SUMMARY
SETTING
Training center on tuberculosis (TB) infection control (IC) for health care workers in the Central Asian Republics region.
OBJECTIVE
To assess the effects of TB IC training courses conducted at the Tuberculosis Infection Control Training Center in Machiton, Tajikistan.
DESIGN
Participants who participated in training (n = 89) during the first year of operation (April 2014–February 2015) were invited to participate in a post-training interview.
RESULTS
Of the 89 participants, 84 (94%) completed the interview and expressed satisfaction with the training. Eighty (95%) participants reported meeting with workplace leadership to discuss the training. Of these, 69 (85%) reported discussing changes required to meet TB IC standards. Self-reported changes in TB IC practices at work facilities post training included the creation of TB IC committees, designation of a TB IC focal person, TB IC planning, policies to separate infectious patients in waiting rooms, provision of masks for infectious patients, development of cough etiquette policies, improved glove availability, hand hygiene programs, and TB IC posters in waiting rooms.
CONCLUSIONS
Participant satisfaction and reported changes in TB IC activities illustrate the potential of these training courses to improve TB IC in the region. Future training courses may be tailored to specific audiences using a structured conceptual framework to impact administration, budgeting, and facilities management of TB IC practices.
Keywords: Tajikistan, TB, infection control, training, evaluation
THE CENTRAL ASIA REPUBLICS (CAR) region is composed of five independent countries that were once part of the former Soviet Union: Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, and Uzbekistan. Tuberculosis (TB) prevalence in this region is just under 200 cases per 100 000 population, ranging from 88 cases (Turkmenistan) to 196 cases (Kyrgyzstan) per 100 000.1 The emergence of multidrug-resistant TB (MDR-TB; i.e., TB resistant to at least isoniazid and rifampicin, the two most potent anti-tuberculosis drugs) has become a major concern in the region.2 Transmission of TB in health care facilities has contributed to the TB burden in the CAR region, and research suggests an occupational risk of TB for health care workers (HCWs),3–6 particularly in facilities where TB infection control (IC) practices are absent.6 Dramatic political and economic changes in Tajikistan since the 1990s have made investing in IC measures difficult, and led to a lack of institutional capacity to adequately address TB IC.
To develop human resources to strengthen TB IC practices in the region, Project Hope and the US Agency for International Development (USAID) teamed up with the Ministry of Health and Social Protection of Population Republic of Tajikistan (MoHSPPRT) to establish the Tuberculosis Infection Control Demonstration Site and Base for National Training (TB IC Training Center) at the National Center for Tuberculosis, Pulmonology and Thoracic Surgery in Machiton District, Tajikistan.7
A 4-day TB IC course was created in collaboration with the US Centers for Disease Control and Prevention (CDC) and the Vladimir TB Center in Russia. The training course included discussions, group and individual participant work, discussion, and demonstration sessions. Specific topics included TB IC hierarchy (administrative controls, environmental controls, and personal protection equipment) as well as TB IC planning, prioritization, advocacy, implementation, monitoring and evaluation. At the conclusion of the course, participants were expected to possess the knowledge and skills necessary 1) to identify and describe appropriate TB IC measures based on situational analysis, 2) to plan and design TB IC activities in accordance with national and international IC guidelines, and 3) to conduct monitoring and evaluation activities for TB IC programs (Appendix Table A*). In 2014, the Center conducted six training courses (one course for trainers and five cascade courses in which the initial group of trainees were the trainers) with participants from Tajikistan. A CAR regional training course was conducted in February 2015, with participants from Kazakhstan, Kyrgyzstan, Tajikistan, and Uzbekistan; the course has been included in this evaluation.
STUDY POPULATION AND METHODS
Study design and population
To assess the initial impact of the TB IC training, we conducted a cross-sectional post-training evaluation, with an average of 10 months between training completion and evaluation. The eligible study population included all 89 HCWs who attended at least one training course during the period April 2014–February 2015 at the TB IC Training Center at Machiton. Training participants were mailed an introductory letter describing the purpose of the evaluation and the timeframe during which they would be contacted by study staff to complete an interview. A standardized interview questionnaire was developed based upon the first two objectives of the training curriculum, which anticipated that by the end of the training participants would be able to 1) identify and describe appropriate TB IC measures, and 2) plan and design TB IC activities.
The questionnaire contained close-ended demographic questions, as well as questions to assess knowledge retention, sharing of training information, and changes implemented in TB IC practices at the participant’s workplace. Knowledge retention by participants was assessed using the same pre- and post-training knowledge test used for each training course. Knowledge scores were calculated for each participant as a percentage of questions with correct answers out of the total number of questions in the test. The questionnaire also included open-ended questions inviting participants to provide concluding comments or recommendations regarding the training center and program. Questions were written in English and translated into Russian and Tajik. The interview questionnaire was reviewed and approved by Project Hope and training center staff responsible for the development and conduct of the TB IC training.
Data collection
Interviews were primarily conducted in person in Russian or Tajik, based on the language preference of the participant, by trained interview staff. For participants unable to meet in person, interviews were conducted over the phone. Interview staff transcribed the participants’ responses into English for analysis.
Data analysis
Data were entered into an Epi Info™ database (Centers for Disease Control and Prevention, Atlanta, GA, USA) by trained staff and then reviewed and compared to the original study documents by the study coordinator for accuracy. Cumulative scores were calculated from items evaluating TB IC knowledge. Quantitative analyses, including descriptive statistics, were conducted in SAS (Statistical Analysis System, Cary, NC, USA). Thematic qualitative analysis was performed by two staff members identifying and comparing themes, with any discrepancies resolved by the study coordinator.
Ethics
The study received approval from the Regional Director Europe/Eurasia of Project Hope and from USAID, Washington DC, USA. The project was determined not to be human subject research by the US CDC and did not require approval by an institutional review board. Verbal informed consent was obtained from all participants before interviewing.
RESULTS
Participant characteristics and work facilities
At the time of evaluation, 89 HCWs had participated in a training course at the training center during its first year of operation. A total of 84 participants completed the interview (94% participation rate). Of the five participants not included in this evaluation, the contact information for two participants was incorrect, two participants refused to participate, and one participant terminated the interview early for reasons not clear to the interviewer.
Just under half (n = 35, 42%) of the participants reported a TB center or TB hospital as their current workplace (Table 1). Sixty (71%) participants had more than 4 years of work experience at their facility. Almost 70% of the participants reported having administrative responsibilities, and 24% reported budgeting responsibilities. Fifty-one participants (60%) reported the training course to be their first on TB IC.
Table 1.
Demographics and workplace information of evaluation participants (n = 84)
| Characteristic | n (%) |
|---|---|
| Sex | |
| Male | 38 (45) |
| Female | 46 (55) |
| Country | |
| Tajikistan | 81 (96) |
| Kyrgyzstan | 1 (2) |
| Kazakhstan | 2 (2) |
| Type of workplace | |
| TB center | 22 (26) |
| Public health center | 21 (25) |
| TB hospital | 13 (15) |
| Epidemiological center | 11 (13) |
| Health department | 4 (5) |
| Medical university | 4 (5) |
| Laboratory | 3 (4) |
| Penitentiary medical facility | 1 (1) |
| National hospital | 1 (1) |
| Other | 4 (5) |
| Time worked at facility, years (n = 82) | |
| <1 | 7 (8) |
| 1–3 | 16 (19) |
| 4–6 | 18 (21) |
| 7–10 | 10 (12) |
| >10 | 31 (37) |
| Administrative responsibilities | |
| Yes | 58 (69) |
| No | 26 (31) |
| Budgeting responsibilities | |
| Yes | 19 (23) |
| No | 65 (77) |
| Previous IC training | |
| This was the first training | 51 (60) |
| 1–2 other training courses | 19 (23) |
| ≥3 other training courses | 14 (17) |
Knowledge retention
TB IC knowledge scores improved from pre-training to immediate post-training across all training participants (Table 2), with an average absolute improvement of 48 percentage points at post-test. Compared to post-test scores, knowledge scores decreased by an average of 35 percentage points at the time of the evaluation. Training of trainer participants (trained in April 2014) demonstrated the highest mean knowledge retention scores of all training cohorts, with the last regional CAR cohort demonstrating the next highest mean knowledge retention scores.
Table 2.
Tuberculosis Infection Control Training Center pre- and post-test assessment scores and evaluation knowledge retention scores
| Pre-test* % | Post-test† % | Follow-up evaluation‡ % | |
|---|---|---|---|
| All training participants (2014–2015) | (n = 89) | (n = 89) | (n = 84) |
| Median [IQR] | 33 [22–56] | 89 [78–100] | 48 [36–67] |
| Mean | 38 | 86 | 51 |
| Mode | 22 | 100 | 64 |
| Training of trainers (17–14 April 2014) | (n = 15) | (n = 15) | (n = 12) |
| Median [IQR] | 50 [44–58.5] | 100 [89–100] | 77 [64–83] |
| Mean | 51 | 96 | 73 |
| Mode | 44 | 100 | 64 |
| Cascade training (24–26 June 2014) | (n = 12) | (n = 12) | (n = 12) |
| Median [IQR] | 22 [22–56] | 100 [83.5–100] | 50 [46.5–59] |
| Mean | 35 | 92 | 50 |
| Mode | 22 | 100 | 50 |
| Cascade training (6–8 August 2014) | (n = 13) | (n = 13) | (n = 13) |
| Median [IQR] | 22 [11–33] | 78 [67–89] | 39 [32–43] |
| Mean | 24 | 79 | 37 |
| Mode | 22 | 67 | 46 |
| Cascade training (20–22 August 2014) | (n = 11) | (n = 11) | (n = 11) |
| Median [IQR] | 11 [11–53] | 95 [80.8–100] | 38 [36–59.3] |
| Mean | 26 | 90 | 46 |
| Mode | 11 | 100 | 36 |
| Cascade training (17–19 September 2014) | (n = 12) | (n = 12) | (n = 12) |
| Median [IQR] | 39 [30.3–56] | 100 [89–100] | 40 [23.3–46] |
| Mean | 42 | 96 | 37 |
| Mode | 22 | 100 | 46 |
| Cascade training (22–24 September 2014) | (n = 13) | (n = 13) | (n = 13) |
| Median [IQR] | 33 [33–44] | 89 [83.5–89] | 61 [37.5–64.5] |
| Mean | 37 | 86 | 50 |
| Mode | 33 | 89 | 61 |
| CAR training (10–12 February 2015) | (n = 15) | (n = 12) | (n = 12) |
| Median [IQR] | 44 [33–72.5] | 78 [67–89] | 63 [41.3–77.8] |
| Mean | 47 | 76 | 59 |
| Mode | 33 | 89 | 43 |
Conducted immediately prior to TB IC training.
Conducted immediately following TB IC training.
Conducted 1–10 months after TB IC training.
IQR = interquartile range; CAR = Central Asian Republics; TB = tuberculosis; IC = infection control.
Sharing training information
Participants were asked if they shared the information they learned at the TB IC course upon returning to their work facility, as this may reflect retained knowledge and engagement in, and perceived value of, the training. Among the 84 participants, 80 (95%) reported meeting with their workplace leadership to discuss their experience at the training (Table 3). Of those, 69 (86%) reported that they had conveyed the need to make changes at their workplace to meet the TB IC standards they had learned during the training.
Table 3.
Training participant leadership meetings, facility changes discussed, and dissemination of training information among colleagues (n = 84)
| Activity | n (%) |
|---|---|
| When you returned from the IC course, did you meet with leaders in your workplace to discuss the training? | |
| Yes | 80 (95) |
| No | 4 (5) |
| During the meeting did you discuss the need to make changes in your workplace according to the information acquired? (n = 80) | |
| Yes | 69 (86) |
| No | 11 (14) |
| Have any of these changes been made? (n = 69) | |
| Yes | 16 (23) |
| No | 55 (77) |
| After the training, did you share what you learned with colleagues at your workplace? | |
| Yes | 83 (98) |
| No | 1 (2) |
| When you shared information, was this during informal conversations with co-workers or during formal presentations to a group? | |
| Informal conversations | 37 (45) |
| Formal presentations (e.g., meeting, lecture) | 46 (55) |
| Number of formal presentations given, median [IQR] | 2 [1–4] |
| Number of people who attended a formal presentation, median [IQR] | 22 [15–60] |
IC = infection control; IQR = interquartile range.
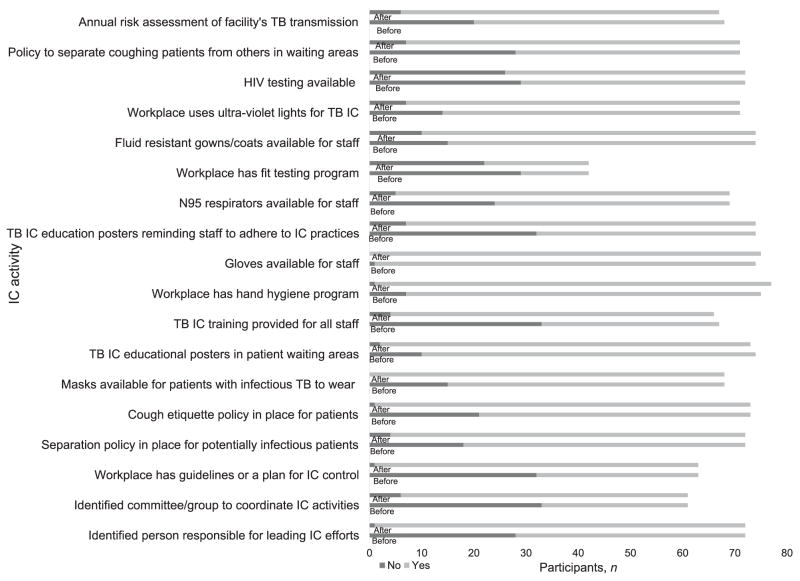
Changes in tuberculosis infection control practice
Participants were asked to describe IC practices at their work facility both before and after they attended the TB IC course. These questions aimed to demonstrate whether the TB IC course encouraged participants to plan and design TB IC activities at their work facility (Figure 1). Nine participants who identified themselves as not working in a facility providing laboratory or clinical services were not included in this analysis.
Figure 1.
Changes in facility TB IC practices before and after the TB IC training, as reported by participants. TB = tuberculosis; HIV = human immunodeficiency virus; IC = infection control.
The changes reported by participants varied, and included the organization of TB IC activities, changes in facility policies, and staff and patient education. The proportion of participants who reported that a designated staff member was leading IC activities at their facility increased from 28 (37%) before to 55 (73%) after the training. Twenty-eight (37%) participants reported a TB IC committee or group at their workplace before they attended the training compared with 55 (65%) after the training. Participants also reported increases in IC measures and activities at the time of evaluation in work facilities that had IC guidelines (n = 39, 52% before training vs. n = 70, 93% after training), offered TB IC training to all facility staff (n = 34, 45% before training vs. n = 62, 83% after training), and implemented a hand hygiene program (n = 67, 89% before training vs. n = 74, 99% after training). Smaller improvements in TB IC practices were observed in the use of personal protective equipment, environmental controls, and risk assessments. For example, 45 (60%) participants reported having N95 respirators available for staff at their work facility before the training compared to 66 (88%) after the training. While the availability of N95 respirators is important, so is fit-testing these respirators: only 13 (17%) participants reported having a fit-testing program for staff before the training. During the evaluation, this improved slightly to 20 (27%) participants reporting a fit-test program. Glove availability also increased after training (n = 73, 97% vs. n = 75, 100%). Finally, the number of participants conducting annual risk assessments of TB transmission at their workplace increased after training from 48 (64%) before to 61 (81%) after.
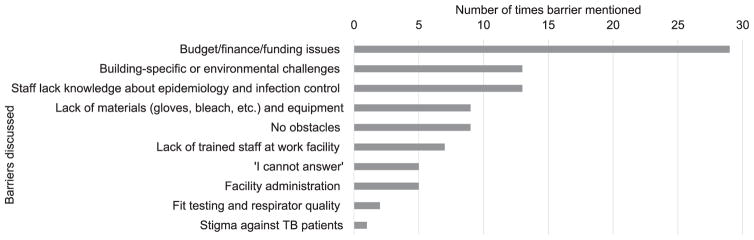
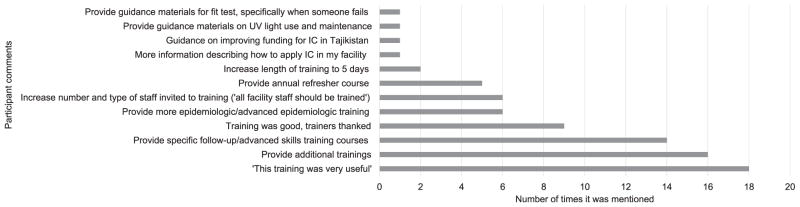
Barriers to implementation of tuberculosis infection control and recommendations for training improvement
Participants discussed barriers they had experienced initiating or implementing IC practices at their work facilities following the TB IC training (Figure 2). Among the participants who responded to these questions, the most frequently mentioned barrier was related to budget, finance, and funding (n = 29, 35%) for IC activities, followed by environmental challenges (n = 13, 14%), and lack of staff knowledge of TB IC (n = 13, 14%). The top three suggestions for improving TB IC training included providing additional TB IC training (n = 16, 30%), advanced skills and refresher training (n = 14, 26%), and expanding the type of staff invited to training courses (n = 6, 11%) (Figure 3).
Figure 2.
Participant identified barriers to implementing IC. TB = tuberculosis; IC = infection control.
Figure 3.
Participants’ comments and suggestions for improvement. UV = ultrviolet; IC = infection control.
Participant satisfaction
In response to a question asking participants for final comments or their overall perception of the training courses, participants reported being generally satisfied with the TB IC training provided by the training center and a desire to attend additional training courses in the future. Twenty-seven participants (39%) reported that the training was useful or good; another eight (10%) requested that this training be offered to work colleagues and/or all medical staff working in facilities; and five (6%) reported wanting more training courses offered. All interviewed participants (100%) also agreed that they would be interested in attending additional courses if invited by the training center.
DISCUSSION
This evaluation sought to assess participants’ knowledge retention, sharing of training information, and changes in IC activities at participants’ workplaces following TB IC training courses conducted during the first year of operation of the TB IC National Training Center. Findings from this evaluation illustrate the potential for such courses in reducing nosocomial transmission of TB in the CAR region. This has important implications in a setting where MDR-TB rates are some of the highest globally,2 and where infection rates and prevalence of TB disease in HCWs are not well studied or documented.
An important aim of these courses was to effect positive change in TB IC practices. Results suggest that participants were motivated to return to their work facility and engage with facility leadership and work colleagues to share their knowledge about TB IC principles and practices, and potential improvements within their physical work facilities. The training also appears to have had a positive impact on TB IC practices in the participants’ workplaces, particularly with regard to increased uptake of administrative controls.
This evaluation also identified opportunities to improve the TB IC training courses provided at Machiton. For example, participants noted that limited financial resources hindered the expansion of TB IC practices. Given that one quarter of the participants reported responsibility with budgeting at their work place and that 77% reported that no TB IC changes were made in their work facility after discussing needed changes with facility leadership, it may be beneficial to create a TB IC course specifically aimed at facility leadership to increase knowledge and awareness of TB IC, budgeting needs, and innovative TB IC possibilities. Moreover, expanding training invitations to include staff from all departments, including administration and facilities maintenance, and tailoring training content to these professionals’ work responsibilities, may increase TB IC awareness and engagement throughout health facilities. Participants’ limited knowledge retention of TB IC principles and practices observed during the evaluation indicate the potential advantage of tailored training courses. While some regression in knowledge scores over time is expected,8 the average decrease of 35 percentage points may reflect a lack of information utility. Training participants were primarily care providers and epidemiologists, with more than half (60%) of participants receiving their first exposure to TB IC principles during the training. The knowledge questions most frequently missed were those focusing on technical concepts and environmental and/or engineering interventions required, which are not part of the routine work of these professionals.
Future directions
Future TB IC training curriculums should be developed using behavioral theory and mapped to evaluation conceptual frameworks to ensure rigor and replicability. Curriculums may also benefit from the inclusion of a module dedicated to participants’ development of a TB IC action plan with short-, mid-, and long-range goals for their workplaces.9,10 The module could guide participants to broaden the type of staff with whom they share TB IC messages and information, to tailor the plan to facility-specific needs, to identify accountable facility-specific persons responsible for tasks and activities, to outline time-frames for task and activity completion, and to address potential implementation barriers. Furthermore, the creation of a TB IC peer network program along with the provision of didactic courses may enable participants to remain connected, both to the training center and to each other, after a course is finished, without requiring time and travel for additional training. A formalized peer network would provide a platform for participants to share experiences, brainstorm and problem solve together, and provide motivational support with each other despite physical distance.
Limitations
This evaluation is subject to several limitations. First, the evaluation focuses on the first year of training operations. The majority of training center participants and evaluation respondents were from Tajikistan. Responses and findings may thus be more reflective of this country and into not the CAR region as a whole. Although generalizability may be limited, this is the first training program evaluation conducted in the CAR region. Greater insights into participant competencies post-training and into training impact may be acquired through the use of a structured conceptual framework to guide the planning, implementation, and evaluation of future training. Participants may have provided socially acceptable answers rather than providing a constructive critique of the training they attended.11 Finally, this evaluation collected self-reported changes in TB IC practices from participants, which are subject to both recall and social desirability bias.11
CONCLUSIONS
Training participants self-reported disseminating the TB IC training information to colleagues at their work facilities and positive changes in TB IC practices, particularly administrative controls. As the TB IC demonstration site in Machiton continues to provide TB IC training for the CAR region, the content of future training courses may be tailored to the job responsibilities of course participants, and expanded to guide participants in planning for change at their workplaces. The target audience of TB IC training may also be expanded to include administrators and facilities maintenance staff. A structured conceptual framework should be used to guide these changes to the curriculum.
Acknowledgments
The authors would like to thank the former head of Machiton Hospital, S Rustamov; the NTP Tajikistan Manager, O Bobokhojaev; the Deputy Minister of Health, Tajikistan; and N Jafarov for their support of TB IC; all of the training participants who contributed to this evaluation; G Blackwelder from the US Centers for Disease Control and Prevention (CDC), G Volchenkov from the Vladimir oblast TB Center, and A Mirzoyan, the Global Fund to fight AIDS, Tuberculosis and Malaria (the Global Fund) portfolio manager for supporting Project Hope and TB IC training efforts in Tajikistan.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US CDC or of the US Agency for International Development (USAID). This was a collaborative evaluation study by Project Hope and CDC.
This project was funded by USAID. The demonstration site and training center is operated by Project Hope and housed directly under the USAID/TB CARE II project in Tajikistan. Funding for telemedicine conference equipment was provided by the Global Fund. The evaluation of this demonstration site and training center was supported by Project Hope and the CDC.
Conflicts of interest: None of the authors have a commercial or other financial interest associated with the information presented in this manuscript. References in this manuscript to any specific commercial products, process, service, manufacturer, or company does not constitute its endorsement or recommendation by the US Government, USAID, or CDC. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the CDC or USAID.
APPENDIX
Table A.
Curriculum of the TB IC training conducted at the TB Infection Control Demonstration Site and Base for National Training at the National Tuberculosis Center, Pulmonology and Thoracic Surgery, Machiton District, Tajikistan
| Framework used to guide the training: WHO policy on infection control in health-care facilities, congregate settings and households Training objectives:
|
| Domain | Training topics and content | Presentation format | |
|---|---|---|---|
| Introduction | Topic: Overview of TB control Contents: |
|
|
|
|
||
| Topic: Basics of TB infection and transmission Contents: |
|||
|
|
||
| Topic: TB IC: the hierarchy/package of interventions Contents: |
|||
|
|
||
| Managerial activities: actions considered to be essential for the effective implementation of TB IC measures | Topic: Managerial activities Contents: |
|
|
|
|
||
| Topic: TB IC implementation framework Contents: |
|||
|
Case study: Risk assessment | ||
| Administrative controls: policies, procedures, and enforcement measures to prevent exposure to disease-causing organisms | Topic: Administrative controls Contents: |
|
|
|
|
||
| Topic: Case study: Rwanda Contents:
|
|||
| Topic: TB IC facility plans Contents: |
|||
|
|
||
| Environmental controls: measures to prevent the spread and reduce the concentration of infectious droplet nuclei | Topic: Environmental (engineering) Controls—Introduction
|
Contents:
|
|
| Topic: Environmental (engineering) controls—ventilation Contents: |
|||
|
|
||
| Topic: Environmental (engineering) controls—UVGI Contents: |
|||
|
|
||
| Topic: Environmental (engineering) controls—filters and RACs Contents: |
|||
|
|
||
| Topic: Biosafety in the TB laboratory Contents: |
|||
|
|
||
| Respiratory protection controls: the use of personal protective equipment to reduce risk for exposure to infectious droplet nuclei that have been expelled into the air from a patient with infectious TB disease | Topic: Basic components of infection control Contents: |
|
|
|
|
||
| Topic: Personal respiratory protection Contents: |
|||
|
|
||
| Topic: Respirator fit testing Contents: |
|||
|
|
||
TB = tuberculosis; IC = infection control; WHO = World Health Organization; HIV = human immunodeficiency virus; MDR-TB = multidrug-resistant TB; HCW = health care worker; UVGI = ultraviolet germicidal irradiation; RAC = room air cleaner.
Footnotes
The appendix is available in the online version of this article, at http://www.ingentaconnect.com/content/iuatld/ijtld/2017/00000021/00000005/art00017
References
- 1.World Health Organization. Global tuberculosis control, 2015. Geneva, Switzerland: WHO; 2015. WHO/HTM/TB/2015.22. [Google Scholar]
- 2.World Health Organization. Multidrug and extensively drug-resistant TB (M/XDR-TB) 2010 global report on surveillance and response. Geneva, Switzerland: WHO; 2010. [Accessed January 2017]. WHO/HTM/TB/2010.3. http://whqlibdoc.who.int/publications/2010/9789241599191_eng.pdf. [Google Scholar]
- 3.Joshi R, Reingold AL, Menzies D, Pai M. Tuberculosis among health-care workers in low- and middle-income countries: a systematic review. PLOS MED. 2006;3:e494. doi: 10.1371/journal.pmed.0030494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fennelly KP, Iseman MD. Health care workers and tuberculosis: the battle of a century. Int J Tuberc Lung Dis. 1999;3:363–364. [PubMed] [Google Scholar]
- 5.Pearson ML, Jereb JA, Frieden TR, et al. Nosocomial transmission of multidrug-resistant Mycobacterium tuberculosis A risk to patients and health care workers. Ann Intern Med. 1992;117:191–196. doi: 10.7326/0003-4819-117-3-191. [DOI] [PubMed] [Google Scholar]
- 6.Roth VR, Garrett DO, Laserson KF, et al. A multicenter evaluation of tuberculin skin test positivity and conversion among health care workers in Brazilian hospitals. Int J Tuberc Lung Dis. 2005;9:1335–1342. [PubMed] [Google Scholar]
- 7.Trusov A, Ismoilova J, Tonkel T, Aleksandrin A. Infection prevention and control in TB programs. Health Aff (Millwood) 2016;35:556. doi: 10.1377/hlthaff.2016.0050. [DOI] [PubMed] [Google Scholar]
- 8.McKenna SP, Glendon AI. Occupational first aid training: decay in cardiopulmonary resuscitation (CPR) skills. J Occup Psychol. 1985;58:109–117. [Google Scholar]
- 9.Pan American Health Organization. Final Report of the International Workshop on Tuberculosis Control in Prisons; San Pedro Sula, Honduras. 11–13 August 2003; Washington DC, USA: PAHO; 2003. [Accessed January 2017]. http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=21848&Itemid. [Google Scholar]
- 10.Mangan JM, Arias M, Sierra T, et al. Evaluating the strengths and weaknesses of tuberculosis educational activities for prisoners in Honduras. Int J Tuberc Lung Dis. 2006;10:1152–1158. [PubMed] [Google Scholar]
- 11.Malham PB, Saucier G. The conceptual link between social desirability and cultural normativity. Int J Psychol. 2016;51:474–480. doi: 10.1002/ijop.12261. [DOI] [PubMed] [Google Scholar]