Abstract
Background
The obesogenic and diabetogenic effects of the environmental toxin BPA during critical windows of development are well-recognized. Liver and skeletal muscle play a central role in the control of glucose production, utilization and storage.
Objectives
We hypothesized that maternal BPA exposure disrupts insulin signaling in rat offspring liver and skeletal muscle. We determined the protein expression of hepatic and skeletal muscle insulin signaling molecules including insulin receptor beta (IR-β), its downstream target insulin receptor substrate 1 (IRS-1) and glucose transporters (GLUT2; GLUT4) and hepatic glucose regulating enzymes phosphoenolpyruvate carboxykinase (PEPCK) and glucokinase (GCK).
Study Design
Rat dams had ad libitum access to filtered drinking water (Control) or drinking water with BPA from 2 weeks prior to mating and through pregnancy and lactation. Offspring litters were standardized to 4 males and 4 females and nursed by the same dam. At weaning, BPA exposure was removed from all offspring. Glucose tolerance was tested at 6 weeks and 6 months. Liver and skeletal muscle was collected from 3 week-old and 10 month-old offspring for protein expression (Western Blot) of IR-β, IRS-1, GLUT2, GLUT4, PEPCK and GCK.
Results
Male, but not female BPA offspring had impaired glucose tolerance at 6 weeks and 6 months. Both male and female adult offspring had higher glucose-stimulated insulin secretion as well as ratio of stimulated insulin to glucose. Male BPA offspring had higher liver protein abundance of the 200 kD IR-β precursor (2-fold), and IRS-1 (1.5-fold), while GLUT2 was 0.5-fold of the control at 3 weeks of age. In adult male BPA offspring the abundance of IR-β was higher (2-fold) and GLUT4 was 0.8-fold of the control in skeletal muscle. In adult female BPA offspring the skeletal muscle protein abundance of GLUT4 was 0.4–fold of the control.
Conclusions
Maternal BPA had sex- and tissue-specific effects on insulin signaling components, which may contribute to increased risk of glucose intolerance in offspring. Glucose transporters were consistently altered at both ages as well as in both sexes and may contribute to glucose intolerance. These data suggest that maternal BPA exposure should be limited during pregnancy and lactation.
Keywords: BPA, fetal programming, GLUT4, Insulin Signaling, Rat
INTRODUCTION
The world-wide incidence of metabolic diseases, including type II diabetes, has increased dramatically over the past 30 years.1;2 While there is little doubt that diet, exercise and genetic factors all play a role in an individual’s susceptibility to type II diabetes, evidence from human and animal models suggests that predisposition to the development of metabolic disease also begins in utero.3 This concept of “developmental programming” states that early environmental exposures during pregnancy and/or lactation programs changes in gene expression that alters growth and development with consequences for the long-term health of the offspring.3
Recent public health concerns have been raised regarding the potential long-term effects of exposure to the endocrine disrupter chemical bisphenol A (4,4-dihydroxyl-2,2-diphenylpropane; BPA) during the vulnerable period of perinatal development.4 BPA is an industrial chemical used primarily to make polycarbonate plastic and epoxy resins. It is used in the production of everyday items including carbon-free paper, sports equipment, medical devices, reusable food and drink containers and dental sealants. The abundant use of BPA has made this endocrine disrupter chemical ubiquitous in our environment, leading to chronic low dose exposure.5 According to the 2003–2004 National Health and Nutrition Examination Survey (NHANES) BPA was detected in the urine of >90% of the survey participants.6 Moreover, children had the highest urinary BPA concentrations, followed by adolescents and adults.6 In addition, BPA has been detected in maternal serum, amniotic fluid, fetal cord blood and breast milk.7
During periods of increased glucose availability, tight homeostatic regulation of blood glucose levels is primarily achieved by the actions of insulin to inhibit hepatic glucose production and to increase the uptake and storage of glucose in peripheral insulin-sensitive tissues, such as skeletal muscle.8 Hence, any disruption to glucose-stimulated insulin secretion or to the ability of peripheral tissues to respond to insulin action via intracellular insulin signaling pathways will likely have adverse consequences for glucoregulation.8 Using NHANES data (2003–2004; 2005–2006; 2007–2008), the majority of published human epidemiological studies have shown positive associations between urinary concentrations of BPA, glucose intolerance and diabetes.9–12 Similarly, studies in animals have shown impaired glucose tolerance and altered secretion of insulin from the endocrine pancreas in adult mice13–16 and rats17;18 that were exposed to BPA perinatally. Studies in adult mice and rats have implicated changes in pancreatic β-cell mass, as well as lower expression of genes that normally optimize β-cell function, such as Pdx-1, in the mechanism by which BPA alters glucoregulation.14;17;20;21 However, homeostatic regulation of blood glucose is determined by both pancreatic β-cell insulin secretion and its effects on peripheral, insulin-sensitive tissues. The biological effects of insulin, including uptake of glucose into fat and muscle cells and suppression of glucose synthesis in the liver are mediated by activation of the insulin receptor and the biochemical insulin transduction pathway. Previous studies have focused on BPA-induced alterations in insulin secretion and beta cell mass or function 14;17;20;21, but whether perinatal exposure to BPA has age-, sex- or tissue-specific effects on the protein abundance of insulin signaling components is unknown. Hence, the current study determined whether perinatal exposure to BPA alters the protein abundance of insulin signaling components in offspring liver and muscle at weaning and in adulthood.
MATERIALS AND METHODS
All procedures were approved by the Animal Care Committee at the Los Angeles Biomedical Research Institute at Harbor-University of California, Los Angeles, and were conducted in accordance with guidelines provided by the American Accreditation Association of Laboratory Care and the Public Health Service Policy on Humane Care and Use of Laboratory Animals.
Animals
Eleven virgin female Sprague Dawley rats (9 weeks old; Charles River Laboratories, Hollister, CA) were housed in a facility with constant temperature (21±1 °C) and a controlled 12:12-hour light/dark cycle. A rat model of maternal exposure to BPA was created using ad libitum access to BPA (Sigma-Aldrich Corp., St. Louis, MO, USA) in drinking water 2 weeks prior to and through pregnancy and lactation. The amount of BPA consumed was 239±8 μg/day/body weight over the course of pregnancy and 466±33 μg/day/body weight during lactation (due to increased water intake during lactation). At birth, blood from all excess newborn pups was pooled to create sufficient volume to determine the plasma BPA level. Newborns from BPA-treated dams had a plasma BPA level (0.62 ng/ml) within the range of values measured in human umbilical cord blood, whereas BPA was undetectable in plasma from the newborns of Control dams.19;20 There were no differences in body weights between control (male: 6.85 ± 0.10 g; female: 6.62 ± 0.11 g) and BPA-treated (male: 6.84 ± 0.18 g; female: 6.65 ± 0.08 g; two way ANOVA with sex and treatment as factors) offspring within each sex at birth, or at any time point thereafter.
At 11 weeks of age, rats were mated and continued on their respective treatments during pregnancy and lactation. After birth, at 1 day of age, litters were culled to 8 pups (4 males and 4 females) per dam to standardize nursing. All pups were nursed by their respective dams until 3 weeks of age. At weaning BPA exposure was removed and the rat pups were housed 4 per cage with the same sex. The animals were separated to two per cage at 125 g and into singular housing when their weight was above 250 g, such that no cage contained more than 500 g of total rat body weight. All rats were housed in BPA-free polycarbonate cages (Ancar Corp; Bellmore, NY). The cages were filled with paperchip bedding (Sherpherd Specialty Papers; Watertown, TN) with cardboard tubes for enrichment. All weaned offspring had ad libitum access to a standard control diet (LabDiet 5001; LabDiet, St. Louis, MO) and filtered drinking water with no further BPA exposure.
Glucose tolerance and plasma analyses
At 6 and 24 weeks of age, 1 male and 1 female offspring from each litter underwent a glucose tolerance test (GTT). Following an overnight fast, D-glucose (1 mg/g body weight) was injected intraperitoneally (i.p) in conscious rats. Blood glucose values were determined in tail bleed blood prior to (time 0) and 15, 30, 60, 120, and 180 minutes after glucose administration using a Hemocue B-glucose analyzer (HemoCue Inc, Mission Viejo, CA). Plasma insulin concentrations were determined prior to the glucose challenge (time 0; 6 and 24 weeks of age) and during the challenge at 15 and 180 minutes (24 weeks). Blood was collected into heparinized tubes at 0, 15 and 180 minutes, centrifuged immediately at 3,000 g and 4°C for 10 min and the plasma was stored at −80 °C. Plasma insulin concentrations were measured using a commercially available, rodent-specific ELISA kit (10-1250-01; Mercodia, Uppsala, Sweden).
Tissue collection
At 3 weeks and 10 months of age, offspring were anesthetized by 5% isoflurane/2% oxygen by mask and exsanguinated via cardiac puncture. Euthanasia was confirmed by decapitation. Plasma, as well as liver and gastrocnemius skeletal muscle tissue were collected, snap-frozen in liquid nitrogen and stored at −80 °C until analysis. The offspring in the current study were part of a larger study of the long-term effects of perinatal BPA exposure on offspring growth and appetite regulation (these data will be published separately). Consequently, offspring tissues were not available at the exact ages corresponding to the in vivo measurements of glucose clearance. Tissues collected at ages closest to the in vivo experiments were used to determine the protein abundances of components of the insulin signaling pathway.
Protein extraction and Western blotting
Liver and skeletal muscle protein was extracted in radioimmunoprecipitation assay buffer (1x) containing protease inhibitors (HALT cocktail; Pierce, Rockford, IL) and the total protein concentration in the supernatant was determined using a bicinchoninic acid assay (BCA kit; Pierce, Rockford, IL). Western Blotting was performed as previously described,21 using primary antibodies from Santa Cruz Biotechnology (Texas, USA; 1:1000) against insulin receptor beta subunit (IR-β; sc-711), insulin receptor substrate 1 (IRS-1; sc-559), glucose transporter 2 (GLUT2; sc-9117), glucose transporter 4 (GLUT4; sc-1607), phosphoenolpyruvate carboxykinase (PEPCK; sc-32879) and glucokinase (GCK; sc-7908). Goat anti-rabbit IgG HRP conjugate (#1706515; Bio-Rad, California, USA; 1:2000) and donkey anti-goat IgG HRP conjugate (sc-2020; Santa Cruz Biotechnology, Texas, USA; 1:2000) were used as secondary antibodies. The depicted bands had the expected molecular weights.
Statistical analysis
For all studies 5–6 offspring were studied per group (one of the 4 male offspring and one of the 4 female offspring from each of 6 control and 5 BPA-treated litters), with the exception of newborn plasma for BPA measurement where blood was pooled from all excess pups. No differences were found in the protein abundance of insulin signaling components in skeletal muscle from the 6 week-old glucose intolerant male offspring, hence skeletal muscle was not analyzed from 6 week-old female offspring that did not show a glucose intolerant phenotype at 3 weeks of age. Values are means ± standard error of the mean (SEM). Statistical significance (SigmaStat Statistical Software version 2.0) was assessed using unpaired Student’s t- test and two-way repeated measures ANOVA, as appropriate. Statistical significance was accepted when P < 0.05.
RESULTS
Fasting glucose and insulin
At 3 and 6 weeks of age, male and female fasting blood glucose and plasma insulin concentrations, and the ratio of insulin to glucose, were not different between control and BPA offspring. In contrast, at 24 weeks of age, male BPA offspring had higher plasma insulin concentrations, though the blood glucose concentrations and the ratio of insulin to glucose were comparable to controls. In addition, 24 week-old female BPA offspring had similar blood glucose concentrations and insulin levels, though the ratio of insulin to glucose was increased compared to controls (Table 1).
Table 1.
Blood Glucose and Plasma Insulin Concentrations
Concentrations of blood glucose and plasma insulin during the glucose tolerance test (GTT) (1 mg/g body weight i.p. D-glucose at time = 0 min), and the ratio of insulin to glucose in male and female offspring of control and BPA-treated rat dams from birth to 24 weeks of age. Values are mean ± s.e.m.
| Age | Variable | Time of data collection | Male | Female | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Control | BPA | Control | BPA | |||
| 3 Weeks | ||||||
| Basal blood glucose (mg/dl) | At tissue collection | 124 ± 5 | 121 ± 12 | 122 ± 5 | 101 ± 10 | |
| Basal plasma insulin (ng/ml) | At tissue collection | 0.19 ± 0.01 | 0.31 ± 0.13 | 0.18 ± 0.01 | 0.18 ± 0.01 | |
| Insulin:glucose ratio | At tissue collection | 1.5 ± 0.2 | 2.3 ± 0.7 | 1.5 ± 0.2 | 1.9 ± 0.2 | |
|
| ||||||
| 6 Weeks | ||||||
| Basal plasma glucose (mg/dl) | GTT 0 min | 80 ± 7 | 77 ± 7 | 88 ± 4 | 86 ± 6 | |
| Basal plasma insulin (ng/ml) | GTT 0 min | 0.18 ± 0.01 | 0.20 ± 0.01 | 0.20 ± 0.01 | 0.21 ± 0.01 | |
| Insulin:glucose ratio | GTT 0 min | 2.7 ± 0.5 | 2.5 ± 0.3 | 2.3 ± 0.2 | 2.4 ± 0.2 | |
|
| ||||||
| 24 Weeks | ||||||
| Basal plasma glucose (mg/dl) | GTT 0 min | 87 ± 2 | 102 ± 2 | 102 ± 4 | 92 ± 4 | |
| Basal plasma insulin (ng/ml) | GTT 0 min | 0.60 ± 0.08 | 1.02 ± 0.49* | 0.40 ± 0.03 | 0.58 ± 0.11 | |
| Insulin:glucose ratio | GTT 0 min | 6.8 ± 0.8 | 9.98 ± 4.67 | 4.0 ± 0.4 | 6.28 ± 1.05* | |
| Plasma glucose (mg/dl) | GTT 15 min | 147 ± 6 | 154 ± 8 | 139 ± 7 | 125 ± 11 | |
| Plasma insulin (ng/ml) | GTT 15 min | 1.46 ± 0.25 | 2.98 ± 0.42* | 0.51 ± 0.05 | 1.47 ± 0.46* | |
| Insulin:glucose ratio | GTT 15 min | 9.7 ± 1.3 | 19.5 ± 2.7* | 3.7 ± 0.5 | 11.7 ± 3.3* | |
P<0.05 versus control within the same sex. Data were analysed by two-way ANOVA with sex and treatment as factors.
Glucose tolerance test (GTT)
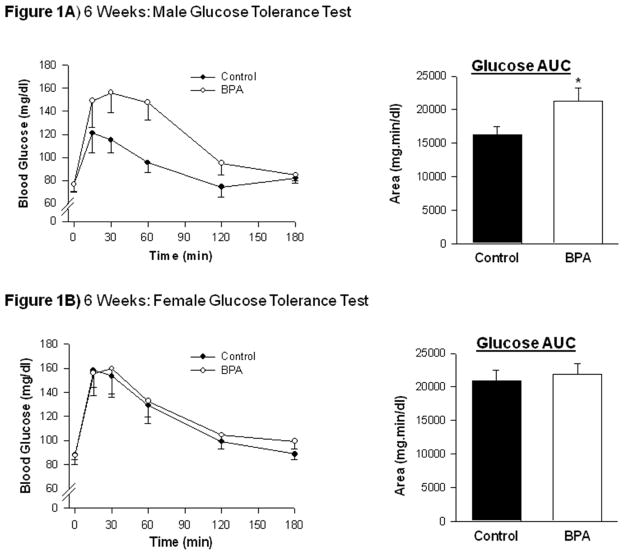
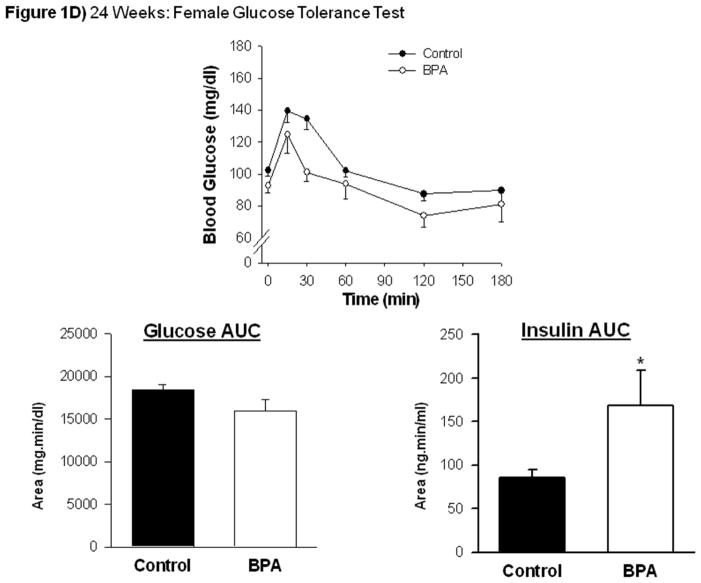
At both ages (6 and 24 weeks), administration of glucose generated an immediate increase in the blood concentration of glucose (P<0.05) that was maximal between 15 and 30 minutes post-injection in both BPA and control offspring (Figure 1). In 6 week-old BPA males, the area under the glucose curve was higher than in controls and remained higher in adulthood at 24 weeks of age (Figure 1A and 1C). However, perinatal exposure to BPA did not affect the time course of glucose clearance or the area under the glucose curve in female offspring at 6 or 24 weeks of age (Figure 1B and 1D).
Figure 1.
Values are mean ± SEM in the blood concentration of glucose and the area under the glucose clearance curve (AUC) following glucose administration (1 mg/g body weight i.p. D-glucose at time = 0 min) in (A) male and (B) female control (solid symbols; n = 6) and BPA-treated (open symbols; n = 6) rat offspring at 6 weeks of postnatal age, and in (C) male and (D) female control (solid symbols; n = 5) and BPA-treated (open symbols; n = 5) rat offspring at 24 weeks of postnatal age. *P< 0.05 versus control within the same sex; two-way repeated measures ANOVA plus Tukey test, with time and treatment as factors (glucose clearance curve) and Student’s t test (area under the curve).
At 24 weeks of age, the increase in blood glucose was accompanied by rapid insulin release in all offspring. Although there were similar rates of glucose clearance in BPA and control male and female offspring, the area under the glucose-stimulated insulin curve was higher in both BPA males and females compared with controls (Figures 1C and 1D). Additionally, the ratio of stimulated insulin to glucose was higher in both male and female BPA offspring (Table 1).
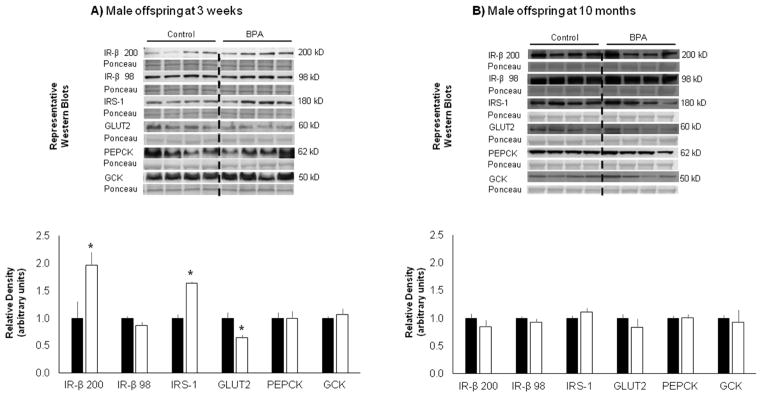
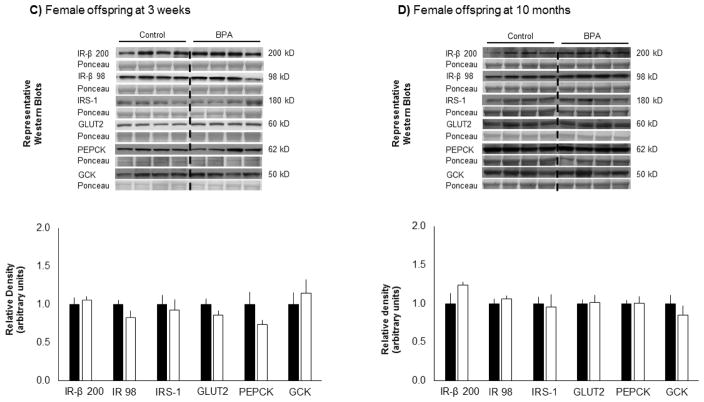
Liver Insulin signaling components
At 3 weeks of age, the protein abundance of GLUT2 was lower and the abundances of the 200 kD IR-β precursor and IRS-1 were higher in male BPA offspring compared with controls (Figure 2A). However, perinatal BPA did not affect any of the liver insulin signaling components in female BPA offspring (Figure 2C and 2D). Furthermore, the protein abundance of GCK or PEPCK liver enzymes was not different in either sex (Figure 2A – 2D).
Figure 2.
Representative Western Blots and quantitative analysis of the protein abundance of the insulin receptor beta (IR-β; 200 kD precursor molecule; 98 kD mature IR-β subunit), the insulin receptor substrate 1 (IRS-1), the glucose transporter 2 (GLUT2) and the enzymes phosphoenolpyruvate carboxykinase (PEPCK) and glucokinase (GCK) in liver tissue from male control (solid bars; n = 5) and BPA-treated (open bars; n = 5) rat offspring at (A) 3 weeks and (B) 10 months of postnatal age and (C) female control (solid bars; n = 5) and BPA-treated (open bars; n = 5) rat offspring at 3 weeks and (D) 10 months of postnatal age. Ponceau S staining served as a loading control. Values are mean ± SEM. *P< 0.05 versus control within the same immunoblot; Student’s t test.
At 10 months of age, there were no differences in the protein abundance of any of the measured liver insulin signaling components or enzymes in BPA male or female offspring (Figures 2B and 2D).
Skeletal Muscle Insulin signaling components
At 3 weeks of age, the protein abundance of GLUT4 and IR-β was not different between male BPA and control offspring (Figure 3A). In contrast, at 10 months of age, the protein abundance of GLUT4 was lower in both BPA male and female offspring. In addition, BPA males had higher abundance of IR-β compared with controls (Figures 3B and 3C).
Figure 3.
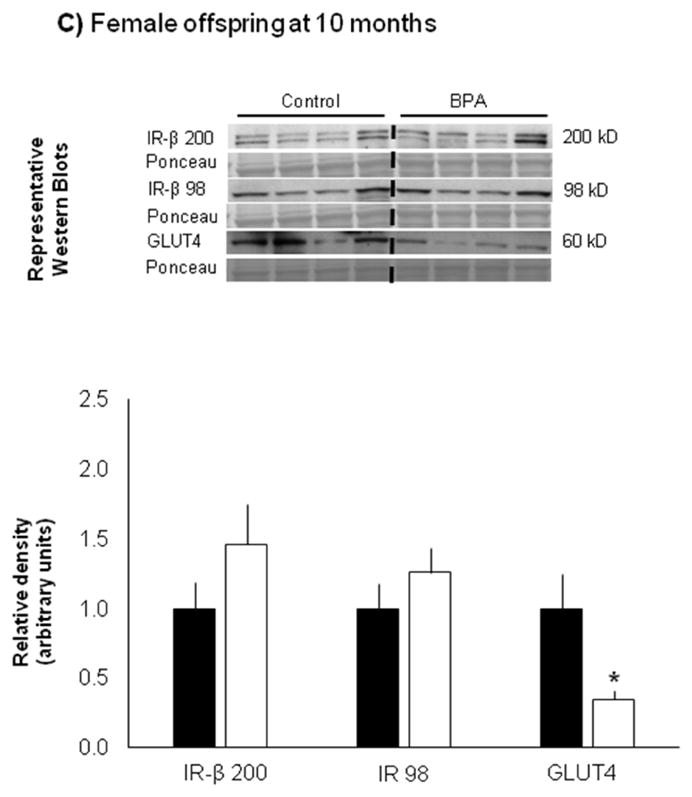
Representative Western Blots and quantitative analysis of the protein abundance of the insulin receptor beta (IR-β) and the glucose transporter 4 (GLUT4) in skeletal muscle from male control (solid bars; n = 5) and BPA-treated (open bars; n = 5) rat offspring at (A) 3 weeks and (B) 10 months of postnatal age and female control (solid bars; n = 5) and BPA-treated (open bars; n = 5) rat offspring at (C) 10 months of postnatal age. Ponceau S staining served as a loading control. Values are mean ± SEM. *P< 0.05 versus control within the same immunoblot; Student’s t test.
COMMENT
Perinatal exposure to BPA was associated with age- and sex-dependent changes in glucose tolerance and insulin sensitivity, consistent with previous rodent studies.14;17;22;23 Since blood glucose regulation is determined by both insulin secretion and peripheral insulin sensitivity we determined the effects of perinatal BPA on the protein abundance of components of the insulin signaling pathways in offspring liver and skeletal muscle. The present study showed lower protein abundance of GLUT2 and higher protein abundance of IRS-1 in the liver of male BPA-treated offspring at weaning. In addition, both BPA male and female offspring had lower protein abundance of GLUT4 in skeletal muscle in adulthood.
Higher abundance of the insulin receptor precursor molecule in male offspring liver at weaning, as well as in skeletal muscle in adulthood, was not associated with age-, sex-, or tissue-specific changes in the protein abundance of the mature, functional IR-β subunit. These data contrast with decreased abundance of the mature IR-β subunit in liver and skeletal muscle from adult rats after exposure to a high dose (200 mg/kg body weight) of BPA.24,25 Conversely, the protein abundance of IRS-1 was higher in the liver of male BPA-treated offspring, consistent with BPA-increased IRS-1 in adult mouse liver. 26 In the latter study, the authors speculated that higher liver protein abundance of IRS-1 in BPA than control mice may counteract the BPA-induced decrease in insulin receptor phosphorylation as a compensatory mechanism to avoid insulin resistance.26 Whether BPA altered insulin receptor phosphorylation in the current study is unknown, since that the data are limited by the collection of offspring tissues after an overnight fast and not under insulin-stimulated conditions.
At weaning, the protein abundance of the bi-directional glucose transporter GLUT2 was lower in liver tissue from BPA- than from control-males. Similarly, lower GLUT2 abundance has been demonstrated in isolated pancreatic islets in vitro,27 in adult rat testis and pancreas in vivo,28 and in the pancreas of male and female offspring after BPA treatment.17 In contrast, studies of adult male mice and rats exposed to BPA demonstrated variable, dose-dependent effects on GLUT2 expression in the liver.24;29 Notably, lower liver GLUT2 abundance in the current study did not likely impair liver maintenance of blood glucose levels in the fasted state, since there were no differences in fasting blood glucose levels between control and BPA males at 3 weeks of age.
Lower abundance of the glucose transporter GLUT4 in skeletal muscle from adult male and female offspring is consistent with previous studies of BPA-treated adult male rats. 25 Since skeletal muscle is the major peripheral site of glucose uptake, usage and storage, any BPA-induced deficiency in skeletal muscle insulin signaling is likely to predispose offspring to the development of insulin resistance.30 Moreover, heterozygous GLUT4 knockout mice exhibit peripheral insulin resistance, specifically implicating the GLUT4 transporter in the development of insulin resistance.31–33 Accordingly, in the current study both male and female adult offspring were insulin resistant, as evidenced by higher insulin:glucose ratios and greater area under the insulin curves during the glucose tolerance test. However, since tissue for protein studies was not collected at the time of the glucose tolerance test further mechanistic studies are required to confirm that lower GLUT4 abundance contributes to BPA-induced glucose intolerance and to determine whether perinatal BPA affects translocation of the GLUT4 transporter to the plasma membrane and subsequent glucose uptake.25
Perinatal exposure to BPA induces sex-specific changes in rat liver lipid metabolism34 and disrupts sexually dimorphic behaviors in mice.35 The molecular mechanism underlying the sex-specific effects of BPA in these studies and in the current study is unknown, but may be mediated by BPA interactions with estrogen receptors and estrogen signaling pathways. BPA can bind to both classical and non-classical G-protein-coupled estrogen receptors36–38 that regulate central and peripheral glucose metabolism39 and may interfer with estrogen signaling by activation or inhibition of the receptor.40 Classical estrogen receptors show sex- and tissue-specific patterns of expression throughout development, but whether these signaling pathways are disrupted during perinatal development in the insulin sensitive tissues of BPA-exposed offspring is unknown. BPA may also alter insulin signaling by altered methylation of genes, such as GLUT4.41 Indeed, altered methylation of the estrogen receptor α (Esr1) and several other genes has been shown following perinatal exposure to BPA.35;42 Gene methylation and demethylation is catalyzed by DNA methyltransferase (DNMT) enzymes. Accordingly, altered expression of the enzymes DNMT1 and DNMT3a have been demonstrated in rodent brain tissue35 and in preadipocytes exposed to BPA in vivo and in vitro, respectively.19 Further studies of receptor expression patterns and site-specific gene methylation are required to correlate epigenetic effects of BPA, sex- and tissue-specific changes in gene expression and offspring phenotypes. In addition, although there were no differences in weights between control and BPA offspring in the current study, changes in the insulin signaling pathway may have occurred secondary to BPA-induced changes in offspring body composition (fat mass), lipid homeostasis and/or inflammation.19;34
Using a model of maternal treatment with BPA that produces maternal and newborn plasma BPA concentrations that are similar to the range of values measured in serum from pregnant women and human umbilical cord blood19 we have shown that BPA disrupts glucose homeostasis and alters the abundance of insulin signaling components in the exposed offspring. Early life exposure to BPA should therefore be considered a possible risk factor for the development of insulin resistance and diabetes.
Acknowledgments
Financial Support: This work was supported by the National Institutes of Health Grants R21ES023112-01 (MD, MGR) and RO3 HD079722-01 (JKJ, MD, MGR), and National Center for Advancing Translational Sciences UCLA- CTSI Grant U11TR000124 (MD).
The authors thank Stacy Behare for technical assistance.
Footnotes
Conflicts: The authors report no conflict of interest
Paper presentation information: SMFM’s 36th Annual Pregnancy Meeting, Atlanta GA, February 1–6, 2016
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Jocelyn PC. The enzymic oxidation of glutathione in rat liver homogenates. Biochem J. 1970;117(5):947–949. doi: 10.1042/bj1170947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Desai M, Jellyman JK, Ross MG. Epigenomics, gestational programming and risk of metabolic syndrome. Int J Obes (Lond) 2015;39(4):633–641. doi: 10.1038/ijo.2015.13. [DOI] [PubMed] [Google Scholar]
- 4.Rubin BS, Soto AM. Bisphenol A: Perinatal exposure and body weight. Mol Cell Endocrinol. 2009;304(1–2):55–62. doi: 10.1016/j.mce.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlisle J, Chan D, Golub M, Henkel S, Painter P, et al. Office of Enrironmental Health Hazard Assessment. Toxicological Profile for Bisphenol A. California Environmental Protection Agency; 2009. pp. 1–47. [Google Scholar]
- 6.Calafat AM, Ye X, Wong LY, Reidy JA, Needham LL. Exposure of the U.S. population to bisphenol A and 4-tertiary-octylphenol: 2003–2004. Environ Health Perspect. 2008;116(1):39–44. doi: 10.1289/ehp.10753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV. Human exposure to bisphenol A (BPA) Reprod Toxicol. 2007;24(2):139–177. doi: 10.1016/j.reprotox.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 8.Saltiel AR, Kahn CR. Insulin signalling and the regulation of glucose and lipid metabolism. Nature. 2001;414(6865):799–806. doi: 10.1038/414799a. [DOI] [PubMed] [Google Scholar]
- 9.Silver MK, O’Neill MS, Sowers MR, Park SK. Urinary bisphenol A and type-2 diabetes in U.S. adults: data from NHANES 2003–2008. PLoS ONE. 2011;6(10):e26868. doi: 10.1371/journal.pone.0026868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shankar A, Teppala S. Relationship between urinary bisphenol A levels and diabetes mellitus. J Clin Endocrinol Metab. 2011;96(12):3822–3826. doi: 10.1210/jc.2011-1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melzer D, Rice NE, Lewis C, Henley WE, Galloway TS. Association of urinary bisphenol a concentration with heart disease: evidence from NHANES 2003/06. PLoS ONE. 2010;5(1):e8673. doi: 10.1371/journal.pone.0008673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lang IA, Galloway TS, Scarlett A, Henley WE, Depledge M, Wallace RB, et al. Association of urinary bisphenol A concentration with medical disorders and laboratory abnormalities in adults. JAMA. 2008;300(11):1303–1310. doi: 10.1001/jama.300.11.1303. [DOI] [PubMed] [Google Scholar]
- 13.Alonso-Magdalena P, Morimoto S, Ripoll C, Fuentes E, Nadal A. The estrogenic effect of bisphenol A disrupts pancreatic beta-cell function in vivo and induces insulin resistance. Environ Health Perspect. 2006;114(1):106–112. doi: 10.1289/ehp.8451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu J, Yu P, Qian W, Li Y, Zhao J, Huan F, et al. Perinatal bisphenol A exposure and adult glucose homeostasis: identifying critical windows of exposure. PLoS ONE. 2013;8(5):e64143. doi: 10.1371/journal.pone.0064143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ropero AB, Alonso-Magdalena P, Garcia-Garcia E, Ripoll C, Fuentes E, Nadal A. Bisphenol-A disruption of the endocrine pancreas and blood glucose homeostasis. Int J Androl. 2008;31(2):194–200. doi: 10.1111/j.1365-2605.2007.00832.x. [DOI] [PubMed] [Google Scholar]
- 16.Alonso-Magdalena P, Ropero AB, Carrera MP, Cederroth CR, Baquie M, Gauthier BR, et al. Pancreatic insulin content regulation by the estrogen receptor ER alpha. PLoS ONE. 2008;3(4):e2069. doi: 10.1371/journal.pone.0002069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wei J, Lin Y, Li Y, Ying C, Chen J, Song L, et al. Perinatal exposure to bisphenol A at reference dose predisposes offspring to metabolic syndrome in adult rats on a high-fat diet. Endocrinol. 2011;152(8):3049–3061. doi: 10.1210/en.2011-0045. [DOI] [PubMed] [Google Scholar]
- 18.Ma Y, Xia W, Wang DQ, Wan YJ, Xu B, Chen X, et al. Hepatic DNA methylation modifications in early development of rats resulting from perinatal BPA exposure contribute to insulin resistance in adulthood. Diabetologia. 2013;56(9):2059–2067. doi: 10.1007/s00125-013-2944-7. [DOI] [PubMed] [Google Scholar]
- 19.Desai M, Jellyman J, Han G, Ferrini M, Ross MG. In Vivo and In Vitro BPA Exposture Effects on Adiposity and Appetite. Environ Health Perspect. 2016 In press. [Google Scholar]
- 20.Ikezuki Y, Tsutsumi O, Takai Y, Kamei Y, Taketani Y. Determination of bisphenol A concentrations in human biological fluids reveals significant early prenatal exposure. Hum Reprod. 2002;17(11):2839–2841. doi: 10.1093/humrep/17.11.2839. [DOI] [PubMed] [Google Scholar]
- 21.Desai M, Guang H, Ferelli M, Kallichanda N, Lane RH. Programmed upregulation of adipogenic transcription factors in intrauterine growth-restricted offspring. Reprod Sci. 2008;15(8):785–796. doi: 10.1177/1933719108318597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alonso-Magdalena P, Vieira E, Soriano S, Menes L, Burks D, Quesada I, et al. Bisphenol A exposure during pregnancy disrupts glucose homeostasis in mothers and adult male offspring. Environ Health Perspect. 2010;118(9):1243–1250. doi: 10.1289/ehp.1001993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garcia-Arevalo M, Alonso-Magdalena P, Rebelo Dos SJ, Quesada I, Carneiro EM, Nadal A. Exposure to bisphenol-A during pregnancy partially mimics the effects of a high-fat diet altering glucose homeostasis and gene expression in adult male mice. PLoS ONE. 2014;9(6):e100214. doi: 10.1371/journal.pone.0100214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jayashree S, Indumathi D, Akilavalli N, Sathish S, Selvaraj J, Balasubramanian K. Effect of Bisphenol-A on insulin signal transduction and glucose oxidation in liver of adult male albino rat. Environ Toxicol Pharmacol. 2013;35(2):300–310. doi: 10.1016/j.etap.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 25.Indumathi D, Jayashree S, Selvaraj J, Sathish S, Mayilvanan C, Akilavalli N, et al. Effect of bisphenol-A on insulin signal transduction and glucose oxidation in skeletal muscle of adult male albino rat. Hum Exp Toxicol. 2013;32(9):960–971. doi: 10.1177/0960327112470273. [DOI] [PubMed] [Google Scholar]
- 26.Batista TM, Alonso-Magdalena P, Vieira E, Amaral ME, Cederroth CR, Nef S, et al. Short-term treatment with bisphenol-A leads to metabolic abnormalities in adult male mice. PLoS ONE. 2012;7(3):e33814. doi: 10.1371/journal.pone.0033814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song L, Xia W, Zhou Z, Li Y, Lin Y, Wei J, et al. Low-level phenolic estrogen pollutants impair islet morphology and beta-cell function in isolated rat islets. J Endocrinol. 2012;215(2):303–311. doi: 10.1530/JOE-12-0219. [DOI] [PubMed] [Google Scholar]
- 28.D’Cruz SC, Jubendradass R, Jayakanthan M, Rani SJ, Mathur PP. Bisphenol A impairs insulin signaling and glucose homeostasis and decreases steroidogenesis in rat testis: an in vivo and in silico study. Food Chem Toxicol. 2012;50(3–4):1124–1133. doi: 10.1016/j.fct.2011.11.041. [DOI] [PubMed] [Google Scholar]
- 29.Marmugi A, Ducheix S, Lasserre F, Polizzi A, Paris A, Priymenko N, et al. Low doses of bisphenol A induce gene expression related to lipid synthesis and trigger triglyceride accumulation in adult mouse liver. Hepatology. 2012;55(2):395–407. doi: 10.1002/hep.24685. [DOI] [PubMed] [Google Scholar]
- 30.DeFronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009;32(Suppl 2):S157–S163. doi: 10.2337/dc09-S302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zisman A, Peroni OD, Abel ED, Michael MD, Mauvais-Jarvis F, Lowell BB, et al. Targeted disruption of the glucose transporter 4 selectively in muscle causes insulin resistance and glucose intolerance. Nat Med. 2000;6(8):924–928. doi: 10.1038/78693. [DOI] [PubMed] [Google Scholar]
- 32.Stenbit AE, Tsao TS, Li J, Burcelin R, Geenen DL, Factor SM, et al. GLUT4 heterozygous knockout mice develop muscle insulin resistance and diabetes. Nat Med. 1997;3(10):1096–1101. doi: 10.1038/nm1097-1096. [DOI] [PubMed] [Google Scholar]
- 33.Kadowaki T. Insights into insulin resistance and type 2 diabetes from knockout mouse models. J Clin Invest. 2000;106(4):459–465. doi: 10.1172/JCI10830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Strakovsky RS, Wang H, Engeseth NJ, Flaws JA, Helferich WG, Pan YX, et al. Developmental bisphenol A (BPA) exposure leads to sex-specific modification of hepatic gene expression and epigenome at birth that may exacerbate high-fat diet-induced hepatic steatosis. Toxicol Appl Pharmacol. 2015;284(2):101–112. doi: 10.1016/j.taap.2015.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kundakovic M, Gudsnuk K, Franks B, Madrid J, Miller RL, Perera FP, et al. Sex-specific epigenetic disruption and behavioral changes following low-dose in utero bisphenol A exposure. Proc Natl Acad Sci U S A. 2013;110(24):9956–9961. doi: 10.1073/pnas.1214056110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alonso-Magdalena P, Laribi O, Ropero AB, Fuentes E, Ripoll C, Soria B, et al. Low doses of bisphenol A and diethylstilbestrol impair Ca2+ signals in pancreatic alpha-cells through a nonclassical membrane estrogen receptor within intact islets of Langerhans. Environ Health Perspect. 2005;113(8):969–977. doi: 10.1289/ehp.8002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nadal A, Alonso-Magdalena P, Soriano S, Quesada I, Ropero AB. The pancreatic beta-cell as a target of estrogens and xenoestrogens: Implications for blood glucose homeostasis and diabetes. Mol Cell Endocrinol. 2009;304(1–2):63–68. doi: 10.1016/j.mce.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 38.Alonso-Magdalena P, Ropero AB, Soriano S, Garcia-Arevalo M, Ripoll C, Fuentes E, et al. Bisphenol-A acts as a potent estrogen via non-classical estrogen triggered pathways. Mol Cell Endocrinol. 2012;355(2):201–207. doi: 10.1016/j.mce.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 39.Faulds MH, Zhao C, Dahlman-Wright K, Gustafsson JA. The diversity of sex steroid action: regulation of metabolism by estrogen signaling. J Endocrinol. 2012;212(1):3–12. doi: 10.1530/JOE-11-0044. [DOI] [PubMed] [Google Scholar]
- 40.Wetherill YB, Akingbemi BT, Kanno J, McLachlan JA, Nadal A, Sonnenschein C, et al. In vitro molecular mechanisms of bisphenol A action. Reprod Toxicol. 2007;24(2):178–198. doi: 10.1016/j.reprotox.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 41.Wang J, Cao M, Yang M, Lin Y, Che L, Fang Z, et al. Intra-uterine undernutrition amplifies age430 associated glucose intolerance in pigs via altered DNA methylation at muscle GLUT4 promoter. Br J Nutr. 2016;116(3):390–401. doi: 10.1017/S0007114516002166. [DOI] [PubMed] [Google Scholar]
- 42.Kundakovic M, Champagne FA. Epigenetic perspective on the developmental effects of bisphenol A. Brain Behav Immun. 2011;25(6):1084–1093. doi: 10.1016/j.bbi.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]