Abstract
Background
Well-being is important to healthy aging. The present study examined the trajectories and determinants of well-being in older women (n = 248) over a 39-month period.
Methods
Participants completed measures of optimism, pessimism, functional limitations, physical activity, and self-efficacy. Well-being, operationalized as life satisfaction, was assessed at baseline, 12, 24 and 39 months. Latent growth and class analyses examined trajectories of well-being and antecedents of change.
Results
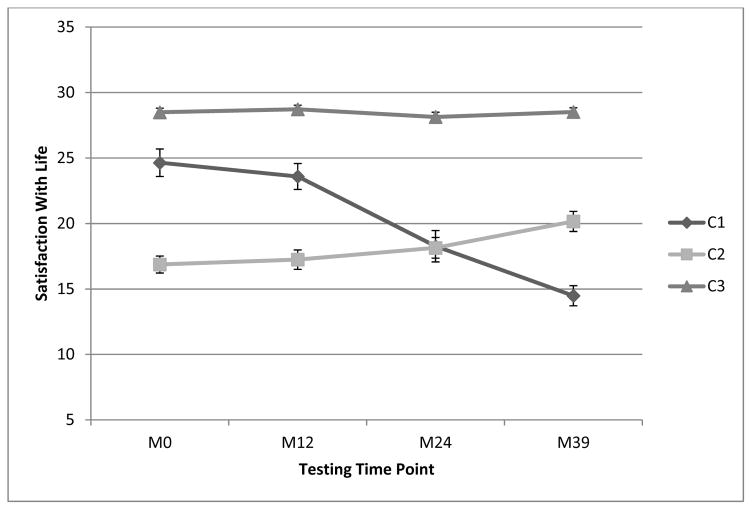
The overall model testing a linear growth pattern fit the data well, [χ2(df=5)=7.77, p=.17, CFI=.98, RMSEA=.05] revealing an overall significant, but modest decline in well-being. Three latent classes were further revealed; one class (n=34, 13.3%) began with moderate levels of well-being (Mi=25.4, p<.001), which decreased across time (Ms=−3.12, p<.001). A second class (n=54, 21.8%) began with lower well-being (Mi=17.1, p<.001) that remained low (Ms=.702, p=.378). The third class (n=161, 64.9%) started with high levels of well-being (Mi=28.4, p<.001) which were maintained (Ms=−.027, p=.841). Higher optimism and lower pessimism differentiated between declining well-being and maintaining well-being across time.
Conclusions
Optimism and pessimism appear to differentiate patterns of well-being in community-dwelling older women. Promoting optimism-inducing strategies may be useful for maintaining well-being in older adulthood.
Keywords: Aging, Well-Being, Optimism, Latent Class Analysis, Women’s Health
Introduction
Older adults are the fastest growing subset of the population with numbers expected to double from 35 million to 71 million by 2030 (Goulding, Rogers & Smith, 2003). These increases are likely to result in considerable health, economic, and societal burden, as well as have implications for well-being, a key component of successful aging. Overall well-being involves an individual’s cognitive and affective evaluations of their life and encompasses constructs such as life satisfaction, happiness, physical well-being, personal growth and satisfying social relationships (Diener, 2009). However, declining well-being has been associated with increasing age, as the level of dependence (i.e., greater functional limitations) and institutionalization increases (Kostka & Jachimowicz, 2010) and steep declines in well-being in older adulthood appear to be related to imminent mortality and often occur during late older-adulthood (Gerstorf et al., 2010).
It is important to note that declines in well-being do not universally accompany aging. Indeed some research indicates that well-being remains stable in older age despite increasing comorbidities and functional limitations (Kunzmann, Little & Smith, 2000), which has been labeled a “paradox”. Data from the German Socio-Economic Panel indicated that life satisfaction is a relatively stable construct across time. Life satisfaction, or well-being, may even become more stable in older adulthood as these judgments often incorporate evaluations of past accomplishments in addition to current experiences (Kunzmann et al., 2000). Furthermore, a number of behavioral, demographic, and personal factors have been associated with the maintenance of well-being in older adulthood.
Covariates of Well-Being Trajectories
Physical factors, such as functional limitations and disability, play an important role in well-being trajectory in later life. Functional limitations involve perceived deterioration of specific aspects of physical health and decreasing levels of independence for older adults, which can negatively impact well-being in older adult populations (Verbrugge & Jette, 1994). Over half of older adults report limitations in at least one domain of physical function and declines in functional ability are more prevalent in older women (National Center for Health Statistics; Woods et al., 2005). Perceptions of physical limitations, in addition to the objective degree of physical impairment, influence appraisals of well-being (Rejeski & Mihalko, 2001).
Healthy aging entails not only maintenance of physical health and prevention of disease and disability, but also psychological resilience (Bowling & Iliffe, 2011). Psychosocial factors, both dispositional and modifiable, such as optimism and self-efficacy, are important predictors of well-being across the lifespan (Kostka & Jachimowicz, 2010). Optimism is a dispositional tendency towards positive expectancies across various life domains (Steptoe, Wright, Kunz-Ebrecht, & Iliffe, 2006). Optimism has been associated with healthy aging and generalized optimistic expectations are correlated with better health, health outcomes, and well-being among older adults (Carver, Scheier, & Segerstrom, 2010; Steptoe et al., 2006). Importantly, optimism is associated with physical health status in older adults, independent of demographic factors, chronic illness, negative affect and BMI (Steptoe et al., 2006). Carver and colleagues (2010) argue that the trait of optimism provides cognitive, coping, and contextual resources that promote better mental and physical health. Conversely, pessimism is associated with poorer health and health-damaging behaviors. Where optimists tend to be confident and persistent in the face of challenges, pessimists tend to be doubtful and hesitant.
Self-efficacy, a modifiable personal factor that represents individual beliefs in ability to accomplish specific tasks, influences health outcomes and well-being, in part, via health-specific behaviors (Bandura, 2001). Promoting well-being in older adulthood requires encouraging positive attitudes and behaviors over the life course (Bowling & Iliffe, 2011), processes which rely, at least in part, on self-efficacy. Personal agency, or a sense of personal control in a variety of life circumstances, is rooted in self-efficacy beliefs and provides crucial information for life satisfaction evaluations. Individuals who have high efficacy evaluations believe that they are capable of influencing specific aspects of behavior and well-being. As later life is marked by specific challenges such as changes in physical abilities and social structure, older adults need to leverage efficacy and agency beliefs more rigorously to maintain perceived well-being (Bandura, 2001; Chipperfield et al., 2012). Self-efficacy for walking is especially important for older adults as changes in physical function may threaten well-being; indeed walking ability is a vital activity of daily living in older adulthood. Evidence indicates that self-efficacy can be enhanced in older adult populations (McAuley et al., 2011), which may influence trajectories of well-being in late life. One of the ways through which optimism and self-efficacy influence health outcomes is by supporting the formation of habitual health behaviors, such as physical activity. Physical activity itself is associated with well-being primarily through its effects on preserving physical and mental health status and preventing functional limitations (Motl & McAuley, 2010). These personal and physical health factors have implications for how individuals approach and interpret life events, confront adversity, succeed in goal-directed behavior, and experience aging (Bandura, 2001; Carver et al., 2010). Changes in well-being experienced in older adulthood may vary greatly with factors such as socio-demographics, concomitant diseases, functional status, and lifestyle behaviors (Barger, Donoho, & Wayment, 2009; McAuley et al., 2008; Motl & McAuley, 2010).
The Present Study
Most studies describing longitudinal patterns of well-being have treated their samples as homogeneous groups and examined only mean level changes in well-being across time rather than considering whether differential trajectories of growth in well-being in older adulthood exist. Physical and psychosocial factors may influence individuals differently, hence the importance of examining the potential for divergent trajectories of change among sub-groups. The purpose of this study was to examine well-being growth trajectories in older adult women and to determine whether differing classes of change existed across time. A secondary purpose was to determine differential patterns of change across time could be explained by baseline levels of psychosocial factors, physical activity, co-morbidities, demographics, and functional limitations, all of which have previously been linked to well-being (Barger, Donoho, & Wayment, 2009; McAuley et al., 2008; Rejeski & Mihalko, 2001).
Given that sub-group trajectories of well-being in older adults have been infrequently studied, we conceptualized a relatively simple pattern of changes across time in this study. It was hypothesized that we would observe three sub-groups characterized by 1) the maintenance of well-being, 2) declines in well-being, and 3) improvements in well-being across time. To evaluate the fit of the proposed three-class solution, it is tested against a two class and four class solution. We hypothesized that positive trends in well-being would occur in individuals with higher levels of optimism, self-efficacy, and physical activity whereas declines in well-being would be associated with initially higher levels of pessimism and functional limitations. It was further hypothesized that older age and higher co-morbidity would be associated with declining well-being.
Method
Participants
Older (M age = 68.10 years, range 59–84 years) African American (n = 81) and Caucasian (n = 167) women were recruited to participate in a prospective study of women’s health (McAuley et al., 2008). Inclusion criteria for participation in the program were: (a) female, (b) race being African-American or Caucasian, (c) ethnicity being Non-Hispanic/Latino, (d) no history of neurological disorder, (e) no history of physical disability that would prohibit an assessment of physical function, and (f) adequate mental status, as assessed by the Pfeiffer Mental Status Questionnaire (Pfeiffer, 1975). Participants were recruited via the local media and flyers sent to senior centers, fitness centers, adult health care facilities, local businesses, and African American churches.
Measures
Demographic and health information
Basic demographic information (i.e. race, age, income, education) and a health history were collected from all participants. From the health history questionnaire, we calculated a summary score for disease status, with higher scores reflecting more co-morbid conditions. Standard comorbidities, such as stroke, myocardial infarction, diabetes, hypertension, kidney disease, chronic obstructive pulmonary disease, cancer, etc., were identified and summed to create a cumulative incidence score per participant (e.g. score of 2 indicates the presence of 2 illnesses).
Subjective Well-Being
The 5-item Satisfaction with Life Scale (SWLS; Diener, Emmons, Larsen & Griffin, 1985) was used to assess subjective well-being. Each item is a 7-point Likert scale from strongly disagree (1) to strongly agree (7). Reliability of scores for this measure was very good (α = .87). Pavot and Diener’s review of research using the SWLS suggests that it is sensitive enough to detect small changes in life satisfaction and is valid in older adult populations (Pavot & Diener, 2009).
Dispositional Optimism and Pessimism
The Life Orientation Test—Revised (LOT-R) was used to assess dispositional optimism and pessimism (Scheier, Carver, & Bridges, 1994). The LOT-R is a 10-item measure including three items phrased positively, representing optimism (e.g., “In uncertain times, I usually expect the best”); three items phrased negatively, representing pessimism (e.g., “If something can go wrong for me, it will”); and four filler items not used in scoring. Participants indicated the extent of their agreement with each of the items on a 5-point Likert scale, where 0 = strongly disagree; 1 = disagree, 2 = neutral, 3 = agree, and 4 = strongly agree. The LOT-R is an abbreviated version of the original Life Orientation Test (Scheier & Carver, 1985) and has demonstrated a strong correlation with the original LOT (r = 0.95) (Scheier et al., 1994). Reliability of scores for the pessimism (α = .75) and the optimism (α = .69) subscales were acceptable.
Functional Limitations
The function component of the Abbreviated Late Life Function and Disability Instrument (LL-FDI; McAuley et al., 2005) was used to assess functional limitations. This measure consists of three subscales assessing advanced lower extremity function, basic lower extremity function, and upper extremity function which are summed to provide an index of overall functional limitations. Individuals are asked to rate the extent to which they feel limited in performing certain activities (e.g. getting into and out of a car or pouring from a large pitcher) by selecting a value from 1 (cannot do) to 5 (none), with higher scores reflecting less difficulty in performing tasks.
Self-Efficacy
Walking self-efficacy assessed participants’ beliefs in their capability to successfully walk for a specified duration of time, ranging from 5- to 40-minute bouts, at a moderately fast pace without stopping and reflects a task-specific measure of self-efficacy. The self-efficacy for walking scale (available here: http://www.epl.illinois.edu/meas_sewdur.html) has been previously validated in older adults (McAuley et al., 2000). The scale consisted of eight items, with each item representing an incrementally longer duration ranging from 5 to 40 minutes (e.g. I believe that I can walk for 5 minutes at a moderately fast pace without stopping). The eight items, with ratings ranging from 0 (not confident at all) to 100 (completely confident), were averaged to calculate a total score, resulting in a possible range of 0–100 for each efficacy scale. Reliability of scores was excellent (α = .98).
Physical Activity
The Physical Activity Scale for the Elderly (PASE) was used to assess physical activity (Washburn, Smith, Jette, & Janney, 1993). It is a 10-item instrument specifically designed to assess physical activity levels in large samples of older adults and the factor structure and construct validity have been validated in community-dwelling older adults (Martin et al., 1999). The PASE combines information from several domains including leisure, household, and occupational activity. The total PASE score was computed by multiplying the amount of time spent in each activity (hours/week) or participation (yes/no) in an activity by the empirically derived item weights and summing over all activities. This provides an overall activity count for participation in physical activity over the previous seven days. Higher scores reflect greater physical activity participation.
Procedures
Well-being was collected at baseline and months 12, 24, and 39 of a prospective study of older adult African American and Caucasian women. Participants completed baseline measures of optimism, pessimism, physical activity, demographics, self-efficacy, and functional limitations which were then used to differentiate trajectories of change in well-being assessed across the 39 month period. Prior to any involvement in the study, participants were screened for eligibility and reviewed and signed an informed consent document. A questionnaire assessing basic demographics and health and medication information was collected, which was followed by the psychosocial questionnaire packet. All procedures and protocols were approved by an Institutional Review Board.
Data Analysis
The data were analyzed using Mplus software (version 6.0) with the robust full information likelihood estimator (Múthen & Múthen, 2010). We examined changes in well-being across the 39-month period using standard linear latent growth curve modeling (LGM). This involved testing a fixed linear time series to establish initial status and rate of change in well-being across time. We evaluated the fit of the LGM using multiple criteria [e.g., significant p value associated with χ2, comparative fit index (CFI) ≥ .95, and the root mean square error of approximation (RMSEA) ≤ .08](Hu & Benter, 1999).
Next we conducted a series of latent class analyses (LCA) to determine whether there were subgroups within the sample that exhibited different initial levels and different patterns of growth in well-being over time. We conducted analyses to determine whether the hypothesized three classes fit the data and compared this to both a two and four class solution. The final class solution was based on the Bayesian Information Criterion (BIC) and the parametric bootstrapped likelihood ratio test (BLRT) following the guidelines provide by Burnham and Anderson (2004) and Rafferty (1995). In addition, entropy values and most likely class membership probabilities were computed with values ranging between 0 and 1 with higher values indicating higher likelihood of replication. Finally, we conducted a conditional LCA using optimism, pessimism, self-efficacy, functional limitations, co-morbidities, and physical activity as auxiliary variables. The auxiliary variables allowed us to test whether mean level values on each of these variables differ for any underlying latent classes. The auxiliary variables can be considered substantive covariates that inform class membership and can support theoretical statements as to which covariates/auxiliary factors distinguish between classes. As it is not possible to simultaneously examine multiple categorical auxiliary variables, income and education were analyzed separately. All other analyses were conducted simultaneously but the effects are reported independently.
Results
Sample Characteristics and Missing Data
Descriptive statistics for the sample are shown in Table 1 and correlations among study variables in Table 2. Of the 248 women enrolled in the study at baseline, 231 were available at 12 months, 217 at 24 months, and 183 at 39 months. Missing data for primary study outcome of well-being at 0, 12, 24, and 39 months, were 0%, 7.2%, 12.9%, and 26.5%, respectively. For the baseline antecedents of change in well-being variables, missing data was as follows, race (0%), age (0%), income (7.6%), education (2%), comorbidities (0%), physical activity (4.4%), functional status (0%), walking self-efficacy (0%), optimism (8.0%) and pessimism (8%). Study characteristics have been previously reported in McAuley et al., 2008.
Table 1.
Baseline Descriptive Statistics for Study Variables and Demographics.
| Range | Mean ± SD (n = 248) | |
|---|---|---|
| Age | 59–84 yrs | 68.1 ± 6.10 |
| Well-Being (SWLS) | 5–35 | 25.5 ± 6.50 |
| Optimism (LOT-R) | 3–12 | 8.71 ± 1.77 |
| Pessimism (LOT-R) | 0–12 | 3.49 ± 2.29 |
| Number of comorbidities | 0–4 | 1.13 ± 1.03 |
| Physical activity (PASE) | 0–425 | 156 ± 70.6 |
| Functional limitations (LL-FDI) | 37–75 | 63.7 ± 7.80 |
| Self-efficacy for walking | 0–100 | 71.6 ± 31.80 |
| College-graduate | - | 39.5% n = 98 |
| Income > $40,000/year | - | 35.9% n = 89 |
| Married | - | 52.4% n = 129 |
Note: Study characteristics have been previously reported in McAuley et al., 2008.
Table 2.
Correlations among Auxiliary variables and Well-Being at Baseline
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | |
|---|---|---|---|---|---|---|---|---|
| 1. Age | -- | |||||||
| 2. Co-morbidity | .11 | -- | ||||||
| 3. Self-efficacy | −.23** | −.41** | -- | |||||
| 4. Physical Activity | −.20** | −.28** | .34** | -- | ||||
| 5. Functional Limitation | −.26** | −.40** | .56** | .37** | -- | |||
| 6. Optimism | .01 | −.08 | .03 | .11 | .07 | -- | ||
| 7. Pessimism | .03 | .10 | −.13* | −.11 | −.09 | −.41** | -- | |
| 8. Well-being | −.03 | −.27** | .30** | .12 | .43** | .20** | −.26** | -- |
p <. 05,
p < .01
Latent Growth Curve Model
The overall model testing of a linear growth pattern provided an excellent fit to the data, χ2 (df = 5) = 7.77, p =.17 CFI = .98, RMSEA = .05. Both the intercept (25.56) and the slope (−0.37) were significant, as were the variances (p < .05). Overall, there was a significant but modest reduction in well-being across the 39-month period. The slope and the intercept were not significantly correlated (r = −.13, p = .41). An additional test for the presence of a quadratic trajectory was non-significant (−0.03, p = .78) and not pursued further.
Latent Class Growth Modeling
The hypothesized three-class solution was initially compared for goodness of fit with a two and four class solution using the BIC statistics and the parametric bootstrapped likelihood ratio test (BLRT). The three- and four-class solutions both fit the data well. The three- and four-class models were a better fit than the two-class model with a decrease in the BIC that was sufficiently large (−25 and −34, respectively) to suggest the non-equivalency of models (Rafferty, 1995). This was further supported by significant (p <.0001) BLRTs. The three- and four-class solutions were more similar with a small decrease (−9) in the BIC for the four-class solution over the three-class solution. The four-class solution fit the data slightly better but resulted in one class with a very small sample size (n = 6) and two classes with similar trajectories, which essentially supported a three-class solution. To be conservative and parsimonious, the three-class solution was further pursued.
Examination of the three classes extracted revealed one (C1) small (n = 33, 13.3%) class that began with higher levels of well-being at baseline (Mi =25.4, p < .001) which decreased across time (Ms = −3.12, p < .001). The second class (C2) (n = 54, 21.8%) began with lower values of well-being (Mi =17.1, p < .001) which remained low across the 39-month period (Ms = .702, p = .378). The third, largest class (C3) (n = 161, 64.9%) showed high initial levels of well-being (Mi =28.4, p < .001) which were maintained over time (Ms = −.027, p = .841). For this three-class model, entropy was .73 and most-likely class member probabilities varied between .78 and .91. These figures suggest that the model could be replicated 73% of the time and that class assignment was between 78% and 91% accurate.
Conditional Latent Class Growth Modeling with Auxiliary Variables
The final model included age, co-morbidity, functional limitations, physical activity, and psychosocial factors (i.e., optimism, pessimism, self-efficacy) as auxiliary variables to further examine the distinctiveness of the patterns found in the LCA. The mean difference for each outcome by latent class is shown in Table 4. As can be seen, only optimism and pessimism contributed to the pattern difference between C1 (i.e., declining well-being over time) being significantly less optimistic and more pessimistic compared to individuals in C3 (i.e., maintaining high levels of well-being). None of the other variables significantly differentiated between those two classes. However, co-morbidities, functional limitations, self-efficacy, optimism and pessimism differentiated between the patterns of C2 (i.e., initial low well-being persisting across time) & C3 (initially high well-being maintained). Individuals who maintained high levels of well-being had lower comorbidity, fewer functional limitations, higher efficacy, higher optimism, and lower pessimism compared to C2. Finally, education did not differ by class and income was lower in C2 compared to C3 (p < .01) and C1 (p = .06). As these latter two constructs were measured as categorical variables, we do not include their values in Table 4.
Table 4.
Mean Values for Auxiliary Variables by Class
| Auxiliary Variable | Class 1 Mean (SE) |
Class 2 Mean (SE) |
Class 3 Mean (SE) |
|---|---|---|---|
| Age | 69.07 (1.12) | 68.34 (0.98) | 67.78 (0.50) |
| Co-Morbidities2 | 1.16 (0.18) | 1.48 (0.18) | 1.01 (0.08) |
| Functional Limitations2 | 63.18 (1.52) | 59.79 (1.44) | 65.14 (0.58) |
| Self-Efficacy2 | 73.13 (6.31) | 60.62 (5.60) | 74.91 (2.51) |
| Physical Activity | 157.1 (13.2) | 157.3 (12.4) | 158.5 (5.90) |
| Optimism1,2 | 7.83 (0.36) | 8.28 (0.27) | 9.05 (0.14) |
| Pessimism1,2 | 4.21 (0.44) | 4.18 (0.33) | 3.12 (0.19) |
difference between class 1 and class 3 at p < .05
difference between class 2 and class 3 at p < .05
Discussion
The objective of the present study was to examine the trajectory of well-being in older community-dwelling women across a 39-month period and to determine whether differential trajectories in well-being were influenced by psychosocial, lifestyle, and physical correlates of well-being. Although the overall growth pattern reflected a slight decrease in well-being over time, our latent profile analysis indicted that three distinct classes of growth patterns were present in this sample; one in which well-being was high at baseline and declined across time (C1), a second where well-being started low and stayed low (C2), and a third class in which high baseline well-being was maintained across time (C3). The first class appeared to be driving the overall decrease in well-being.
Auxiliary Covariates & Well-Being Trajectory
Comorbidity, functional limitations, and self-efficacy affected initial well-being scores. Individuals who reported initially high self-efficacy and low functional limitations were more likely to also report high well-being at baseline. Of the array of possible antecedents, only baseline levels of optimism and pessimism discriminated between the two growth patterns that started with high well-being. Specifically, optimism was higher and pessimism lower at baseline in those individuals who began with higher well-being and maintained these levels (C3) versus those who began with higher well-being and experienced declines across time (C1). Conversely, pessimism was greater and optimism lower in those individuals who demonstrated a growth pattern of well-being which declined over time (C1). In comparing C2 (well-being started low and stayed low) to C3 (well-being started high and stayed high), women in C3 had fewer comorbidities, higher income, fewer functional limitations, higher self-efficacy, higher optimism, and lower pessimism at baseline compared to individuals who initially had lower well-being (C2).
We anticipated that factors such as physical activity levels, health status, self-efficacy, and functional limitations would be determinants of well-being. They were, though none of these variables were associated with changes in well-being across time. Comorbidity, functional limitations, and self-efficacy affected the initial well-being scores but did not differentiate between individuals who maintained well-being (C2 or C3) versus those whose well-being declined (C1). None of the predictor variables differentiated between the declining well-being sub-group and the sub-group in which well-being started low and stayed low (C1 vs. C2). This finding could be due to the relative proximity of well-being in the two sub-groups. Although, C2 started with significantly lower well-being, the sample population was a generally healthy one.
Optimism & Well-Being
Only optimism and pessimism were significant contributors to the declining well-being class pattern. Optimism may influence well-being in older adulthood by decreasing negative affect, encouraging positive coping strategies, and predisposing individuals towards healthy behaviors. Previous research has demonstrated that optimists tend to experience lower negative affect, such as anxiety, depression, anger, sadness, and despair, in the face of adversity compared to more pessimistic individuals (Carver et al., 2010). The tendency for optimists to experience less distress than pessimists when faced with difficulty cannot be completely explained by disposition alone. Optimistic tendencies also influence coping strategies. Pessimism has been correlated with more escapist coping strategies, whereas optimism is associated with more pro-active coping strategies (Solberg Nes & Segerstrom, 2006). Finally, optimism appears to affect behavior such that optimist individuals tend to persevere in goal-directed behavior and engage actively in health-promoting and disease-minimizing behaviors (Carver et al., 2010). Our findings are supportive of other work in which optimism has played an important role in well-being (Carver, Smith, Petronis, & Antoni, 2006). These results suggest that optimism and pessimism appear to differentiate developing patterns of well-being in older adulthood, independent of other factors typically associated with well-being (i.e., physical activity, co-morbidities, and self-efficacy).
It would appear that being more optimistic plays a protective role in preserving well-being regardless of socio-demographic characteristics, and in the face of challenges to health. As clear benefits are associated with optimism, an important question is how optimism can be feasibly enhanced. Although optimism is viewed as stable and test-retest correlations for optimism are generally high (Lucas, Diener, & Suh, 1996; Matthews, Raikkonen, Sutton-Tyrrell, & Kuller, 2004), there are intra-individual variations in optimism, both momentarily and over extended periods. Test-retest correlations have been observed to be as low as .35 (Segerstrom, 2007), indicating that change in dispositional optimism, at least for some people, is possible.
As Carver et al. (2010) have noted, there are strategies for increasing optimism in older adults. Such strategies focus on shifting cognitive patterns into a more positive framework, which may reduce distress and encourage persistence towards personal goals (Carver et al., 2010). It is important to note that much of the intervention research has been focused on reducing negative thoughts (i.e. reducing pessimism) and less so on enhancing positive thoughts (i.e., increasing optimism) (Riskind, Sarampote, & Mercier, 1996). However, reductions in negative thinking, and by extension pessimism, are no guarantee of an increase in positive thinking and thereby optimism (Matthews et al., 2004). It has been suggested that intervention strategies should focus on both challenging negative cognitive patterns, which may be “optimism-suppressing” and actively engaging positive strategies (Carver et al., 2010; Riskind et al., 1996).
Another mechanism for increasing optimistic thinking is through cultivating social support. Social support, especially emotional support, is an antecedent of overall well-being in middle-age and older adults (Karademas, 2006). Increasing social support, especially in the very old, is crucial to well-being as it not only optimism and well-being directly (Karademas, 2006) but also impacts physical health (Everard, Lach, Fisher & Baum, 2000), mental health (Reker, 1997). Social support has been found to mediate the relationship between optimism and distress in individuals who have experienced trauma (Dougall, Hyman, Hayward, McFeeley, & Baum, 2001). However, individuals who initially are more optimistic have broader social networks and better social support (Brissette et al., 2002). Some evidence indicates that people are more accepting of optimistic individuals and find interactions with optimists to be more enjoyable (Carver, Kus, & Sheier, 1994). Given the importance of close relationships, this represents an additional advantage to optimism (Carver et al., 2010).
In addition, participation in physical activity may be related to optimism in older age. Regular physical activity is associated with positive mood and greater perceptions of happiness. Physical activity may result in higher levels of optimism through multiple pathways. Physical activity provides individuals with mastery of experiences, which is important for the development of both self-efficacy and optimistic cognitions (Kavussanu & McAuley, 1995). Physical activity may also impact optimism through its effects on anxiety and depression (Dunn, Trivedi, & O’Neal, 2001) as these affective states show a strong inverse relationship with optimism (Dewberry & Richardson, 1990). There is initial evidence that higher levels of physical activity are related to higher levels of optimism (Kavussanu & McAuley, 1995) however the directionality of this relationship remains unclear.
Boosting optimism, through using cognitive behavioral strategies, enhancing social support, or engaging in physical activity, may result in preserving well-being in later adulthood. Well-being is influenced by multiple life domains including physical health, mental health, socioeconomic factors, and social relationships (McAuley et al., 2008; Motl & McAuley, 2010). Anticipating good, rather than bad, as optimists do, is linked to core processes which dictate behavioral choices (Carver et al., 2010), and influence how individuals confront problems, interpret a variety of life situations, and recover from adversity. More optimistic individuals are more likely to engage in healthy behaviors such as physical activity, smoking cessation, and moderate alcohol consumption. Moreover, optimism has been associated with good physical health status in older adults independent of demographic factors, chronic illness, medication count, negative affectivity and BMI (Steptoe et al., 2006). Increasing optimistic thought processes may provide older adult women with cognitive and behavioral resources that promote better mental, physical and social health (Carver et al., 2010; Riskind et al., 1996), and in turn improve global well-being. It is important to note that some research indicates dangers of being overly optimistic. Maintaining realistic expectations may help individuals cope with anxiety or uncertainty (Lang, Weiss, Gerstorf & Wanger, 2013). Interventions targeting optimism in older adults should be careful to encourage positive, yet realistic, expectancies.
Strengths & Limitations
We note several strengths to this study. Rather than simply examining how well-being changed across that period, we used contemporary statistical analysis to determine whether there were underlying classes of individuals who change differentially across time. Further, we were able to establish the importance of optimism and pessimism as antecedents to these trajectories of change. We acknowledge, however, that several factors limit the generalizability of this study. There were fewer African Americans represented in our sample than Caucasians and our data likely reflect a self-selection sampling bias. However, we see the fact that 32.5% of our sample is African American as a strength because the surrounding area is approximately 12.7% African American. Our sample represents substantial diversity considering the locale. However, the sample population was relatively well-educated. There was a minority with a different pattern than reported here in the four-class solution that was tested. Further investigations with larger sample sizes may be able to elucidate an additional pattern. Despite these limitations, these data offer intriguing findings relative to the role of personal factors such as optimism in changes in well-being in older women. Future research should be directed towards addressing how to improve well-being in older adult women, perhaps through enhancing optimistic cognitions.
Conclusions
Results extend the current literature by suggesting that the trajectory of well-being in late life is complex with individual variation in change being influenced, in part, by an array of baseline parameters. These results support previous literature regarding the importance of psychological resources, such as optimism and self-efficacy, for maintaining well-being in older adulthood (Bowling & Iliffe, 2011, Carver et al., 2010). Optimism has been linked to various health benefits including better emotional well-being, more effective coping strategies, better physical health outcomes, and improved well-being (Carver et al., 2010). Our data underscore the role of optimism in maintaining well-being in older adulthood. Health professionals should consider psychological resources when examining well-being in older adults, in addition to indices of physical health status. From a personality psychology perspective, these findings emphasize the reality of individual differences. Further research is warranted, especially in older adults who are at risk of significant decreases in well-being, in order to effectively identify individuals at risk for declining well-being and develop effective intervention strategies. In the public health goal of adding years to life and life to years, it remains crucial to not only prevent disease but also to incorporate strategies to improve psychological resiliency such as enhancing optimistic cognitions.
Figure 1.
Trajectories of Well-Being Across Time by Class
Table 3.
Overall Mean Subjective Well-Being Across Time in Older Adult Women
| Mean | SE | |
|---|---|---|
| Month 0 | 25.5 | 6.50 |
| Month 12 | 25.7 | 6.33 |
| Month 24 | 24.8 | 6.85 |
| Month 39 | 24.9 | 6.58 |
Acknowledgments
EAO is funded by NIA #1F31AG042232
EM is funded by NIA #R37 AG025667 and NIA # 2R01AG020118
Footnotes
All authors declare no conflict of interest.
References
- Bandura A. Social cognitive theory: An agentic perspective. Anual Review of Psychology. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Barger SD, Donoho CJ, Wayment HA. The relative contributions of race/ethnicity, socioeconomic status, health, and social relationships to life satisfaction in the United States. Quality of Life Research. 2009;18(2):179–189. doi: 10.1007/s11136-008-9426-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A, Iliffe S. Psychological approach to successful ageing predicts future quality of life in older adults. Health and Quality of Life Outcomes. 2011;9:13. doi: 10.1186/1477-7525-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brissette I, Scheier MF, Carver CS. The role of optimism in social network development, coping, and psychological adjustment during a life transition. Journal of Personality and Social Psychology. 2002;82:102–111. doi: 10.1037//0022-3514.82.1.102. [DOI] [PubMed] [Google Scholar]
- Burnham K, Anderson D. Multimodel inference: Understanding AIC and BIC in model selection. Sociological Methods & Research. 2004;33(2):261–304. doi: 10.1177/0049124104268644. [DOI] [Google Scholar]
- Carver CS, Kus LA, Scheier MF. Effects of good versus bad mood and optimistic versus pessimistic outlook on social acceptance versus rejection. Journal of Social and Clinical Psychology. 1994;13:138–151. [Google Scholar]
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clinical Psychology Review. 2010;30(7):879–889. doi: 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, Smith RG, Petronis VM, Antoni MH. Quality of life among long-term survivors of breast cancer: Different types of antecedents predict different classes of outcomes. [Article] Psycho-Oncology. 2006;15(9):749–758. doi: 10.1002/pon.1006. [DOI] [PubMed] [Google Scholar]
- Chipperfield JG, Newall NE, Perry RP, Stewart TL, Bailis DS, Ruthig JC. Sense of control in late life: health and survival implications. Personality and Social Psychology Bulletin. 2012;38(8):1081–1092. doi: 10.1177/01461672444758. [DOI] [PubMed] [Google Scholar]
- Dewberry C, Richardson S. Effect of anxiety on optimism. Journal of Social Psychology. 1990;130(6):731–738. doi: 10.1080/00224545.1990.9924625. [DOI] [PubMed] [Google Scholar]
- Diener E. Subjective well being. In: Diener E, editor. The Science of well-being: The collected works of Ed Diener. Vol. 37. Netherlands: Springer Science and Business Media, B.V; 2009. pp. 11–58. Social Indicators Research Series. doi:10.1007-978-90-481-2350-6_2. [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Dougall AL, Hyman KB, Hayward MC, McFeeley S, Baum A. Optimism and traumatic stress. Journal of Applied Social Psychology. 2001;31:223–245. [Google Scholar]
- Dunn AL, Trivedi MH, O’Neal H. Physical activity dose-response effects on outcomes of depression and anxiety. Medicine & Science in Sports & Exercise. 2001;33(6):S587–S597. doi: 10.1097/00005768-200106001-00027. [DOI] [PubMed] [Google Scholar]
- Everard KM, Lach HW, Fisher EB, Baum C. Relationship of activity and social support to the functional health of older adults. Journal of Gerontology: Social Sciences. 2000;55B(4):S208–S212. doi: 10.1093/geronb/55.4.s208. [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Ram N, Mayraz G, Hidajat M, Lindenberger U, Wagner G, Schupp J. Late-life decline in well-being across adulthood in Germany, the United Kingdom and the United States: Something is seriously wrong at the end of life. Psychology and Aging. 2010;25(2):477–485. doi: 10.1037/a0017543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulding MR, Rogers ME, Smith SM. Public health and aging: Trends in aging - United States and worldwide (Reprinted from MMWR, vol 52, pg 101–106, 2003) Jama-Journal of the American Medical Association. 2003;289(11):1371–1373. [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Karademas EC. Self-efficacy, social support and well-being: The mediating role of optimism. Personality and Individual Differences. 2006;40:1281–1290. [Google Scholar]
- Kavussanu M, McAuley E. Exercise and optimism: Are highly active individuals more optimistic? Journal of Sport & Exercise Psychology. 1995;17:246–258. [Google Scholar]
- Kostka T, Jachimowicz V. Relationship of quality of life to dispositional optimism, health locus of control and self-efficacy in older subjects living in different environments. [Article] Quality of Life Research. 2010;19(3):351–361. doi: 10.1007/s11136-010-9601-0. [DOI] [PubMed] [Google Scholar]
- Kunzmann U, Little TD, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychology and Aging. 2000;15(3):511–526. doi: 10.1037//0882-7974.15.3.511. [DOI] [PubMed] [Google Scholar]
- Lang FR, Weiss D, Gerstorf D, Wagner GG. Forecasting life satisfaction across adulthood: Benefits of seeing a dark future? Pscyhology and Aing. 2013;28(1):249–261. doi: 10.1037/a0030797. [DOI] [PubMed] [Google Scholar]
- Lucas RE, Diener E, Suh E. Discriminant validity of well-being measures. Journal of Personality and Social Psychology. 1996;71(3):616–628. doi: 10.1037/0022-3514.71.3.616. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health characteristics of adults aged 55 years and over: United States, 2004–2007. National Health Statistics Reports. 2009;16:1–32. [PubMed] [Google Scholar]
- Martin KA, Rejeski WJ, Miller ME, James MK, Ettinger WH, Messier SP. Validation of the PASE in older adults with knee pain and physical disability. Medicine and Science in Sports and Exercise. 1999;31(5):627–633. doi: 10.1097/00005768-199905000-00001. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Raikkonen K, Sutton-Tyrrell K, Kuller LH. Optimistic attitudes protect against progression of carotid atherosclerosis in healthy middle-aged women. Psychosomatic Medicine. 2004;66(5):640–644. doi: 10.1097/01.psy.0000139999.99756.a5. [DOI] [PubMed] [Google Scholar]
- McAuley E, Blissmer B, Katula J, Duncan TE. Exercise environment, self-efficacy, and affective responses to acute exercise in older adults. Psychology & Health. 2000;15(3):341–355. doi: 10.1080/08870440008401997. [DOI] [Google Scholar]
- McAuley E, Doerksen SE, Morris KS, Motl RW, Hu L, Wojcicki TR, … Rosengren KR. Pathways from physical activity to quality of life in older women. Annals of Behavioral Medicine. 2008;36(1):13–20. doi: 10.1007/s12160-008-9036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley E, Elavsky S, Motl RW, Konopack JF, Hu L, Marquez DX. Physical activity, self-efficacy, and self-esteem: Longitudinal relationships in older adults. Journals of Gerontology Series B-Psychological Sciences and Social Sciences. 2005;60(5):P268–P275. doi: 10.1093/geronb/60.5.p268. [DOI] [PubMed] [Google Scholar]
- McAuley E, Mailey EL, Mullen SP, Szabo AN, Wojcicki TR, White SM, … Kramer AF. Growth Trajectories of Exercise Self-Efficacy in Older Adults: Influence of Measures and Initial Status. Health Psychology. 2011;30(1):75–83. doi: 10.1037/00021567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motl RW, McAuley E. Physical Activity, Disability, and Quality of Life in Older Adults. [Article] Physical Medicine and Rehabilitation Clinics of North America. 2010;21(2):299. doi: 10.1016/j.pmr.2009.12.006. [DOI] [PubMed] [Google Scholar]
- Muthen L, Muthen B. Mplus (Version 6.0) Los Angeles, CA: 2010. [Google Scholar]
- Pavot W, Diener E. Review of the Satisfaction With Life Scale. In: Diener E, editor. Assessing Well-Being: The Collected Works of Ed Diener. Vol. 39. 2009. pp. 101–117. [Google Scholar]
- Pfeiffer E. Short portable mental status questionnaire for assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Rafferty A. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. [Google Scholar]
- Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. Journals of Gerontology: Series A. 2001;56A(Special Issue 11):23–35. doi: 10.1093/gerona/56.suppl_2.23. [DOI] [PubMed] [Google Scholar]
- Reker GT. Personal meaning, optimism, and choice: Existential predictors of depression in community and institutional elderly. The Gerontologist. 1997;37(6):709–716. doi: 10.1093/geront/37.6.709. [DOI] [PubMed] [Google Scholar]
- Riskind JH, Sarampote CS, Mercier MA. For every malady a sovereign cure: optimism training. Journal of Cognitive Psychotherapy. 1996;10(2):105–117. [Google Scholar]
- Scheier MF, Carver CS. Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychology. 1985;4(3):219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the life orientation test. Journal of Personality and Social Psychology. 1994;67(6):1063–1078. doi: 10.1037/0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Segerstrom SC. Optimism and resources: Effects on each other and on health over 10 years. Journal of Research in Personality. 2007;41(4):772–786. doi: 10.1016/j.jrp.2006.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg Nes L, Segerstrom SC. Dipositional optimism and coping: A meta-analytic review. Personality and Social Psychology Review. 2006;10:235–251. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: Associations with healthy ageing. British Journal of Health Psychology. 2006;11:71–84. doi: 10.1348/135910705x42850. [DOI] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. The disablement process. Social Science & Medicine. 1994;38(1):1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): Development and evaluation. Journal of Clinical Epidemiology. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- Woods nF, LaCroix AZ, Gray SL, Aragaki A, Cochrane BB, Brunner RL, et al. Frailty: Emergence and consequences in women aged 65 and older in the women’s health initiative observational study. Journal of the American Geriatric Society. 2005;53:1321–1330. doi: 10.1111/j.1532-5415.2005.53405.x. [DOI] [PubMed] [Google Scholar]