Abstract
Study Design
Prospective Cohort
Background
The high risk of second ACL injuries after return-to-sport highlights the importance of return-to-sport decision-making. Objective return-to-sport criteria frequently use LSI’s to quantify quadriceps strength and hop scores. Whether using the uninvolved limb in LSI’s is optimal is unknown.
Objectives
To evaluate the uninvolved limb as a reference standard for limb symmetry indexes (LSI’s) utilized in return-to-sport testing and its relationship with second ACL injury rates.
Methods
Seventy athletes completed quadriceps strength and 4 single-legged hop tests before ACL reconstruction (ACLR) and 6 months after ACLR. LSI’s for each test compared involved limb measures at 6 months to uninvolved measures at 6 months. Estimated pre-injury capacity (EPIC) levels for each test compared involved measures at 6 months to uninvolved measures before ACLR. Second ACL injuries were tracked for a minimum 2-year follow-up after ACLR.
Results
Forty (57.1%) patients achieved 90% LSI’s for quadriceps strength and all hop tests. Only 20 (28.6%) patients met 90% EPIC levels (comparing involved limb at 6 months after ACLR to uninvolved limb before ACLR) for quadriceps strength and all hop tests. Twenty-four (34.4%) patients who achieved 90% LSI’s for all measures 6 months after ACLR did not achieve 90% EPIC levels for all measures. EPIC levels were more sensitive to LSI’s in predicting second ACL injuries (LSI’s: 0.273 (95% CI: 0.010–0.566); EPIC: 0.818 (95% CI: 0.523–0.949)).
Conclusion
LSI’s frequently overestimate knee function after ACLR and may be related to second ACL injury risk. These findings raise concern whether the variable ACL return-to-sport criteria utilized in current clinical practice are stringent enough to achieve safe and successful return-to-sport.
Level of Evidence
Therapy, level 2b.
Keywords: ACL, anterior cruciate ligament, rehabilitation, return-to-sport, symmetry
INTRODUCTION
Anterior cruciate ligament (ACL) injury frequently results in muscle weakness, poor knee function, and increased risk for second injury despite surgical reconstruction (ACLR).2,8,15,17–20 Overall second ACL injury rates reaching upwards of 49%3 suggest inadequacy in current criteria used to determine an athlete’s readiness to return-to-sport. Adherence to objective return-to-sport criteria reduces re-injury risk,8 but criteria used to clear patients for return-to-sport is not standardized and varies considerably.3 Evidence to establish optimal objective levels of knee function that maximize functional outcomes and protect against second ACL injury is needed.
Objective return-to-sport criteria often utilize measures of quadriceps strength and single-legged hop tests, with limb to limb differences typically expressed as limb symmetry indexes (LSI’s).3 LSI’s use concurrent measures of the uninvolved limb as a reference standard. While the uninvolved limb is widely used as a “healthy” control, bilateral muscle strength deficits have been demonstrated after ACL injury11,16,20 challenging the validity of symmetry measures in objective return-to-sport criteria. It is unknown if measurements of the uninvolved limb prior to ACLR provide a better reference than LSI’s during return-to-sport testing. Therefore, the purpose of this study was to evaluate the uninvolved limb as a reference standard for symmetry indexes utilized in return-to-sport testing and its relationship with second ACL injury rates. Preliminary evidence is presented to demonstrate potential benefits of using uninvolved limb function prior to instead of after ACLR to determine return-to-sport readiness. We hypothesized that the involved limb function of athletes after ACLR would more frequently match uninvolved limb function measured concurrently after ACLR compared to uninvolved limb function measured before ACLR, and that EPIC levels would better predict second ACL injuries than LSI’s.
METHODS
Athletes active in cutting and pivoting activities4 before complete, unilateral ACL injury between the ages of 14–55 were secondarily analyzed within a completed randomized control trial and an ongoing prospective clinical trial.6,9 Exclusion criteria included a repairable meniscus, symptomatic grade III injury to other knee ligaments, >1 cm2 full-thickness articular cartilage lesion, or prior ACL injury. This study was approved by the University of Delaware Human Subjects Review Board and all patients provided written informed consent.
Patients completed 2 testing sessions before ACLR ((Testing 1) quadriceps strength testing initially after ACL injury; (Testing 2) single-legged hop testing following initial impairment resolution after ACL injury) and 1 testing session after ACLR (Testing 3: quadriceps strength testing and single-legged hop testing 6 months after ACLR) (FIGURE 1). Quadriceps strength was tested bilaterally in 90 degrees of knee flexion by recording maximal voluntary isometric contractions using the burst superimposition technique to ensure normal quadriceps activation12 during the initial physical therapy evaluation acutely after ACL injury. Patients continued rehabilitation prior to ACLR until initial impairments were resolved (effusion, range of motion, pain, gait impairments, quadriceps strength)12 and hop testing could be safely completed (second testing session). Four single-legged hop tests (single, crossover, triple hop for distance; 6-meter timed) were completed on each limb (uninvolved first).15 After 2 practice trials, the average of 2 trials was recorded in each limb for each hop test.
FIGURE 1.
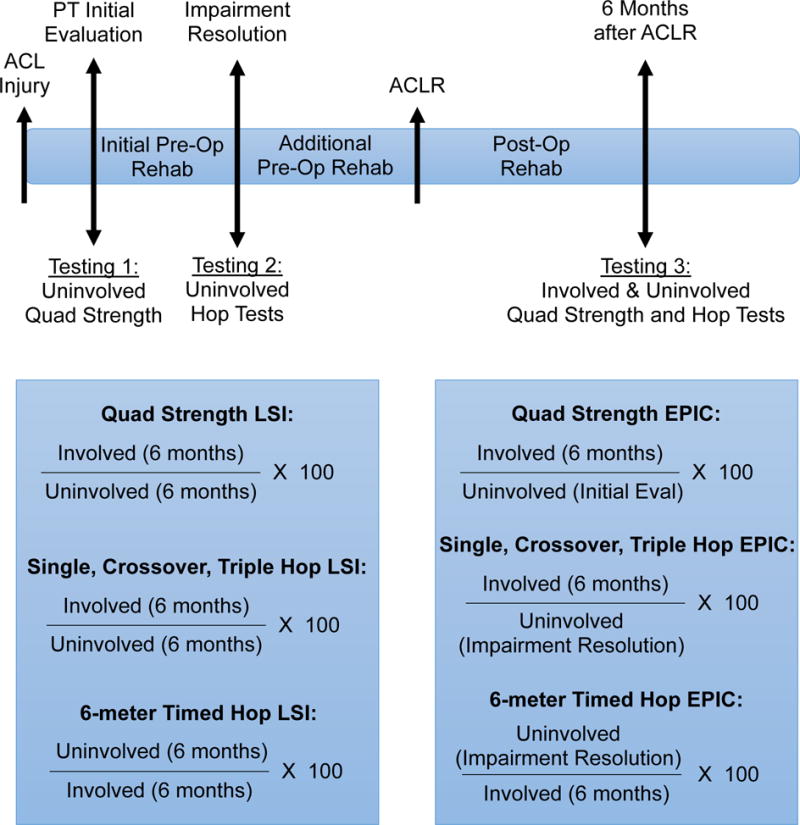
Timeline for testing and rehabilitation after ALC injury and equations used for calculation of LSI’s (limb symmetry indexes) and EPIC levels (estimated pre-injury capacity). Abbreviations: PT, physical therapy; ACLR, anterior cruciate ligament reconstruction; Pre-Op, pre-operative; Post-Op, post-operative; rehab, rehabilitation.
Patients underwent progressive, criterion-based post-operative rehabilitation early after ACLR1 and then repeated quadriceps strength and single-legged hop testing 6 months after ACLR (Testing 3) with LSI’s calculated (see FIGURE 1). Six-month testing was chosen because it is a common time to begin sporting activities.3 Symmetry was defined using a cut-off of 90% in accordance with established University of Delaware return-to-sport criteria requiring 90% or greater LSI’s in quadriceps strength and all 4 single-legged hop tests within a larger test battery.1 Return-to-sport criteria for included subjects also required at least 90% on the Knee Outcome Survey Activities of Daily Living Scale, and Global Rating Score of Knee Function prior to physician clearance for returning-to-sport.1 An LSI of 85–90% or greater is common in other published return-to-sport criteria18,19 and thought to account for normal levels of interlimb asymmetry.13,21
In addition to computing LSI’s 6 months after ACLR, estimated pre-injury capacity (EPIC) levels were calculated by comparing the involved limb function at 6 months to uninvolved scores prior to ACLR (FIGURE 1). A 90% cut-off was operationally defined as achieving EPIC levels for quadriceps strength and hop scores.
At subsequent follow-up testing patients reported if they had incurred second ACL injuries during a minimum 2-year follow-up. All second injuries were confirmed by a licensed physician or physical therapist.
Statistical analyses were completed using PASSW 23.0 software (SPSS Inc., Chicago, IL). Correlational analyses were used to test if time from ACL injury to initial uninvolved testing (before ACLR) influenced EPIC levels. Sensitivity, specificity, and positive and negative likelihood ratios with 95% confidence intervals (CI) were calculated to assess the ability of LSI’s and EPIC levels to determine second ACL injury risk.10 Statistical significance was set at α≤0.05.
RESULTS
The initial cohort eligible for this study included 182 patients. Thirty-seven subjects completed non-operative management of ACL injury, 9 did not complete hop testing prior to ACLR, 6 did not complete hop testing 6 months after ACLR, 28 did not return for testing 6 months after ACLR, and 32 were excluded to avoid unreliable EPIC measurements due the use of different electromechanical dynamometers for quadriceps strength testing at each testing session. Thus, 70 patients (26.6±10.0 years; 32.9% women; BMI 24.9±3.8 kg/m2) were used in the current analysis.
Patients completed initial uninvolved quadriceps strength testing 1.5±2.0 months and single-legged hop tests 1.9±2.1 months after ACL injury. ACLR occurred 4.4±4.0 months after injury (28 hamstring gracilis autograft, 42 soft tissue allograft). The time from ACL injury to initial uninvolved testing did not impact strength or hop EPIC levels (p: 0.400–0.892, Pearson r: -0.108–0.037).
Forty (57.1%) patients achieved 90% LSI’s for quadriceps strength and all single-legged hop tests. Only 20 (28.6%) patients met 90% EPIC levels (comparing involved limb at 6 months after ACLR to uninvolved limb before ACLR) for quadriceps strength and all hop tests. Twenty-four (34.4%) patients who achieved 90% LSI’s for all measures 6 months after ACLR did not achieve 90% EPIC levels for all measures. TABLE 1 provides details for why 90% LSI’s and EPIC levels were not achieved. When LSI’s and EPIC levels were not achieved, mean quadriceps strength and hops scores ranged from 5.1%-14.6% below 90% cut-off values (TABLE 2).
TABLE 1.
Number of patients who did not meet 90% LSI and 90% EPIC levels due to quadriceps strength alone, combination of quadriceps strength and single-legged hop tests, or only single-legged hop tests. Abbreviations: LSI’s, limb symmetry indexes; EPIC, estimated pre-injury capacity; quad, quadriceps.
| Did Not Meet 90% LSI’s Due To: | n: | Did Not Meet 90% EPIC Levels Due To: | n: |
|---|---|---|---|
| Quad Strength | 9 | Quad Strength | 12 |
| Quad Strength + 1 Hop | 4 | Quad Strength + 1 Hop | 4 |
| Quad Strength + 2 Hops | 1 | Quad Strength + 2 Hops | 7 |
| Quad Strength + 3 Hops | 1 | Quad Strength + 3 Hops | 0 |
| Quad Strength + 4 Hops | 1 | Quad Strength + 4 Hops | 3 |
| 1 Hop | 4 | 1 Hop | 14 |
| 2 Hops | 5 | 2 Hops | 8 |
| 3 Hops | 1 | 3 Hops | 2 |
| 4 Hops | 4 | 4 Hops | 0 |
TABLE 2.
Mean quadriceps strength and single-legged hop values when LSI’s or EPIC levels were less than 90% for each measure, respectively. Abbreviations: LSI’s, limb symmetry indexes; EPIC, estimated pre-injury capacity; SD, standard deviation; quad, quadriceps.
| Did Not Meet 90% LSI’s Due To: | n: | Mean (SD) (%) | Did Not Meet 90% EPIC Levels Due To: | n: | Mean (SD) (%) |
|---|---|---|---|---|---|
| Quad Strength | 16 | 83.6 (3.2) | Quad Strength | 26 | 78.8 (8.3) |
| Single Hop | 18 | 81.1 (6.2) | Single Hop | 18 | 75.4 (17.6) |
| Crossover Hop | 12 | 83.6 (4.3) | Crossover Hop | 18 | 83.3 (5.4) |
| Triple Hop | 8 | 84.9 (3.3) | Triple Hop | 12 | 81.7 (5.9) |
| 6-meter Timed Hop | 9 | 83.5 (4.5) | 6-meter Timed Hop | 18 | 80.8 (6.5) |
Eleven patients sustained a second ACL injury (ACLR to second injury: median: 78 wks; range: 27–276 wks) (TABLE 3). Eight (4 ipsilateral, 4 contralateral) of the 11 patients with a second ACL injury passed 90% LSI return-to-sport criteria in quadriceps strength and single-legged hop tests 6 months after initial ACLR, but 6 (4 ipsilateral, 2 contralateral) of these 8 did not achieve 90% EPIC levels in these measures. Achieving 90% EPIC levels was superior to 90% LSI’s in predicting second ACL injuries (LSI’s: sensitivity: 0.273 (95% CI: 0.010–0.566), specificity: 0.542 (95% CI: 0.417–0.663), positive likelihood ratio: 0.596 (95% CI: .218–1.627), negative likelihood ratio: 1.341 (95% CI: 0.871–2.064); EPIC: sensitivity: 0.818 (95% CI: 0.523–0.949), specificity: 0.305 (95% CI: 0.203–0.432), positive likelihood ratio: 1.177 (95% CI: 0.850–1.631), negative likelihood ratio: 0.596 (95% CI: 0.161–2.212)).
TABLE 3.
Patients with second ACL injuries including whether quadriceps strength and all four single-legged hop test LSI’s and EPIC values were at least 90%, respectively. Abbreviations: LSI’s, limb symmetry indexes; EPIC, estimated pre-injury capacity.
| Patient | ACLR to 2nd ACL Injury (wks) | LSI’s ≥ 90% | EPIC ≥ 90% | Side of Injury |
|---|---|---|---|---|
| 1 | 70 | Yes | Yes | Contralateral |
| 2 | 28 | Yes | Yes | Contralateral |
| 3 | 250 | Yes | No | Ipsilateral |
| 4 | 78 | Yes | No | Ipsilateral |
| 5 | 252 | Yes | No | Contralateral |
| 6 | 27 | Yes | No | Ipsilateral |
| 7 | 60 | Yes | No | Ipsilateral |
| 8 | 114 | Yes | No | Contralateral |
| 9 | 108 | No | No | Ipsilateral |
| 10 | 62 | No | No | Ipsilateral |
| 11 | 276 | No | No | Ipsilateral |
DISCUSSION
The purpose of this study was to evaluate the uninvolved limb as a reference standard for symmetry indexes utilized in return-to-sport testing and its relationship with second ACL injury rates. The results of this study demonstrate that achievement of limb symmetry in quadriceps strength and single-legged hop tests after ACLR does not guarantee prior functional levels (per the uninvolved limb before ACLR) have been met. Forty of 70 patients met University of Delaware return-to-sport criteria of at least 90% symmetry in quadriceps strength and 4 single-legged hop tests 6 months after ACLR, but only 16 of these 40 patients achieved 90% EPIC levels when comparing the involved limb at 6 months to uninvolved limb function prior to ACLR. Preliminary data suggests that the use of 90% EPIC levels is superior to 90% LSI’s in predicting second ACL injuries.
The lower number of patients who met 90% EPIC levels compared to 90% LSI’s may be explained by current criterion-based pre-operative and post-operative rehabilitation that focuses on unilateral strengthening and neuromuscular training.1 The uninvolved limb likely experiences limited physical activity beyond walking and activities of daily living during the extended period between injury and return-to-sport, a drastic decline from demands faced during pre-injury levels of sports activities. Reduced physical activity levels may result in compensatory adaptations by a subgroup of patients with ACL injury including decreased muscle strength in the uninvolved leg after ACL injury.11,16,20 Decreased function and performance of the uninvolved limb over time will produce inflated limb symmetry indexes and may misrepresent the functional ability of the ACL-injured limb.
Eight of 11 patients who suffered a second ACL injury passed 90% LSI return-to-sport criteria for quadriceps strength and single-legged hop tests 6 months after ACLR. However, 6 of the 8 (4 ipsilateral, 2 contralateral) who met return-to-sport criteria did not meet 90% EPIC levels in all measures. It is possible that athletes who attained 90% LSI’s but not 90% EPIC levels 6 months after ACLR had remaining bilateral functional deficits that were unresolved after return-to-sport activities were resumed. Persistent bilateral functional impairments could be a factor in the incidence of both ipsilateral and contralateral second ACL injuries in our cohort, and the significantly increased risk of both ipsilateral and contralateral second ACL injuries which has previously been reported early after athletes return-to-sport.17 The small sample of patients in our study with second ACL injury likely resulted in the large sensitivity and specificity confidence intervals present. Further study is needed with a larger cohort of patients with second ACL injury to validate the current preliminary findings.
Few studies have examined alternate measurements to LSI’s to compare the function and performance of the involved limb after ACLR. Prospective pre-season functional testing of athletes is the ideal criterion to provide patient-specific rehabilitation milestones after injury. Pre-injury functional data would eliminate the limitation of EPIC measurements which requires pre-operative testing of the uninvolved limb. However, pre-injury testing requires extensive resources and time commitments making widespread implementation in high school, college, and recreational settings unrealistic. The benefit of including pre-operative rehabilitation on post-operative outcomes after ACL injury is clear,7 and this period presents an opportunity for objective measurement of baseline uninvolved limb function to later compare the involved limb during return-to-sport testing. Age, sex, and sports matched normative values present an alternative strategy to patient-specific pre-injury data and EPIC measurements but are not widely developed.5,14
The high number of patients who passed return-to-sport criteria but failed to meet levels of knee function in the uninvolved limb present prior to ACLR raises concerns regarding current return-to-sport practice guidelines. Despite evidence that stringent objective return-to-sport criteria minimizes the risk of additional knee injury,8 the requirement for only 80–85% symmetry or absence of any objective criteria is frequent.3 The cut-off of 90% symmetry within this study as part of the University of Delaware return-to-sport criteria represents one of the most demanding criteria published and currently used in ACL return-to-sport testing.1,3 However, even when meeting these strict criteria, symmetry measures underestimated the baseline functional performance of many patients.
The current findings provide grounds for discussion regarding the validity of limb symmetry and current return-to-sport criteria utilized after ACL injury. The nature of the current analysis limits our ability to develop strong conclusions whether utilizing EPIC measurements is superior to LSI’s in decreasing risk of second ACL injuries because EPIC levels were not computed during 6-month functional testing. Thus, further bilateral strengthening and neuromuscular training to achieve 90% EPIC levels were not implemented. Other limitations include a small sample size, the low occurrence of second ACL injuries, and cohort attrition (including patients tested on different dynamometers). However, the current study does highlight the need for rigorous testing of objective return-to-sport criteria to establish best practice for safe clearance to sport and improve rates of second ACL injury. Determination of the most valid and reasonable reference on which to compare the function of the involved limb must be included.
CONCLUSION
Even with the use of rigorous return-to-sport criteria, recovery of knee function is frequently overestimated when using measures of limb symmetry. Preliminary evidence suggests the inability to restore knee function exhibited prior to ACLR may increase risk for second ACL injuries. The current findings raise concern whether the variable return-to-sport criteria utilized in current clinical practice after ACL injury are stringent enough to achieve a safe and successful return-to-sport.
KEY POINTS.
Findings
Achievement of limb symmetry in quadriceps strength and single-legged hop tests after ACLR does not guarantee prior functional levels (per the uninvolved limb) have been met. Preliminary data suggests that the use of 90% EPIC levels is superior to 90% LSI’s in predicting second ACL injuries.
Implications
The current findings raise concern whether the variable return-to-sport criteria utilized in current clinical practice after ACL injury are stringent enough to achieve a safe and successful return-to-sport.
Caution
EPIC levels were not computed at the time of 6 month functional testing; thus, is not known whether further rehabilitation to attain 90% EPIC levels would have resulted in improved outcomes.
Acknowledgments
We would like to thank David Logerstedt, PT, MPT, PhD, MA, SCS, Andrew Lynch, PT, DPT, PhD, and the University of Delaware Physical Therapy Clinic for providing the physical therapy treatments and assisting with data collection for our research participants. We also thank Martha Callahan and the Delaware Rehabilitation Institute’s Clinical Research Core (http://www.udel.edu/dri/ResCore.html) for their assistance with patient recruitment, scheduling, and data management.
Statement of the sources of grant support: Funding for this study was provided by the NIH (R37 HD037986, R01 AR048212, P30 GM103333).
Footnotes
Statement of Institutional Review Board approval of the study protocol: This study was approved by the University of Delaware Institutional Review Board.
Statement of financial disclosures and conflict of interest:
I affirm that I have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript.
Name of the public trials registry and the registration number: N/A (clinical trial initiated prior to 1/1/2013)
References
- 1.Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current Concepts for Anterior Cruciate Ligament Reconstruction: A Criterion-Based Rehabilitation Progression. J Orthop Sports Phys Ther. 2012 doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sport Med. 2014;48(21):1543–52. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 3.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sport Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 5.DeCarlo M, Sell K. Normative data for range of motion and single‐leg hop in high school athletes. J Sport Rehabil. 1997;6:246–255. [Google Scholar]
- 6.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A Progressive 5-Week Exercise Therapy Program Leads to Significant Improvement in Knee Function Early After Anterior Cruciate Ligament Injury. J Orthop Sport Phys Ther. 2010;40(11):705–721. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Failla MJ, Logerstedt DS, Grindem H, et al. Does Extended Preoperative Rehabilitation Influence Outcomes 2 Years After ACL Reconstruction?: A Comparative Effectiveness Study Between the MOON and Delaware-Oslo ACL Cohorts. Am J Sports Med. 2016 doi: 10.1177/0363546516652594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016 doi: 10.1136/bjsports-2016-096031. Epud ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res. 2009;27(6):724–729. doi: 10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herbert R. Confidence Interval Calculator. 2013 Available at: http://www.pedro.org.au/english/downloads/confidence-interval-calculator Accessed November 30, 2016.
- 11.Hiemstra LA, Webber S, MacDonald PB, Kriellaars DJ. Contralateral limb strength deficits after anterior cruciate ligament reconstruction using a hamstring tendon graft. 2007 doi: 10.1016/j.clinbiomech.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: Part 1, outcomes. Am J Sport Med. 2008;36(1):40–47. doi: 10.1177/0363546507308190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Myer GD, Schmitt LC, Brent JL, et al. Utilization of Modified NFL Combine Testing to Identify Functional Deficits in Athletes Following ACL Reconstruction. J Orthop Sport Phys Ther. 2011;41(6):377–387. doi: 10.2519/jospt.2011.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myers BA, Jenkins WL, Killian C, Rundquist P. Normative data for hop tests in high school and collegiate basketball and soccer players. Int J Sport Phys Ther. 2014;9(5):596–603. [PMC free article] [PubMed] [Google Scholar]
- 15.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sport Med. 1991;19(5):513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 16.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sport Med. 2008;27(3):405–24. vii–ix. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 17.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42(7):1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–9. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomee R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sport Traumatol Arthrosc. 2011;19(11):1798–1805. doi: 10.1007/s00167-011-1669-8. [DOI] [PubMed] [Google Scholar]
- 20.Urbach D, Nebelung W, Becker R, Awiszus F. Effects of reconstruction of the anterior cruciate ligament on voluntary activation of quadriceps femoris. J Bone Jt Surg. 2001;83:1104–1110. doi: 10.1302/0301-620x.83b8.11618. [DOI] [PubMed] [Google Scholar]
- 21.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sport Phys Ther. 1994;20(2):60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]


