Abstract
PURPOSE
The objective of this study was to determine the cumulative survival rate (CSR) and associated risk factors of Implantium implants by retrospective clinical study.
MATERIALS AND METHODS
Patients who received Implantium implants (Dentium Co., Seoul, Korea) at Korea University Guro Hospital from 2004 to 2011 were included. The period between the first surgery and the last hospital visit until December 2015 was set as the observation period for this study. Clinical and radiographic data were collected from patient records, including all complications observed during the follow-up period. Kaplan-Meier analysis was performed to examine CSR. Multiple Cox proportional hazard model was employed to assess the associations between potential risk factors and CSR.
RESULTS
A total of 370 implants were placed in 121 patients (mean age, 56.1 years; range, 19 to 75 years). Of the 370 implants, 13 failed, including 7 implants that were lost before loading. The 10-year cumulative survival rate of implants was 94.8%. The multiple Cox proportional hazard model revealed that significant risk factor of implant failure were smoking and maxillary implant (P<.05).
CONCLUSION
The 10-year CSR of Implantium implants was 94.8%. Risk factors of implant failure were smoking and maxillary implant.
Keywords: Dental implant, Survival rate, Risk factors, Smoking, Arch
INTRODUCTION
To obtain favorable long-term clinical treatment outcomes of implant approach, fast and firm osseointegration with stable alveolar bone must be achieved, even after functional loading. Current implant surface treatment trends aim to develop an implant surface that is more bioactive and proangiogenic in order to achieve better osseointegration.1 As a result of these efforts, a variety of new commercial implant systems have been introduced to the market. Although a large number of clinical studies have reported successful treatment outcomes of dental implants, most long-term (over 10 years) studies have used several common brands of implant systems.2,3,4,5,6 Additionally conflicting data have been reported about the risk factors of implant failure. Therefore, clinicians are unable to provide concrete answers for patients who underwent failed implant treatments.
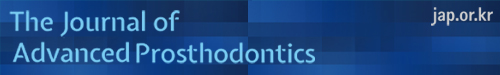
Implantium implants (Dentium Co., Seoul, Korea) is an internal connection type of conical hex with a surface sand-blasted with large grit and acid etched (SLA) (Fig. 1). Since FDA approval of this product in 2004, it has been one of the most widely used implants in South Korea. However, there are only two clinical studies on the product with follow-up longer than five years. Lee et al. have reported that the 5-year cumulative survival rate (CSR) of this implant is 97.37%.7 Park et al. have reported that the 10-year CSR of this implant is 97.9% without assessing risk factors associated with implant failure.8
Fig. 1. Implantium implant (Dentium, Seoul, Korea). (A) Design of implant, (B) microstructure of implant surface (SEM MAG: 3.00 kx).
Therefore, the objective of this retrospective study was to determine the 10-year CSR of Implantium implant and to assess the association between implant failure and related risk factors.
MATERIALS AND METHODS
This retrospective study was conducted based on review of the clinical records of all patients who received Implantium implants at the implant clinic of Korea University Guro Hospital Dental Center from June, 2004 to May, 2011. Implants that underwent splinting with other implant systems were excluded. Records which provided insufficient data presented in clinical charts were excluded as well. As a result, 370 implants in a total of 121 patients were evaluated in this study. The period between the first surgery and the last hospital visit up to December, 2015 was set as the observation period for this study.
All patients were subjected to full thickness flap elevation under local anesthesia. The same surgical procedures were performed for all patients according to the manufacturer's recommendations. In 93 of 370 implants, ancillary surgical procedures (such as guided bone regeneration and sinus augmentation) were performed. The final prosthesis was fabricated with the conventional methods depending on the case and was loaded at least two months after the implant placement. For maintenance, regular follow-up visits (at least once a year) were scheduled after delivery of definitive prosthesis.
Implant survival was assessed with Albrektsson and Zarb's criteria.9 In particular, an implant whose function was stably maintained until final observation was considered as survived, whereas removal and sleeping of the implant were defined as failed. The following nominal and ordinal variables were used to assess implant failure and their associations with implant failure: gender, age (≥ 65 years and < 65 years), systemic chronic disease (diabetes mellitus and/or cardiovascular disease), smoking status (current or none), history of periodontitis, implant location (maxilla, mandible, anterior, posterior), Kennedy classification, implant length and diameter, additional surgery, the kind of abutment, prosthesis type, occlusal materials, and opposing dentition (Table 1).
Table 1. Distribution of implants according to risk factor variables.
| Variables | Characteristics | No of Implant (failed implant) | Variable | Characteristics | No of Implant (failed implant) |
|---|---|---|---|---|---|
| Gender | Male | 222 (10) | Additional surgery | Yes | 93 (5) |
| Female | 148 (3) | No | 277 (8) | ||
| Age | < 65 | 300 (11) | Abutment | Ready-made | 279 (4) |
| ≥ 65 | 70 (2) | Customized | 51 (2) | ||
| Systemic condition | Systemic disease* | 93 (4) | UCLA | 17 (0) | |
| Healthy | 277 (9) | Attachment | 16 (0) | ||
| Smoking | Current | 56 (7) | Prosthesis | Single crown | 60 (2) |
| None | 314 (6) | Bridge | 252 (2) | ||
| History of periodontitis | Yes | 286 (4) | Hybrid | 33 (2) | |
| No | 84 (9) | RPD | 4 (0) | ||
| Jaw | Maxilla | 166 (10) | Overdenture | 14 (0) | |
| Mandible | 204 (3) | Occlusal material | Metal/gold | 270 (5) | |
| Position | Anterior | 71 (3) | Porcelain | 63 (1) | |
| Posterior | 299 (10) | Resin | 30 (0) | ||
| Kennedy classification | Distal extension | 219 (4) | Opposing teeth | Natural tooth | 312 (6) |
| Natural tooth | 312 (6) | FPD | 29 (0) | ||
| Tooth bounded | 103 (5) | RPD | 9 (0) | ||
| Edentulous | 48 (4) | CD | 8 (0) | ||
| Length of implant | Short (≤ 8 mm) | 26 (2) | Overdenture | 5 (0) | |
| Long (> 8 mm) | 344 (11) | ||||
| Width of implant | Regular | 306 (12) | |||
| Wide (≥ 5 mm) | 64 (1) |
Systemic disease included diabetes mellitus and/or cardiovascular disease.
For statistical analysis, SPSS software version 22.0 was used. The CSR of implants was determined using Kaplan Meier analysis. Difference in CSR according to risk factor was assessed by log rank test (Mantel-Cox) (P = .05). Risk factor variables were included in multiple Cox proportional regression analysis, if preliminary Cox analysis demonstrated at least a statistically borderline significance (P < .15).
RESULTS
A total of 370 implants were placed in 121 patients (66 males and 55 females) during the observation period. The average observation period was 7.2 years (S.D. = 2.4 years). The average age of these patients was 56.1 ± 10.5 years (range, 19 to 75 years). The distributions of implants according to factor are summarized in Table 1.
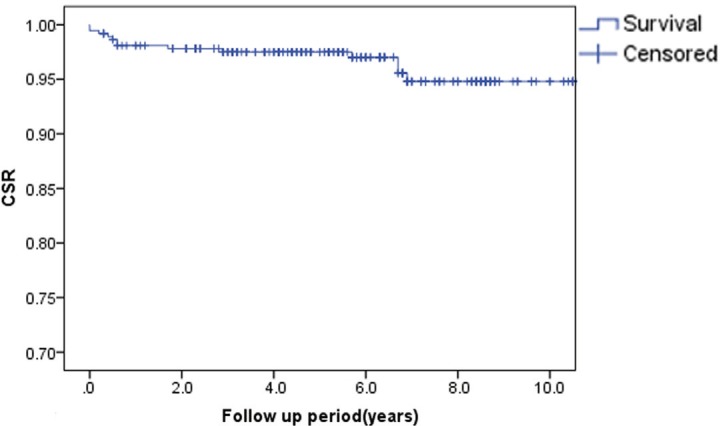
Of the 370 implants placed during the observation period, 13 failed. The 10-year CSR of these implants was 94.8% (Fig. 2).
Fig. 2. Cumulative survival rate (CSR) of Implantium implants by Kaplan-Meier method.
According to the preliminary analysis, smoking (current vs none) and arch (maxilla vs mandible) were included in multiple Cox proportional regression analysis (P < .15). As a result, smoking and maxillary implant were significant risk factors of implant failure with a hazard ratio of 7.48 and 3.92, respectively (Table 2, P < .05).
Table 2. Multivariate associations with cumulative survival rate of implants.
| B (regression coefficient) | P value | Exp (B) (hazard ratio) | Exp (B) 95.0% CI | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Smoking (current vs none) | 2.012 | .000 | 7.478 | 2.492 | 22.436 |
| Jaw (maxilla vs mandible) | 1.365 | .038 | 3.916 | 1.077 | 14.235 |
Significant difference (P < .05).
DISCUSSION
This study showed a 10-year CSR of Implantium implant of 94.8%. Although this result is relatively low compared to that of the Straumann dental implant system (Straumann, Basel, Switzerland) with an SLA surface,4,5 it was a clinically acceptable result. Seven of the 13 failed implants failed before loading, and the other six implants failed after loading. Of the 13 failed implants, re-implantation was performed for eight cases with consent from the patients. For the remaining five cases, restoration was completed by modifying the prosthetic treatment plan followed by maintenance without implant replacement.
A previous 5-year study with similar researchers found various significant factors in implant failure. According to the log-rank test, the significant factors influencing implant failure were occlusal material, prosthesis design, Kennedy classification, arch, reason of tooth loss, smoking and systemic diseases.7 However, in this 10-year follow-up study via multiple regression analysis, the results obtained were narrowed down and presented high specificity. Hence, the results of this 10-year study showed smoking and implant placement in the maxilla as significant factors in implant failure.
Although some clinical reports have suggested that the advent of rough implant surface has resolved the differences between smokers and non-smokers,10,11 recent meta-analysis studies have shown that smoking is still associated with a higher risk of dental implant failure.12,13 Smoking may inhibit both innate and adaptive responses in a variety of ways. The increase in implant failure caused by smoking is mainly attributed to the effects of nicotine on osteogenesis and angiogenesis.13 Nicotine inhibits gene expression including BMP-2, PDGF-AA, TGF-β, and VEGF, which play important roles in osteoblast proliferation, differentiation, and apoptosis.14 Moreover, it induces hyperemia through vasoconstriction and chronic reduction of blood flow and vascularity,15,16 leading to low oxygen and ischemia as well as inadequate blood flow, which ultimately inhibit the normal and/or the healing processes of skeletal structures.17 In this study, current smoking was also found to have significant association with implant failure. Therefore, pre-operative smoking status needs to be addressed for implant treatment. A few investigators have suggested smoking cessation.15,16,18 However, only one clinical study has reported the effectiveness of smoking cessation on implant treatment outcomes.18 More research is needed to draw definitive conclusions regarding the matter.
Previous studies showed contradicting results regarding the association of implant survival rate with arch location of implant.7,19,20,21 According to a meta-analysis of 54 clinical studies with at least 3-years observation period, the annual implant failure rate of maxillary implants is significantly higher than that of mandibular implants.22 This might be due to the fact that the quality and quantity of jaw bone are more often compromised in the maxillary region than in the mandibular region.23,24 In this present study, the survival rate of maxillary implants was found to be significantly lower than that of mandibular implants, and it also was revealed in multivariate regression analysis.
This retrospective study has a limitation in the evaluation of marginal bone loss with consistency and in its reproducibility due to non-standardized radiographic measurements. For this reason, only the survival rate of implants was analyzed without assessing the success rate of implants.
CONCLUSION
Within the limitations of this study, the 10-year CSR of Implantium implants was 94.8%, and smoking and maxillary implant were identified as a significant risk factors of implant failure.
Footnotes
This study was supported by the Korea Health Industry Development Institute (2015-2017 Project No. HI15C0620).
References
- 1.Saghiri MA, Asatourian A, Garcia-Godoy F, Sheibani N. The role of angiogenesis in implant dentistry part I: Review of titanium alloys, surface characteristics and treatments. Med Oral Patol Oral Cir Bucal. 2016;21:e514–e525. doi: 10.4317/medoral.21199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 3.Ekelund JA, Lindquist LW, Carlsson GE, Jemt T. Implant treatment in the edentulous mandible: a prospective study on Brånemark system implants over more than 20 years. Int J Prosthodont. 2003;16:602–608. [PubMed] [Google Scholar]
- 4.Buser D, Janner SF, Wittneben JG, Brägger U, Ramseier CA, Salvi GE. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012;14:839–851. doi: 10.1111/j.1708-8208.2012.00456.x. [DOI] [PubMed] [Google Scholar]
- 5.van Velzen FJ, Ofec R, Schulten EA, Ten Bruggenkate CM. 10-year survival rate and the incidence of peri-implant disease of 374 titanium dental implants with a SLA surface: a prospective cohort study in 177 fully and partially edentulous patients. Clin Oral Implants Res. 2015;26:1121–1128. doi: 10.1111/clr.12499. [DOI] [PubMed] [Google Scholar]
- 6.Rasmusson L, Roos J, Bystedt H. A 10-year follow-up study of titanium dioxide-blasted implants. Clin Implant Dent Relat Res. 2005;7:36–42. doi: 10.1111/j.1708-8208.2005.tb00045.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee JY, Park HJ, Kim JE, Choi YG, Kim YS, Huh JB, Shin SW. A 5-year retrospective clinical study of the Dentium implants. J Adv Prosthodont. 2011;3:229–235. doi: 10.4047/jap.2011.3.4.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park W, Park Y, Park H, Yoo S, Chung S, Han J, Kim SW, Kim DM. A 10-year retrospective radiographic study of implantium dental implants. Int J Periodontics Restorative Dent. 2015;35:49–54. doi: 10.11607/prd.2289. [DOI] [PubMed] [Google Scholar]
- 9.Albrektsson T, Zarb GA. Current interpretations of the osseointegrated response: clinical significance. Int J Prosthodont. 1993;6:95–105. [PubMed] [Google Scholar]
- 10.Balshe AA, Eckert SE, Koka S, Assad DA, Weaver AL. The effects of smoking on the survival of smooth- and rough-surface dental implants. Int J Oral Maxillofac Implants. 2008;23:1117–1122. [PubMed] [Google Scholar]
- 11.Maló P, de Araújo Nobre M, Gonçalves Y, Lopes A. Long-term outcome of implant rehabilitations in patients with systemic disorders and smoking habits: a retrospective clinical study. Clin Implant Dent Relat Res. 2016;18:649–665. doi: 10.1111/cid.12346. [DOI] [PubMed] [Google Scholar]
- 12.Renvert S, Quirynen M. Risk indicators for peri-implantitis. A narrative review. Clin Oral Implants Res. 2015;26:15–44. doi: 10.1111/clr.12636. [DOI] [PubMed] [Google Scholar]
- 13.Chrcanovic BR, Albrektsson T, Wennerberg A. Smoking and dental implants: A systematic review and meta-analysis. J Dent. 2015;43:487–498. doi: 10.1016/j.jdent.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Ma L, Zwahlen RA, Zheng LW, Sham MH. Influence of nicotine on the biological activity of rabbit osteoblasts. Clin Oral Implants Res. 2011;22:338–342. doi: 10.1111/j.1600-0501.2010.02088.x. [DOI] [PubMed] [Google Scholar]
- 15.Morozumi T, Kubota T, Sato T, Okuda K, Yoshie H. Smoking cessation increases gingival blood flow and gingival crevicular fluid. J Clin Periodontol. 2004;31:267–272. doi: 10.1111/j.1600-051X.2004.00476.x. [DOI] [PubMed] [Google Scholar]
- 16.Nair P, Sutherland G, Palmer RM, Wilson RF, Scott DA. Gingival bleeding on probing increases after quitting smoking. J Clin Periodontol. 2003;30:435–437. doi: 10.1034/j.1600-051x.2003.20039.x. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Wan C, Deng L, Liu X, Cao X, Gilbert SR, Bouxsein ML, Faugere MC, Guldberg RE, Gerstenfeld LC, Haase VH, Johnson RS, Schipani E, Clemens TL. The hypoxia-inducible factor alpha pathway couples angiogenesis to osteogenesis during skeletal development. J Clin Invest. 2007;117:1616–1626. doi: 10.1172/JCI31581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bain CA. Smoking and implant failure-benefits of a smoking cessation protocol. Int J Oral Maxillofac Implants. 1996;11:756–759. [PubMed] [Google Scholar]
- 19.Shigehara S, Ohba S, Nakashima K, Takanashi Y, Asahina I. Immediate loading of dental implants inserted in edentulous maxillas and mandibles: 5-year results of a clinical study. J Oral Implantol. 2015;41:701–705. doi: 10.1563/aaid-joi-D-14-00018. [DOI] [PubMed] [Google Scholar]
- 20.Moy PK, Medina D, Shetty V, Aghaloo TL. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005;20:569–577. [PubMed] [Google Scholar]
- 21.Del Fabbro M, Ceresoli V. The fate of marginal bone around axial vs. tilted implants: a systematic review. Eur J Oral Implantol. 2014;7:S171–S189. [PubMed] [Google Scholar]
- 22.Kern JS, Kern T, Wolfart S, Heussen N. A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res. 2016;27:174–195. doi: 10.1111/clr.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Truhlar RS, Orenstein IH, Morris HF, Ochi S. Distribution of bone quality in patients receiving endosseous dental implants. J Oral Maxillofac Surg. 1997;55:38–45. doi: 10.1016/s0278-2391(16)31196-x. [DOI] [PubMed] [Google Scholar]
- 24.He J, Zhao B, Deng C, Shang D, Zhang C. Assessment of implant cumulative survival rates in sites with different bone density and related prognostic factors: an 8-year retrospective study of 2,684 implants. Int J Oral Maxillofac Implants. 2015;30:360–371. doi: 10.11607/jomi.3580. [DOI] [PubMed] [Google Scholar]