Abstract
Purpose
The purpose of this article is to evaluate optic nerve head (ONH) characteristics in an ethnically diverse cohort of young U.S. adults.
Methods
In this study, 409 myopes and 206 nonmyopes (median age 22 years) completed measures including biometry and spectral domain optical coherence tomography from enface (ovality and torsion) and cross-sectional (tilt and crescent width) scans. Associated factors were evaluated using multivariable models.
Results
In myopic versus nonmyopic right eyes, median tilt (6.0° vs. 2.4°; P < 0.0001) and frequency of crescents (49% vs. 10%; P < 0.0001) were higher in myopes. Right eyes with crescents had higher median tilts (8.8° [myopic], 9.0° [nonmyopic]) than those without crescent (2.5° [myopic], 2.1° [nonmyopic]), irrespective of refractive group (both P < 0.0001). Torsion was similar between groups, with a slight difference in ovality (0.89 vs. 0.91; P < 0.03). Data in the left eyes were similar, and modeling was done only for the right myopic eyes. Multivariable models showed that an increased tilt was associated with ethnicity (P < 0.001), the presence of crescent (P < 0.001), and smaller ONH diameter (P < 0.0031), with interactions between ethnicity and crescent (P = 0.002). Specifically, ONH tilt was significantly higher in Asian eyes without crescent (P < 0.0001 for all comparisons), and crescent width was associated with increased tilt in non-Asian eyes (P < 0.02). Crescent width was associated with ethnicity (greatest in Asians) and disc tilt. Interactions were observed between tilt and ethnicity, whereby tilt had a greater effect on crescent width in non-Asian eyes, and crescent width was associated with increased tilt in non-Asian eyes.
Conclusions
The data clarify the influence of ethnicity and myopia on ONH characteristics in young adults and may inform future studies of biomechanical properties or of retinal pathology of the myopic eye.
Keywords: myopia, optical coherence tomography, optic nerve head
The significance of examining anatomical changes in the peripapillary region in a multi-ethnic group of young adults is driven by the increasing prevalence of myopia1 and the susceptibility of this region to early complications from excessive axial elongation.2 In the United States, 42% of adults are myopic (a 66% increase over the past 4 decades).3 In Asian countries, 83% of adults aged 25 to 75 years are projected to be myopic by 2040, with approximately 15% of these adults having high amounts.4 Myopic eyes have a prolate shape, sometimes exhibit staphyloma formation at the posterior pole, and often develop changes in the shape of the optic nerve head (ONH).2,4 These changes are consistent with recent biomechanical theories proposing that stress imposed by the intraocular pressure (IOP) is concentrated around the scleral opening and predicting that tissue strain will be most evident around the ONH.5–7 The expected increases in myopia and the difficulty teasing out the pathophysiology of the myopia itself from its effects on age-related conditions such as glaucoma8 combine to create a significant diagnostic, management, and public health dilemma. Understanding the ONH characteristics of a multi-ethnic group of young adults measured before the onset of ocular disease is likely is a necessary first step toward understanding deviations from normal that might signal disease onset.
The two most common, clinically observed peripapillary changes associated with excessive axial elongation and myopia are tilting of the ONH and crescent formation.2,9,10 Tilt has traditionally been observed clinically using binocular indirect ophthalmoscopy or stereo-paired photographs that allow a three-dimensional (3D) perception, without objective quantification of tilt in the z plane (“cross-sectional”). Myopic crescents are identified with the same techniques and appear as whitish areas adjacent to the ONH, where the sclera can be viewed directly due to a loss of the deep layers of the retina.11 A large study of Asian children demonstrated that tilt and crescent affect 37% and 66.5% as early as age 12 to 16 years.10
A more quantitative strategy that serves as a proxy for measurement of tilt is to calculate the ovality ratio (a ratio comparing the long and short diameters of the ONH). Using this technique, more oval ONHs have been associated with increasing myopia and/or axial length12–15 as well as an altered pattern of retinal nerve fiber layer (RNFL) thickness.15–17 Recently, optical coherence tomography (OCT) has allowed direct measures of ONH cross-sectional tilt, which is expected to be more precise than inferred tilt from an ovality ratio. A comparison of the techniques indicates that measures of tilt and ovality are not interchangeable, given the low to moderate correlation (0.2818 and 0.4819) in the few studies that reported both. However, OCT studies have also shown increased tilt to be associated with increased axial length and myopia17–20 as well as visual field loss in glaucoma patients.19
Additional characteristics of ONH structure have also shown associations with ocular pathology. For example, torsion (deviation of the long axis of the ONH from a vertical reference) has been associated with an increased risk of visual field loss14,21 or with the location of visual field loss in Korean adults with normal tension glaucoma.13,14,22 Beta peripapillary atrophy (BPPA), which until recently has not been differentiated from myopic crescent,23 has been related to axial elongation and myopia10,24,25 as well as an increased risk of visual field loss in glaucoma patients.26–28
Most prior OCT studies evaluating the optic disc have been conducted in homogeneous Asian populations, and many have been conducted in older adults or glaucoma patients. Therefore, little is known about myopia-related changes in the ONH of young adults of different ethnicities living in the United States. Because no standardized measurement of tilt has been used across studies, it is difficult to know the degree to which emerging findings relating ONH characteristics to the development of myopic or other pathologies may be influenced by age, race/ethnicity, or disease status or to the methodological differences between studies.
The purpose of this study was to evaluate ONH characteristics (tilt, crescent width, ovality, and torsion) in a large, ethnically diverse group of myopic and nonmyopic young adults without ophthalmoscopically apparent (nonmyopic) ocular pathology. In addition, we examined factors (e.g., sex, race/ethnicity, myopia status, axial length, disc diameter, central corneal thickness, IOP) that might be associated with tilt or crescent formation.
Methods
The Correction of Myopia Evaluation Trial (COMET) study design29 and main treatment outcomes30,31 have been described previously. The COMET study initially investigated progressive addition lenses as a treatment for myopia and later became a longitudinal observational study of factors associated with the progression and stabilization of myopia. A nonmyopic group of age-, sex-, and ethnicity-matched adults was recruited in year 12 to provide anatomical/structural comparisons.
Participants
A total of 409 myopes (85% of the original COMET cohort, with spherical equivalent myopia from −1.25 to −4.5029 in study year 1) and 206 matched nonmyopic participants completed the study protocol at the four study sites (optometry schools/colleges in Birmingham, AL, USA; Boston, MA, USA; Houston, TX, USA; and Philadelphia, PA, USA). The study conformed to the Declaration of Helsinki, and the research was approved by the institutional review boards at each participating center. Written informed consent was obtained from all participants.
Study Procedures
Refractive error (ARK-700A; Nidek, Japan) and axial length (AL; A-2500; Sonomed, Lake Success, New York, USA) were measured 30 minutes after cyclopegia (two drops of 1% tropicamide).29 Additional measurements taken in myopes at the 11- to 14-year study visits included: OCT imaging, intraocular pressure (IOP; Goldman applanation tonometry), and central corneal thickness (CCT; Pachmate DGH55, Exton, PA, USA). IOP and CCT have been described previously.32 During the 12-year visits, nonmyopes (spherical equivalent between plano and +2.00 D in both eyes) were evaluated according to the same study protocol used for the myopes. Our study was not designed to evaluate other myopia-related ocular pathologies because the protocol did not include methods to standardize such reporting.
OCT Imaging
OCT images were obtained with the RTVue (Model RT-100; Optovue, Inc., Fremont, CA, USA), a Fourier (or Spectral) Domain device that captures 26,000 A scans/second (depth resolution of 5 μm; scanning laser diode with a wavelength of 840 nm). The optic nerve head (ONH) scan consists of 12 radii, each 3.40-mm long, centered on the disc, with a resolution of 7.5 μm in each orientation (RT-100 user's manual). Images were taken before cycloplegia with contact lenses removed. At each visit for the myopes and at the single visit for the nonmyopes, one 3D disc (for registration and en face measurements) and three ONH scans (for cross-sectional measurements) were taken. Scans were retaken if poor alignment, low signal strength (signal strength index < 50), blinks (black lines across the image), or motion artifacts (shearing or breaks of the vessel pattern) were noticed.33
Analysis of OCT Image Quality
All scans (four per eye) were evaluated for quality using offline Optovue software (version A.6.10.100.22; Optovue, Inc.). E.H. or W.M.T. evaluated half of the scan sets for quality. For myopes, the earliest 3D disc scan passing review was selected. Disc margins were manually corrected to exclude any crescent. ONH scans were excluded if signal strength index was < 40 (slightly lower values could be used due to availability of multiple scans), scans were decentered, or “clipped” (due to z axis offset or misalignment of the camera), or if the signal intensity was poor in the measurement area. The most tilted radius was selected by a visual inspection of the six cross-sectional radii. Either grader could initiate an adjudication process to decide whether to include or discard scans. After image quality review, and elimination of participants with pathology or refractive surgery, 97% (398/406) of myopes and 90% (187/206) of nonmyopes had at least two high-quality, usable ONH scans (Fig. 1).
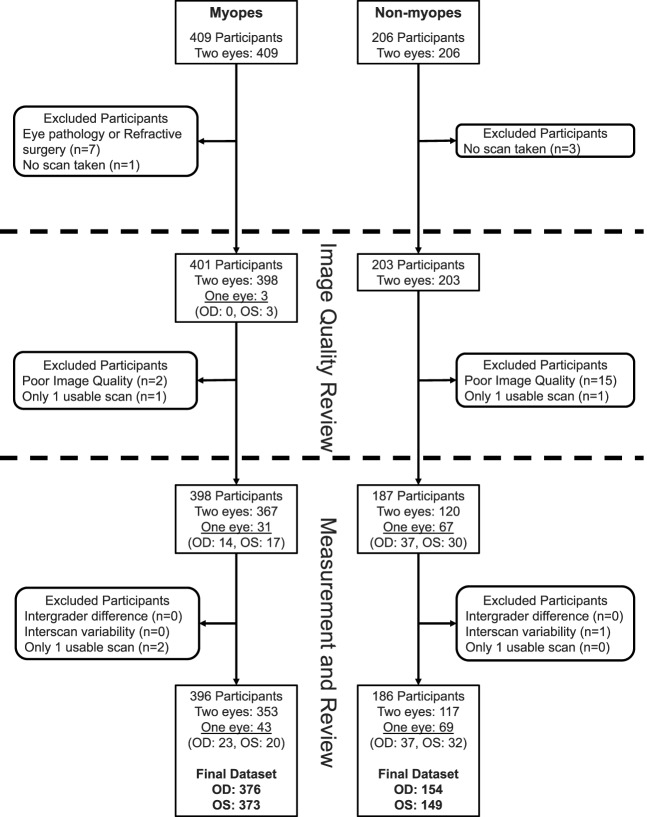
Figure 1.
Flowchart showing the status of participants and eyes after each step of scan review. Among 409 myopes, 8 were removed due to eye pathology (including buried drusen, suspected glaucoma, keratoconus, retinal detachment, and traumatic aphakia), refractive surgery, or lack of scans. Image quality review step: Scans were reviewed for quality in 401 participants, and scans for 3 participants were lost due to poor images or insufficient numbers of remaining scans. Measurement and review step: Measures were taken in both eyes of 367 participants, and either the right eye (OD) (n = 14) or left eye (OS) (n = 17) in the rest. Two participants were removed due to insufficient remaining scans, leaving 396 participants (353 with measures from both eyes, 23 with OD only, and 20 with left eye only). In the final dataset for myopic eyes, measurements were available for 376 (353 + 23) right eyes and 373 (353 + 20) left eyes. Among 206 nonmyopes, 3 participants were excluded because no scans were taken. Image quality review step: 15 nonmyopic participants were excluded due to poor image quality (3D disc scan did not pass review). One additional participant was lost due to an insufficient number of ONH scans. Measurement and review step: Measures were taken in both eyes of 120 nonmyopic participants, and either the OD (n = 37) or OS (n = 30) in the rest. One participant was removed due to high variability in the three ONH scans measured per eye, leaving 186 nonmyopic participants (117 with measures from both eyes, 37 with OD only, and 32 with left eye only). In the final dataset for nonmyopic eyes, measurements were available for 154 (117 + 37) right eyes and 149 (117 + 32) left eyes.
Measurement of Tilt and Crescent
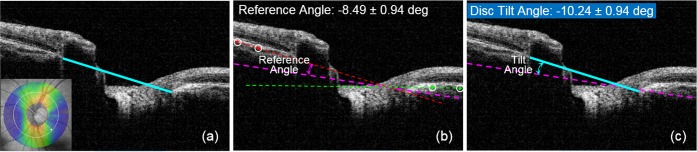
Disc tilt was defined as the angle in degrees between two line segments, one connecting two landmarks on either side of the optic disc opening (ONH landmarks; Fig. 2a), and a reference line determined by the outermost visible portions of the retinal pigment epithelium (RPE) on either side of the disc (Fig. 2b). The reference line (Fig. 2c) bisected the angle between the two RPE lines. This method was developed for the current study because it used more data points to construct the reference line versus using only the Bruch's membrane opening19,20 and because the RPE nearest the neural canal opening may bow backward.28,34 The final tilt angle was measured between the ONH landmarks and the reference lines (Fig. 2c). The orientation of maximum tilt was defined as the clock hour of the most depressed part of the optic disc, determined by visual inspection of the cross-sectional radii, referenced to the en face image.
Figure 2.
(a) Example RTVue ONH scan from the left eye of a myopic participant aged 20.2 years with spherical equivalent –11.78 D and axial length 27.85 mm. The first line segment used to define disc tilt is shown in blue. The landmarks were manually located and correspond to Bruch's membrane opening (nasal; left) or the innermost edge of the anterior scleral canal (temporal; right) in the eye with externally oblique border tissue.35,36 The insert shows the radius (white arrow) used to produce the B scan. Tilt orientation is defined as 4:30 (inferior, temporal), the clock hour that corresponds to the most posterior or depressed part of the optic disc for this left eye. (b) A reference line (dashed magenta) was derived to correct for scan tilt and bisects the angles between the retinal pigment epithelium (RPE) landmark lines (dotted red and green lines), which were drawn using landmarks placed along the visible RPE surface on either side of the optic nerve (encircled red and green dots). The first RPE dot was located near the limits of the measurement window and the second was chosen to select a representative line segment that was not affected by backward bowing of the RPE. Bisecting the RPE angle provided an average correction for scan tilt (−8.49° in this sample scan), evident here by the differences in height of the RPE surface on opposite sides of the image. (c) The final disc tilt angle is calculated by the custom Matlab program as the angle between the dashed magenta reference line and the solid blue line spanning the anterior scleral canal (−10.24 degrees in the left eye).
The disc margin landmarks corresponded to Bruch's membrane opening in areas without crescent or to the innermost termination of the externally oblique border tissue in areas with crescent (Fig. 3).35,36 Myopic crescent was identified as an area adjacent to the ONH lacking an intact RPE/Bruch's membrane layer (RPE/BM), with increased signal intensity from the underlying sclera, located between the termination of the RPE and the disc margin.23,28,37,38 ONH scans that were previously determined to have a crescent required the grader to locate the termination of the RPE/BM using the same cross-sectional scan chosen for tilt measures. The linear distance between the termination of the RPE/BM and the disc margin (crescent width) was calculated.
Figure 3.
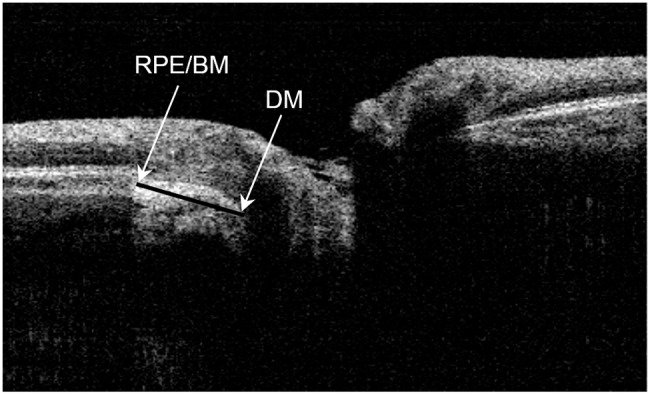
Example RTVue ONH scan from the right eye of a myopic participant aged 24 years with spherical equivalent −5.50D D. axial length 24.92 mm, and a crescent (identified by the increased signal density from the underlying sclera in the crescent between the termination of the RPE/Bruch's membrane complex (RPE/BM) and the disc margin (DM) found at the innermost termination of the externally oblique border tissue canal.
Independent measures of disc tilt and crescent width were performed by each grader for all scans using a custom Matlab program (Lei Liu, PhD, University of Alabama School of Optometry, Birmingham, AL, USA) to semiautomate the process that included steps for the randomization of image order and masking. For each scan, the grader located the necessary landmarks three times. The program averaged the three positions of each landmark, drew the necessary line segments, and computed the reference and the final tilt angle for each scan and crescent width if present. All values were output for centralized data processing and analysis.
Assessment of Intergrader Agreement
Scans with intergrader differences in landmark location >57.8 μm (cutoff based on pilot data analyses) were reviewed and remeasured by one or both graders. The resulting mean intergrader differences (± SD) were smallest for the nasal landmarks when compared with the temporal and crescent landmarks (nasal, 19.1 ± 12.6 μm and 19.8 ± 12.6 μm; temporal, 24.2 ± 14.4 μm and 21.7 ± 13.1 μm; crescent, 30.9 ± 14.6 μm and 27.7 ± 13.8 μm for myopic and nonmyopic eyes, respectively). Inconsequential differences in temporal landmark location occurred between graders for myopes versus nonmyopes (2.6 ± 14.1 μm; P < 0.0001) and for myopic eyes with crescent versus without crescent (2.7 ± 14.4 μm; P < 0.0001). For crescent width, the median intergrader differences ranged from 3.97 to 16.64 μm for myopic and nonmyopic right and left eyes, with 95% of measures agreeing within < 46.44 μm. The intergrader intraclass correlation for crescent width was 0.98 (95% confidence interval [CI] 0.92–1.00).
Scan sets with an absolute intergrader difference >4° in tilt or 1.5 clock hours in location of radii (cutoffs based on pilot data analyses) were then reviewed for possible deletion or remeasurement. The resulting median intergrader differences in tilt ranged from 0.08 to 0.17° for myopic and nonmyopic right and left eyes, with 95% of measures agreeing within 2°. The intergrader intraclass correlation for tilt was 0.98 (95% CI 0.93–1.00) and 95% of measures differed by < 2°.
The final dataset included all eyes with tilt measures that passed review (Fig. 1). Among eyes with crescents, no valid measure was possible for 17 myopes and 3 nonmyopes, most often because landmarks were ambiguous for purposes of measuring crescent width. Measures of crescent width were excluded from an additional three myopes due to insufficient scans remaining after the measurement agreement process was completed. Because of the small intergrader differences, the final measures of disc tilt and crescent width were based on an average of the final values from both graders.
Measurement of Disc Ovality and Torsion
The disc ovality ratio (shortest:longest diameter) was determined objectively using a custom Matlab program that batch processed the en face images and determined the best fitting elliptical shape (lowest mean squared error) compared to the disc margin determined previously. The program also objectively determined torsion (rotation in degrees of the long diameter from vertical) with clockwise assigned a positive value (Fig. 4). Images whose elliptical fits had a mean squared error of 0.35 or greater were excluded. After scan sets with high interscan variability for ovality (n = 14) or torsion (n = 22 among scans with ovality < 0.90) were reviewed, ovality results were available for 99.8% (581/582) of participants and torsion results available for 99.5% (413/415) of participants.
Figure 4.
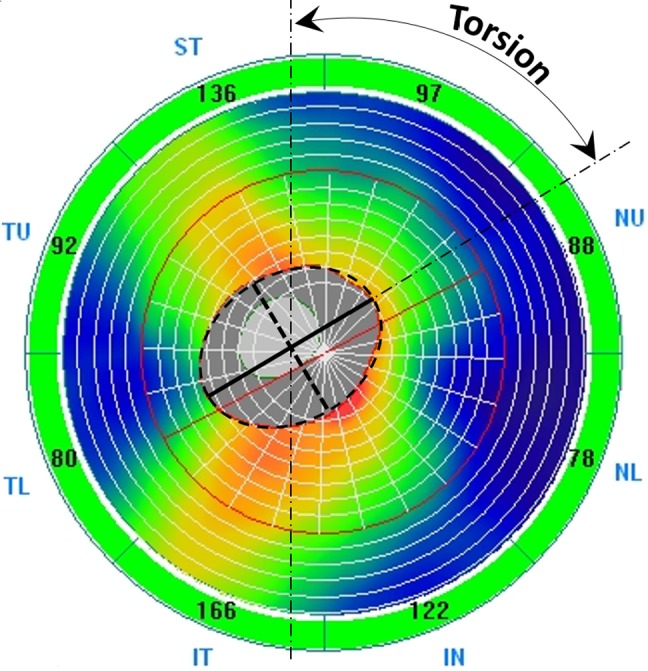
A sample en face thickness map of the optic disc (darker gray oval) from the RTVue ONH scan. The dotted black outline is the fitted ellipse automatically generated by the custom Matlab program. The dotted line inside the optic disc is the minor (short) axis, and the solid black line is the major (long) axis of the fitted ellipse. Torsion was automatically determined by the custom Matlab program as the deviation in degrees of the long axis from the vertical.
Statistical Analysis
To allow for visual comparison of the magnitude and orientation of the measured ONH characteristics and to evaluate symmetry between the right and left eyes, the distribution of median tilt and crescent width within each clock hour of the disc are presented for the right and left eyes in myopes and nonmyopes separately. Comparisons between myopes and nonmyopes were conducted using two-sample t-tests or Wilcoxon rank sum tests for continuous variables and χ2 tests for categorical variables, separately for the right and left eyes. To determine the cut point for the degree of tilt at which the crescent was most likely to be identified, a nonparametric method involving the kernel function to smooth the cumulative distribution function was used. This method estimated the optimal degree of tilt by maximizing the summation of sensitivity and specificity (i.e., Youden Index).
A log-transformed, γ regression model39 was used to evaluate factors associated with disc tilt in myopes (right eye data were used, based on initial analyses indicating that right and left eye data had no important differences that would affect the modeling) due to the high degree of skewness in its distribution. For myopic eyes with crescent, a Tobit model40 was used for crescent width to adjust for truncated values. Age, sex, ethnicity, disc diameter, axial length, IOP, CCT, torsion degree (absolute value), and torsion direction (clockwise/counterclockwise) were evaluated as potential covariates for inclusion in the models in a univariate screen. Visual acuity was not evaluated for associations with tilt or crescent given the narrow range among the participants. Factors with associations of P < 0.10 based on the Wilcoxon rank sum and Kruskal–Wallis (for categorical variables) and Spearman correlation (for continuous variables) were included in the final multivariable models. Disc tilt, crescent (presence/absence), and crescent width (only for eyes with crescents) were also screened for possible inclusion in the final model. For both models, all two-way interactions between covariates were evaluated and only significant interactions were retained. Disc tilt/crescent width results were estimated as adjusted means for each categorical variable and adjusted regression coefficients for continuous variables. In the γ model, because of the log transformation, adjusted means or adjusted regression coefficients were compared between factor categories (e.g., between Asian and White participants) using ratios of means or coefficients instead of absolute differences. For the Tobit model, factor categories were compared using differences between the adjusted means or regression coefficients and F tests based on the regression models.
All statistical analyses were performed using SAS v9.4 (SAS Institute, Cary, NC, USA). Specifically, the γ regression model was fit using the GENMOD procedure with the specified distribution of γ and the logarithm link function, and the Tobit model was fit using the LIFEREG procedure. To account for the multiple pairwise group comparisons in multivariable analyses, P values were adjusted by the Bonferroni method.
Results
Two or three high-quality scans for tilt measures were available for at least one eye in 396 (98.8%) of myopic and 186 (91.6%) of nonmyopic participants with OCT data (Fig. 1). Myopic and nonmyopic participants were similar in mean age (21.9 + 1.3 years), with good representation of females (54.5% vs. 54.3%) and African Americans (27.0% vs. 26.9%) in both groups, respectively (Table 1). As expected, myopic eyes were significantly longer and had more negative spherical equivalent (both P values < 0.0001). No differences were found in IOP or CCT between myopic and nonmyopic eyes.
Table 1.
Characteristics of Myopes and Nonmyopes
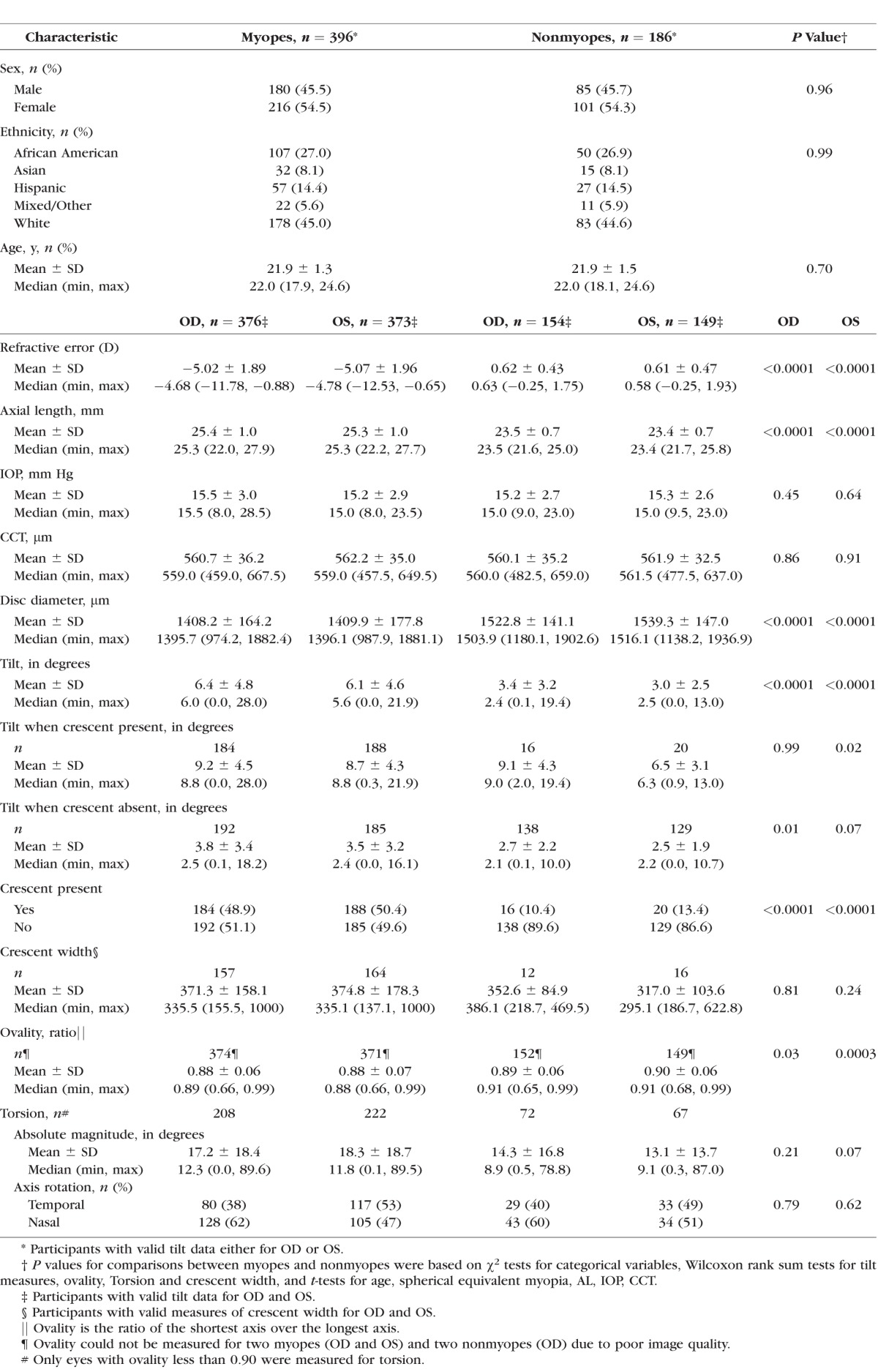
ONH Characteristics in Myopic Versus Nonmyopic Eyes (Table 1)
Tilt.
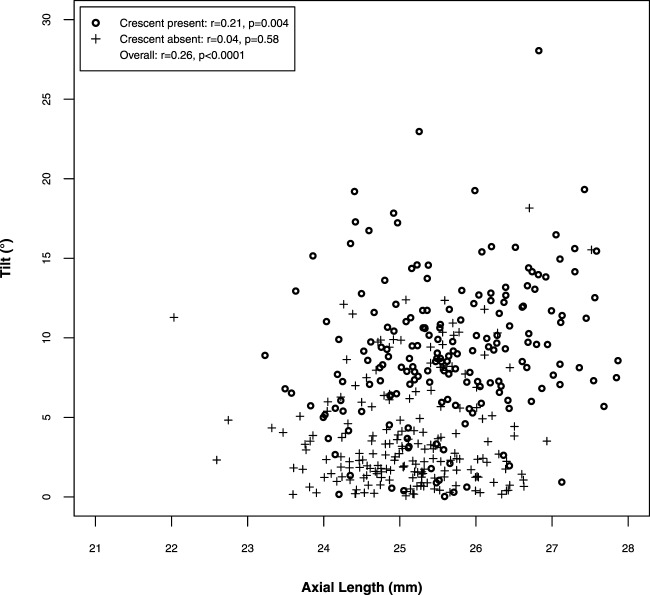
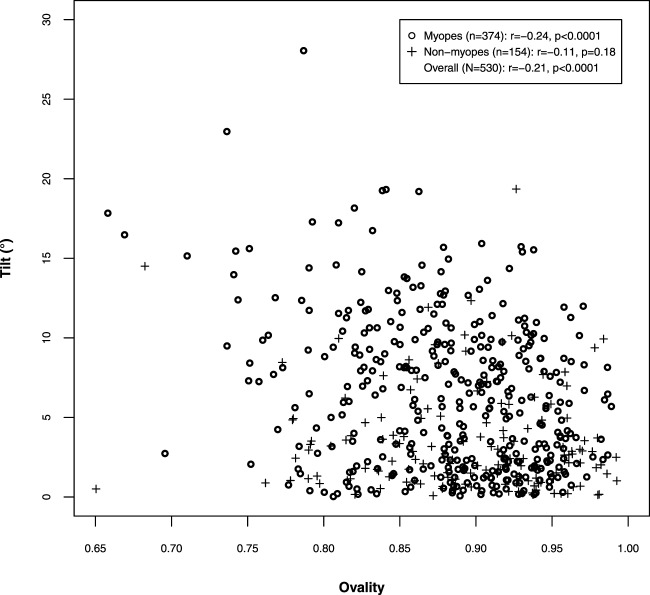
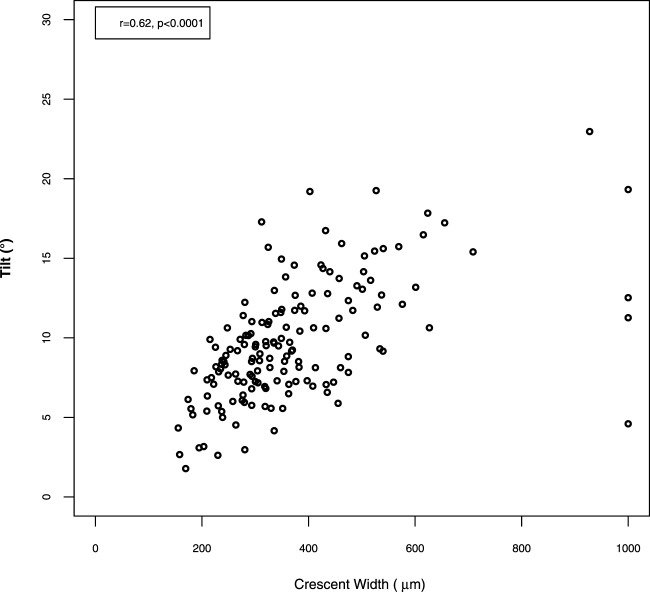
Descriptive data for both eyes are presented in Tables 1 and Supplementary Table S1 and Figures 5a and 5b to show the symmetry between eyes. The ONH was most depressed in the temporal (9:00 or 3:00) or temporal/inferior (8:00 or 4:00) locations in both myopic (80.3%) and nonmyopic (74.7%) right and left eyes, respectively (Figs. 5a, 5b). Because data from the right and left eyes were similar, only right-eye data are discussed. The median tilt (absolute value) was higher in myopic versus nonmyopic eyes (6.0° vs. 2.4°, P < 0.0001, Table 1). In myopic eyes, tilt varied by ethnicity (P < 0.0001), with highest unadjusted median values in Asian participants (10.47°), and roughly half of this value in African American (5.13°), Hispanic (5.25°), and White (5.64°) participants. Increasing amounts of tilt were moderately correlated with more spherical equivalent myopia (r = −0.25, P < 0.0001), longer axial length (r = 0.26, P < 0.0001; Fig. 6), smaller disc diameter (r = −0.22, P < 0.0001), more oval discs (r = −0.24, P < 0.0001; Fig. 7), and wider crescents (r = 0.62, P < 0.001 in eyes with crescent). All values and correlations were similar in left myopic eyes (data not shown).
Figure 5.
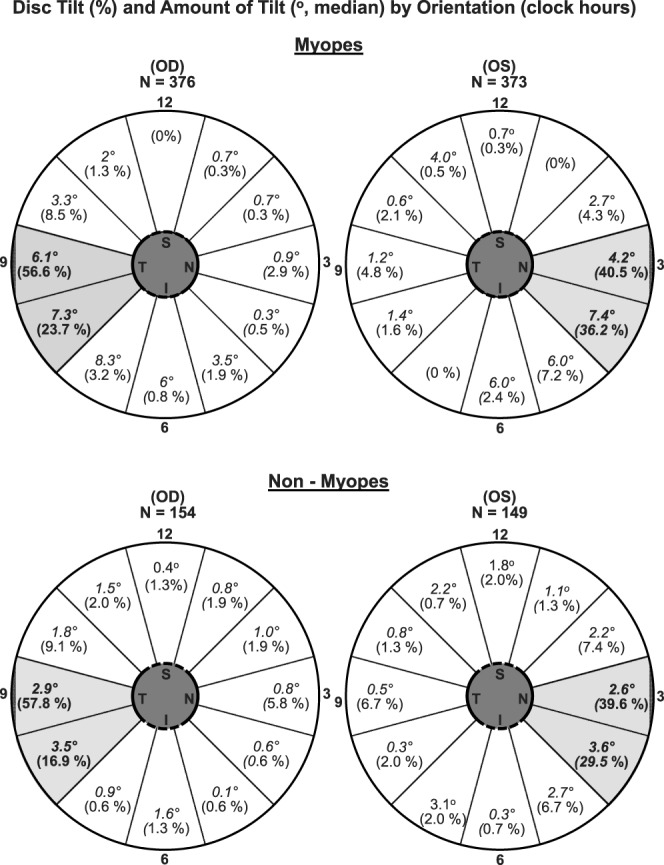
(a) Pie charts show the median degree of tilt at the clock-hour location chosen as most tilted. The shaded area includes 80.3% of right myopic eyes, with 56.6% of eyes tilted most at 9:00 (temporal) and 23.7% tilted most at 8:00 (temporal, inferior). The median amount of tilt was 6.1 degrees at 9:00 and 7.3° at 8:00. Similarly, in left myopic eyes the temporal (3:00) and temporal/inferior (4:00) locations accounted for 40.5% and 36.2%, respectively, of maximum tilts. In left eyes, the median tilt was 4.2° at 3:00 and 7.4° at 4:00. (b) The orientation of the most tilted radius was also at the temporal or temporal, inferior locations in the right (74.4%) and left (69.1%) eyes. However, the median tilt at these locations was roughly half that of the myopic eyes.
Figure 6.
The scatterplot demonstrates a significant relationship between median tilt values and axial length in myopic eyes with crescent (circles; r = 0.21, P = 0.004), but no significant relationship in eyes without crescent (crosses; r = 0.04, P = 0.58).
Figure 7.
The scatterplot comparing the cross sectional measures of maximum tilt with the en face measures of ovality shows a low to moderate correlation in the right, myopic eyes (circles; n = 374, r = −0.24, P < 0.0001) but no significant correlation in right, non-myopic eyes (crosses; n = 154, r = −0.11, P = 0.18).
Crescent.
Crescents were observed more frequently in myopic versus nonmyopic eyes (48.9% vs. 10.4%; P < 0.0001; Table 1). Among eyes with crescents, median crescent width values were similar in both refractive groups (335 μm in 157 myopic versus 386 μm in 12 nonmyopic eyes; P = 0.81). The location of greatest crescent width (determined from en face 3D disc scans) was similar to the location observed for maximum tilt (determined using cross-sectional images), with the temporal and temporal/inferior locations accounting for 98.1% vs. 100% of myopic versus nonmyopic eyes. Wider crescents were observed in eyes with more spherical equivalent myopia (r = −0.27, P = 0.0006), increased axial length (r = 0.21, P = 0.01), a more oval disc (r = −0.25, P = 0.002), smaller disc diameter (r = −0.33, P < 0.0001), and more disc tilt (r = 0.62, P < 0.0001; see Fig. 8).
Figure 8.
The scatterplot shows that higher values of tilt are moderately correlated with crescent width in myopic eyes (r = 0.62, P < 0.0001). Values of 1000 (too large to measure) occurred at any value of tilt and were included in the calculation for r.
Tilt in Eyes With and Without Crescents.
Right eyes with crescents had higher median tilt (8.8° [myopic], 9.0° [nonmyopic]) than those without crescents (2.5° [myopic], 2.1° [nonmyopic]) irrespective of refractive group (both P values < 0.0001). Eyes with crescents had similar tilt regardless of refractive group (P = 0.99). Eyes without crescents had small differences between refractive groups (2.5° in 192 myopic versus 2.1° in 138 nonmyopic eyes; P = 0.01). The degree of tilt with the highest combined sensitivity and specificity for predicting crescent presence was 50 (sensitivity = 84.07% and specificity = 81.37%).
Ovality.
The median ovality ratios showed small but statistically significant differences in myopic versus nonmyopic eyes (0.89 vs. 0.91; P = 0.03). Nearly circular ONHs, with ovality ratios of 0.90 or greater, were seen in 166 (44.4%) vs. 80 (52.6%) of myopic versus nonmyopic eyes, respectively (P = 0.10).
Ovality Versus Tilt.
Ovality was moderately related to disc tilt magnitude in myopic eyes (r = −0.24, P < 0.0001) but not in nonmyopic eyes (r = −0.11, P = 0.18; see Fig. 7). In nonmyopic eyes, 9% (14/152) of ONHs were oval (ovality ratio of 0.80 or less), 4% (n = 6) were tilted (10° or more of cross-sectional tilt) but only <1% (n = 1) matched both criteria. Among myopic eyes, a similar proportion of ONHs were oval (9%; 35/374), but more were tilted (22%; n = 82), and 4% (n = 15) matched both criteria. In addition, 5.35% (n = 20) of myopic eyes were oval but not tilted, and 17.91% (n = 67) were tilted but not oval.
Torsion.
Torsion was reported in a subset of eyes with ovality ratios <0.90. Similar proportions of myopic (208/374, 55.6%) and nonmyopic (72/152, 47.4%) eyes meeting this criterion were included in the analysis (P = 0.09). In myopes versus nonmyopes, respectively, the median absolute value was 12.3° (range, 0.0 to 89.6) vs. 8.9° (range, 0.5 to 78.8), P = 0.21; and the direction of rotation was clockwise for 61.5% (128/208) vs. 59.7% (43/72), P = 0.79. Thus, no significant differences were seen in torsion between myopic versus nonmyopic eyes. Torsion values >|45°| were present in 8.2% (17/208) of myopic versus 6.9% (5/72) of nonmyopic eyes (P = 0.74). Tilt and crescent width were greater in myopic right eyes with counterclockwise versus clockwise torsion (both P = 0.02). In these eyes with counterclockwise torsion, increased tilt and crescent width were associated with higher degrees of torsion (torsion actual value, r = −0.16, P = 0.02 and r = −0.27, P = 0.01, respectively).
Multivariable Analysis
The multivariable models for disc tilt and crescent width were limited to myopes because of the low degree of tilt and low frequency of crescents in nonmyopes. Only right eye data were modeled. Those factors associated with disc tilt (P < 0.10) in the univariate analyses were included in the multivariable models, except for ovality (due to insufficient measures to express elliptical shape independently of cross-sectional tilt), torsion (due to limited sample size), and spherical equivalent myopia (due to its strong relationship to axial length). Neither tilt nor crescent width were associated with age, sex, IOP, or CCT in myopic eyes and thus these factors were not included in the models.
Factors Associated With Disc Tilt in Myopic Eyes (Table 2).
Table 2.
Results of a Multivariable γ Model* for Disc Tilt (Degrees) and Associated Factors
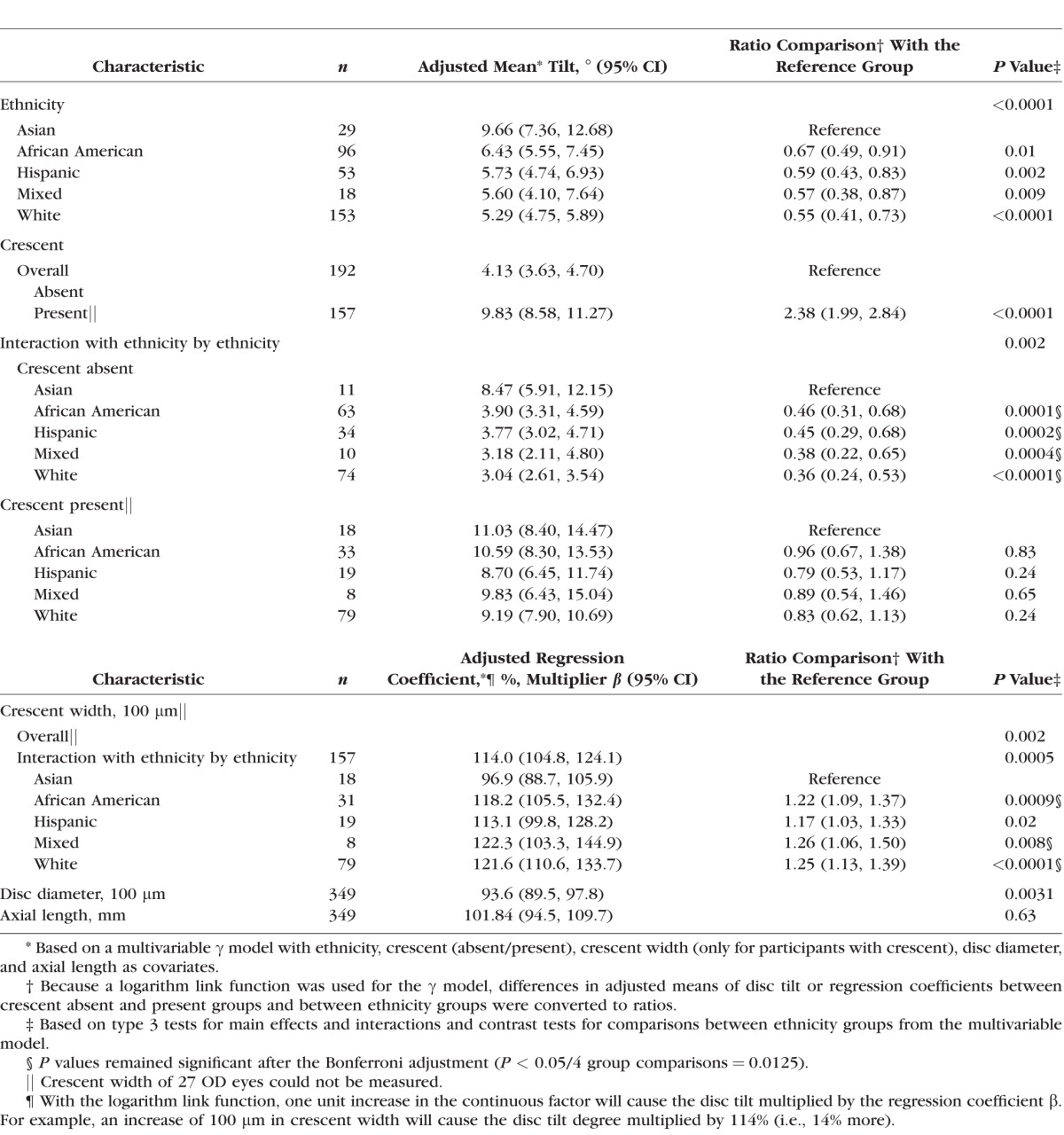
The final γ regression model for degree of disc tilt included ethnicity, disc diameter, axial length, crescent (present/absent), and crescent width (for eyes with crescent only) as covariates, along with the following two interaction terms: ethnicity and either crescent (yes/no) or crescent width. Based on this model, eyes with crescents had more than twice the amount of tilt than eyes without crescents (adjusted mean: 9.83° vs. 4.13°, P < 0.0001), and crescent width was positively associated with tilt such that each 100-μm increase in crescent width was associated with a corresponding 14% increase in the degree of tilt (P = 0.002). In addition, disc diameter, but not axial length, was significantly associated with tilt (P = 0.003). Specifically, each 100-μm increase in disc diameter was associated with a 6.4% reduction in the degree of tilt, that is, a larger disc was associated with less tilt (Table 2).
Disc tilt varied by ethnicity (P < 0.0001), with Asian eyes being the most tilted (adjusted mean 9.66°, 95% CI: 7.36°–12.68°) and Whites the least (adjusted mean 5.29°, 95% CI: 4.75°–5.89°). When compared with Asian eyes, African American, Hispanic, mixed, and White eyes all had significantly less tilt (ratio of the adjusted means ranged from 0.55–0.67, all P values < 0.01). However, a statistically significant interaction was identified between ethnicity and crescent (P = 0.002). In eyes without crescents, Asians had the most tilt (adjusted mean 8.47°, 95% CI: 5.91°–12.15°) and the other ethnic groups had less than half this amount (adjusted mean ranged from 3.04° White to 3.90° African American [ratios of adjusted means ranged from 0.36 to 0.46, all P < 0.0004]). In eyes with crescents, values of tilt were equally high with no significant differences between ethnic groups.
A second interaction was observed between ethnicity and crescent width (P = 0.0005), with a significant association observed between disc tilt and crescent width in all ethnic groups (all P values ≤ 0.02) except Asians (P = 0.49). For the White, African American, Hispanic and Mixed groups, wider crescents were associated with more tilt; with an increase of 100 μm in crescent width associated with 18% more tilt in African Americans (P = 0.004), 13% more in Hispanics (P = 0.05), 22% more in mixed (P = 0.02), and 22% more in Whites (P < 0.0001). For Asians, although crescent width and tilt were inversely related, this was not statistically significant (P = 0.49). Furthermore, when compared with Asian eyes with crescents, the associations between crescent width and tilt were stronger in the other ethnicity groups (P for all comparisons < 0.02).
Factors Associated With Crescent Width in Myopic Eyes (Table 3).
Table 3.
Results of a Multivariable Tobit Model* for Crescent Width and Associated Factors
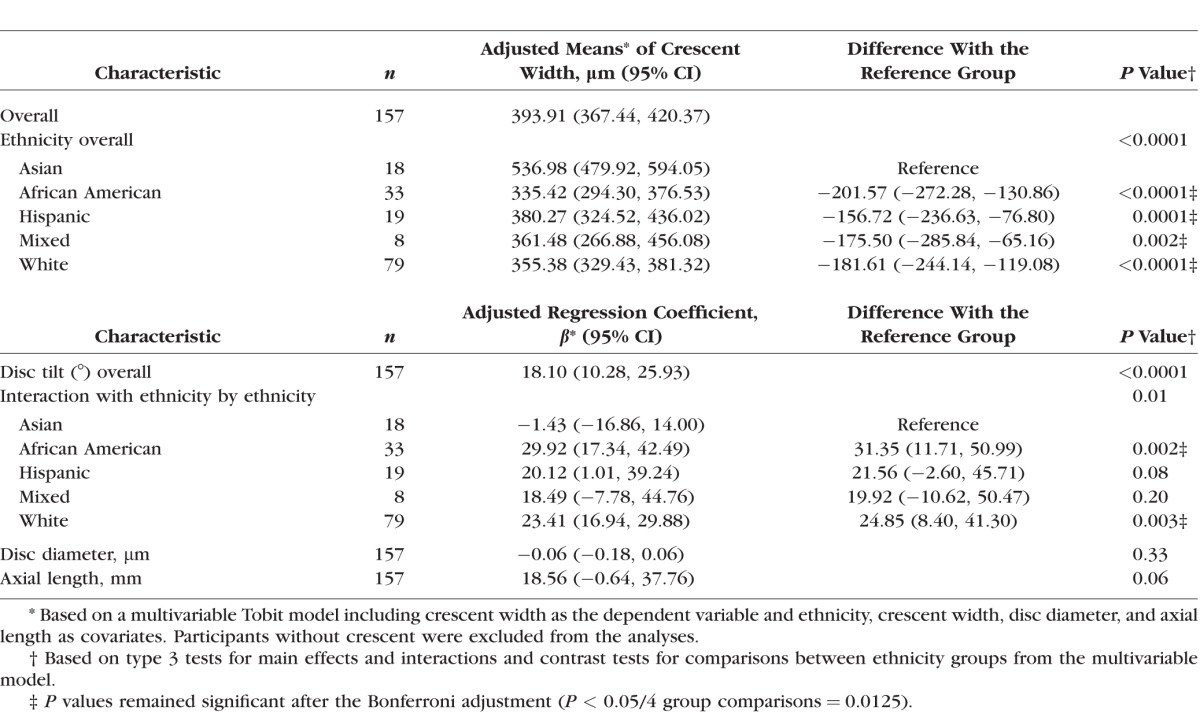
A second multivariable model (Tobit) was used to investigate the factors associated with crescent width in myopic eyes with a crescent and available crescent width data (n = 157). Crescent width was associated with ethnicity (P < 0.0001) and disc tilt (P < 0.0001; Table 3). Asians had the widest crescents (adjusted mean: 536.98 μm, 95% CI: 479.92–594.05 μm), and African Americans the smallest (adjusted mean: 335.42 μm, 95% CI: 294.30–376.53 μm), with a statistically significant difference in crescent width observed between Asians and each of the other ethnic groups (P ≤ 0.002 for all comparisons). A 1° increase in tilt was associated with a small increase of 18.10 μm (95% CI: 10.28–25.93) in crescent width (P < 0.0001). An interaction between tilt and ethnicity was observed (P = 0.01), with significant associations between tilt and crescent width seen for White (P < 0.0001), African- American (P < 0.0001), and Hispanic eyes (P = 0.04), but not for Asian (P = 0.86) or mixed eyes (P = 0.17). When compared with Asians, the associations between tilt and crescent width were strongest and reached statistical significance only for African Americans (P = 0.002) and Whites (P = 0.003). Neither disc diameter (P = 0.33) nor axial length (P = 0.06) were significantly associated with crescent width.
Discussion
Overview
This is the first study to compare four key ONH characteristics (maximum disc tilt, crescent width, ovality, and torsion) in a multi-ethnic population of young adults with and without myopia living in the United States. Crescent was observed approximately five times more frequently in myopic eyes when compared with nonmyopic eyes (49% vs. 10%) and the median degree of tilt was about double (6.0° vs. 2.4°). The degree of tilt was at least twice as high in eyes with crescents versus those without, regardless of refractive group, indicating a strong relationship between tilt and crescent.
Ethnicity was also strongly associated with tilt and crescent, with ONHs in Asian eyes having the most tilt, even in the absence of crescent, and the widest crescents among all ethnic groups. However, in eyes with crescents, tilt was similar across ethnic and refractive groups, further reflecting the stronger relationship between crescent and tilt. Unlike tilt and crescent, all measures of torsion were similar in myopes and nonmyopes, and a clinically inconsequential difference was found in ovality ratios between refractive groups, suggesting lesser importance for these measures in distinguishing between young adult myopic and nonmyopic eyes.
Ovality and Torsion in Myopes and Nonmyopes
Our median ovality ratios were nearly identical to those reported in a cohort of Japanese high school students (0.9218) suggesting that our automated method for OCT scan measurement is valid. Hosseini reported a higher correlation between tilt and ovality in an older, predominantly White clinical population with suspected or definite glaucoma,19 raising the possibility that these associations differ according to age or pathology. Because many previous studies use ovality as a proxy measure for tilt, their results should be interpreted very carefully because these measures are not interchangeable.10,12,13,15,16 Future research should address these two disc characteristics separately to better understand the biomechanical stresses and strains that influence final ONH shape.
Although we found no overall differences in torsion between refractive groups, we examined the subset of myopic right eyes with “inferior” or counterclockwise rotation because of recent reports that counterclockwise rotation was associated with reduced RNFL and macular thickness as well as ocular characteristics including more oval discs and larger BPPA.41 Consistent with Sung et al.41 we found a lower frequency of young myopic adults with counterclockwise rotation of the right ONH and we also observed that increased cross-sectional tilt and wider crescents were associated with the degree of rotation in this group. Longitudinal studies would be useful to investigate whether torsion changes over time, and whether counterclockwise rotation or tilt are risk factors for age related visual loss in myopes with20 or without glaucoma.
Tilt and Crescent in Myopic and Nonmyopic Eyes
The median values for disc tilt (2° to 10°) in this study were near the low range of values (3.5° to 22°) reported by others.14,17,18,19,20 However, studies are not directly comparable because of the differences between study participants (in terms of age, ethnicity, sex, and associated ocular conditions such as glaucoma), instrumentation (various OCT devices or HRT), landmark selection (usually Bruch's membrane opening, which includes the crescent, or at the inner limiting membrane surface), corrections for image tilt, or the selection of the radius measured. Although these differences between previous studies limit comparisons, our data, which are based on standard methods for all participants, help to clarify the influence of ethnicity and crescent on tilt values.
In addition to the higher frequency of crescents in myopic eyes and the increased amount of tilt in eyes with crescents, we also found that maximum tilt and greatest crescent width typically occurred at the temporal and temporal/inferior locations. These characteristics are consistent with the acquired changes in ONH shape observed during myopic progression in a cohort of Korean children followed longitudinally.9 Some studies have limited discussions of “tilted” ONHs to eyes with an inferior tilt, a characteristic that evokes a congenital condition called tilted disc syndrome.42 Few ONHs in our study had inferior tilts and crescents (six myopic right eyes and zero nonmyopic eyes). Because an unequivocal distinction between acquired and congenital changes would require longitudinal observations and because few myopic eyes had both characteristics, we did not eliminate any eyes from analysis.
The occurrence (10% to 13%) of crescents in nonmyopic eyes was surprising, as was their similarity to crescents in myopic eyes in terms of median width and associated tilt as well as landmark identification of the disc margin and crescent termination, explaining why the intergrader agreement did not vary much by refractive error. Interestingly, crescents in nonmyopic eyes were found for all values of axial length, from 21.5 mm to < 25 mm.
Because of the relatively infrequent occurrence of crescent and high tilt values in nonmyopic eyes, the remaining discussion is limited to myopic eyes.
Factors Associated With Tilt and Crescent in Myopes
Disc Tilt.
The association we found between crescent and tilt was not unexpected, but the actual quantification of the association (adjusted values of 9.83° in eyes with crescent versus 4.13° in eyes without crescent) was striking. On average, eyes with crescents had similar, high values of tilt, regardless of ethnicity. However, unsuspectedly high values of tilt occurred in Asian eyes without crescents (median value 9.9), values that were at least double when compared with other ethnicities.
The association between smaller disc diameter and increased disc tilt is interesting. Because we measured the actual distance, not a projection of the diameter to the en face plane, smaller diameter is not confounded by rotation around the vertical axis. Our findings may reflect regional differences in the distensibility of the peripapillary sclera, allowing some ONHs to enlarge (equal stress and strain in all peripapillary locations), whereas others tilt (asymmetric stress and/or strain). When adjusted for other factors, axial length was not associated with the degree of disc tilt in these young adult myopes. However, others14,19 have noted a positive association between increased axial length and disc tilt or higher degrees of visual field loss in glaucoma patients. Possible reasons for the different results may include age and the presence of glaucoma.
Crescent Width.
Quantification of crescent width depends on the reliable location of landmarks, which we were able to achieve in this study. In our young adult myopes, wider crescents were associated with Asian ethnicity and more disc tilt in the multivariable model. Our model also showed that increased tilt was associated with increased crescent width in non-Asian ethnic groups, similar to longitudinal changes related to myopia progression reported by Kim et al.9 Crescents are often thought to occur in eyes with excessive axial elongation, but axial length was not independently associated with crescent width or tilt in our myopic eyes after adjustment for other covariates. Roughly half of the crescents occurred in myopic eyes with “normal” axial lengths between 23 and <26 mm,24 an observation that supports Curtin's proposal that it is the presence of crescent, rather than a particular value of axial length, that indicates the length that is “excessive” for the individual eye. In other words, tissue strain around the ONH may result in crescent formation at a variety of axial lengths, probably depending on multiple other biomechanical factors. No evidence of RPE/Bruch's membrane was seen in the majority of our scans with crescents, consistent with recent reports that Bruch's membrane was not present in “myopic crescents” at young ages, but was present in the BPPA in the majority of older adults.23 Other groups that have reported associations between BPPA and tilt have probably included eyes with either BPPA and/or crescents. Future research should tease these factors out as the former could signal age-related changes and the latter reflects changes present at least by young adult age23 that might or might not portend an increased risk of age-related eye pathology.
Clinical Implications
Our data show that higher values of tilt should be suspected in all Asian eyes and in all eyes with crescents regardless of ethnicity. Previously, we have shown that choroidal thinning is related to increased spherical equivalent myopia, longer axial length, crescent, and Asian ethnicity.43 To the extent that increased tilt and crescent width signal excessive tissue strain in and around the ONH5–7 and considering that choroidal thinning may signal nonperfusion of overlying retinal tissues, Asian eyes may have an increased susceptibility to develop reduced acuity, retinal detachment, glaucomatous optic atrophy, or other myopic pathologies as they age.4,44,45 This potentially heightened susceptibility coupled with the extreme projected increase in prevalence of myopia among older Asian adults4 portend a mounting challenge to deliver eye and rehabilitative vision care in Asian nations. For other ethnicities, eyes without crescents have low values of tilt, and perhaps a lower risk of pathologic complications.
We have shown that axial length is not significantly associated with increased tilt when ethnicity, crescent, and ONH diameter are considered. Although tilt has recently been identified as a potential risk factor for reduced visual function2,19 or for shifting of the peak RNFL thicknesses,17 the actual value of tilt that is problematic is not known and our data cannot address this point.
The ovality measure should not be used as a proxy for tilt based on our data showing the majority of ONHs that were tilted by 10° or more were not identified by an ovality ratio of 0.80. The other commonly used clinical observation of tilt using stereo-paired photographs was also problematic and might have identified only two of our study eyes (those with tilt > 20°, a criterion shown to be necessary for reliable detection of tilt by Takasaki et al.18). Studies using photographs have reported higher frequencies of tilt in Asian children living outside the United States, raising the possibility that ethnicity and other cultural or geographic factors influence disc tilt or that photographic interpretation can vary. Choosing between these possibilities would require additional studies including quantitative measures such as those undertaken here.
Based on our experience, young adult eyes with crescents lack Bruch's membrane, therefore requiring manual corrections to the disc margin to ensure valid measures of ONH characteristics. The associations we described for tilt and crescent may not hold in the eyes of older adults with BPPA, which has a different microstructure, even though the ophthalmoscopic signs are similar. Given the importance of BPPA on glaucoma progression and the lack of progression seen in middle-aged adults with “BPPA without Bruch's membrane,”23 care should be taken before diagnosing or treating young adults with myopic crescent as low-tension glaucoma patients, in the absence of demonstrated progressive visual field loss.46
Strengths and Limitations
The strengths of this study include its multi-ethnic population, clear definitions of the ONH characteristics, and the careful and standardized process of measurement that was followed. Our measures of tilt and crescent width depended on a disc margin that frequently required manual corrections when crescents were present, and thus were time consuming. We measured a single radius, judged to be most tilted, and used the same radius to measure crescent width. Because the radius of maximum tilt often occurred in a similar location as the widest crescent; we believe that our results would be similar had we quantified crescents differently. Although crescent width could not be measured in 15% of the myopic eyes with crescents because of either the selection or the quality of the scans obtained, there was no apparent systematic loss of measures that would affect our findings. Neither fundus photos nor visual fields were available. Thus, we could not reference our clock hour or torsion values to the line connecting the disc and macula. We could not evaluate potential relationships between ONH characteristics and visual field sensitivity. Although we do not suspect visual field loss in any of the young adults we included in the study, it is possible that a few were included. However, it is not likely that our results were influenced to any great extent by occult pathology.
The custom Matlab program that we developed, which matched elliptical shapes to the disc margin, provided fast, reliable, and valid measures of elliptical shape, radii, and torsion. Although we limited our reports of torsion to eyes with an ovality ratio <0.90, actual measures of torsion were determined in all eyes. Our method may simplify future research investigating relationships between torsion and visual field loss.
Finally, although our data are cross-sectional, roughly half of young myopic adults had evidence (tilt and/or crescent) of tissue strain in response to biomechanical factors occurring early in life. Longitudinal studies will be necessary to determine whether such eyes are at increased risk to develop age-related ocular pathology including glaucoma, retinal detachments, or other myopia-related pathologies.
Conclusion and Future Directions
Our data, based on carefully collected measurements in a multi-ethnic group of young adults, help to clarify the influence of ethnicity and spherical equivalent myopia on ONH characteristics. Overall, roughly 50% of young adult myopes had crescents compared to only 10% of nonmyopes. Eyes with crescents had higher values of tilt, and eyes without crescents had low values of tilt, regardless of refractive group. An exception occurred for Asian eyes without crescents, with tilt values that were roughly 150% those of other ethnic groups. In myopes, after adjustment for covariates, axial length was not associated with tilt or crescent width, but smaller disc diameter was related to increased tilt. Ovality was found to be an unacceptable proxy measure for tilt, and few eyes had the degree of tilt likely to be reliably detected by expert interpretation of stereo-paired photographs. In our experience, eyes with crescents lack RPE/Bruch's membrane in the peripapillary whitish zone seen by ophthalmoscopy. These eyes require manual determination of the disc margin for valid measures of ONH characteristics and are likely to have higher levels of tilt that cannot be verified without direct measurement of OCT scans. Automatic algorithms to determine the disc margin in eyes with myopic crescents would greatly simplify and improve the validity of OCT ONH measurements. These data may inform future studies of biomechanical properties, or of retinal pathology, of the myopic eye.
Supplementary Material
Acknowledgments
The authors thank Lei Liu, PhD, for writing the custom Matlab programs and for many helpful discussions related to data measurement and review.
Supported by the following National Eye Institute (United States) Grants: EY11805, EY11740, EY11756, EY11754, EY11752, EY11755.
Disclosure: W.L. Marsh-Tootle, None; E. Harb, None; W. Hou, None; Q. Zhang, None; H.A. Anderson, None; K. Weise, None; T.T. Norton, None; J. Gwiazda, None; L. Hyman, None
Appendix. COMET Study Group
Study Chair: J. Gwiazda (Study Chair/PI), T. Norton, K. Grice (1996–1999), C. Fortunato (1999–2000), C. Weber (2000–2003), A. Beale (2003–2005), D. Kern (2005–2008), S. Bittinger (2008–2011), L. Deng (2010–present), D. Ghosh (2011–2013), R. Trumbull (2013–present), R. Pacella (1996–1998).
Coordinating Center: L. Hyman (PI), M.C. Leske (until 2003), M. Hussein (until 2003), L.M. Dong (2003–2010), M. Fazzari (2011–2012), W. Hou (2012–present), L. Dias (1998–present), R. Harrison (1997–1998), W. Zhu (until 2006), E. Schoenfeld (until 2005), Q. Zhang (2006–present), Y. Wang (2000–2005), A. Yassin (1998–1999), E. Schnall (1997–1998), C. Rau (1999–2000), J. Thomas (2000–2004), M. Wasserman (2004–2006), Y. Chen (2006–2008), S. Ahmed (2009–2011), L. Merill (2011–2013), L. Passanant (1998–2004), M. Rodriguez (2000–2013), A. Schmertz (1998), A. Park (1999–2000), P. Neuschwender (until 1999), G. Veeraraghavan (1999–2001), A. Santomarco (2001–2004), L. Sisti (2005–2006), L. Seib (2007–present).
National Eye Institute: D. Everett (Project Officer).
Clinical Centers:
University of Alabama at Birmingham School of Optometry: W. Marsh-Tootle (PI), K. Weise (1998–present), M. Frazier (2010–present), C. Baldwin (1998–2013), C. Dillard (2009–2013), K. Becker (1999–2003), J. Raley (1997–1999), A. Rawden (1997–1998), N. Harris (1998–1999), T. Mars (1997–2003), R. Rutstein (until 2003).
New England College of Optometry: D. Kurtz (PI until 2007), E. Weissberg (1999–present, PI since 2007), B. Moore (until 1999), E. Harb (2008–present), R. Owens (until 2013), S. Martin (until 1998), J. Bolden (1998–2003), J. Smith (2001–2008), D. Kern (2005–2008), S. Bittinger (2008–2011), D. Ghosh (2011–2013), B. Jaramillo (2000–2003), S. Hamlett (1998–2000), L. Vasilakos (2002–2005), S. Gladstone (2004–2007), C. Owens (2006–2009), P. Kowalski (until 2001), J. Hazelwood (2001–2003).
University of Houston College of Optometry: R. Manny (PI), C. Crossnoe (until 2003), K. Fern, H. Anderson (2010–present), S. Deatherage (until 2007), C. Dudonis (until 2007), S. Henry (until 1998), J. McLeod (1998–2004, 2007–2008), M. Batres (2004–2006), J. Quiralte (1998–2005), G. Garza (2005–2007), G. Solis (2007–2011), J. Do (2012–2013), A. Ketcham (2007–2011).
Pennsylvania College of Optometry: M. Scheiman (PI), K. Zinzer (until 2004), E. Feigenbutz (2010–2011), K. Pollack (2003–2013), C. Feinstein (2010–2012), T. Lancaster (until 1999), T. Elliott (until 2001), M. Bernhardt (1999–2000), D. Ferrara (2000–2001), J. Miles (2001–2004), S. Wilkins (2001–2003), R. Wilkins (2002–2003), J.N. Lynch (2003–2005), D. D'Antonio (2005–2008), L. Lear (2006–2008), S. Dang (2008–2010), C. Sporer (2010–2011), M. Jameson (2011–2013), A. Grossman (2001–2003), M. Torres (1997–2000), H. Jones (2000–2001), M. Madigan-Carr (2001–2003), T. Sanogo (1999–2003), J. Bailey (until 2003).
Data and Safety Monitoring Committee: R. Hardy (Chair), A. Hillis, D. Mutti, R. Stone Sr., C. Taylor.
References
- 1. Holden BA,, Fricke TR,, Wilson DA,, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016; 123: 1036–1042. [DOI] [PubMed] [Google Scholar]
- 2. Koh V,, Tan C,, Tan PT,, et al. Myopic maculopathy and optic disc changes in highly myopic young Asian eyes and impact on visual acuity. Am J Ophthalmol. 2016; 164: 69–79. [DOI] [PubMed] [Google Scholar]
- 3. Vitale S,, Sperduto RD,, Ferris FL., 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009; 127: 1632–1639. [DOI] [PubMed] [Google Scholar]
- 4. Verkicharla PK,, Ohno-Matsui K,, Saw SM. Current and predicted demographics of high myopia and an update of its associated pathological changes. Ophthalmic Physiol Opt. 2015; 35: 465–475. [DOI] [PubMed] [Google Scholar]
- 5. Burgoyne CF,, Downs JC,, Bellezza AJ,, et al. The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Retin Eye Res. 2005; 24: 39–73. [DOI] [PubMed] [Google Scholar]
- 6. Norman RE,, Flanagan JG,, Sigal IA,, et al. Finite element modeling of the human sclera: influence on optic nerve head biomechanics and connections with glaucoma. Exp Eye Res. 2011; 93: 4–12. [DOI] [PubMed] [Google Scholar]
- 7. Fazio MA,, Grytz R,, Bruno L,, et al. Regional variations in mechanical strain in the posterior human sclera. Invest Ophthalmol Vis Sci. 2012; 53: 5326–5333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hsu CH,, Chen RI,, Lin SC. Myopia and glaucoma: sorting out the difference. Curr Opin Ophthalmol. 2015; 26: 90–95. [DOI] [PubMed] [Google Scholar]
- 9. Kim TW,, Kim M,, Weinreb RN,, et al. Optic disc change with incipient myopia of childhood. Ophthalmology. 2012; 119: 21–26. [DOI] [PubMed] [Google Scholar]
- 10. Samarawickrama C,, Mitchell P,, Tong L,, et al. Myopia-related optic disc and retinal changes in adolescent children from Singapore. Ophthalmology. 2011; 118: 2050–2057. [DOI] [PubMed] [Google Scholar]
- 11. Jonas JB,, Budde WM,, Panda-Jonas S. Ophthalmoscopic evaluation of the optic nerve head. Surv Ophthalmol. 1999; 43: 293–320. [DOI] [PubMed] [Google Scholar]
- 12. Tay E,, Seah SK,, Chan SP,, et al. Optic disk ovality as an index of tilt and its relationship to myopia and perimetry. Am J Ophthalmol. 2005; 139: 247–252. [DOI] [PubMed] [Google Scholar]
- 13. Park HY,, Lee K,, Park CK. Optic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopia. Ophthalmology. 2012; 119: 1844–1851. [DOI] [PubMed] [Google Scholar]
- 14. Choi JA,, Park HY,, Shin HY,, et al. Optic disc tilt direction determines the location of initial glaucomatous damage. Invest Ophthalmol Vis Sci. 2014; 55: 4991–4998. [DOI] [PubMed] [Google Scholar]
- 15. Chung JK1,, Yoo YC. Correct calculation circle location of optical coherence tomography in measuring retinal nerve fiber layer thickness in eyes with myopic tilted discs. Invest Ophthalmol Vis Sci. 2011; 52: 7894–7900. [DOI] [PubMed] [Google Scholar]
- 16. Shin HY,, Park HY,, Park CK. The effect of myopic optic disc tilt on measurement of spectral-domain optical coherence tomography parameters. Br J Ophthalmol. 2015; 99: 69–74. [DOI] [PubMed] [Google Scholar]
- 17. Hwang YH,, Yoo C,, Kim YY. Myopic optic disc tilt and the characteristics of peripapillary retinal nerve fiber layer thickness measured by spectral-domain optical coherence tomography. J Glaucoma. 2012; 21: 260–265. [DOI] [PubMed] [Google Scholar]
- 18. Takasaki H,, Higashide T,, Takeda H,, et al. Relationship between optic disc ovality and horizontal disc tilt in normal young subjects. Jpn J Ophthalmol. 2013; 57: 34–40. [DOI] [PubMed] [Google Scholar]
- 19. Hosseini H,, Nassiri N,, Azarbod P,, et al. Measurement of the optic disc vertical tilt angle with spectral-domain optical coherence tomography and influencing factors. Am J Ophthalmol. 2013; 156: 737–744. [DOI] [PubMed] [Google Scholar]
- 20. Park HY,, Choi SI,, Choi JA,, et al. Disc torsion and vertical disc tilt are related to subfoveal scleral thickness in open-angle glaucoma patients with myopia. Invest Ophthalmol Vis Sci. 2015; 56: 4927–4935. [DOI] [PubMed] [Google Scholar]
- 21. Lee KS,, Lee JR,, Kook MS. Optic disc torsion presenting as unilateral glaucomatous-appearing visual field defect in young myopic Korean eyes. Ophthalmology. 2014; 121: 1013–1019. [DOI] [PubMed] [Google Scholar]
- 22. Park HY,, Lee KI,, Lee K,, et al. Torsion of the optic nerve head is a prominent feature of normal-tension glaucoma. Invest Ophthalmol Vis Sci. 2014; 56: 156–163. [DOI] [PubMed] [Google Scholar]
- 23. Hwang YH,, Jung JJ,, Park YM,, et al. Effect of myopia and age on optic disc margin anatomy within the parapapillary atrophy area. Jpn J Ophthalmol. 2013; 57: 463–470. [DOI] [PubMed] [Google Scholar]
- 24. Curtin BJ. The Myopias: Basic Science and Clinical Management. Philadelphia, PA: Harper & Row; 1985. [Google Scholar]
- 25. Cheng SC,, Lam CS,, Yap MK. Prevalence of myopia-related retinal changes among 12-18 year old Hong Kong Chinese high myopes. Ophthalmic Physiol Opt. 2013; 33: 652–660. [DOI] [PubMed] [Google Scholar]
- 26. Jonas JB. Clinical implications of peripapillary atrophy in glaucoma. Curr Opin Ophthalmol. 2005; 16: 84–88. [DOI] [PubMed] [Google Scholar]
- 27. De Moraes CG,, Juthani VJ,, Liebmann JM,, et al. Risk factors for visual field progression in treated glaucoma. Arch Ophthalmol. 2011; 129: 562–568. [DOI] [PubMed] [Google Scholar]
- 28. Hayashi K,, Tomidokoro A,, Lee KY,, et al. Spectral-domain optical coherence tomography of β-zone peripapillary atrophy: influence of myopia and glaucoma. Invest Ophthalmol Vis Sci. 2012; 53: 1499–1505. [DOI] [PubMed] [Google Scholar]
- 29. Hyman L,, Gwiazda J,, Marsh-Tootle WL,, et al. The Correction of Myopia Evaluation Trial (COMET): design and general baseline characteristics. Control Clin Trials. 2001; 22: 573–592. [DOI] [PubMed] [Google Scholar]
- 30. Gwiazda J,, Hyman L,, Hussein M,, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003; 44: 1492–1500. [DOI] [PubMed] [Google Scholar]
- 31. Gwiazda JE,, Hyman L,, Norton TT,, et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci. 2004; 45: 2143–2151. [DOI] [PubMed] [Google Scholar]
- 32. Fern KD,, Manny RE,, Gwiazda J,, & the COMET Group. Intraocular pressure and central corneal thickness in the COMET cohort. Optom Vis Sci. 2012; 89: 1225–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mwanza JC,, Oakley JD,, Budenz DL,, et al. Cirrus Optical Coherence Tomography Normative Database Study Group. Ability of cirrus HD-OCT optic nerve head parameters to discriminate normal from glaucomatous eyes. Ophthalmology. 2011; 118: 241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee S,, Han SX,, Young M,, et al. Optic nerve head and peripapillary morphometrics in myopic glaucoma. Invest Ophthalmol Vis Sci. 2014; 55: 4378–4393. [DOI] [PubMed] [Google Scholar]
- 35. Reis AS,, Sharpe GP,, Yang H,, Nicolela MT,, Burgoyne CF,, Chauhan BC. Optic disc margin anatomy in patients with glaucoma and normal controls with spectral domain optical coherence tomography. Ophthalmology. 2012; 119: 738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Strouthidis NG,, Yang H,, Downs JC,, Burgoyne CF. Comparison of clinical and three-dimensional histomorphometric optic disc margin anatomy. Invest Ophthalmol Vis Sci. 2009; 50: 2165–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lee KY,, Tomidokoro A,, Sakata R,, et al. Cross-sectional anatomic configurations of peripapillary atrophy evaluated with spectral domain-optical coherence tomography. Invest Ophthalmol Vis Sci. 2010; 51: 666–671. [DOI] [PubMed] [Google Scholar]
- 38. Nonaka A,, Hangai M,, Akagi T,, et al. Biometric features of peripapillary atrophy beta in eyes with high myopia. Invest Ophthalmol Vis Sci. 2011; 52: 6706–6713. [DOI] [PubMed] [Google Scholar]
- 39. Dodd S,, Bassi A,, Bodger K,, Williamson P. A comparison of multivariable regression models to analyse cost data. J Eval Clin Pract. 2006; 12: 76–86. [DOI] [PubMed] [Google Scholar]
- 40. Russell RA,, Crabb DP. On Alternative methods for measuring visual field decay: Tobit linear regression. Invest Ophthalmol Vis Sci. 2011; 52: 9539–9540. [DOI] [PubMed] [Google Scholar]
- 41. Sung MS,, Kang YS,, Heo H,, Park SW. Characteristics of optic disc rotation in myopic eyes. Ophthalmology. 2016; 123: 400–407. [DOI] [PubMed] [Google Scholar]
- 42. Vongphanit J,, Mitchell P,, Wang JJ. Population prevalence of tilted optic disks and the relationship of this sign to refractive error. Am J Ophthalmol. 2002; 133: 679–685. [DOI] [PubMed] [Google Scholar]
- 43. Harb E,, Hyman L,, Gwiazda J,, et al. Choroidal thickness profiles in myopic eyes of young adults in the Correction of Myopia Evaluation Trial Cohort. Am J Ophthalmol. 2015; 160: 62–71.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mrejen S,, Spaide RF. Optical coherence tomography: imaging of the choroid and beyond. Surv Ophthalmol. 2013; 58: 387–429. [DOI] [PubMed] [Google Scholar]
- 45. Ikuno Y1,, Tano Y. Retinal and choroidal biometry in highly myopic eyes with spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2009; 50: 3876–3880. [DOI] [PubMed] [Google Scholar]
- 46. Doshi A1,, Kreidl KO,, Lombardi L,, Sakamoto DK,, Singh K. Nonprogressive glaucomatous cupping and visual field abnormalities in young Chinese males. Ophthalmology. 2007; 114: 472–479. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.