus retinitis, or low vision from any cause.9 The NEI-VFQ25 yields a total score that includes all items except one that asks about general health. In addition, twelve subscale scores can be computed: general health, general vision, near vision, distance vision, driving, peripheral vision, color vision, and ocular pain as well as vision-specific role limitations, dependency, social function, and mental health. The NEI-VFQ25 is scored as an un-weighted average of the included items transformed to a 0 to 100 scale, with higher scores indicating better visual functioning. This study was approved by the Institutional Review Board, was HIPPA compliant, and adhered to the tenets of the Declaration of Helsinki. The CIGTS is registered on clinicaltrials.gov (NCT00000149).
Statistical Methods
Descriptive statistics were calculated for patient characteristics as well as for all VA and VF measures using means and standard deviations (SD) for continuous variables, and frequencies and percentages for categorical variables. Stability of VA and VF was assessed using correlations of measures at consecutive visits over time. A line plot was used to display correlations between visits over time.
Associations between binocular approximations and binocular tests of VA and VF (obtained from the same visit) were assessed using Pearson correlations (r). Correlation analysis was performed using data from all time points with available binocular measures, and at a 5-year cross-section. Linear mixed regression modeling was used to test the ability of the relevant binocular approximation to predict the corresponding binocular test (obtained from the Esterman binocular VF and binocular VA tests). Multivariable models were investigated by including all binocular approximations of VF and VA and used step-wise procedures (best-subset models and backward selection) to determine which binocular approximations best predicted the result from testing binocular visual function (Esterman binocular VF or binocular VA). These models accounted for correlation among the repeated measures taken on a subject over time, and model fit statistics were compared between univariate and multivariable models.
Associations between VR-QOL measures and both binocular approximations and binocular testing of VA and VF were assessed using Pearson correlations. Univariate and multivariable linear mixed regression models were also used to assess the clinical measure most predictive of VR-QOL based on fit statistics. Multivariable models used step-wise procedures to determine which measures best predicted the VR- QOL. SAS version 9.4 was used for all statistical analysis (SAS Institute, Cary, NC).
Results
Of the 607 CIGTS subjects, 575 (95%) had at least one binocular VF or VA test. Since binocular tests of VA and VF were added 34 months into the study, which was 8 months prior to the conclusion of enrollment, we had binocular test results for only 37 subjects at baseline, and no measurements for 32 subjects who were lost to follow-up prior to binocular test initiation. Most subjects (91%) had their first binocular test of visual function taken by 3 years after enrollment (range 0–8 years). The 32 subjects who had no binocular testing of visual function were similar to the complementary group in all demographic and clinical variables except baseline IOP in the study eye, which was lower in subjects with no binocular testing (26.1 mmHg vs. 27.6 mmHg, respectively; p=0.0273).
The 575 subjects who had at least one binocular test were on average 58 years old (SD=10.9), 55% male, 56% White, and 17% reported having diabetes (Table 1); they had mean follow-up of 7.5 years (range 0.7 to 11.3 years) from enrollment. The average baseline MD of the study eye was −5.5 dB (SD=4.3 dB) and the average baseline VA was 85.7 letters (SD=5.7 letters).
Table 1.
Descriptive statistics for the subset of subjects with at least 1 binocular visual field or visual acuity test (n=575)
| Continuous Variables | Mean (SD) | Min, Max |
|---|---|---|
| Age | 58.0 (10.9) | 28.8, 75.8 |
| Baseline MD - study eye | −5.5 (4.3) | −23.5, 3.4 |
| Baseline VA - study eye | 85.7 (5.7) | 70.0, 99.0 |
| Baseline IOP - study eye | 27.6 (5.7) | 19.0, 50.0 |
| Follow-up (years) | 7.5 (1.9) | 0.7, 11.3 |
| Baseline VAQ score | 2.0 (0.7) | 1.0, 4.4 |
| 4.5 year NEI-VFQ score (n=380) | 91.8 (8.9) | 31.5, 100.0 |
| Categorical Variables | Frequency (Percent ) | |
|
| ||
| Gender | ||
| Male | 316 (55.0) | |
| Female | 259 (45.0) | |
| Race | ||
| White | 323 (56.2) | |
| Black | 216 (37.6) | |
| Asian | 9 (1.6) | |
| Other | 27 (4.7) | |
| Diabetes | 95 (16.5) | |
| Hypertension | 216 (37.6) | |
SD = Standard Deviation; Min = Minimum; Max = Maximum; MD = Mean Deviation; VA = Visual Acuity; IOP = Intraocular Pressure; VAQ = Visual Activities Questionnaire; NEI-VFQ = National Eye Institute Visual Function Questionnaire
Table 2 summarizes baseline descriptive statistics on each of the binocular approximations. Binocular tests of visual function (Esterman test for binocular VF and binocular VA) are also summarized descriptively at the time of first binocular test. On average, baseline MD of the better eye (worse eye) was −2.5 dB (−5.7 dB) and baseline VA of the better eye (worse eye) was 87.9 letters (84.2 letters). Average better eye location was 0.36 units (SD=0.44 units) and average worse eye location was 1.29 units (SD=0.91 units). Binocular summation for MD was on average 6.5 dB (SD=4.7 dB) and was 121.8 letters (SD=6.9 letters) for VA. Binocular measures of visual function averaged 85.9 letters for VA (SD=6.4 letters) and 95.5% for the Esterman score (SD=6.1).
Table 2.
Definitions and descriptive statistics of visual function (visual field and visual acuity) for binocular tests and binocular approximations
| Measured at First Binocular Test | ||||
|---|---|---|---|---|
| Variables (n=575) | Definition | Directionality | Mean (SD) | Min, Max |
| Binocular Tests | ||||
| Binocular VA (n=573) | VA measured using both eyes | ↑ Better | 85.9 (6.4) | 50.0, 100.0 |
| Esterman Efficiency Score (n=535) | Percent of 120 VF test points correctly identified using both eyes | ↑ Better | 95.5 (6.1) | 48.0, 100.0 |
| Binocular Approximations | Measured at Baseline | |||
| Better Eye MD | Maximum of Right Eye MD, Left Eye MD | ↑ Better | −2.47 (2.70) | −18.07, 3.38 |
| Worse Eye MD | Minimum of Right Eye MD, Left Eye MD | ↑ Better | −5.72 (4.35) | −23.55, 1.88 |
| Average Eye MD | (Right Eye MD + Left Eye MD)/2 | ↑ Better | −4.09 (3.17) | −18.62, 2.63 |
| Better Eye VA | Maximum of Right Eye VA, Left Eye VA | ↑ Better | 87.9 (4.8) | 70.0, 100.0 |
| Worse Eye VA | Minimum of Right Eye VA, Left Eye VA | ↑ Better | 84.2 (5.6) | 70.0, 99.0 |
| Average Eye VA | (Right Eye VA + Left Eye VA)/2 | ↑ Better | 86.1 (4.9) | 70.0, 99.5 |
| Binocular Summation MD | √(Right Eye MD2 + Left Eye MD2) | ↓ Better | 6.54 (4.71) | 0.26, 26.34 |
| Binocular Summation VA | √(Right Eye VA2 + Left Eye VA2) | ↑ Better | 121.8 (6.9) | 99.0, 140.7 |
| Better Location* | [Min Pt1 (LE, RE) + Min Pt2 (LE, RE) + …. + Min Pt56 (LE, RE)]/56 | ↓ Better | 0.36 (0.44) | 0.00, 2.52 |
| Worse Location* | [Max Pt1 (LE, RE) + Max Pt2 (LE, RE) + …. + Max Pt56 (LE, RE)]/56 | ↓ Better | 1.29 (0.91) | 0.00, 3.78 |
| Pointwise Binocular Summation* | [√(RE Pt12+LE Pt12) + √(RE Pt22+LE Pt22) +….+ √(RE Pt562+LE Pt562)]/56 | ↓ Better | 1.37 (1.00) | 0.00, 4.39 |
based on the visual field total deviation plot points scored as 0=p≥0.05, 1=p<0.05, 2=p<0.02, 3=p<0.01, 4=p<0.005 for the probability of deviation from normal values
SD = Standard Deviation; MD = Mean Deviation; VA = Visual Acuity; RE = Right Eye; LE = Left Eye; Pt = Point, for the 56 points in the superimposed RE and LE fields; Min = Minimum; Max = Maximum
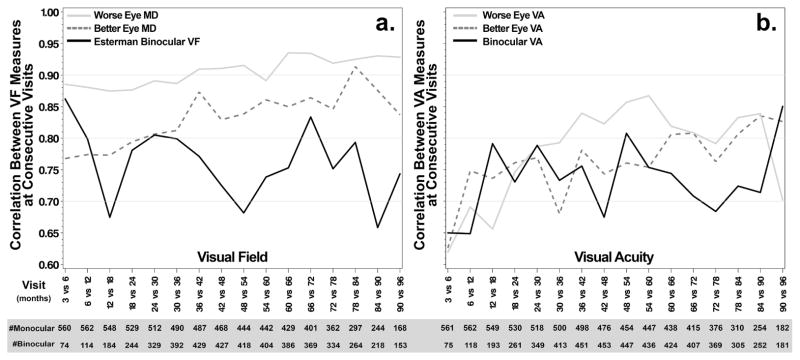
The correlations between better or worse eye MD measures taken at consecutive visits over follow-up (e.g., 3 vs. 6 months, 6 vs. 12 months) were large, ranging from 0.77 (for 3 vs. 6 months) to 0.91 (for 78 vs. 84 months) for better eye MD, and ranging from 0.87 (for 12 vs. 18 months) to 0.94 (for 60 vs. 66 months) for worse eye MD. These correlations increased over follow-up time (Figure 1a). For Esterman VF, the corresponding correlations were somewhat smaller (ranging from 0.66 to 0.86). Correlations between consecutive visits for better eye or worse eye VA measures were moderate to large and also increased over time (ranging from 0.63 to 0.84 for better eye and from 0.62 to 0.87 for worse eye; Figure 1b). Correlations between measures of binocular VA at consecutive visits were similar in magnitude to the better eye correlations, but mostly smaller than worse eye correlations. In general, the binocular test of VF and VA showed greater variability in the pairwise correlations over time compared to that observed for binocular approximations; however, larger variability of binocular tests before 24 months may be influenced by smaller sample sizes, which also occurs with all measurements taken at 90+ months. Correlations gradually decreased between measurements taken at non- consecutive visits further apart in time, such that, for example, measures taken at 3 and 12 months were generally more correlated with each other than measures taken at 3 and 60 months or 3 and 90 months (Supplemental eFigures 1a–f; available at http://www.aaojournal.org).
Figure 1.
Correlations between measures at consecutive visits over time for binocular tests and binocular approximations of (a) visual field and (b) visual acuity
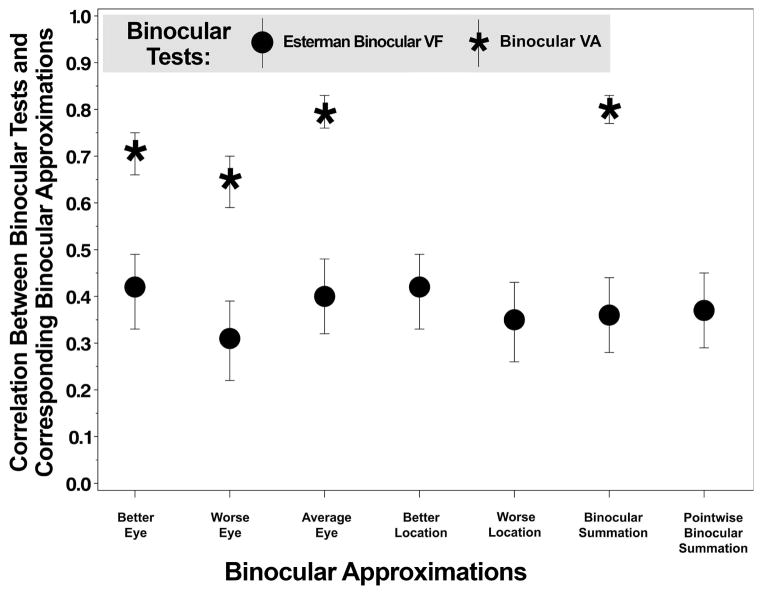
Correlations between binocular tests and binocular approximations (both obtained at the 5-year cross-section of follow-up) are displayed in Figure 2. The Esterman score was significantly correlated with all binocular approximations of MD, with correlations ranging from 0.31 (worse eye MD) to 0.42 (better eye MD, all p<0.0001). Binocular VA showed larger correlations with binocular approximations, with correlations ranging from 0.65 (worse eye VA) to 0.80 (binocular summation, all p<0.0001). Sensitivity analyses showed similar correlations when using data from all available follow-up visits (Supplemental eTable 1; available at http://www.aaojournal.org).
Figure 2.
Correlations between binocular tests of visual function and corresponding binocular approximations, all measured at a 5-year cross-section
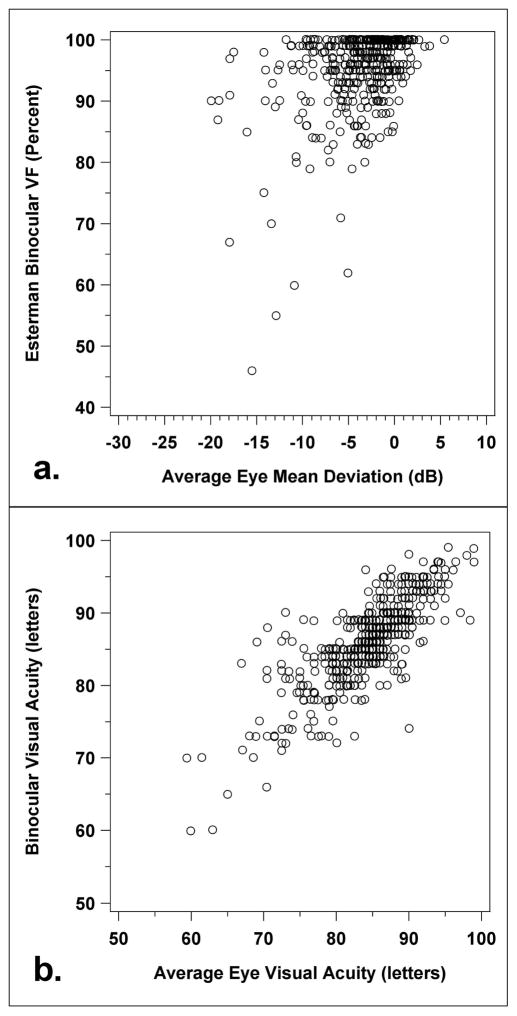
Figure 3 shows scatterplots illustrating the correlation between (a) average eye MD (dB) and Esterman binocular VF (percent), and (b) average eye VA (letters) and binocular VA (letters), all measured at the 5-year cross-section of follow-up. Esterman binocular VF is not as well predicted by average eye MD as binocular VA is predicted by average eye VA. Specifically, the distribution of average eye MD measures ranged from −20.9 dB to +5.4 dB and reflected a slight skew toward lower values. In contrast, most Esterman binocular VF values were above 90% and showed a strong ceiling effect at 100%, with outliers trailing toward the lower values (Figure 3a). Alternatively, a clear positive linear trend was observed between increasing binocular VA with increasing average eye VA (Figure 3b).
Figure 3.
Scatterplot of (a) Esterman binocular visual field versus average eye mean deviation and (b) binocular visual acuity versus average eye visual acuity, all measured at a 5-year cross-section
Supplemental eTable 2 (available at http://www.aaojournal.org) displays model fit statistics for univariate and best subset multivariable linear models predicting binocular visual function from the binocular approximations. Fit statistics indicate that the best binocular approximations to predict binocular visual function are better eye and better location for VF and binocular summation for VA. Multivariable models provided minimal improvement over single variable models (R2 increased from 0.25 to 0.27 for the linear models of VF; R2 increased from 0.81 to 0.85 for the linear models of VA).
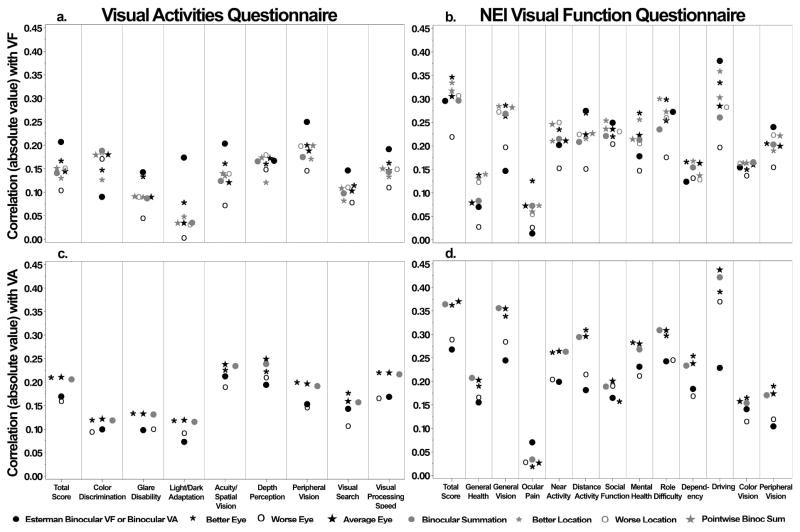
Correlations of VR-QOL measures with binocular test results and binocular approximations, all obtained at a 5.5-year cross-section of follow-up, are displayed in Figures 4a–4d. The Esterman binocular VF score showed higher correlations with the VAQ than all binocular approximations in 7 of 9 subscales of the VAQ (r =−0.14 to −0.25, all p<0.05). In contrast, binocular VA was less correlated with the VAQ in all subscales (r=−0.07 to −0.21) than correlations with most of the binocular approximations of VA (better eye, average eye, and binocular summation of VA, r=−0.09 to −0.25). Correlations between the worse eye VA and the VAQ were similar to those observed between binocular VA and VAQ. These trends were also found in relevant subscales of the NEI-VFQ25 (peripheral vision, distance activities, driving).
Figure 4.
Correlations of quality of life measures with binocular tests and binocular approximations of visual function measures, all obtained at a 5.5-year cross-section of follow-up (to maximize sample size). Correlations include total and subscale scores of the (a) VAQ with visual field, (b) NEI-VFQ with visual field, (c) VAQ with visual acuity, and (d) NEI-VFQ with visual acuity. VAQ = Visual Activities Questionnaire; NEI-VFQ = National Eye Institute Visual Function Questionnaire; VF = Visual Field; VA = Visual Acuity
Supplemental eTable 3 (available at http://www.aaojournal.org) displays model fit statistics for univariate and best subset multivariable models predicting VR-QOL from binocular tests and binocular approximations. All measures of visual function, whether binocular tests or approximations, were significantly associated with VR-QOL in univariate models; however, all associations were modest and reflected limited explanatory value (R2 values <0.19). Multivariable models showed little improvement in model fit. Models predicting the NEI-VFQ25 total score had greater explained variation than comparable models predicting the VAQ total score.
Discussion
Binocular vision allows the ability to perceive three-dimensional structure (stereopsis), which enhances visual function. Most people receive visual input from both eyes, and PROs that assess visual function are based on binocular vision, yet tests that are routinely conducted in clinical practice are monocular measures. This disconnect raises the question of whether the association between PROs and clinical tests of VA and VF would improve if binocular rather than monocular measures were used. It would be ideal if there were some way of using these commonly obtained monocular tests to approximate well what the patient is experiencing using both eyes.
This study had two goals. The first goal was to explore various approaches to combining monocular tests to optimally approximate binocular tests of visual function. The second goal was to compare the relative strength of associations between PROs and both binocular tests and various binocular approximations.
We found that measured binocular VA was well estimated by binocular approximations. Correlations ranged from 0.65 to 0.80 for the four binocular VA approximations we evaluated, with the highest correlations shown for the average of the two eye’s monocular tests (0.79) and the binocular summation formula (0.80). In the Los Angeles Latino Eye Study (LALES),10 wherein binocular and monocular VA test results were available on 1,831 subjects, correlation between the average of the two eye’s monocular VA tests with the binocular VA test was not reported, but the correlation between better eye VA and binocular VA was 0.93, which is much stronger than the correlation we found (0.71). In both the LALES and our results, the better eye VA correlated more strongly with binocular VA than the worse eye VA (0.93 vs. 0.72 for LALES and 0.71 vs. 0.65 for CIGTS, respectively). These results indicate that in the absence of access to actual binocular VA measures, the average of the two eyes’ VA or the better eye VA provide a quite strong correlation with binocular VA.
In contrast to VA, we found that binocular VF (using the Esterman test) was not well estimated by any binocular approximation approach we evaluated. While all correlations between binocular VF test results and binocular approximations differed significantly from zero (p<0.0001), they were weak to modest in strength, ranging from 0.31 to 0.42. We attribute these modest correlations to an evident ceiling effect in Esterman test scores (Figure 3a), wherein almost 9 out of every 10 Esterman scores were 90% or higher. This is similar to the clustering of Esterman scores between 80% and 100% reported by Jampel,11 who noted that this narrow range of values may limit the ability to relate Esterman scores with other measures of visual function. Our CIGTS participants’ average eye MD values were mostly in the −10 to 0 dB range at five years post-treatment; in this range, the ceiling effect of the Esterman score masked any association. In the CIGTS participants who had average eye MD values that were less than −10 dB, nearly the entire range of Esterman scores was observed, which calls into question the usefulness of the Esterman score or, alternatively, our ability to combine monocular MD measures to approximate the Esterman score.
Correlations of both binocular tests and binocular approximations (VA and VF) with the PRO questionnaires showed results that differed for VA and VF. For VA, correlations with the VAQ were generally weak (e.g., correlations between total VAQ score and VA measures ranged from 0.16 to 0.21). Binocular approximations of VA showed correlations with the VAQ that were generally better than those with the actual binocular test of VA. The better eye, average eye, and binocular summation measures of VA demonstrated the highest correlations with the total VAQ score and most VAQ subscales. This was true as well for the NEI-VFQ25 total score and most subscales. For example, the better eye, average eye, and binocular summation measures of VA showed the highest correlations with the NEI-VFQ25 total score (0.36 to 0.37) whereas the binocular VA test result correlated the lowest (0.27). These results are unexpected, given our premise that clinically assessed binocular tests of VA and VF should relate more closely to the patient’s report of their visual function than monocular tests or binocular approximations based on monocular tests.
For VF, the premise that binocular tests should relate more closely to PROs than binocular approximations received some, albeit limited, support. The Esterman binocular test of VF correlated more strongly than any of the binocular approximations with the VAQ total score and with 6 of the 8 VAQ subscales. While this was not the case for the NEI-VFQ25 total score and 8 of 11 subscales, the Esterman VF was more strongly correlated with the NEI-VFQ25 subscales most relevant to visual field (peripheral vision, distance activities, driving) than any of the monocular measures. The difference in results between the VAQ and NEI-VFQ25 might be explained by the fact that, in contrast to the VAQ, the NEI-VFQ25 has several subscales that lack a direct association with visual field loss (e.g. mental health, ocular pain).
Past studies have shown mixed results for the association of various binocular VF tests or binocular approximations with PRO and performance measures. Using baseline CIGTS data, Mills et al.3 found correlations between the VAQ total score and the better or worse eye VF (−0.19 and −0.11, respectively) that were almost identical to our findings for measures taken at 5 years follow-up (−0.17 and −0.10, respectively). Based on a study of 147 patients with glaucoma, Parrish et al.12 reported moderate to high correlations between the Esterman VF test and the 51-item NEI-VFQ, with distance activity and peripheral vision domain correlations of −0.56 and −0.60, respectively, whereas we found correlations for these two domains of −0.27 and −0.24, respectively, using the 25-item NEI-VFQ. This discrepancy may be due to differing number of subscale items between questionnaires, as most of the 51-item NEI-VFQ domains have more items than the 25-item NEI-VFQ. While this is true for the distance activities domain (7 items vs. 3 items, respectively), the peripheral vision domain is based on a single item in both questionnaires and yet yielded different correlations.
Because of lack of breadth (ceiling effect) in the Esterman VF test, Jampel et al.13 tested a modified version of this test, with a decreased stimulus intensity, and found that the NEI-VFQ25 total score and several of its domain scores were less correlated with the modified Esterman score than the best location approach7. More recently, Arora et al.14 contrasted relationships of better eye MD and an integrated VF measure (binocular summation7) with performance measures such as mobility and reading speed. They concluded that associations of performance with the better eye MD were comparable to the binocular summation method, as did McKean-Cowdin et al.15 in evaluating the LALES findings. Also, Owen et al.16 reported that an integrated VF measure making use of the both eyes’ central 20 degree VF sensitivity values17 provided a better prediction of which patients will lose their driving licenses than better or worse eye VF measures.
Our findings are based on tests from CIGTS participants, who were required to have 20/40 or better VA in both eyes at study entry, and the large majority retained this level of VA at the five year visit from which our findings are derived. Also, most CIGTS participants did not have advanced VF loss in either eye or substantial inter-eye difference in VA or VF, which needs to be considered in evaluating our findings. For example, Asaoka et al.18 found that particularly in patients with advanced VF loss, a binocular integrated VF that merged sensitivity values from monocular VF tests yielded higher (better) MD values than use of the better eye MD. Their study, however, did not evaluate associations of the binocular integrated VF with patient-reported or performance outcomes to confirm the purported advantage of this integrated approach.
We conclude based on our analysis of the CIGTS data that for VA, there is little added benefit in performing binocular testing in the clinical setting, because binocular VA is highly correlated with binocular approximations such as the better eye’s VA, and less correlated with VR-QOL than the better eye VA. However, for VF our results indicate some added benefit in performing binocular VF tests, as the Esterman test results correlated better with the VAQ and relevant subscales of the NEI-VFQ25 than binocular approximations based on monocular measures. The evident ceiling effect of the Esterman score within the range of MD values of CIGTS participants is a problem that may limit its benefit for use in studies that involve patients with mild to moderate glaucoma. Development of a better measure of binocular VF than the Esterman test may mitigate this limitation.
Supplementary Material
eFigure 1. Correlations between repeated measures over follow-up for a) Esterman binocular VF, b) Better eye mean deviation (MD), c) Worse eye MD, d) Binocular visual acuity (VA), e) Better eye VA, and f) Worse eye VA.
Acknowledgments
Financial Support: Supported by NIH/NEI grant EY025719; The sponsor or funding organization had no role in the design or conduct of this research.
Footnotes
Presented in part at the annual meeting of the Association for Research in Vision and Ophthalmology, Seattle, WA, May 2016
No conflicting relationship exists for any author
This article contains additional online-only material. The following should appear online-only: eFigure1a–1f and eTable 1, eTable 2, eTable 3
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sloane ME, Ball K, Owsley C, et al. The Visual Activities Questionnaire: developing an instrument for assessing problems in everyday visual tasks. Tech Dig Noninvasive Assess Vis Syst. 1992;1:26–9. [Google Scholar]
- 2.Mangione CM, Lee PP, Gutierez P, et al. Development of the 25-item National Eye Institute Visual Function Questionnaire (NEI-VFQ) Arch Ophthalmol. 2001;119:1050–8. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 3.Mills RP, Janz NK, Wren PA, et al. Correlation of visual field with quality-of-life measures at diagnosis in the Collaborative Initial Glaucoma Treatment Study (CIGTS) J Glaucoma. 2001;10:192–8. doi: 10.1097/00061198-200106000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Musch DC, Lichter PR, Guire KE, et al. The Collaborative Initial Glaucoma Treatment Study (CIGTS): study design, methods, and baseline characteristics of enrolled patients. Ophthalmology. 1999;106:653–62. doi: 10.1016/s0161-6420(99)90147-1. [DOI] [PubMed] [Google Scholar]
- 5.Ferris FL, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–6. [PubMed] [Google Scholar]
- 6.Early Treatment Diabetic Retinopathy Study Research Group. Early treatment diabetic retinopathy study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology. 1991;98:741–56. doi: 10.1016/s0161-6420(13)38009-9. [DOI] [PubMed] [Google Scholar]
- 7.Mills RP. Statistical aids to visual field interpretation. J Ocular Pharm. 1991;7:89–95. doi: 10.1089/jop.1991.7.89. [DOI] [PubMed] [Google Scholar]
- 8.Esterman B. Functional scoring of the binocular field. Ophthalmology. 1982;89:1226–34. doi: 10.1016/s0161-6420(82)34647-3. [DOI] [PubMed] [Google Scholar]
- 9.Nelson-Quigg JM, Cello K, Johnson CA. Predicting binocular visual field sensitivity from monocular visual field results. Invest Ophthalmol Vis Sci. 2000;41:2212–21. [PubMed] [Google Scholar]
- 10.Azen SP, Varma R, Preston-Martin S, et al. Binocular visual acuity summation and inhibition in an ocular epidemiological study: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2002;43:1742–8. [PubMed] [Google Scholar]
- 11.Jampel HD. Glaucoma patients’ assessment of their visual function and quality of life. Trans Am Ophthalmol Soc. 2001;99:301–17. [PMC free article] [PubMed] [Google Scholar]
- 12.Parrish RK, Gedde SJ, Scott IU, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–55. doi: 10.1001/archopht.1997.01100160617016. [DOI] [PubMed] [Google Scholar]
- 13.Jampel HD, Friedman DS, Quigley H, Miller R. Correlation of the binocular visual field with patient assessment of vision. Invest Ophthalmol Vis Sci. 2002;43:1059–67. [PubMed] [Google Scholar]
- 14.Arora KS, Boland MV, Friedman DS, et al. The relationship between better-eye and integrated visual field mean deviation and visual disability. Ophthalmology. 2013;120:2476–84. doi: 10.1016/j.ophtha.2013.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McKean-Cowdin R, Wang Y, Wu J, et al. Impact of visual field loss on health-related quality of life in glaucoma. The Los Angeles Latino Eye Study. Ophthalmology. 2008;115:941–8. doi: 10.1016/j.ophtha.2007.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Owen VMF, Crabb DP, White ET, et al. Glaucoma and fitness to drive: using binocular visual fields to predict a milestone to blindness. Invest Ophthalmol Vis Sci. 2008;49:2449–55. doi: 10.1167/iovs.07-0877. [DOI] [PubMed] [Google Scholar]
- 17.Crabb DP, Viswanathan AC, McNaught AI, et al. Simulating binocular visual field status in glaucoma. Br J Ophthalmol. 1998;82:1236–41. doi: 10.1136/bjo.82.11.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asaoka R, Crabb DP, Yamashita T, et al. Patients have two eyes!: binocular versus better eye visual field indices. Invest Ophthalmol Vis Sci. 2011;52:7007–11. doi: 10.1167/iovs.11-7643. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Correlations between repeated measures over follow-up for a) Esterman binocular VF, b) Better eye mean deviation (MD), c) Worse eye MD, d) Binocular visual acuity (VA), e) Better eye VA, and f) Worse eye VA.