Abstract
Objective
Adult attachment discourse patterns and current family relationship quality were examined as predictors of health behaviors and number of Metabolic Syndrome (MetS) criteria met.
Methods
A sample of 215 White/European American and Black/African American adults, aged 35 to 55, were examined cross-sectionally. Discourse was assessed with the Adult Attachment Interview (AAI), specifically: 1) coherence, a marker of attachment security, 2) unresolved trauma/loss, a marker of disorganized and distorted cognition related to trauma, and 3) idealization, the tendency to minimize the impact of stressful experiences. Health behaviors of diet, exercise, smoking and alcohol use were also assessed, as were adverse childhood experiences, current depressive symptoms and relationship functioning. MetS includes hypertension, hyperglycemia, high triglycerides, low HDL cholesterol, and obesity.
Results
Using path analysis and accounting for childhood adversity and depressive symptoms, AAI coherence and unresolved trauma or loss were directly linked to number of MetS criteria met (β = −.22 and .21 respectively). Idealization was indirectly linked to MetS through poor diet (β = −.26 and −.36 respectively), predicting 21% of the variance in number of MetS criteria met.
Conclusions
Attachment representations related to stress appraisal and care-seeking behaviors appear to serve as cognitive mechanisms increasing risk of MetS.
Keywords: adult attachment, metabolic syndrome, adverse childhood experiences
The attachment system is hypothesized to be the primary system of safety and stress management across the life span (Ainsworth, 1985, 1991; Bowlby, 1969/1982; Bretherton, 1985; Waters, Kondo-Ikemura, Posada, & Richters, 1991; Weiss, 1982). Development of the attachment system includes learning to identify danger and distress and employing attachment relationship-oriented behaviors to manage stress and restore physiological and psychological homeostasis. The benefits of infant attachment with respect to safety, security, and socialization have been extensively explored (Cassidy & Shaver, 2008). In contrast, life span benefits of the attachment system have been much less frequently studied (Coan, 2008; Magai, 2008). Nevertheless, it has been hypothesized that as a system of safety and homeostasis, the attachment system in adults should significantly impact on health behaviors and outcomes (Ciechanowski, Sullivan, Jensen, Romano, & Summers, 2003; Feeney & Ryan, 1994; Fricchione, 2011; Glanz & Schwartz, 2008; Maunder & Hunter, 2009).
Development of the attachment system
Attachment or secure base behaviors, emerging in infancy and manifested across the life span, include maintaining awareness of attachment figures’ availability, and seeking proximity, protection, reassurance, and comfort from attachment figures in times of stress. Optimally, proximity to and responsiveness of attachment figures lead to restoration of both physiological and psychological equilibrium and a return to a pre-stress level of functioning (Ainsworth, 1991; Marvin, Cooper, Hoffman, & Powell, 2002). In low stress times, secure base behaviors are characterized by use of the attachment figure’s encouragement and support to explore and master the environment (Bretherton, 1985; Hostinar, Sullivan, & Gunnar, 2013). On a daily, even moment-to-moment, basis, the caregiver actively teaches the child and reinforces the set point for what is safe and what is unsafe (Waters et al., 1991). Whereas the emergence of the attachment system in infancy is biologically based and essentially universal in humans, the quality or expression of attachment behavior depends on the quality of caregiver secure base support (Ainsworth, Blehar, Waters, & Wall, 1978; Bowlby, 1969/1982; Posada et al., 1995).
Attachment representations are cognitions that develop in the context of attachment relationships from day-to-day interactions with those key people in life who provide secure base support, usually parents/caregivers, and in later life, adult partners (Ainsworth, 1991; Bowlby, 1969/1982; Waters et al., 1991). In infancy, the quality of the representation corresponds to the quality of the attachment relationship and the behavioral interactions within that relationship (Ainsworth et al., 1978; Main, Kaplan, & Cassidy, 1985). With development, the representations generalize and can be understood as scripts or ‘road maps’ that operate outside of conscious awareness. They guide attention and assessment in novel and stressful situations and inform behavioral responses aimed at restoration of safety and equilibrium, especially the use of attachment figures (Bowlby, 1969/1982; Bretherton & Munholland, 2008; Dykas, Woodhouse, Cassidy, & Waters, 2006; Main et al., 1985; Waters & Waters, 2006; Waters, Brockmeyer, & Crowell, 2013). Table 1 shows the hypothesized and observed correspondence between early attachment patterns and adult attachment discourse, behavior, and cognitions (Crowell et al., 2002; Main et al., 1985; Raby, Cicchetti, Carlson, Egeland, & Collins, 2013; Waters, Hamilton, & Weinfield, 2000).
Table 1.
| Adult Attachment | Attachment in infancy | Discourse characteristics | Cognitions and behaviors in adulthood |
|---|---|---|---|
| Secure-autonomous Classification | Secure: Caregiving characterized by availability, sensitivity, cooperativeness, responsiveness. Child actively seeks caregiver(s) for help when in danger or distress; comforted by contact, allowing for return to exploration - equilibrium restored. | Clear, coherent, cooperative, and organized discourse; the speaker makes logical connections between past experience and present functioning even if attachment experiences in childhood were sub-optimal | Flexible, adaptive; attachment figures are important & useful, or should be; approach for help is direct -- expectation that others will be supportive and helpful; nevertheless flexible and adaptive to the situation; support is accepted and is reassuring; equilibrium restored |
| Insecure Classifications | Caregiving is non-optimal but “ordinary”/non-traumatic; patterns are observed in normative samples | Incoherent: lacks believability, lacks sufficient information, is irrelevant, and/or is indirect, ‘jargony’, stereotypic | Behavioral strategy is not flexible or adaptive to varying situations |
| Insecure-Dismissing Classification | Anxious Avoidant: Caregiving is “rejecting”; i.e., child is pushed to be prematurely independent and self-soothing when stressed. Child avoids caregiver when distressed, turns away; appears calm, but arousal is high | Negative events and attachment experiences are minimized and set aside-either “forgotten” or viewed as irrelevant; attachment figures are idealized, and being ‘normal’ or ‘typical’ is emphasized | Problems not acknowledged, e.g., “it’s not big deal”; others are not approached for help, especially not emotional support or problems that are considered “trivial” or “personal”; although there may be good general social skills and enjoyment of others |
| Insecure-Preoccupied Classification | Anxious-ambivalent/resistant: Caregiving is erratic and non-contingent, either intrusive or disengaged. Child’s approach and contact when distressed is mixed with anger and resistance; OR minimal approach with passive, fussy, and helpless behavior; not easily soothed | Preoccupation with attachment figures, confused and oscillating perspectives, use of jargon and stereotypic phrasing; there may be hot, active anger in discussion of attachment experiences or passive, confused utterances | Active approach when distressed, but not easily reassured, rather increasing anxiety and uncertainty about others’ availability and ability to help. Passive form is associated with low approach, helplessness and confusion when stressed. |
| Unresolved Status | Experience of important loss and/or of abuse; May occur in any caregiving context, although more likely in an insecure environment | While discussing the event, disorganized and unusual wording and/or un-integrated thoughts and beliefs about causation, timing, and the reality of the traumatic experience | Variable, depends on major classification: Unresolved/Secure less affected; Unresolved/Preoccupied most common, may include dissociation, fearfulness |
Drawing upon these hypotheses, the functioning of the adult attachment system and its hypothesized influence on health should depend upon 1) how well one knows what to do in stressful situations (the quality of the attachment script as it develops over time), and 2) the quality of one’s present relationship circumstances or current attachment context, i.e., the support system.
Adult attachment and health
It has been hypothesized that adult attachment representations have implications for health behaviors and health outcomes (Ciechanowski et al., 2003; Feeney & Ryan, 1994; G Fricchione, 2011; Glanz & Schwartz, 2008; Maunder & Hunter, 2009). The most adaptive (secure) representation should theoretically enhance the ability to evaluate stress accurately and lead to flexible, adaptive, and effective care seeking in general and with respect to health. Thus a secure attachment system leads to adaptive use of resources, more rapid resolution of arousal associated with stress, and consequently, lower allostatic load (McEwen & Getz, 2013). Insecure adult attachment representations (dismissing/avoidant and preoccupied/anxious) are hypothesized to lead to less accurate assessments and less flexible and adaptive coping strategies, as well as more prolonged arousal under stressful conditions (Ciechanowski et al., 2003; Crowell et al., 2002; Feeney & Ryan, 1994; Kidd & Sheffield, 2005; Maunder & Hunter, 2001; Maunder & Hunter, 2009). For example, a dismissing/avoidant attachment stance would be associated with poor identification of stressful experiences, including avoiding and/or dismissing cues and symptoms, over-rating or idealizing one’s own well-being, and/or avoiding the use of close others as supports when stressed. Adults and infants with this attachment pattern show apparent calm in the face of stress, but manifest concurrent high physiological arousal (Dozier & Kobak, 1992; Sroufe & Waters, 1977). In contrast, a preoccupied/anxious attachment stance is associated with heightened detection of and response to stress, and active, even “hyperactive” care seeking, but with decreased ‘soothability’ and sustained arousal (Ciechanowski et al., 2004; Crowell et al., 2002; Feeney & Ryan, 1994). Both of these insecure patterns would theoretically lead to greater allostatic load.
In addition to ordinary attachment experiences that lead to the ‘organized’ strategies, i.e., the secure, dismissing, or preoccupied patterns, attachment-relevant childhood trauma also impacts attachment representations and secure base behaviors (Creasey, 2002; Madigan, Moran, Schuengel, Pederson, & Otten, 2007; Main et al., 1985). In the Adult Attachment Interview, unusual discourse or un-integrated memories and beliefs about causation, timing, and reality of a loss or abuse experiences are markers of lack of resolution of the trauma (George, Kaplan, & Main, 1985; Madigan et al., 2007). With respect to health outcomes, fear and arousal could be high in situations that are not currently dangerous, thus increasing allostatic load and impacting health (McEwen, 1998; McEwen & Getz, 2013; Stovall-McCough & Cloitre, 2006). Furthermore, fear could negatively impact care-seeking behaviors (Ciechanowski et al., 2003; Creasey, 2002; Feeney & Ryan, 1994; Stovall-McCough & Cloitre, 2006).
Measurement
Most investigations linking attachment to health outcomes have used self-report attachment-style measures, which describe feelings and behavior in close relationships, (Ciechanowski et al., 2003; D’Argenio et al., 2009; Feeney & Ryan, 1994; Jaremka et al., 2013; McWilliams & Bailey, 2010). Anxiety and emotionality regarding close relationships, i.e., the self-reported anxious style, is associated with increased symptom reporting, and the avoidant style with poorer management of diabetes and headaches (Ciechanowski et al., 2004; D’Argenio et al., 2009; Feeney & Ryan, 1994; McWilliams & Bailey, 2010; Porter, Davis, & Keefe, 2007). One study has shown a developmental outcome: the anxious-resistant attachment pattern in infancy predicted reports of physical health problems 30 years later (Puig, Englund, Simpson, & Collins, 2012).
In contrast to self-reports, the Adult Attachment Interview (AAI) has not been used to examine health behaviors or health outcomes. Yet, the AAI is a measure that is both theoretically and empirically linked to attachment representations and a secure base script, in which discourse style is a marker for the quality of the representation/script (Dykas et al., 2006; George et al., 1985; Waters, Brockmeyer, & Crowell, 2013b). Patterns assessed with the AAI are not linked to specific experiences, but to the meaning attributed to experiences and the manner in which they are discussed. Therefore attachment security is reflected in overall coherence of discourse and is possible even in adverse circumstances (George et al., 1985). From a measurement perspective, AAI coherence (representational security) approximates the ‘road map concept’, that is, the ability to identify danger/stress and subsequently navigate a course of action with respect to engaging and utilizing resources, especially close relationships (Waters et al., 2013).
Furthermore, the AAI identifies particular incoherent/insecure discourse patterns that could be associated with health outcomes. Idealization is characterized by denial or discounting the importance of stress and negative experiences. Individuals who use idealization emphasize ‘normality’ and give socially desirable responses. The unresolved discourse pattern is triggered by discussion of the attachment-related adversities of loss and of abuse and is expressed in disorganized cognitions and memories. Childhood trauma and adversity themselves are clearly linked to health outcomes, and cognitive disorganization may play a role in this association (Bentley & Widom, 2009; Danese & McEwen, 2012; Davis et al., 2013a; Hostinar et al., 2013; Sullivan, 2012; Thomas, Hyponnen, & Power, 2008).
Adult attachment relationships and health
The attachment literature has not focused on the quality of current attachment relationships and adult health. However, there is an extensive literature linking social support with health behaviors and well-being; indeed “the link between social ties and health has become a veritable social fact” (Umberson, Crosnos, & Reczek, 2010), p. 139. Social relationships are ‘convoys’ that can promote healthy behavior and deter risky behavior (Cohen, 2004; Repetti, Taylor, & Seeman, 2002; Umberson et al., 2010). Stress buffering occurs through belief in availability of support which “eliminates or reduces effects of stressful experiences by promoting less threatening interpretations of adverse events and effective coping strategies” (Cohen, 2004), p. 677, and through decreased arousal (Umberson et al., 2010). These mechanisms are consistent with attachment theory’s perspectives on felt security and restoration of homeostasis associated with secure-base contact as well as with animal studies of maternal caregiving and physiological buffering (Bowlby, 1958,Bowlby, 1969/1982; Hostinar et al., 2013; Sullivan, 2012).
Close relationships also contribute to poor health, increasing risk via stress and through problematic health behaviors (Cohen, 2004; Eaker, Sullivan, Kelly-Hayes, D’Agostino, & Benjamin, 2007; Gable & Gosnell, 2013; Kiecolt-Glaser & Newton, 2001; Repetti et al., 2002; Umberson et al., 2010). Poor relationships with attachment figures, that is, parents and partners, are particularly salient stressors that impact on health-related behaviors and health outcomes, e.g., heart disease, wound healing {Ackard, 2006 #117) Dietary and exercise habits are especially linked to past and current family relationships, in contrast to alcohol use and smoking that are more influenced by peer relationships (Umberson et al., 2010). Family members may also either support or dismiss the need for medical care and adherence to recommendations (DiMatteo, 2004).
The current study
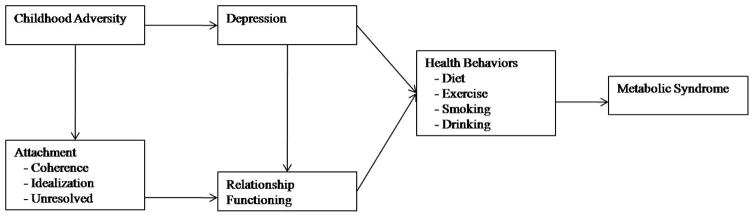
Using a sample of mixed-risk midlife adults who have not yet manifested serious illness, we hypothesized a path from attachment representations to current attachment relationship quality leading to 1) health behaviors of diet, smoking, exercise, and alcohol use, and 2) the metabolic syndrome (MetS) (see Figure 1).
Figure 1.
Hypothesized path model of the links between adult attachment representations and health
MetS is strongly predictive of subsequent ill health, especially adult-onset diabetes, hypertension, and cardiovascular disease (Grundy et al., 2005) and is associated with childhood adversity and toxic caregiving environments (Chichlowska et al., 2009; Davis et al., 2013b; Midei, Matthews, Chang, & Bromberger, 2012; Parker et al., 2003; Pervanidou & Chrousos, 2012). We used a sum of MetS components, i.e., obesity, high blood pressure, high serum triglycerides, low HDL cholesterol, and high fasting glucose, as an indicator of metabolic health risk.
AAI coherence of transcript was used as an indicator of the script, i.e., the ability to effectively assess stress and to guide coping/adaptive responses to alleviate the stress (Waters et al., 2013). Coherence predicts adult attachment behavior, that is, the ability to use and provide secure base support within a committed partnership (Creasey, 2002; Crowell et al., 2002; Simpson, Rholes, Orina, & Grich, 2002; Treboux, Crowell, & Waters, 2004). We therefore predicted that coherence is associated with the quality of current close family relationships. However, if coherence indeed is indicative of a script or ‘road map’ that has developed since early childhood to guide attention and behavior with respect to stressful experiences, then coherence should also predict health independent of current relationship quality. We also examined two forms of incoherence noted above: 1) unresolved status and 2) idealization, given the potential that they are markers for poor identification of stressors, sustained stress responses, and maladaptive care seeking.
Unresolved status reflects childhood trauma/adversity’s impact on memory and interpretation of stressors (Hostinar et al., 2013), thus increasing allostatic load over time, and hence, metabolic health (Danese & McEwen, 2012; McEwen & Getz, 2013; McEwen & Stellar, 1993).
Idealization has relevance to our model in two ways: First, it indicates a tendency to avoid or ignore stressful experiences. With respect to health, this stance would lead to sustained arousal, increased allostatic load, and possibly managing arousal in ways other than through attachment relationships, e.g., substance use or overeating (Danese & McEwen, 2012; Dozier & Kobak, 1992; Pervanidou & Chrousos, 2012). Secondarily, it can be considered a control variable with respect to social desirability in self-reports of relationship functioning.
Lastly, we include childhood adversity and depressive symptoms in our theoretical model as they are powerful family and stress-related variables that impact physical health and may help explain associations between attachment variables and health or represent an alternative path to poor health in midlife (Ciechanowski et al., 2003; Danese & McEwen, 2012; Davis et al., 2013b; DiMatteo, Lepper, & Croghan, 2000; Lin et al., 2004; Vythilingam et al., 2002).
Method
Sample
Participants were 215 White/European American and Black/African American adults (mean age = 45.9; ±3.3; range 35–55 years) of diverse socioeconomic background who were part of a study examining psychosocial influences on physical and mental health in midlife. The sample was generally representative of the population of Boston, MA with regard to proportion of men and women, White/European Americans, and those with a Bachelor’s degree or higher, but with a higher proportion of Black/African Americans (Census, 2012). The sample was 56% Black/African American and 52% were women. Recruitment aimed at balancing employment status and then educational level within groups divided by race and gender. Institutional Review Boards of participating institutions approved the study. Participants gave written informed consent.
Fifty-two participants of predominantly European American-descent (96.5%) were recruited from a 30+ year longitudinal study (Hauser, Powers, & Noam, 1991; Hauser et al., 1984) that originally assessed psychosocial functioning in adolescents (mean age = 14.6; range 13–18 years). An additional 163 participants of comparable age (between 40–50 years old) and current socioeconomic status were recruited over 20 months through advertising (radio, newspapers, health fairs) in the Boston area. Those with serious medical illnesses, e.g., heart disease, cancer, diabetes were excluded from the study. Of 963 individuals who inquired about participation, 247 did not return calls or come for their visit, 44 were not interested after learning more, 501 were ineligible or their inclusion would skew balance among groups with respect to employment and education, and 171 came for assessment. Eight potential participants were excluded during the physical health evaluation, because electrocardiogram findings indicated past myocardial infarction or fasting finger-stick blood glucose level indicated diabetes.
To ensure that the two samples were comparable, a dummy variable indicating the sample group and interactions between sample group and each predictor of interest were included as covariates in statistical models, first with the dummy only and second with the dummy and interactions. There were no significant differences in outcomes or patterns of outcomes associated with sample group. Moreover, the pattern of results remained evident with or without the sample group covariates. Therefore, the two samples were combined to enhance statistical power. The combined sample was 25% (n=53) White/European American men; 20% (n=42) White/European American women; 23% (n=50) Black/African American men; 32% (n=70) Black/African American women. Thirty-six percent of participants had a Bachelor’s degree or higher, 31% were unemployed, and 60% were in a committed relationship.
Procedure
Participants arrived at 8:00 AM at the Clinical Research Center of Beth Israel Deaconess Medical Center, (Boston, MA) after an overnight fast. Nurses conducted screening ECGs and measured seated blood pressure twice with a 5-minute interval, and once standing. A physician conducted a standardized medical history and completed a physical examination. The dietician obtained anthropometric measures. Blood was drawn and stored in −80. Participants then went to Judge Baker Children’s Center (Boston, MA) for psychosocial assessments.
Measures
Childhood adversity
Cumulative adversity (CDC, 2012) before age 18 was assessed using a) the Evaluation of Lifetime Stressors interview (Krinsley, 1996), b) the Structured Clinical Interview for Diagnoses Diagnostic and Statistical Manual (DSM) IV-R Non-Patient Version Axis 1 including the Post-Traumatic Stress Disorder module (First, Spitzer, & Williams, 2002), and c) the Adult Attachment Interview yielding narrative descriptions of childhood adversities (George et al., 1985).
Two coders reviewed each interview. An adversity was tallied if the participant presented an unambiguous description, regardless of the meaning attributed. The most prevalent adversities were parental divorce (42%), physical abuse (41%), prolonged separation from parent (34%), sexual abuse (30%), domestic violence (29%), emotional abuse (23%), parental substance abuse (21%), and death of a first-degree family member (20%). A cumulative adversity sum score was obtained (range 0–13).
Adversity severity was assessed using a modified version of DSM-III-R Axis IV scale for children and adolescents. Childhood was broken into 4 blocks (0–5 years, 6–10 years, 11–14 years, and 15–18 years). Adversities for each block were rated using a 5-point scale (0 = none, 1= mild, 2 =moderate, 3 =severe, 4 =extreme). For example, a time block that included abuse could be rated as moderate, severe, or extreme depending on such factors as who the perpetrator was, use of weapons, and other life contexts, e.g., racial discrimination. A summary score was generated from the mean of the four block ratings and rounded to the nearest half number (M = 1.88; ±1.37). Although the DSM Axis IV no longer uses this scale because agreement among clinicians was not optimal (Rey, Stewart, Plapp, Bashir, & Richards, 1988), agreement between two trained blind coders on 24% of the sample using the scale was good, r = .85.
Adversity chronicity was also assessed on a 4-point scale. As for severity, chronicity was rated for the 4 time blocks of childhood. A score of 0 was given for no adversity; 1 for single episodes or acute events, e.g., hospitalization for an acute illness or death of a grandparent, 2 = a chronic situation such as an alcoholic caregiver or poverty, and 3 = mixed, i.e., episodic stresses occurring in the context of chronic adversity. A summary score was generated from the four block ratings and rounded to the nearest whole number (M = 1.53; ± 1.15). Inter-rater agreement was very high, r = .96.
Cumulative adversity, severity of adversity, and chronicity of adversity were strongly correlated with each other (range r = .50 – .76). We multiplied the number of childhood adversities X severity X chronicity to create an overall adversity score (M=20.9; range 0 to 137). Because this variable was positively skewed, a log transformation was performed that improved normality of the distribution.
The Adult Attachment Interview (George et al., 1985)
The AAI was used to assess state of mind regarding attachment. The interview asks about attachment experiences with caregivers in childhood, including broad descriptions and specific memories to support general assessments. Validity, stability, and reliability of the AAI are well demonstrated (Hesse, 2009). Interviews were audiotaped, transcribed, and scored using the Main coding system (Main & Goldwyn, 1994).
Two trained, experienced coders blind to all other information regarding participants scored the interviews. They achieved 82% (κ = .73) agreement for 3 classifications (Secure, Dismissing, and Preoccupied) on 43 AAIs (29%). Five discourse scales, scored on a 1–9 point scale, were used: coherence of transcript, idealization of mother and of father, and unresolved for loss and for abuse. Coherence reflects the quality, quantity, relevance, and manner of responding to questions and is a proxy for security, agreement was Pearson r = .83. Idealization was scored for each parent (or other attachment figure) and the higher score was used in analyses; agreement for idealization score was r = .85. The Unresolved state of mind with respect to loss scale captures disorganized discourse regarding the death(s) of close others, and the Unresolved state of mind with respect to abuse scale captures similar discourse regarding experiences of physical and sexual abuse. The higher Unresolved score was used as an indicator of overall unresolved status (≥5). Agreement for the overall Unresolved score was r = .77 and for unresolved status, 88%. Disagreement between coders was settled by conference.
Relationship functioning
The Social Adjustment Scale (SAS)(Weissman & Paykel, 1974)) is a well-established interview assessing functioning in the preceding 2 months in domains of work, friendships/leisure, relationships with extended family, spouse/partner, and parenting (Weissman, Kasl, & Klerman, 1976). We used the domain scores for relationships with extended family (e.g., parents, siblings, adult children) and immediate family (spouse/partner, children). Potential scores range from 1 (excellent) to 7 (very poor) for each domain.
Positive quality in the relationship domains reflects the ability to effectively maintain and derive support and pleasure from well-balanced relationships, whereas poor quality reflects lack of reciprocity or balance, dissatisfaction, disengagement, and/or discord. For extended family relationships, participants are asked about conflicts, discussing feelings openly, feeling let down by family members, guilt over behavior, and ability to seek advice or help from family. For spouse/partner relationships, topics include arguments, discussion of feelings, balance in decision making, sharing of practical tasks, and affection. For parenting relationships, participants report involvement and interactions with children, and feelings of affection, worry, guilt and/or burden. A score of 1 reflects a very well-functioning relationship in terms of support, trust, and balance. As more negative features are reported, scores go up, e.g,, a score of 3 reflects both strengths and noticeable weaknesses in terms of regrets, imbalance, communication, etc. Scores for the relationship domains were averaged to obtain a relationship functioning score.
Coding was completed during audio-recorded interviews conducted by trained PhD or Master’s level research associates. A randomly selected subset of interviews (10%; n=22) were independently coded for agreement on all domains and one summary global adjustment score, achieving 91% agreement.
Depression symptoms
The Beck Depression Inventory-II (BDI)(Beck, Steer, & Brown, 1996) is a valid, reliable self-report assessment of depression symptoms. The continuous BDI-II score was used in analyses.
Metabolic Syndrome (MetS)
We used the National Cholesterol Education Program (NCEP/ATPIII) definition of MetS (Grundy et al., 2005) in the analyses, but waist to hip ratio was used as the indicator of central obesity rather than waist circumerference (Srikanthan, Seeman, & Karlamangla, 2009; Welborn & Dhaliwal, 2007). MetS is diagnosed if a person has ≥ 3 of 5 features: a) central obesity (i.e., waist to hip ratio > .90 for men, >.85 for women), b) triglycerides >150 mg/dl (1.7 mmol/l), c) low HDL cholesterol (<40 mg/dl for men, <50 mg/dL for women) or current treatment for hyperlipidemia, d) blood pressure > 130/85 or treatment for hypertension, and e) fasting glucose > 100 mg/dl (5.6 mmol/l) or treatment for hyperglycemia (not at the level of DM). We assessed the number of features present (0–5) as a continuous MetS score.
Diet
The Block Food Frequency Questionnaire (FFQ) (Block et al., 1986) was used to assess dietary intake over the past year. A nutrient intake score was calculated by multiplying the consumption frequency for each food item by its serving size, and then summing according to the Alternative Healthy Eating Index food groups (AHEI) (McCullough et al., 2002; McCullough & Willett, 2006). The AHEI score is based on vegetables, fruit, cereal fiber, nuts and soy, ratio of white to red meat, trans fat, ratio of polyunsaturated to saturated fatty acids, multivitamin use, and alcohol consumption. The possible range of scores is 2.5 (worst) to 87.5 (best).
Exercise
Participants reported the type and typical duration of aerobic and anaerobic regular exercise including type of sport, hours per week, months per year, and total years of practice as well as daily activities such as walking, resting, dancing, or gardening. The energy expenditure of the reported exercise during the past three months was estimated using metabolic equivalent hours per week (Ainsworth et al., 2011).
Smoking and alcohol use
The standardized medical history included smoking and alcohol consumption. Packs per day and drinks per week were used in analyses.
Statistical Analysis
Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted at Beth Israel Deaconess Medical Center (Harris et al., 2009). REDCap is a secure, web-based application that supports data capture for research studies. Across all participants and variables, 79% of the data was complete. Reasons for missingness varied (e.g., failure to draw blood, recording equipment failure) and were unrelated to key variables.
Descriptive analyses and correlations were performed using SPSS v21. Pearson correlations examined bivariate relations among variables to check for multicollinearity; they were not hypothesis generating. Path analyses were performed using Lisrel v8.80.
Results
Descriptive and Bivariate Analyses
Table 2 presents descriptive statistics (N = 215). There were more Black/African American women than other race/gender categories, χ2 (1) = 4.24, p < .05. Twenty-three percent of the sample had met criteria for MetS. Nearly 60% had 1–2 MetS risk factors (mean = 1.66).
Table 2.
| Mean (standard deviation)/Percentage | Range | |
|---|---|---|
| Race/Gender | White/European American men= 25% Black/African American men= 23% White/European American women = 20% Black/African American women = 32% |
|
| Adversity Sum | 3.18 (2.69) | 0 – 13 |
| Overall Adversity | 20.91 (27.92) | 0 – 137 |
| Coherence | 3.49 (1.63) | 1 – 8 |
| Idealization | 3.29 (1.68) | 1 – 8.5 |
| Unresolved Loss or Trauma | 36% | |
| Relationship Functioning | 2.37 (1.22) | 1 – 7 |
| Depression | 10.14 (9.68) | 0 – 39 |
| Diet | 44.81 (12.22) | 18.17 – 76.06 |
| Exercise/Activity (hours/week) | 16.84 (17.54) | 0 – 67.5 |
| Smoking (packs/day) | .19 (.37) | 0 – 2.5 |
| Drinking (drinks/week) | 2.94 (7.34) | 0 – 70 |
| Waist-Hip Ratio | 1.06 (.09) | .86 – 1.27 |
| Triglycerides mg/dl | 102.53 (73.93) | 35 – 582 |
| HDL Ratio | 1.23 (.38) | .38 – 2.53 |
| Hypertension | 36% | |
| Fasting Blood Glucose mg/dl | 97.84 (29.97) | 63 – 268 |
| MetS Sum Score | Mean = 1.66 (1.20) 0 Factors = 18% 1 Factor = 31% 2 Factors = 28% 3 Factors = 14% 4 Factors = 8% 5 Factors = <1% |
0 – 5 |
Table 3 presents zero-order correlations among variables. MetS sum scores were associated with coherence (r = −.22, p < .05), unresolved status (r = .18, p < .05), relationship functioning (r = .18, p < .05), diet (r = −.35, p < .001), and smoking (r = .22, p < .01).
Table 3.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Black/African American | -- | |||||||||||
| 2. Female | .14* | -- | ||||||||||
| 3. Childhood Adversity | .36*** | .14 | -- | |||||||||
| 4. Idealization | .03 | −.17* | −.23* | -- | ||||||||
| 5. Unresolved Loss or Trauma | .08 | −.11 | −.12 | .04 | -- | |||||||
| 6. Coherence | −.13 | .17* | −.11 | −.39*** | .14 | -- | ||||||
| 7. Relationship Functioning | .02 | −.16* | .24** | −.18* | −.12 | −.14 | -- | |||||
| 8. Depression | .16* | .10 | .26** | −.10 | .19* | −.10 | .34*** | -- | ||||
| 9. Diet | −.14 | .10 | −.16 | −.21* | −.09 | .22* | −.34*** | −.22* | -- | |||
| 10. Exercise | −.09 | −.13 | −.06 | .13 | −.03 | .01 | −.14 | −.22* | .27*** | -- | ||
| 11. Smoking (packs/day) | −.03 | −.07 | .30*** | .01 | −.06 | .05 | .17* | .23** | −.15 | .02 | -- | |
| 12. Alcohol (drinks/week) | −.02 | −.05 | −.01 | −.08 | −.13 | .04 | .01 | .01 | .08 | .19* | .02 | -- |
| 13. MetS Sum Score | .01 | −.09 | .06 | .10 | .19* | −.22* | .18* | .08 | −.35*** | −.18* | .22** | −.13 |
p < .001;
p < .01;
p < .05
Multivariate Analyses
A series of path analyses were conducted. An initial analysis tested the effects of health behaviors, i.e., smoking, alcohol consumption, exercise, and diet, on the number of MetS components, controlling for race and gender. Alcohol consumption and exercise were unrelated to MetS and were removed from the model. The next model included smoking and diet, which were statistically significant predictors (βsmoking = .18, p < .05; βdiet = −.34, p < .001) and together explained 16% of the variance in the MetS sum score (p < .001).
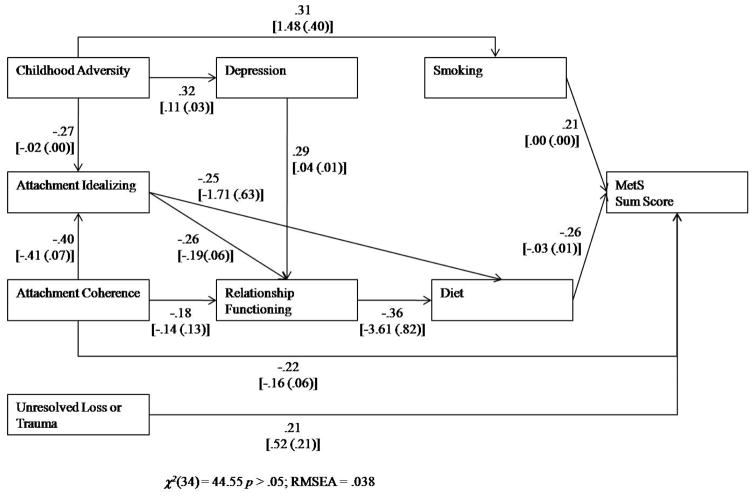
We tested the hypothesized path to MetS, controlling for race and gender, and found this model was a poor fit for the data [χ2(29) = 55.58, p < .01, RMSEA = .066]. We revised the model, removing non-significant paths and including suggested paths based on the modification indices, again controlling for race and gender. The final model was a good fit for the data [χ2(28) = 39.89, p > .01, RMSEA = .045] and is presented in Figure 2. Attachment coherence, unresolved status, diet and smoking emerged as direct predictors of the MetS score, and accounted for 21% of its variance. Several paths are of note.
Figure 2.
Best fitting path model linking adult attachment representations and health with standardized coefficients above and understandardized coefficients below (standard errors in parentheses).
Attachment coherence to MetS
There were indirect and direct paths to the MetS sum score from attachment variables. First, there were direct paths from coherence to MetS sum scores and from unresolved status to MetS sum scores. Lower coherence was linked to more MetS components, as was unresolved status. Second, there was an indirect path from incoherence to MetS sum score through poor relationship functioning then to poor diet leading to more MetS components. Idealization followed an indirect path to MetS through diet, with greater idealization being associated with worse diet that, in turn, predicted more MetS components.
Childhood adversity
Idealization was lower in those reporting more childhood adversity. There was an indirect path from childhood adversity to MetS through smoking: Individuals with more childhood adversity smoked more, which led to a higher MetS score. There was also an indirect path from childhood adversity to MetS through depressive symptoms, which led to worse relationship functioning, then poorer diet, and then to MetS.
We tested the model with each of the MetS components to determine whether any one was particularly vulnerable to these pathways of risk. Results yielded no good fitting models, suggesting that these pathways are not specific to any one component but to a more general state of health.
Given that MetS score is not an ordinal scale, we also performed a multinomial logistic regression. Given the limited number of participants who had four risk factors, we created a four-level variable for this analysis that had categories for having 0, 1, 2 or ≥3 MetS criteria. The reference category was the ≥3 group (indicating full MetS). Results supported those presented in the path model.
Discussion
Results of this study show previously unreported links between adult attachment discourse, relationship functioning, and health behaviors in adulthood that led to vulnerable metabolic status in midlife. These paths were evident even when accounting for childhood adversity and depressive symptoms.
We hypothesized that attachment representational security as indexed by AAI coherence would be directly and indirectly linked to midlife physical health. The direct path from coherence to MetS is consistent with the concept that adult attachment security is an indicator of homeostatic regulation that is achieved through effectively discriminating and responding to potential dangers and stressors. The ability to assess the internal and external environment leads to adaptive coping strategies, especially the use of close relationships as stress buffers, and subsequent rapid physiological and psychological recovery from stress (Ainsworth et al., 1978; Bowlby, 1969/1982; Hostinar et al., 2013). Importantly, the results are consistent with both ‘bottom-up’ and ‘top-down’ cognitive control of stress and regulation of the hypothalamic-pituitary-adrenal (HPA) axis, dysregulation of which is considered to play a major role in metabolic functioning (Coan, 2008; Danese & McEwen, 2012; Pervanidou & Chrousos, 2012; Spencer & Tilbrook, 2011). To our knowledge, such a cognitive mechanism regulating hormonal and metabolic functioning has not been previously described, but it is consistent with hypothesized and demonstrated links between early attachment experiences, social buffering of stress, subsequent fear learning and memory, and associations with neuroendocrine functioning in both humans and animals (Hostinar et al., 2013; Landers & Sullivan, 2012; Sullivan, 2012).
Unresolved status
Unresolved attachment status was also directly linked to the number of MetS components participants manifested. This result suggests that there may be a separate pathway to stress identification and management associated with traumatic events and the development of a disorganized state. Early and chronic stress and trauma are well known to predict health outcomes, impacting on energy regulating hormonal systems (Danese & McEwen, 2012; Davis et al., 2013b). Significant trauma in both humans and animal models leads to activation of biological stress response systems, including the HPA axis, and temporary cognitive disorganization, especially in brain areas associated with memory, including the hippocampus, amygdala, and prefrontal cortex (Bremner, 2005; Freed, Yanagihara, Hirsch, & Mann, 2009; Hostinar et al., 2013; Landers & Sullivan, 2012; Najib, Lorberbaum, Kose, Bohning, & George, 2004).
By definition, unresolved attachment status indicates a disorganized state of mind characterized by impaired memory processes and a lack of integration of the experience beyond a typical recovery period (AAI coding specifies that the event occurred more than a year prior to the interview for unresolved status to be scored). Our results suggest that unresolved status impacts metabolic functioning through a ‘bottom-up’ dysregulation of the brain areas (e.g., amygdala and hypothalamus) involved in memory and stress identification. We hypothesize that frightening memories are repeatedly cued increasing allostatic load, overriding more salient and proximal cues of new stresses and dangers, and disrupting care seeking processes.
Idealization
Idealization was the third attachment component associated with health outcomes, specifically that of poor diet. Idealization is indicative of a coping strategy that avoids, denies, or dismisses the importance of danger or stress in the internal or external environment, striving to present an image of normality. Indeed, in laboratory-based stressful situations, infants and adults who employ avoidant strategies appear outwardly calm (M. D. S. Ainsworth et al., 1978; Dozier & Kobak, 1992; Main et al., 1985; Sroufe & Waters, 1977). But compared with individuals classified as secure, physiological assessments show high levels of arousal as measured by heart rate and skin conductance, as well as slow recovery time, indicating that avoidance is ineffective in regulating heightened arousal.
With respect to diet, stressful circumstances stimulate preference for foods that are high in fats and carbohydrates (Spencer & Tilbrook, 2011). Idealizing/avoidant individuals are at a relative disadvantage in assessing day-to-day stresses and utilizing relationship-based coping strategies. Our findings suggest that those who idealize are more vulnerable to a reward-based system of coping that uses high fat and carbohydrate foods rather than close others (Volkow, Wang, & Baler, 2011). Furthermore, an idealizing individual may normalize/rationalize their poor diet and its subsequent consequences, limiting their cognitive control over this health risk behavior.
Lastly, both attachment coherence and idealization are associated with reports of higher quality family relationships. The former result is consistent with previous work that more secure/coherent representations predict better relationship functioning (Crowell et al., 2002; Simpson et al., 2002). However, both coherent and idealizing individuals report good family relationships; the former because they have overall more adaptive and functional relationships and the latter because they idealize or normalize relationships, and may indeed enjoy family members even if they do not use them as resources when stressed (Treboux et al., 2004).
Childhood adversity
Childhood adversity indirectly impacted on MetS. Consistent with previous findings (Anda, et al., 1999), adverse childhood experiences were associated with smoking, a well-known health risk behavior. Smoking is an established behavior for middle-aged adults, a habit that typically develops before the age of 18 within the peer group (Services, 2012; Umberson et al., 2010). It is therefore not surprising that this health risk is associated with early social circumstances rather than with current family relationships or cognitions.
Another path that linked childhood adversity to MetS was via depressive symptoms and impaired or stressful family relationship functioning that in turn linked with poor dietary habits. This aspect of our hypothesized model fits with previously demonstrated findings linking childhood adversity to depression (Bosch, Seifritz, & Wetter, 2012; Hammen, Kim, Eberhart, & Brennan, 2009; Meyer & Paul, 2011; Wiersma et al., 2009), depression to family functioning (Bulloch, Williams, Lavorato, & Patten, 2009; Heene, Buysse, & Van Oost, 2007; Kaufman et al., 2004; Meyer & Paul, 2011), and family functioning to diet (Ackard, Neumark-Sztainer, Story, & Perry, 2006; Umberson et al., 2010). The effect of family relationships on diet is multi-factorial, ranging from metabolic changes within the individual associated with stress to common factors such as socioeconomic status contribute to both family functioning and diet (Umberson et al., 2010).
Limitations
Path analyses allow us to order variables based upon hypothesized mechanisms and to demonstrate that the data fits well with such a hypothesized model. Nevertheless, the study is cross-sectional and cannot examine causal pathways. The relatively small sample size is a limitation to including other potential explanatory variables such as socioeconomic status or hormonal pathways that could provide further explanation of mechanisms.
Bias in retrospective reporting of childhood adversities may represent another limitation. However, several important studies support the validity of such retrospective reports, finding negligible differences between prospective and retrospective reports (Brown, Craig, Harris, Handley, & Harvey, 2007; Miller, Chen, & Parker, 2011; Scott, McLaughlin, Smith, & Ellis, 2012). Furthermore our retrospective evaluations of adversity are based on interview data rather than self-report questionnaires and employ a comprehensive method of assessing childhood adversity (Davis et al., 2013b).
Conclusions
We find evidence that Adult Attachment Interview discourse markers are directly and indirectly linked to midlife physical health. The findings are consistent with the hypothesis that adult attachment status is an indicator of homeostatic regulation through effective discrimination of and responses to potential dangers and stressors. Coherence appears to reflect the quality of the attachment-based guide or ‘road map’ for recognizing and managing stress and danger especially through social support buffering processes. The cognitive effects of unresolved abuse and loss appear to independently disrupt this attachment “guidance” system, over and above the impact of insecure/incoherent processes that emerge from ordinary, but non-optimal attachment experiences.
From the standpoint of reversing potential effects of negative childhood experiences on health, it is important to note that attachment representational patterns originate in infancy and are very stable constructs. However, they are shaped by attachment experiences and the caregiving environment later in life (Crowell & Hauser, 2008; Crowell et al., 2002), and secure base behaviors and cognitions can be considered as potential targets for intervention.
Acknowledgments
This research was supported by the National Institute of Aging, grant 44934, National Institute of Diabetes and Digestive and Kidney Diseases grant 81913, and Grant Number UL1 RR025758-Harvard Clinical and Translational Science Center, from the National Center for Research Resources.
References
- Ackard D, Neumark-Sztainer D, Story M, Perry C. Parent–child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine. 2006;30:59–66. doi: 10.1016/j.amepre.2005.09.013. [DOI] [PubMed] [Google Scholar]
- Ainsworth B, Haskell W, Herrmann S, Meckes N, Bassett D, Jr, Tudor-Locke C, … Leon A. Compendium of Physical Activities: a second update of codes and MET values. Medicine and Science in Sports and Exercise. Medicine and Science in Sports and Exercise. 2011;43(8):1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- Ainsworth MDS. Attachments across the life span. Bulletin of the New York Academy of Medicine. 1985;61(9):792–811. [PMC free article] [PubMed] [Google Scholar]
- Ainsworth MDS. Attachments and other affectional bonds across the life cycle. In: Parkes CM, Stevenson-Hinde J, Marris P, editors. Attachment across the life cycle. London: Routledge; 1991. pp. 33–51. [Google Scholar]
- Ainsworth MDS, Blehar M, Waters E, Wall S. Patterns of attachment: A psychological study of the Strange Situation. Hillsdale, NJ: Lawrence Erlbaum; 1978. [Google Scholar]
- Anda R, Croft J, Felitti V, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. Manual for the Beck Depression Inventory-II. Vol. 82. Psychological Corporation; 1996. [Google Scholar]
- Bentley T, Widom C. A 30-year follow-up of the effects of child abuse and neglect on obesity in adulthood. Obesity. 2009;17:1900–1905. doi: 10.1038/oby.2009.160. [DOI] [PubMed] [Google Scholar]
- Block G, Hartman A, Dresser C, Carroll M, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. American Journal of Epidemiology. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- Bosch O, Seifritz E, Wetter T. Stress-related depression: Neuroendocrine, genetic, and therapeutical aspects. World J Biol Psychiatry. 2012 Jun 7; doi: 10.3109/15622975.2012.665477. epub. [DOI] [PubMed] [Google Scholar]
- Bowlby J. The nature of the child’s tie to its mother. International Journal of Psycho-Analysis. 1958;39:350–373. [PubMed] [Google Scholar]
- Bowlby J. Attachment and Loss: Attachment. Vol. 1. New York: Basic Books; 1969/1982. [Google Scholar]
- Bremner JD. Effects of traumatic stress on brain structure and function: relevance to early responses to trauma. Journal of Trauma & Dissociation. 2005;6(2):51–68. doi: 10.1300/J229v06n02_06. [DOI] [PubMed] [Google Scholar]
- Bretherton I. Attachment theory: Retrospect and prospect. In: Bretherton I, Waters E, editors. Growing points of attachment theory and research. 1–2. Vol. 50. Chicago: Monographs of the Society for Research in Child Development; 1985. pp. 3–35. Serial No. 209. [Google Scholar]
- Bretherton I, Munholland K. In: H. o. A. T., research and clinical application. 2. Cassidy J, Shaver P, editors. New York: Guilford; 2008. rev. ed. [Google Scholar]; Cassidy J, Shaver P, editors. Handbook of Attachment: Theory, research and clinical application. 2. New York: Guilford PRess; Internal working models in attachment relationships: Elaborating a central construct in attachment theory; pp. 102–127. [Google Scholar]
- Brown G, Craig T, Harris T, Handley R, Harvey A. Validity of retrospective measures of early maltreatment and depressive episodes using the Childhood Experiences of Care and Abuse (CECA) instrument-a life course study of adult chronic depression. Journal of Affective Disorders. 2007;103:217–224. doi: 10.1016/j.jad.2007.06.003. [DOI] [PubMed] [Google Scholar]
- Bulloch A, Williams J, Lavorato D, Patten S. The relationship between major depression and marital disruption is bidirectional. Depression and Anxiety. 2009;26(12):1172–1177. doi: 10.1002/da.20618. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Shaver P, editors. Handbook of Attachment: Theory, Research, and Clinical Applications. 2. New York: Guilford Press; 2008. [Google Scholar]
- CDC. Adverse Childhood Experiences Study. 2012 Retrieved July 1, 2012, from http://www.cdc.gov/ace/
- Census, U. US Census Bureau: State and County Quick Facts. Boston (city), Massachusetts: 2012. Jun 6, Retrieved July 18, 2012. [Google Scholar]
- Chichlowska K, Rose K, Diez-Roux A, Golden S, McNeill A, Heiss G. Life course socioeconomic conditions and metabolic syndrome: The Atherosclerosis Risk in Communities (ARIC) Study. Annals of Epidemiology. 2009;19:875–883. doi: 10.1016/j.annepidem.2009.07.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciechanowski P, Russo J, Katon W, Von Korff M, Ludman E, Lin E, … Bush T. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosomatic Medicine. 2004;66:720–728. doi: 10.1097/01.psy.0000138125.59122.23. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Sullivan M, Jensen M, Romano J, Summers H. The relationship of attachment style to depression, catastrophizing and health care utilization in patients with chronic pain. Pain. 2003;104:627–637. doi: 10.1016/S0304-3959(03)00120-9. [DOI] [PubMed] [Google Scholar]
- Coan J. Toward a neuroscience of attachment. In: Cassidy J, Shaver P, editors. Handbook of Attachment: Theory, Research, and Clinical Applications. New York: The Guilford Press; 2008. pp. 241–265. [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Creasey G. Associations between working models of attachment and conflict management behavior in romantic couples. Journal of Counseling Psychology. 2002;49(3):365–375. doi: 10.1037/0022-0167.49.3.365. [DOI] [Google Scholar]
- Crowell J, Treboux D, Gao Y, Fyffe C, Pan H, Waters E. Assessing secure base behavior in adulthood: Development of a measure, links to adult attachment representations, and relations to couples’ communication and reports of relationships. Developmental Psychology. 2002;38:679–693. [PubMed] [Google Scholar]
- Crowell JA. A lifespan perspective: Elements of continuity and discontinuity in the attachment system (Continuità e discontinuità nel sistema dell’attaccamento) In: Cavanna CLD, Zavatini G-C, editors. Love and Attachment in Couples: Psicologia delle relazioni di coppia. Bologna: Il Mulino; 2009. [Google Scholar]
- Crowell JA, Hauser S. Adult Attachment Interviews in a high risk sample: Stability and relation to functioning from adolescence to 39 years. In: Steele H, Steele M, editors. Clinical Applications of the Adult Attachment Interview. New York: Guilford Press; 2008. pp. 223–244. [Google Scholar]
- Crowell JA, Treboux D, Gao Y, Fyffe C, Pan H, Waters E. Assessing secure base behavior In adulthood: Development of a measure, links to adult attachment representations, and relationships to couples’ communication and reports of relationships. Developmental Psychology. 2002;38:679–693. [PubMed] [Google Scholar]
- D’Argenio A, Mazzi C, Pecchioli L, Di Lorenzo G, Siracusano A, Troisi A. Early trauma and adult obesity: Is psychological dysfunction the mediating mechanism? Physiology & Behavior. 2009;98:543–546. doi: 10.1016/j.physbeh.2009.08.010. [DOI] [PubMed] [Google Scholar]
- Danese A, McEwen B. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiology & Behavior. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- Davis C, Dearing E, Usher N, Trifiletti S, Zaichenko L, Offen E, … Crowell J. Detailed assessments of childhood adversity enhance prediction of central obesity independent of gender, race, adult psychosocial risk and health behaviors. Metabolism. 2013a doi: 10.1016/j.metabol.2013.1008.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C, Dearing E, Usher N, Trifiletti S, Zaichenko L, Offen E, … Crowell JA. Detailed assessments of childhood adversity enhance prediction of central obesity independent of gender, race, adult psychosocial risk and health behaviors. Metabolism. 2013b doi: 10.1016/j.metabol.2013.1008.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo M. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- DiMatteo M, Lepper H, Croghan T. Depression Is a risk factor for noncompliance With medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. JAMA. 2000;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- Dozier M, Kobak R. Psychophysiology in attachment interviews: Convergin evidence for deactivating strategies. Child Development. 1992;63(6):1473–1480. doi: 10.1111/j.1467-8624.1992.tb01708.x. [DOI] [PubMed] [Google Scholar]
- Dykas M, Woodhouse S, Cassidy J, Waters H. Narrative Assessment of Attachment Representations: Links between Secure Base Scripts and Adolescent Attachment. Attachment and Human Development. 2006;8:221–240. doi: 10.1080/14616730600856099. [DOI] [PubMed] [Google Scholar]
- Eaker E, Sullivan L, Kelly-Hayes M, D’Agostino R, Benjamin E. Marital status, marital strain, and the risk of coronary heart disease of total mortality: The Framingham Offspring Study. Psychosomatic Medicine. 2007;69(6):509–513. doi: 10.1097/PSY.0b013e3180f62357. [DOI] [PubMed] [Google Scholar]
- Feeney J, Ryan S. Attachment style and affect regulation: Relationships with health behaviour and family experiences of illness in a student sample. Health Psychology. 1994;13(4):334–345. doi: 10.1037//0278-6133.13.4.334. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP) New York: iometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Freed P, Yanagihara T, Hirsch J, Mann J. Neural mechanisms of grief regulation. Biological Psychiatry. 2009;68(1):33–40. doi: 10.1016/j.biopsych.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fricchione G. Compassion and Healing in Medicine and Society: On the Nature and Use of Attachment Solutions to Separation Challenges. Baltimore, MD: Johns Hopkins University Press; 2011. [Google Scholar]
- Fricchione G. Compassion and Healing in Medicine and Society. On the Nature and Uses of Attachment Solutions to Separation Challenges. Johns Hopkins University Press; 2011. [Google Scholar]
- Gable S, Gosnell C. Approach and avoidance behavior in interpersonal relationships. Emotion Review. 2013;5(4):269–274. doi: 10.1177/1754073913477513. [DOI] [Google Scholar]
- George C, Kaplan N, Main M. The Adult Attachment Interview. University of California; Berkeley: 1985. Unpublished manuscript. [Google Scholar]
- Glanz K, Schwartz M. Stress, coping and health behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health behavior and health education: theory, research and practice. San Francisco: Jossey-Bass; 2008. pp. 211–236. [Google Scholar]
- Grundy S, Cleeman J, Daniels S, Donato K, Eckel R, … Franklin B, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Hammen C, Kim E, Eberhart N, Brennan P. Chronic and acute stress and the prediction of major depression in women. Depression and Anxiety. 2009;26(8):718–723. doi: 10.1002/da.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser S, Powers S, Noam G. Adolescents and Their Families: Paths of Ego Development. New York: Free Press; 1991. [Google Scholar]
- Hauser S, Powers S, Noam G, Jacobson A, Weiss B, Follansbee D. Family contexts of adolescent ego development. Child Development. 1984;55:195–213. [PubMed] [Google Scholar]
- Heene E, Buysse A, Van Oost P. An interpersonal perspective on depression: The role of marital adjustment, conflict, communication, attributions, and attachment within a clinical sample. Family Process. 2007;46(4):499–514. doi: 10.1111/j.1545-5300.2007.00228.x. [DOI] [PubMed] [Google Scholar]
- Hesse E. The Adult Attachment Interview: Protocol, Method of Analysis, and Empirical Studies. In: Cassidy J, Shaver PR, editors. Handbook of Attachment: Theory, Research and Clinical Applications. New York: Guilford Press; 2009. pp. 552–598. [Google Scholar]
- Hostinar C, Sullivan R, Gunnar M. Psychobiological mechanisms underlying the social buffering of the hypothalamic-pituitary-adrenocortical axis: A review of animal models and human studies across development. Psychological Bulletin. 2013 doi: 10.1037/a0032671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka L, Glaser R, Loving T, Malarkey W, Stowell J, Kiecolt-Glaser J. Attachment anxiety is linked to alterations in cortisol production and cellular immunity. Psychological Science. 2013 doi: 10.1177/0956797612452571. http://pss.sagepub.com/content/early/2013/01/10/0956797612452571. [DOI] [PMC free article] [PubMed]
- Kaufman J, Yang B, Douglas-Palumberi H, Houshyar S, Lipschitz D, Krystal J, Gelertner J. Social supports and serotonin transporter gene moderate depression in maltreated children. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(4):17316–17321. doi: 10.1073/pnas.0404376101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidd T, Sheffield D. Attachment style and symptom reporting: Examining the mediating effects of anger and social support. British Journal of Health Psychology. 2005;10:531–541. doi: 10.1348/135910705X43589. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J, Newton T. Marriage and health: His and hers. Psychological Bulletin. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Krinsley K. Psychometric review of the Evaluation of Lifetime Stressors (ELS) questionnaire and interview. In: Stamm B, editor. Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press; 1996. [Google Scholar]
- Landers M, Sullivan R. The development and neurobiology of infant attachment and fear. Developmental Neurosciences. 2012;34:2–3. doi: 10.1159/000336732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin E, Katon W, Von Korff M, Rutter C, Simon G, Oliver M, … Young B. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–2160. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- Madigan S, Moran G, Schuengel C, Pederson D, Otten R. Unresolved maternal attachment representations, disrupted maternal behavior and disorganized attachment in infancy: Links to toddler behavior problems. Journal of Child Psychology and Psychiatry. 2007;48:1042–1050. doi: 10.1111/j.1469-7610.2007.01805.x. [DOI] [PubMed] [Google Scholar]
- Magai C. Attachment in middle and later life. In: Cassidy J, Shaver P, editors. Handbook of Attachment: Theory, Research, and Clinical Applications. New York: Guilford Press; 2008. [Google Scholar]
- Main M, Goldwyn R. Adult Attachment Rating and Classification Systems, Version 6.0. University of California; Berkeley: 1994. Unpublished manuscript. [Google Scholar]
- Main M, Kaplan N, Cassidy J. Security of infancy, childhood, and adulthood: A move to the level of representation. In: Bretherton I, Waters E, editors. Growing points of attachment theory and research. 1–2. Vol. 50. 1985. pp. 66–106. Monographs for the Society for Research in Child Development. Serial No. 209. [Google Scholar]
- Marvin R, Cooper G, Hoffman K, Powell B. The Circle of Security project: Attachment-based intervention with caregiver-pre-school child dyads. Attachment and Human Development. 2002;4(1):107–124. doi: 10.1080/14616730252982491. [DOI] [PubMed] [Google Scholar]
- Maunder R, Hunter J. Attachment and psychosomatic medicine: Developmental contributions to stress and disease. Psychosomatic Medicine. 2001;63:556–567. doi: 10.1097/00006842-200107000-00006. [DOI] [PubMed] [Google Scholar]
- Maunder R, Hunter J. Assessing pattern of adult attachment in medical patients. General Hospital Psychiatry. 2009;31:123–130. doi: 10.1016/j.genhosppsych.2008.10.007. [DOI] [PubMed] [Google Scholar]
- McCullough M, Feskanich D, Stampfer M, Giovannucci E, Rimm E, Hu F, … Willet W. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. The American Journal of Clinical Nutrition. 2002;76(6):1261–1271. doi: 10.1093/ajcn/76.6.1261. [DOI] [PubMed] [Google Scholar]
- McCullough M, Willett W. Evaluating adherence to recommended diets in adults: the Alternate Healthy Eating Index. Public Health Nutrition. 2006;9:152–157. doi: 10.1079/phn2005938. [DOI] [PubMed] [Google Scholar]
- McEwen B. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen B, Getz L. Lifetime experiences, the brain and personalized medicine: An integrative perspective. Metabolism. 2013;62:520–526. doi: 10.1016/j.metabol.2012.08.020. [DOI] [PubMed] [Google Scholar]
- McEwen B, Stellar E. Stress and the individual. Mechanisms leading to disease. Archives of Internal Medicine. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- McWilliams L, Bailey S. Associations between adult attachment ratings and health conditions: Evidence from the National Comorbidity Survey Replication. Health Psychology. 2010;29(4):446–453. doi: 10.1037/a0020061. [DOI] [PubMed] [Google Scholar]
- Meyer D, Paul R. A cross-national examination of marriage and early life stressors as correlates of depression, anxiety, and stress. The Family Journal. 2011;19(3):274–280. [Google Scholar]
- Midei A, Matthews K, Chang Y-F, Bromberger J. Childhood physical abuse is associated with incident metabolic syndrome in midlife women. Health Psychology. 2012 doi: 10.1037/a0027891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller G, Chen E, Parker K. Psychological stress in childhood and susceptibility to the chronic issues of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137(6):959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najib A, Lorberbaum J, Kose S, Bohning D, George M. Regional brain activity in women grieving a romantic relationship breakup. American Journal of Psychiatry. 2004;161:2245–2256. doi: 10.1176/appi.ajp.161.12.2245. [DOI] [PubMed] [Google Scholar]
- Parker L, Lamont D, Unwin N, Pearce M, Bennett S, Dickinson H, … Craft A. A life course study of risk for hyperinsulinaemia, dyslipidaemia and obesity (the central metabolic syndrome) at age 49–51 years. Diabetic Medicine. 2003;20:406–415. doi: 10.1046/j.1464-5491.2003.00949.x. [DOI] [PubMed] [Google Scholar]
- Pervanidou P, Chrousos G. Metabolic consequences of stress during childhood and adolescence. Metabolism. 2012;61:611–619. doi: 10.1016/j.metabol.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Porter L, Davis D, Keefe F. Attachment and pain: Recent findings and future directions. Pain. 2007;128(3):195–198. doi: 10.1016/j.pain.2007.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posada G, Gao Y, Fang W, Posada R, Tascon M, Schoelmerich A, … Synnevaag B. The secure- base phenomenon across cultures: Children’s behavior, mothers’ preferences, and experts’ concepts. In: Waters E, Vaughn B, Posada G, Kondo-Ikemura K, editors. Caregiving, Cultural and Cognitive Perspectives on Secure-Base Behavior and Working Models: New Growing Points of Attachment Theory and Research. 2–3. 1995. pp. 27–48. [Google Scholar]
- Puig J, Englund M, Simpson J, Collins W. Predicting adult physical illness from infant attachment: a propective longitudinal study. Health Psychology, Advance online publication. 2012 doi: 10.1037/a0028889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raby KL, Cicchetti D, Carlson EA, Egeland B, Collins WA. Genetic contributions to continuity and change in attachment security: A prospective, longitudinal investigation from infancy to young adulthood. Journal of Child Psychiatry and Psychology. 2013;54(11):1223–1230. doi: 10.1111/jcpp.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti R, Taylor S, Seeman T. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. [PubMed] [Google Scholar]
- Rey J, Stewart G, Plapp J, Bashir M, Richards I. DSM-III Axis IV Revisited. American Journal of Psychiatry. 1988;145:286–292. doi: 10.1176/ajp.145.3.286. [DOI] [PubMed] [Google Scholar]
- Scott K, McLaughlin K, Smith D, Ellis P. Childhood maltreatment and DSM-IV adult mental disorders: Comparison of prospective and retrospective findings. British Journal of Psychiatry. 2012;200:469–475. doi: 10.1192/bjp.bp.111.103267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Services, U. S. D. o. H. a. H. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2012. [Google Scholar]
- Simpson J, Rholes WS, Orina MM, Grich J. Working models of attachment, support giving, and support seeking in a stressful situation. Personality and Social Psychology Bulletin. 2002;28:598–608. [Google Scholar]
- Spencer S, Tilbrook A. The glucocorticoid contribution to obesity. Stress. 2011;14(3):233–246. doi: 10.3109/10253890.2010.534831. [DOI] [PubMed] [Google Scholar]
- Srikanthan P, Seeman TE, Karlamangla AS. Waist-hip-ratio as a predictor of all-cause mortality in high-functioning older adults. Annals of Epidemiology. 2009;19:724–731. doi: 10.1016/j.annepidem.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sroufe LA, Waters E. Heart rate as a convergent measure in clinical and developmental research. Merrill-Palmer Quarterly. 1977;23:3–27. [Google Scholar]
- Stovall-McCough KC, Cloitre M. Unresolved attachment, PTSD, and dissociation in women with child abuse histories. Journal of Clinical and Consulting Psychology. 2006;74:219–228. doi: 10.1037/0022-006X.74.2.219. [DOI] [PubMed] [Google Scholar]
- Sullivan R. The neurobiology of attachment to nurturing and abusive caregivers. Hastings Law Journal. 2012;63(6):1553–1570. [PMC free article] [PubMed] [Google Scholar]
- Thomas C, Hyponnen E, Power C. Obesity and type 2 diabetes risk in mid-adult life: the role of childhood adversity. Pediatrics. 2008;121:e1240–1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- Treboux D, Crowell JA, Waters E. When “new” meets “old”: configurations of adult attachment representations and their implications for marital functioning. Dev Psychol. 2004;40(2):295–314. doi: 10.1037/0012-1649.40.2.295. [DOI] [PubMed] [Google Scholar]
- Umberson D, Crosnos R, Reczek C. Social relationships and health behavior across the life course. Annual Review of Sociology. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N, Wang GJ, Baler R. Reward, dopamine and the control of food intake: implications for obesity. Trends in Cognitive Sciences. 2011;15(1):37–46. doi: 10.1016/j.tics.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vythilingam M, Heim C, Newport J, Miller A, Anderson E, Bronen R, … Bremner J. Childhood trauma associated with smaller hippocampal volume in women with major depression. American Journal of Psychiatry. 2002;159(12):2072–2080. doi: 10.1176/appi.ajp.159.12.2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters E, Hamilton CE, Weinfield N. The stability of attachment security from infancy to adolescence and early adulthood: General introduction. Child Development. 2000;71:678–706. doi: 10.1111/1467-8624.00175. [DOI] [PubMed] [Google Scholar]
- Waters E, Kondo-Ikemura K, Posada G, Richters J, editors. Learning to love: Milestones and mechanisms. Vol. 23. Hillsdale, NJ: Erlbaum; 1991. [Google Scholar]
- Waters H, Waters E. The attachment working models concept: Among other things, we build script-like representations of secure base experiences. Attachment and Human Development. 2006;8(3):185–197. doi: 10.1080/14616730600856016. [DOI] [PubMed] [Google Scholar]
- Waters T, Brockmeyer S, Crowell J. AAI coherence predicts caregiving and care seeking behavior: Secure base script knowledge helps explain why. Attachment and Human Development. 2013a;15(3):316–331. doi: 10.1080/14616734.2013.782657. [DOI] [PubMed] [Google Scholar]
- Waters T, Brockmeyer S, Crowell JA. AAI coherence predicts caregiving and care seeking behavior: Secure base script knowledge helps explain why. Attachment and Human Development. 2013b;15(3):316–331. doi: 10.1080/14616734.2013.782657. [DOI] [PubMed] [Google Scholar]
- Weiss R. Attachment in adult life. In: Parkes CM, Stevenson-Hinde J, editors. The place of attachment in human behavior. Englewood Cliffs, NJ: Prentice Hall; 1982. [Google Scholar]
- Weissman M, Kasl S, Klerman G. Follow-up of depressed women after maintenance treatment. American Journal of Psychiatry. 1976;133(7):757–760. doi: 10.1176/ajp.133.7.757. [DOI] [PubMed] [Google Scholar]
- Weissman M, Paykel E. The depressed woman: A study of social relationships. Chicago: University of Chicago Press; 1974. [Google Scholar]
- Welborn TA, Dhaliwal SS. Preferred clinical measures of central obesity for predicting mortality. European Journal of Clinical Nutrition. 2007;61:1373–1379. doi: 10.1038/sj.ejcn.1602656. [DOI] [PubMed] [Google Scholar]
- Wiersma J, Hovens J, van Oppen P, Gittay E, van Schalk D, Beekman A, Penninx B. The importance of childhood trauma and childhood life events for chronicity of depression in adults. The Journal of Clinical Psychiatry. 2009;70(7):983–989. doi: 10.4088/jcp.08m04521. [DOI] [PubMed] [Google Scholar]