Common antibiotics might do more than just kill bacteria. New research suggests that some antibiotics can protect against the nerve damage associated with diseases such as amyotrophic lateral sclerosis (ALS), dementia, stroke and epilepsy. The beneficial effects of a family of β-lactam antibiotics, which includes antibiotics such as penicillin, was recently discovered by Jeffrey Rothstein and colleagues,1 who found that these antibiotics could protect against the dysfunctional effects of the neurotransmitter glutamate in mice by activating the expression of a glutamate transporter. This finding suggests a new role for some of the most commonly used pharmaceuticals in the world.
Glutamate's Jekyll-and-Hyde effects
The amino acid glutamate has long been a target in the search for drugs to modify neurologic effects. Such interest is based on the fact that glutamate is a workhorse of the mammalian central nervous system (CNS), functioning primarily as an excitatory neurotransmitter but also contributing to learning and memory.2 However, when present in excessive amounts or for prolonged periods in the brain, glutamate has a dark side: in such situations, it can destroy neurons and thereby contribute to neurodegenerative diseases.2
Glutamate-mediated toxicity is thought to result from the malfunctioning of glutamate's release and reuptake cycle. Normally, glutamate present in the cytoplasm of a neuron is transported into synaptic vesicles, subsequently released into the synaptic cleft to initiate neurotransmission, and then reabsorbed by neurons and surrounding glial cells to terminate its action. The rapid removal of glutamate from the extracellular space prevents neurons from being exposed to its toxic effects, a feat accomplished by proteins called excitatory amino acid transporters (EAATs), whose malfunction can directly result in neurotoxic effects.
Five EAATs are currently known in humans, but EAAT2 appears to be a particularly important glutamate transporter. EEAT2 provides 90% of the total glutamate uptake, and its altered expression in several neurodegenerative diseases suggests an important role in their pathophysiology.2 For example, the selective loss of EAAT2 expression has been shown to be correlated with the development of ALS and epilepsy.3
The importance of EAAT2 in balancing glutamate's positive and negative effects makes this protein a prime target in the search for drugs to combat neurodegenerative diseases. Nevertheless, there is as yet no practical pharmaceutical capable of positively modulating EAAT2.1
New tricks for old drugs
Rothstein and colleagues' work therefore represents a significant step forward in the search for drugs that modulate EAAT2 expression. They screened 1040 FDA-approved drugs and nutritionals as part of a National Institutes of Health project to search for potential new uses for these compounds. Rothstein and colleagues performed blinded screens that involved adding each drug to rodent spinal cord tissue cultures for 5–7 days and then determining the expression levels of GLT1, the mouse equivalent of human EETA2, in each tissue sample.
Of the 1040 drugs, the structurally related family of β-lactam antibiotics, which include penicillin and cephalosporin antibiotics, were surprisingly effective at increasing the levels of rodent GLT1 protein expression. And in the case of the representative cephalosporin, ceftriaxone, this induction occurred at a concentration found in the CNS during ceftriaxone therapy for meningitis.4 In contrast, non β-lactam antibiotics such as kanamycin and vancomycin had no effect on GLT1 protein expression. The effect of β-lactam antibiotics also extended to human cells lines, where Rothstein and colleagues revealed that the EAAT2 promoter could be similarly activated.
Rothstein and colleagues went on to look at the effect of ceftriaxone in adult rats. They found that a 5–7 day course of ceftriaxone increased GLT1 expression in the rat brain three-fold. This increase correlated with higher levels of glutamate transport in these animals, suggesting that the biochemical activity of GLT1 also increased on ceftriaxone exposure. Similar experiments with penicillin revealed that this antibiotic was also capable of increasing the biochemical activity of GLT1, although to a lesser extent than ceftriaxone, a fact Rothstein and colleagues suggest is due to penicillin's inability to penetrating the brain as effectively as ceftriaxone.
No therapies currently exist to modulate glutamate-mediated injury through glutamate transporters. However, Rothstein and colleagues hypothesized that increasing the levels of glutamate transporters such as EAAT2/GLT1 may help protect neurons from injury. The research group therefore wondered whether β-lactam antibiotics could protect neurons from the negative effects of glutamate. In one set of experiments designed to test this hypothesis, daily injections of ceftriaxone were given to mice engineered to develop symptoms similar to ALS, including muscle weakness and loss of body weight. In each case, ceftriaxone therapy delayed the onset of these symptoms, ultimately extending the lifespan of these mice by 10 days as compared to untreated animals.
Although preliminary, Rothstein and colleagues' results suggest that commonly used β-lactam antibiotics might provide some protection against nerve damage. It is still too early to begin prescribing such antibiotics, since such measures must await a formal clinical trial to ascertain any benefit in human patients. However, such a trial does not appear to be far off. A press release from Johns Hopkins, where Rothstein and colleagues undertook their current study, states that a study of the effect of ceftriaxone treatment in ALS patients is set for the spring (www.hopkinsmedicine.org/Press_releases/2005/01_05_05.html). Thus, it appears that drugs praised for their ability to kill bacteria might still have a few undiscovered tricks up their sleeves. — David Secko, Vancouver
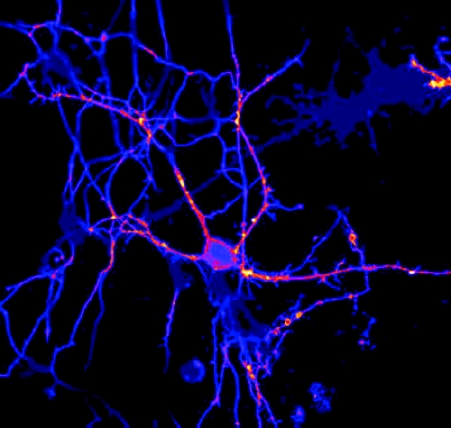
Figure. Two rat hippocampal neurons expressing lipid modified YFP. The lipid modifications cause them to be concentrated 1) at sites of cell:cell contact, presumably synapses and 2) in the growth cones of growing branches. Reprinted with permission by Dr. David Zacharias, The Whitney Laboratory for Marine Bioscience.
References
- 1.Rothstein JD, Patel S, Regan MR, Haenggeli C, Huang YH, Bergles DE, et al. β-Lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature 2005;433:73-7. [DOI] [PubMed]
- 2.Shigeri Y, Seal RP, Shimamoto K. Molecular pharmacology of glutamate transporters, EAATs and VGLUTs. Brain Res Rev 2004;45(3):250-65. [DOI] [PubMed]
- 3.Maragakis NJ, Rothstein JD. Glutamate transporters in neurologic disease. Arch Neurol 2001;58(3):365–70. [DOI] [PubMed]
- 4.Nau R, Prange HW, Muth P, Mahr G, Menck S, Kolenda H, et al. Passage of cefotaxime and ceftriaxone into cerebrospinal fluid of patients with uninflamed meninges. Antimicrob Agents Chemother 1993;37(7):1518-24. [DOI] [PMC free article] [PubMed]


